Abstract
Objectives
The aim was to compare the accuracy of linear bone measurements of cone beam CT (CBCT) with multidetector CT (MDCT) and validate intraoral soft-tissue measurements in CBCT.
Methods
Comparable views of CBCT and MDCT were obtained from eight intact cadaveric heads. The anatomical positions of the gingival margin and the buccal alveolar bone ridge were determined. Image measurements (CBCT/MDCT) were performed upon multiplanar reformatted data sets and compared with the anatomical measurements; the number of non-assessable sites (NASs) was evaluated.
Results
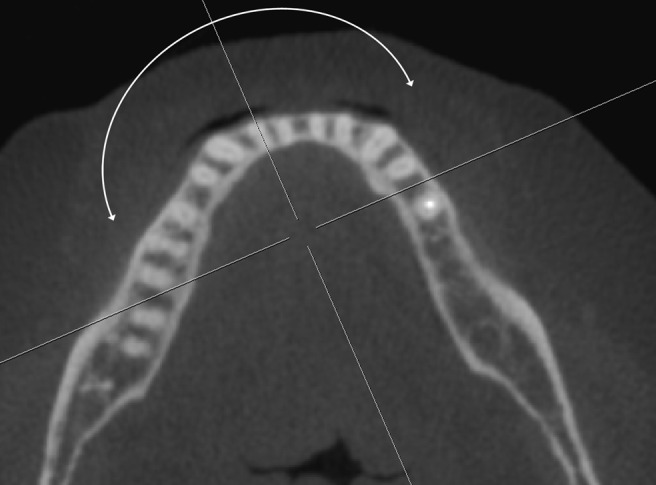
Radiological measurements were accurate with a mean difference from anatomical measurements of 0.14 mm (CBCT) and 0.23 mm (MDCT). These differences were statistically not significant, but the limits of agreement for bone measurements were broader in MDCT (−1.35 mm; 1.82 mm) than in CBCT (−0.93 mm; 1.21 mm). The limits of agreement for soft-tissue measurements in CBCT were smaller (−0.77 mm; 1.07 mm), indicating a slightly higher accuracy. More NASs occurred in MDCT (14.5%) than in CBCT (8.3%).
Conclusions
CBCT is slightly more reliable for linear measurements than MDCT and less affected by metal artefacts. CBCT accuracy of linear intraoral soft-tissue measurements is similar to the accuracy of bone measurements.
Keywords: computed tomography, CBCT, image quality, accuracy, soft tissue
Introduction
Cone beam CT (CBCT) was originally developed at the Mayo Clinic in 1982 for angiography procedures.1 Since its introduction into craniofacial imaging, CBCT has proved to be a valuable diagnostic tool, primarily because of its lower radiation exposure than multidetector CT (MDCT),2-6 but also for the short acquisition time, small physical size and moderate costs.7-9 Today clinicians frequently request linear measurements performed upon cross-sectional image data. The question has therefore been raised whether CBCT may be capable of replacing MDCT for these needs in dentomaxillofacial imaging. So far, various efforts have been made to compare accuracy and image quality of CBCT and MDCT. However, an adequate understanding of the inherent differences in the properties of both types of image data is necessary to draw an appropriate comparison.
One particular advantage of CBCT data volume is its composition of isotropic voxels providing the same spatial resolution when reconstructed in multiplanar image reformations (MPRs).9 In contrast to this, conventional MDCT data are composed of anisotropic voxels, as the coronal dimension (i.e. along the z-axis) is determined by several factors such as slice collimation and pitch (i.e. table travel per rotation divided by the collimation of the X-ray beam).10 The spatial resolution in the z-axis of current MDCT scanners is limited to 0.4–0.6 mm, and therefore decreases when reconstructed from the original raw data. A further advantage is the comparably shorter acquisition time, which may help reduce motion artefacts due to patient movement. Most CBCT devices are capable of providing a minimal voxel resolution between 0.07 mm and 0.25 mm, exceeding most commercially available high-resolution MDCT scanners.9
On the other hand, CBCT imaging presents a few drawbacks. The displayed greyscale values in CBCT are arbitrary, do not correspond to the Hounsfield unit (HU) scale used in MDCT, and reportedly differ from device to device.11 Yet the ability to derive HUs from grey levels would open new opportunities for qualitative appraisals and comparative research. Mah et al11 attempted to convert greyscale in CBCT into a “rescaled HU” with a proposed coefficient. However, Bryant and colleagues12,13 argued that the greyscale value of CBCT varies linearly with the total mass in the slice. The greyscale value will therefore not only depend on the attenuation coefficient measurement, as described by the Hounsfield equation, but also on the total mass of the object. A further limitation of CBCT imaging is that structures outside the limited field of view (FOV) may produce density variability in the scanned volume and cause a decrease of image contrast.14-16 Lastly, compared with MDCT, CBCT images are associated with increased noise and scatter radiation,17 which result in less soft-tissue contrast resolution.2,7,18 Therefore, it has been argued that CBCT is solely suitable for evaluating calcified structures such as bone or teeth, as CBCT provides images of highly contrasting structures well.2,7,9
Since 2004,19,20 numerous attempts have been made to ascertain CBCT accuracy. The methods routinely applied are (1) the use of geometrical hardware phantoms; (2) the use of anthropomorphic phantoms; or (3) a comparison of a new imaging modality with an extant established imaging modality.21 But validating a new method through comparison lacks a standardized reference, and phantom studies do not render clinical application. Furthermore, the lack of soft tissue in previous studies presents another limitation. Besides failing to reproduce clinical truth appropriately, absence of soft tissue means simply forfeiting the opportunity to measure it. Thus, our study aims to offer a fourth approach: the use of intact cadaveric heads, which may facilitate the depiction of the clinical truth authentically and may enable us to establish a reference value by performing direct soft-tissue measurements.
