Why is the topic of pediatric trauma centers (PTCs) important? The simple answer is that injuries are still the leading cause of death in children in the United States. Unintentional injuries kill more than 12,000 children and young adults between the ages of 1 and 19 years in the U.S. every year.
Injuries are the principal cause of death for children in all nations in the Organization for Economic Cooperation and Development (OECD), the 26 wealthiest nations in the world. Injuries constitute almost 30% of the total burden of childhood disease in the OECD by disability-adjusted life years. For every 100,000 children, the pediatric-injury death rate in the United States is more than twice that of Sweden, Great Britain, or Italy. For every death, there are 160 hospital admissions and 2,000 emergency department visits.
The Concept and History of Trauma Centers
The concept of trauma centers and trauma systems began in 1966 with the publication of a U.S. government report, “Accidental Death and Disability: The Neglected Disease of Modern Society,” prepared by the Committees on Trauma and Shock, Division of Medical Sciences, National Academy of Sciences, National Research Council.1 It described “current practices and deficiencies at various levels of emergency care.” In this report, it was recognized that soldiers who were shot in the jungles of southeastern Asia had a better chance of surviving than did citizens who were shot on the streets of the U.S.
The report, which has shaped the development of trauma systems ever since it was published, recommended the day-to-day use of voice communication facilities by the agencies serving emergency medical needs, a single nationwide telephone number through which to summon an ambulance, surveys and pilot programs to establish the numbers and types of emergency departments for the optimal care of surgical and medical casualties, trauma registries in selected hospitals, and subsequent consideration of a national computerized central registry.
The first English-language journal publication that clearly described the key qualities of a trauma center was written by Walter Pizzi in 1968.2 This was the first mention of the term “trauma center” in the medical literature. Pizzi stressed the importance of 2-way radio communication with skilled ambulance crews, resuscitation of the patient in the field and en route to the hospital, proper design and equipment in the emergency department, the immediate response of the general surgeon to the emergency room, a team approach captained by a surgeon, and a systematic method of patient care—dealing with the airway, breathing, circulation, and splinting of fractures, and including head-to-toe examination, diagnostic imaging, and definitive treatment.
The Committee on Trauma of the American College of Surgeons (ACS) first published its categorization criteria for trauma centers in 1976, in the monograph “Resources for Optimal Care of the Injured Patient.” This document has been updated regularly. The 1976 version included the first checklist of specific criteria for the categorization of hospitals as trauma centers. It and its subsequent revisions have defined trauma centers in America, the resources that they require, and the standards that they should meet.
The essential feature of a trauma center is its ability to provide immediate definitive care to the most severely injured patients. Commitment is most important. Prompt, definitive care must be provided at all times, and the surgeon must be in the emergency department when the critically injured patient arrives. Regular critical evaluation of all aspects of trauma-patient care is required. The creation and dissemination of new knowledge is an essential function of Level I trauma centers.
The Emergence of Pediatric Trauma Centers
The first PTCs appeared soon after adult centers, in the 1970s and 1980s. A PTC must meet all the essential criteria of an adult center, and it must also have the following:
A pediatric trauma service directed by a pediatric surgeon
Trauma surgeons credentialed for pediatric trauma care
Pediatric specialists in general surgery, emergency medicine, orthopedics, neurosurgery, physical medicine & rehabilitation, anesthesia, and critical care
A separate pediatric emergency room and intensive care unit
Pediatric resuscitation equipment in all patient-care areas
Pediatric-specific quality assurance and performance improvement
Today, trauma centers and integrated trauma systems are in place in many areas of the United States; however, there are still too few PTCs to manage all major pediatric trauma cases. In the U.S., there are only 35 Level I and 32 Level II PTCs verified by the ACS. Additional PTCs in some states (Florida, New York, and Pennsylvania, for example) do not use the ACS verification process.
Cross-fertilization of ideas and practices has occurred between the adult and pediatric trauma communities, but the flow has been almost entirely in one direction—from the adult centers to the pediatric. One exception is the profound change in the management of blunt abdominal-organ trauma. Nonoperative management (NOM), first described in children, has become the standard of care in all age groups. The first published report of NOM of splenic injuries on the basis of clinical diagnosis alone appeared in 1968.3 The first publication on NOM of splenic trauma in which the diagnosis was confirmed objectively appeared in 1981.4 In a consecutive series of children with proven splenic injury, 70% were treated by means of NOM. There was no case of delayed rupture. Most of the patients were given no blood, and none died. Nonoperative management met with stiff initial resistance from adult-trauma surgeons; however, after many years, the concept has been accepted in all age groups.