The aim of this study was (a) to compare the image quality and accuracy of CBCT and MDCT compared with anatomical reference standard measurements, and (b) to compare intraoral soft-tissue measurements with bone measurements upon CBCT data. To overcome the limitations of previous comparative studies, we sought to evaluate similar scan protocols for CBCT and MDCT and optimally approximate a clinical situation using intact cadaveric heads.
Materials and methods
Specimen
The sample consisted of eight unmitigated cadaveric heads (five females, three males; age range 65–95 years; mean age 81 years). Each specimen had a complete canine-to-canine dentition in the mandible. The specimens were obtained from a voluntary body donation programme and were supplied by the Anatomical Institute of the local university in accordance with State and Federal regulations (voluntary body donation programme on the basis of informed consent), the Convention on Human Rights and Medicine22 and the recommendation of the National Academy of Medical Science.23 The perfusion was carried out within 4 days after death with a fixation liquid consisting of 2 parts alcohol (70%), 1 part glycerine and 2% Almudor® (Isspest Control, Dietikon, Switzerland; containing 8.1% formaldehyde, 10% glyoxal and 3.7% glutaraldehyde).
Image acquisition
All MDCT and CBCT examinations were carried out prior to the removal of the gingiva. The MDCT scans were performed on a commercially available 40-detector row CT system (Brilliance CT 40, Philips Healthcare, Eindhoven, Netherlands) with the following scan parameters kept identical for all specimens: tube voltage, 120 kV; tube current–time product, 70 mAs; slice collimation, 20 × 0.625 mm; pitch, 0.68; reconstruction slice thickness, 0.67 mm; reconstruction increment, 0.33 mm; window level setting, 2000/500 HU; voxel size, 0.39 mm (x), 0.39 mm (y) and 0.67 mm (z).
All CBCT scans were performed on a commercially available CBCT scanner with an Amorphous Silicon Flat Panel (KaVo 3D eXam®; KaVo Dental GmbH, Bismarckring, Germany). The following scan parameters were kept identical during all CBCT examinations: tube voltage, 120 kV; tube current–time product, 37.07 mAs; reconstruction thickness, 0.4 mm; reconstruction increment, 0.4 mm; voxel size, 0.4 mm (x), 0.4 mm (y) and 0.4 mm (z).
Anatomical measurements (Figure 1a)
Figure 1.
(a) Measurements taken. IE, incisal edge; GM, gingival margin; ABR, alveolar bone ridge. (b) Representative multidetector CT scan, specimen 949
An electronic digital calliper was used for all anatomical measurements (accuracy 0.01 mm, DIN 862). All clinical measurements were repeated after 2 weeks and the mean values were used for further statistical analysis.
Soft tissue measurement
The distance between the incisal edge (IE) and the gingival margin (GM) of all lower front teeth (canine to canine, n = 48).
Bone measurement
The distance between the incisal edge and the alveolar bone ridge (ABR) of all lower front teeth (after gentle removal of the gingiva; canine to canine, n = 48).
The most apical point of the lunar-shaped devolution of the bone ridge was selected.
Image analysis/radiological measurements
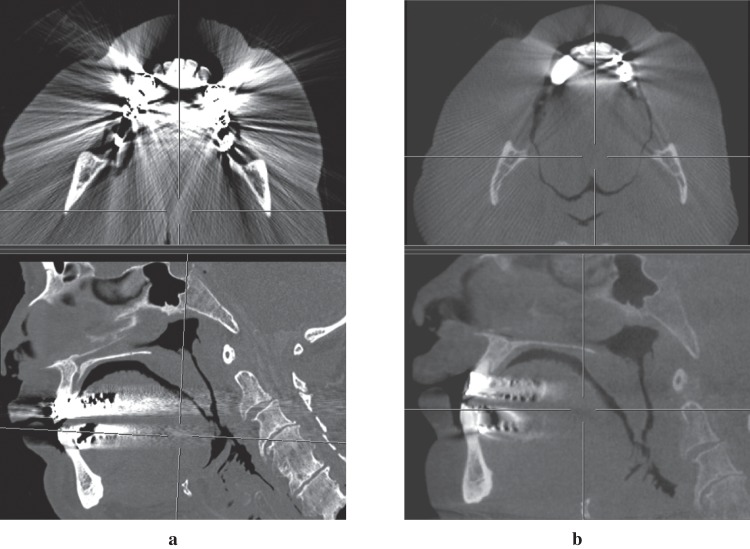
The radiological measurements were performed using a dedicated, commercially available post-processing software tool for digital imaging and communications in medicine (DICOM) data review (Synedra View Personal, v. 1.0.12.1). All images were reconstructed using multiplanar reformatting perpendicular to the curvature of the dentition, making it possible to depict every tooth in its buccolingual profile (Figure 2). MDCT image data were derived from axial-source raw data. All images were magnified on the monitor to the field of interest, and an electronic calliper tool was used to measure the two distances corresponding to the anatomical measurements mentioned above (Figure 1b). The bone measurements (IE–ABR) were evaluated on the CBCT and MDCT scans, and the soft-tissue measurements (IE–GM) only on the CBCT scans. All radiological measurements were taken twice, at least 1 week apart, by the same observer. The monitor used to view the images and measure the distances was set at the highest resolution setting (1680×1050, pixel pitch 0.258 mm).
Figure 2.
Orientation of the multiplanar image reformations perpendicular to the dentition, enabling one to view every assessed tooth in its buccolingual profile
Owing to metal-induced beam hardening artefacts, a total of seven sites were not assessable on MDCT and/or CBCT images. These sites were excluded from further data analyses. From the 41 remaining CBCT data sets, the gingiva could not be distinguished on 10 data sets owing to very tight lip contact, and these sites needed to be excluded from the soft-tissue measurements (IE–GM), and thus only clearly depicted gingiva were assessed (n = 31).
Statistical analysis
Two commercially available software packages (SPSS® v. 17; SPSS Inc., Chicago, IL, and MedCalc v. 11.4.1.0; MedCalc Software, Mariakerke, Belgium) were used for all statistical analyses. To determine intraobserver reliability, the intraclass correlation coefficient (ICC) for absolute agreement based on a one-way random effects analysis of variance was calculated for the radiological measurements. Descriptive statistics for the differences between radiological and anatomical measurements for each category (i.e. MDCT bone measurements, CBCT bone measurements, CBCT soft-tissue measurements) were computed separately. In order to disclose deterministic differences between both methods of measurement, a one-sample Student’s t-test was applied to the differences. Furthermore, the Bland–Altman method24,25 was performed and the limits of agreement were identified. p-values less than 0.05 were considered as statistically significant.
Results
The ICC revealed a very good repeatability of the radiological measurements [r = 0.92; 95% confidence intervals (CI) 0.86 mm; 0.96 mm)]. This high intraobserver reliability is considered a prerequisite for further comparisons of measurements.
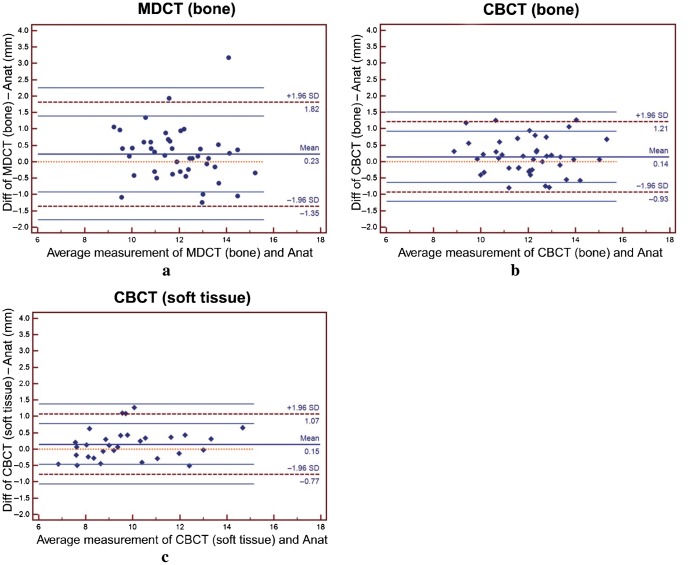
The accuracy of the measurements proved to be acceptable for all protocols (MDCT bone, CBCT bone and soft tissue). The results of the descriptive statistics and the one-sample t-test are given in Table 1. There were more non-assessable sites (NASs) with MDCT (14.5%) than with CBCT (8.3%). The mean difference for all readings was very close to 0 mm, with 0.23 mm for MDCT and 0.14 mm for CBCT (bone and soft tissue, respectively). The one-sample t-test revealed no significant differences between the radiological and clinical measurements, and 0 mm was always within the 95% CI bound. The mean differences between the radiological and anatomical measurements are plotted in Figure 3.