Current Status and Future Needs
What is the current status of PTCs? All available data show that the care of injured children is excellent across North America, given geographic limitations and our inability to treat the most severe closed-head injuries. The focus is now on studying trauma as a disease in accordance with principles of epidemiology and public health, emphasizing the primary and secondary prevention of injuries, and educating the general public and decision-makers about the magnitude of the problem of pediatric trauma.
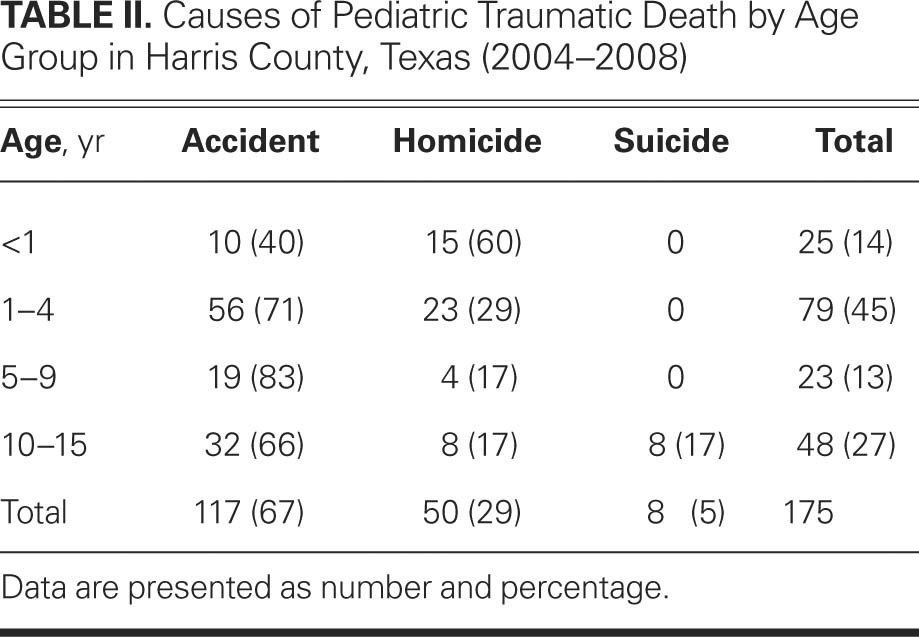
Every Level I trauma center should study its own local referral area and identify issues of need. This starts simply by reviewing (for example) the epidemiology of injury patterns and causes of fatal injury. To cite two such findings, only 13% of all pediatric injury deaths in Harris County, Texas, could have been prevented by better treatment (Table I), and approximately one third were related to homicide or suicide (Table II). To reduce childhood-injury mortality rates, we must find better ways to prevent life-threatening injuries from occurring in the first place. This is especially true in circumstances of child abuse.
Table I. Characteristics of Pediatric Traumatic Deaths in Harris County, Texas (2004–2008)
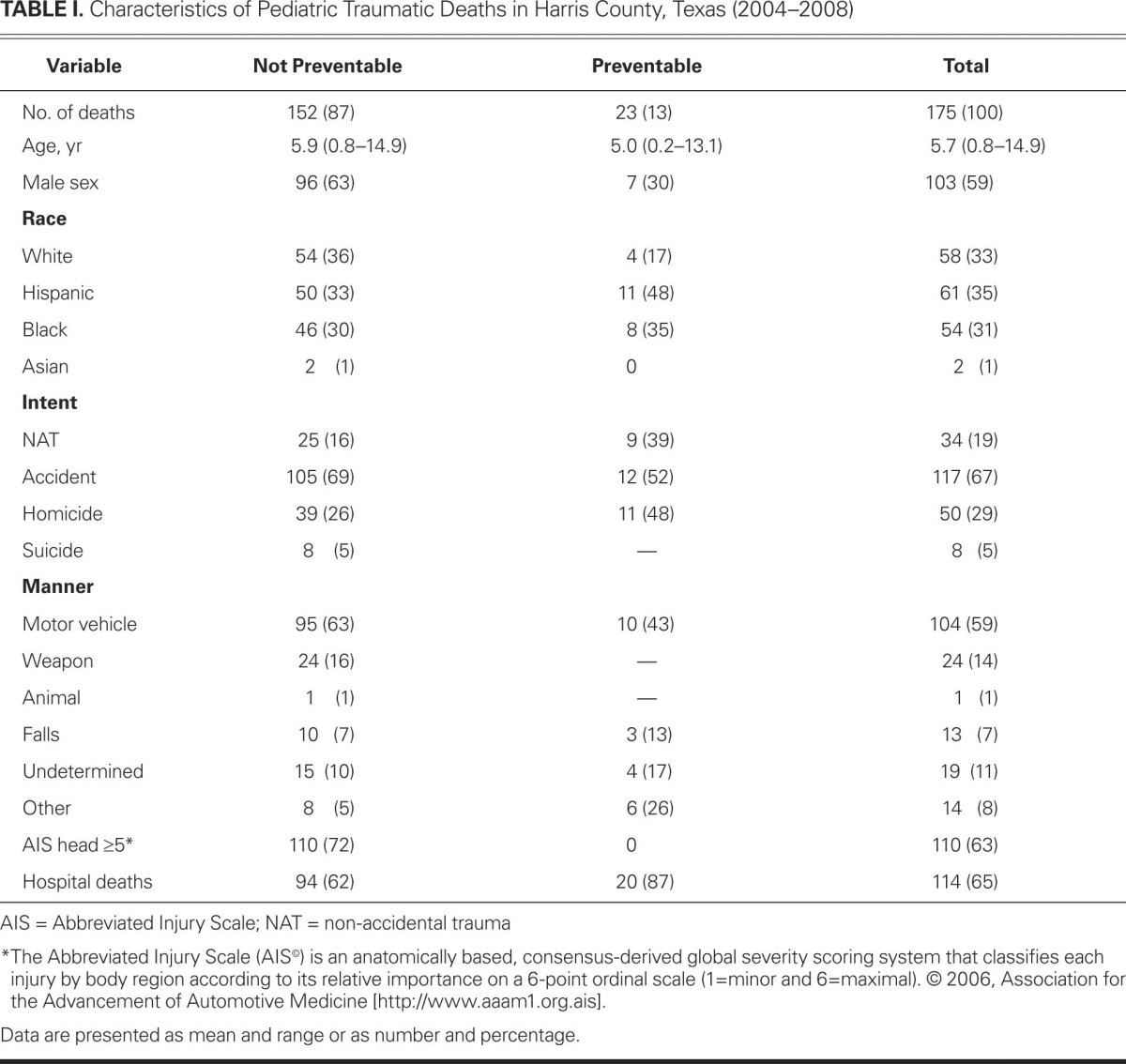
Table II. Causes of Pediatric Traumatic Death by Age Group in Harris County, Texas (2004–2008)