Table 1. Descriptive statistics, one sample t-test, 95% confidence interval (CI) for differences and limits of agreement: positive numbers represent overestimation and negative numbers underestimation of the radiological measurement (Rx) with respect to anatomical measurement (Anat).
| Differences Rx–Anat | n | NASs (%) | p-value | Mean (mm) | SD (mm) | Range (mm) | 95% CI (mm) | Limits of agreement (mm) |
| MDCT bone | 41 | 14.5 | 0.0667 | 0.23 | 0.81 | 4.42 | −0.02; 0.48 | −1.35; 1.82 |
| CBCT bone | 41 | 8.3 | 0.0956 | 0.14 | 0.55 | 2.07 | −0.02; 0.31 | −0.93; 1.21 |
| CBCT soft tissue | 31 | – | 0.0874 | 0.14 | 0.47 | 1.78 | −0.02; 0.32 | −0.77; 1.07 |
CBCT, cone beam CT; MDCT, multidetector CT; NASs, non-assessable sites; SD, standard deviation.
Figure 3.
Box and whisker plot of the differences (Diff) between the radiological (Rx) and anatomical (Anat) measurements. CBCT, cone beam CT; MDCT, multidetector CT
To validate the various measurements, the difference between the measurements was plotted against the mean as recommended by Bland and Altman (Figure 4a–c). The mean value, limits of agreement and the 95% CI for the limits of agreement are marked in the figures. These figures show that, although the mean differences were all close to 0 mm, the limits of agreement for bone measurements were broader in MDCT (−1.35 mm; 1.82 mm) than in CBCT (−0.93 mm; 1.21 mm). These results suggests that MDCT is to some extent less accurate. The limits of agreement for soft-tissue measurements in CBCT, however, were smaller (–0.77 mm; 1.07 mm), indicating a slightly higher accuracy for soft-tissue measurements.
Figure 4.
Bland–Altman plots for (a) multidetector CT (bone), (b) cone beam CT (CBCT) (bone) and (c) CBCT (soft tissue). Mean value (solid thick middle line), limits of agreement (broken lines) and 95% confidence intervals of the limits of agreement (solid thin lines) are shown. Anat, anatomical; Diff, difference; SD, standard deviation
Discussion
Over the last decade, CBCT has gained increased influence in the field of diagnostic maxillofacial imaging, being referred to as the “modality of choice”.26 However, the absolute value of CBCT and its role as a standard of reference remains questionable until it has been carefully and adequately compared with the existing standard of reference, which is MDCT.
Multiple investigations have been conducted to compare CBCT and MDCT using either a dry mandible,27-29 a maxilla,3,30,31 both,32,33 or an anthropomorphic phantom.3,33-36 To the best of our knowledge, only three studies26,36,37 have been published so far using intact human heads to compare the performance of CBCT and MDCT in the dentomaxillofacial area. However, the focus has been laid predominantly on image quality, and not on accuracy of measurements. Hence, in all three studies the obtained measurements were not compared with anatomical measurements. Moreover, it is obvious that measurements taken from images obtained from lower-resolution protocols are prone to giving inferior results.38 However, many previous studies compared high-resolution CBCT protocols with standard MDCT protocols,27-32,35 i.e. comparing voxel sizes of 0.125 × 0.125 × 0.125 mm (CBCT) with voxel sizes of 0.375 × 0.375 × 0.4 mm (MDCT).21 We believe that using scan protocols with a substantial difference in voxel volume [1.95×10−3 mm3 (CBCT) vs. 39.09×10−3 mm3 (MDCT)] renders a comparison inappropriate.
Mindful of the limitations of the above studies, we attempted to perform a comparative study applying a low-resolution CBCT protocol and comparing the obtained measurements with the anatomical truth.
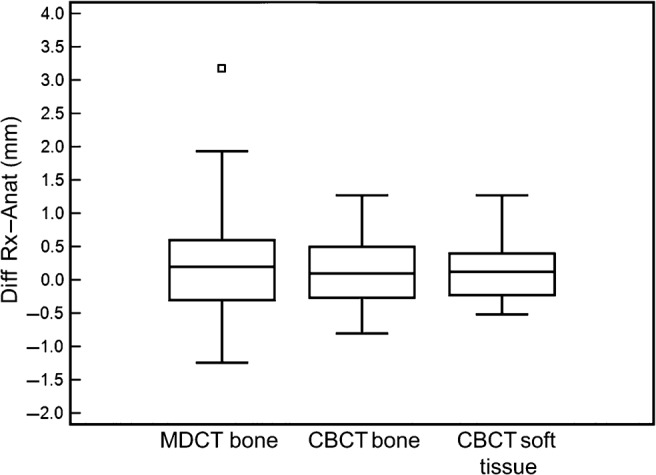
Reduced image quality due to metallic artefacts presents a challenge and serious limitation in dentomaxillofacial imaging.39 Implants, dental reconstructions and orthodontic appliances may cause beam hardening and streaking artefacts, thus decreasing image quality.40 To determine image quality in our study, we have evaluated the number of NASs due to metallic dental reconstructions. The results show that, compared with the CBCT scans, MDCT scans showed more NASs because of the close proximity of the measured area to the metal reconstructions. Moreover, the MDCT data were sometimes compromised in remote areas as well, owing to pronounced streaking or starburst artefacts (Figure 5). By quantifying the NASs (14.5% for MDCT vs 8.3% for CBCT) our study shows a highly relevant finding for clinical practice. However, this is not in accordance with Draenert et al,41 who found stronger beam hardening artefacts in CBCT than in MDCT. A comparison of the two studies is difficult, however, because Draenert et al examined one dental implant (one metal alloy) in a dry skull. The present study, alternatively, aims to approximate clinical practice with greater accuracy using intact cadaveric heads: most of the specimens contained a multitude of metallic reconstructions in various locations. This is important because both variables, composition and orientation of metals, affect the data.38 In general, CBCT produced smoother images with reduced image contrast. Although this hinders the qualitative assessment of tissues, it proved beneficial for the quantitative appraisal of linear measurements.
Figure 5.
Representative scan of the identical specimen (same region and same multiplanar reformatting) with typically constrained data from metal reconstruction. (a) Multidetector CT, (b) cone beam CT. Note the obvious difference in image quality
The broader limits of agreement in MDCT indicate that linear measurements are slightly more accurate when performed upon CBCT rather than MDCT data and confirm the results of previously published studies.19,27,32 Moreover, our data are in accordance with studies reporting a generally better image quality of CBCT for hard-tissue assessments.3,28,31,42
Literature on the accuracy of CBCT-based soft-tissue measurements is scarce. Januário et al43 measured gingival tissue by means of CBCT, and Barriviera et al44 proposed that the palatal masticatory mucosa may be measured on CBCT data. However, both failed to validate their obtained measurements against anatomical reference measurements. In two further studies, Fourie et al45,46 described the accuracy of facial (i.e. extraoral) soft-tissue measurements. However, these results may not be applied to intraoral measurements, because Fourie deemed only mean absolute errors of more than 1.5 mm as clinically significant, which will not hold true for intraoral clinical queries. Furthermore, the CBCT-based measurements were taken from a generated three-dimensional soft-tissue surface model and not from multiplanar reconstructions. Finally, the evaluation of the scanned data on a laptop screen might have been a curtailing factor on the accuracy.
To the best of our knowledge, the present study is the first to describe the accuracy of intraoral soft-tissue measurements on CBCT compared with bone measurements. Interestingly, soft-tissue measurements are slightly more accurate than bone measurements. The reason might simply be because no other tissue is in contact with the gingival surface, making the gingival surface easier to identify.
In clinical practice, ascertaining the thickness of the gingiva or mucosa would be highly advantageous. The success of surgical procedures in periodontology often depends on the thickness of the soft tissue present,47 as well as the thickness of the donor site when grafting connective tissues.48 Furthermore, the width of the free gingival margin is directly related to more frequent and more severe recessions,49 and gingival problems occur generally more often in individuals with a thin gingival biotype.50 Additionally, considerable intra- as well as interindividual variations in thickness of the masticatory mucosa exist.51 As a result, a non-invasive method to assess the thickness of the gingiva has long been sought. Müller et al47 introduced an ultrasonic measuring method, but were forced to admit that it was not reliable enough. More recently, Januário et al43 published an innovative approach to expose the buccal gingiva during the scan by means of a lip retractor (Figure 6). However, their radiological measurements were not verified. The findings of our study validated the accuracy of intraoral soft-tissue measurements and legitimate radiological measures of the gingiva and the masticatory mucosa. Hence, the use of a lip retractor seems highly commendable to expose the buccal gingiva.
Figure 6.