Although great improvements have occurred since 1966, there is still no complete, comprehensive national system of trauma care in the United States. There are major gaps in coverage, especially in rural areas. More PTCs are needed. Each community, region, and state should conduct a needs assessment of trauma care and use it as the basis to develop a trauma-care system.
In summary, PTCs have greatly helped to reduce morbidity and death in childhood injury. Every day, thousands of children are treated successfully in trauma centers across the United States. Trauma centers play an important role in education, research, and injury prevention. Nonetheless, until we are able to reduce our pediatric-injury death rates at least to the level of other developed nations, our work is not finished.
Footnotes
Address for reprints: David E. Wesson, MD, Chief of Pediatric Surgery, Baylor College of Medicine, 1709 Dryden Rd., Suite 1500, Houston, TX 77030
★ CME Credit
Presented at the Joint Session of the Michael E. DeBakey International Surgical Society and the Denton A. Cooley Cardiovascular Surgical Society; Austin, Texas, 21–24 June 2012.
E-mail: davidw@bcm.edu
References
- 1.Committee on Trauma and Committee on Shock, Division of Medical Sciences, National Academy of Sciences, National Research Council. Accidental death and disability: the neglected disease of modern society. Washington (DC): The National Academies Press; 1966. [PubMed]
- 2.Pizzi WF. The management of multiple injury patients. J Trauma 1968;8(1):91–103. [DOI] [PubMed]
- 3.Upadhyaya P, Simpson JS. Splenic trauma in children. Surg Gynecol Obstet 1968;126(4): 781–90. [PubMed]
- 4.Wesson DE, Filler RM, Ein SH, Shandling B, Simpson JS, Stephens CA. Ruptured spleen–when to operate? J Pediatr Surg 1981;16(3):324–6. [DOI] [PubMed]