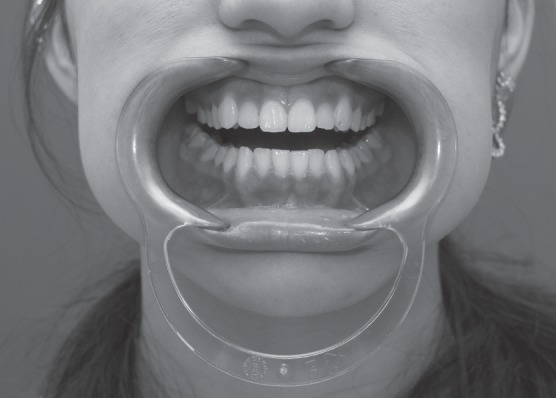
Lip retractor commonly used in orthodontics. This tool might be useful in cone beam CT image acquisition for gingival measurements
Limitations
One limitation is the possible bias of a single observer, probably yielding greater consistency in radiological landmark identification than the varied interpretations of a landmark by several observers. A meta-analysis on identification and reproducibility of radiological (cephalometric) landmarks, however, indicates that the number of observers does not play a significant role in landmark identification,52 and in a more recent study de Oliveira et al53 demonstrated a likewise excellent interobserver reliability in CBCT landmark reproducibility in all three planes of space.
A second constraint may be that unmitigated cadaveric heads render only an approximation of clinical truth. Specifically, the alcohol fixation of the specimens contained low concentrations of glutaraldehyde and formaldehyde, which are known to modify certain tissue properties, e.g. slight muscle expansion and fatty tissue shrinkage,54 and are known to alter periodontal fibre architecture.55 Yet a comparison of soft-tissue and bone measurements must presuppose that fixation does not modify tissue properties. There is evidence supporting glyoxal-based fixation as a suitable fixative for structural evaluation of soft tissue.56 In addition, no significant differences have been reported in bone mineral density and the initial Young’s modulus between alcohol fixation and fresh-frozen specimens.57
Lastly, some concern may be raised as to whether multiple measurements on the same head could be interpreted as independent samples, as this probably violates the assumption of independence required for parametric statistical testing. This problem is discussed in periodontal research58 and is common for all cadaveric studies. In radiology this limitation is possibly less acute than in periodontology (where each site is clearly dependent of the ubiquitous oral habitat and host factors), as the correlation between measurements at different radiological sites is weaker owing to the impact of orientation and distance to metal affecting the imaging.
In conclusion, CBCT image data is inherently different from MDCT image data, generating smoother images with lower image contrast. This serious limitation in regard to qualitative appraisal of soft tissue and bone proved beneficial for the quantitative assessment of linear measurements. Compared with MDCT, CBCT appears to be less susceptible to metal artefacts and slightly more reliable for linear measurements. Therefore, in practice, the clinician’s choice over which CT device to use should depend on the intended diagnostic purpose of each scan to be performed. A further finding is that CBCT accuracy of linear soft-tissue measurements is similar to the accuracy of linear bone measurements. The use of a lip retractor is recommended to enable the exposure of the buccal gingiva.
References
- 1.Robb RA, Sinak LJ, Hoffman EA, Kinsey JH, Harris LD, Ritman EL. Dynamic volume imaging of moving organs. J Med Syst 1982;6:539–554 [DOI] [PubMed] [Google Scholar]
- 2.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 1999;28:245–248 [DOI] [PubMed] [Google Scholar]
- 3.Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S, Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:371–377 [DOI] [PubMed] [Google Scholar]
- 4.Ludlow J, Davies-Ludlow L, Brooks S. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol 2003;32:229–234 [DOI] [PubMed] [Google Scholar]
- 5.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol 2004;33:83–86 [DOI] [PubMed] [Google Scholar]
- 6.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006;35:219–226 [DOI] [PubMed] [Google Scholar]
- 7.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 1998;8:1558–1564 [DOI] [PubMed] [Google Scholar]
- 8.Sukovic P. Cone beam computed tomography in craniofacial imaging. Orthod Craniofac Res 2003;6:31–36 [DOI] [PubMed] [Google Scholar]
- 9.Farman AG, Scarfe WC. The basics of maxillofacial cone beam computed tomography. Semin Orthod 2009;15:2–13 [Google Scholar]
- 10.Silverman PM, Kalender WA, Hazle JD. Common terminology for single and multislice helical CT. AJR Am J Roentgenol 2001;176:1135–1136 [DOI] [PubMed] [Google Scholar]
- 11.Mah P, Reeves TE, McDavid WD. Deriving Hounsfield units using grey levels in cone beam computed tomography. Dentomaxillofac Radiol 2010;39:323–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bryant J. Deriving Hounsfield units from the grey scale of a CBCT? Dentomaxillofac Radiol 2011;40:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryant JA, Drage NA, Richmond S. Study of the scan uniformity from an i-CAT cone beam computed tomography dental imaging system. Dentomaxillofac Radiol 2008;37:365–374 [DOI] [PubMed] [Google Scholar]
- 14.Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, et al. Relationship between density variability and imaging volume size in cone-beam computerized tomographic scanning of the maxillofacial region: an in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:420–425 [DOI] [PubMed] [Google Scholar]
- 15.Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, et al. Effects of image artifacts on gray-value density in limited-volume cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:829–836 [DOI] [PubMed] [Google Scholar]
- 16.van Daatselaar AN, van derStelt PF, Weenen J. Effect of number of projections on image quality of local CT. Dentomaxillofac Radiol 2004;33:361–369 [DOI] [PubMed] [Google Scholar]
- 17.Endo M, Tsunoo T, Nakamori N, Yoshida K. Effect of scattered radiation on image noise in cone beam CT. Med Phys 2001;28:469–474 [DOI] [PubMed] [Google Scholar]
- 18.Araki K, Maki K, Seki K, Sakamaki K, Harata Y, Sakaino R, et al. Characteristics of a newly developed dentomaxillofacial X-ray cone beam CT scanner (CB MercuRayTM): system configuration and physical properties. Dentomaxillofac Radiol 2004;33:51–59 [DOI] [PubMed] [Google Scholar]
- 19.Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants 2004;19:228–231 [PubMed] [Google Scholar]
- 20.Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom). Dentomaxillofac Radiol 2004;33:291–294 [DOI] [PubMed] [Google Scholar]
- 21.Loubele M, Van Assche N, Carpentier K, Maes F, Jacobs R, van Steenberghe D, et al. Comparative localized linear accuracy of small-field cone-beam CT and multislice CT for alveolar bone measurements. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:512–518 [DOI] [PubMed] [Google Scholar]
- 22.European Union. Additional protocol to the convention on human rights and biomedicine, on transplantation of organs and tissues of human origin. ETS 186, Art 16–18; 2002. [PubMed] [Google Scholar]
- 23.Swiss Academy of Medical Science Verwendung von Leichen und Leichenteilen in der medizinischen Forschung sowie Aus-, Weiter- und Fortbildung. Schweiz. Ärzteztg 2009;90:102–107 [Google Scholar]
- 24.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–310 [PubMed] [Google Scholar]
- 25.Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 1995;346:1085–1087 [DOI] [PubMed] [Google Scholar]
- 26.Heiland M, Pohlenz P, Blessmann M, Habermann CR, Oesterhelweg L, Begemann PC, et al. Cervical soft tissue imaging using a mobile CBCT scanner with a flat panel detector in comparison with corresponding CT and MRI data sets. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:814–820 [DOI] [PubMed] [Google Scholar]
- 27.Suomalainen A, Vehmas T, Kortesniemi M, Robinson S, Peltola J. Accuracy of linear measurements using dental cone beam and conventional multislice computed tomography. Dentomaxillofac Radiol 2008;37:10–107 [DOI] [PubMed] [Google Scholar]
- 28.Liang X, Jacobs R, Hassan B, Li L, Pauwels R, Corpas L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT): Part I. On subjective image quality. Eur Radiol 2010;75:265–269 [DOI] [PubMed] [Google Scholar]
- 29.Liang X, Lambrichts I, Sun Y, Denis K, Hassan B, Li L, et al. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT). Part II: On 3D model accuracy. Eur Radiol 2010;75:270–274 [DOI] [PubMed] [Google Scholar]
- 30.Loubele M, Maes F, Schutyser F, Marchal G, Jacobs R, Suetens P. Assessment of bone segmentation quality of cone-beam CT versus multislice spiral CT: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:225–234 [DOI] [PubMed] [Google Scholar]
- 31.Hashimoto K, Kawashima S, Araki M, Iwai K, Sawada K, Akiyama Y. Comparison of image performance between cone-beam computed tomography for dental use and four-row multidetector helical CT. J Oral Sci 2006;48:27–34 [DOI] [PubMed] [Google Scholar]
- 32.Al-Ekrish AA, Ekram M. A comparative study of the accuracy and reliability of multidetector computed tomography and cone beam computed tomography in the assessment of dental implant site dimensions. Dentomaxillofac Radiol 2011;40:67–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mischkowski RA, Pulsfort R, Ritter L, Neugebauer J, Brochhagen HG, Keeve E, et al. Geometric accuracy of a newly developed cone-beam device for maxillofacial imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:551–559 [DOI] [PubMed] [Google Scholar]
- 34.Loubele M, Guerrero ME, Jacobs R, Suetens P, van Steenberghe D. A comparison of jaw dimensional and quality assessments of bone characteristics with cone-beam CT, spiral tomography, and multi-slice spiral CT. Int J Oral Maxillofac Implants 2007;22:446–454 [PubMed] [Google Scholar]
- 35.Suomalainen A, Kiljunen T, Kaser Y, Peltola J, Kortesniemi M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac Radiol 2009;38:367–378 [DOI] [PubMed] [Google Scholar]
- 36.Carrafiello G, Dizonno M, Colli V, Strocchi S, Pozzi Taubert S, Leonardi A, et al. Comparative study of jaws with multislice computed tomography and cone-beam computed tomography. Radiol Med 2010;115:600–611 [DOI] [PubMed] [Google Scholar]
- 37.Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e25–31 [DOI] [PubMed] [Google Scholar]
- 38.Lee M-J, Kim S, Lee S-A, Song H-T, Huh Y-M, Kim D-H, et al. Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multi-detector CT1. Radiographics 2007;27:791–803 [DOI] [PubMed] [Google Scholar]
- 39.Abrahams JJ. Dental CT imaging: a look at the jaw. Radiology 2001;219:334–345 [DOI] [PubMed] [Google Scholar]
- 40.Naranjo V, Llorens R, Alcaniz M, Lopez-Mir F. Metal artifact reduction in dental CT images using polar mathematical morphology. Comput Methods Programs Biomed 2011;102:64–74 [DOI] [PubMed] [Google Scholar]
- 41.Draenert FG, Coppenrath E, Herzog P, Muller S, Mueller-Lisse UG. Beam hardening artefacts occur in dental implant scans with the NewTom cone beam CT but not with the dental 4-row multidetector CT. Dentomaxillofac Radiol 2007;36:198–203 [DOI] [PubMed] [Google Scholar]
- 42.Honda K, Larheim TA, Maruhashi K, Matsumoto K, Iwai K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofac Radiol 2006;35:152–157 [DOI] [PubMed] [Google Scholar]
- 43.Januário AL, Barriviera M, Duarte WR. Soft tissue cone-beam computed tomography: a novel method for the measurement of gingival tissue and the dimensions of the dentogingival unit. J Esthet Restor Dent 2008;20:366–373; discussion 74 [DOI] [PubMed] [Google Scholar]
- 44.Barriviera M, Duarte WR, Januario AL, Faber J, Bezerra AC. A new method to assess and measure palatal masticatory mucosa by cone-beam computerized tomography. J Clin Periodontol 2009;36:564–568 [DOI] [PubMed] [Google Scholar]
- 45.Fourie Z, Damstra J, Gerrits PO, Ren Y. Accuracy and repeatability of anthropometric facial measurements using cone beam computed tomography. Cleft Palate Craniofac J 2011;48:623–630 [DOI] [PubMed] [Google Scholar]
- 46.Fourie Z, Damstra J, Gerrits PO, Ren Y. Accuracy and reliability of facial soft tissue depth measurements using cone beam computer tomography. Forensic Sci Int 2010;199:9–14 [DOI] [PubMed] [Google Scholar]
- 47.Müller H-P, Schaller N, Eger T. Ultrasonic determination of thickness of masticatory mucosa: A methodologic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:248–253 [DOI] [PubMed] [Google Scholar]
- 48.Studer SP, Allen EP, Rees TC, Kouba A. The thickness of masticatory mucosa in the human hard palate and tuberosity as potential donor sites for ridge augmentation procedures. J Periodontol 1997;68:145–151 [DOI] [PubMed] [Google Scholar]
- 49.Yared KFG, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop 2006;130:6.e1–6.e8 [DOI] [PubMed] [Google Scholar]
- 50.Seibert J, Lindhe J. Esthetics in periodontal therapy. 3rd edn. Copenhagen: Munksgaard; 1997. pp 647–681 [Google Scholar]
- 51.Muller HP, Schaller N, Eger T, Heinecke A. Thickness of masticatory mucosa. J Clin Periodontol 2000;27:431–436 [DOI] [PubMed] [Google Scholar]
- 52.Trpkova B, Major P, Prasad N, Nebbe B. Cephalometric landmarks identification and reproducibility: a meta analysis. Am J Orthod Dentofacial Orthop 1997;112:165–170 [DOI] [PubMed] [Google Scholar]
- 53.de Oliveira AEF, Cevidanes LHS, Phillips C, Motta A, Burke B, Tyndall D. Observer reliability of three-dimensional cephalometric landmark identification on cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:256–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Docquier PL, Paul L, Cartiaux O, Lecouvet F, Dufrane D, Delloye C, et al. Formalin fixation could interfere with the clinical assessment of the tumor-free margin in tumor surgery: magnetic resonance imaging-based study. Oncology 2010;78:115–124 [DOI] [PubMed] [Google Scholar]
- 55.Burn-Murdoch RA, Tyler DW. Physiological evidence that periodontal collagen in the rat exists as fibres prior to histological fixation. Arch Oral Biol 1981;26:995–999 [DOI] [PubMed] [Google Scholar]
- 56.Wang Y, Lee K, Pai S, Ledoux W. Histomorphometric comparison after fixation with formaldehyde or glyoxal. Biotech Histochem 2011;86:359–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stefan U, Michael B, Werner S. Effects of three different preservation methods on the mechanical properties of human and bovine cortical bone. Bone 2010;47:1048–1053 [DOI] [PubMed] [Google Scholar]
- 58.Imrey PB. Considerations in the statistical analysis of clinical trials in periodontitis. J Clin Periodontol 1986;13:517–532 [DOI] [PubMed] [Google Scholar]