Abstract
A 49-year-old woman who had idiopathic thrombocytopenic purpura was admitted to our hospital with severe chest pain. Electrocardiography revealed inferolateral myocardial infarction. The patient underwent immediate coronary angiography, which revealed thrombi in the left coronary system. Percutaneous intervention was not indicated, because the thrombi had occluded the distal segments of multiple coronary arteries. Administration of tirofiban satisfactorily dissolved the thrombi.
Key words: Coronary thrombosis, multivessel; myocardial infarction; platelet aggregation inhibitors/therapeutic use; purpura, thrombocytopenic, idiopathic/therapy; tirofiban
WEBSITE FEATURE
Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disorder in which autoantibodies bind platelets, leading to their sequestration by the reticuloendothelial system.1 Patients with ITP typically have mucocutaneous bleeding. Although such reports are rare, thrombotic complications such as acute myocardial infarction (MI) and stroke also occur in patients with ITP.2–4 We present the case of a middle-aged woman with ITP who sustained an acute MI caused by multivessel coronary thrombosis.
Case Report
In January 2011, a 49-year-old woman was admitted to our hospital with severe chest pain. Her initial physical examination was normal. Her medical history included chronic ITP, which had been diagnosed 20 years earlier, and a splenectomy, which she had undergone in June 2003. At the current admission, electrocardiography showed ST-segment elevation in leads II, III, aVF, and V4 through V6, and ST-segment depression in leads I and AVL (Fig. 1). Bedside echocardiography revealed an ejection fraction of 0.45 and hypokinesia of the apicoanterior and inferolateral walls. Blood tests revealed normal levels of creatine kinase (CK) (41 IU/L) and CK-MB fraction (32 IU/L) upon admission to the emergency service. However, after 12 hours, these levels rose to a maximum of 2,835 IU/L and 363 IU/L, respectively, and remained elevated for 48 hours before decreasing. The peripheral blood platelet count was 54 ×109/L. Her coagulation factor levels (protein C, protein S, and homocysteine) were within normal ranges, and factor V Leiden mutation was not present.
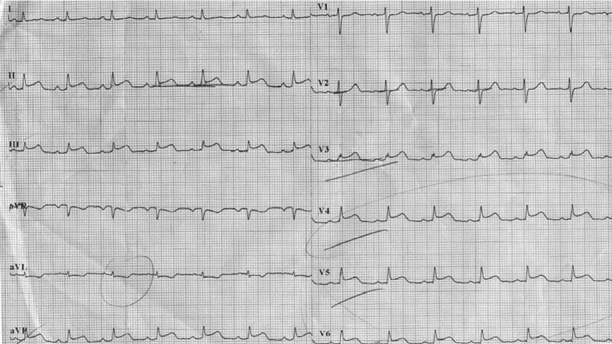
Fig. 1 Electrocardiogram shows ST-segment elevation in leads II, III, aVF, and V4 through V6 on admission.
The patient was diagnosed with acute inferolateral MI, and she was given 300 mg aspirin, 600 mg clopidogrel, an intravenous nitrate infusion, and a bolus injection of 5,000 IU unfractionated heparin. Coronary angiography revealed thrombosis that was causing total occlusion in distal segments of the left anterior descending and left circumflex coronary arteries, the first diagonal branch, and the first obtuse marginal branch (OM1) (Fig. 2). We proceeded with intracoronary administration of tirofiban (the only glycoprotein IIb/IIIa [GPIIb/IIIa] antagonist available to us at the time), at a rate of 10 µg/kg/min for 2 to 3 minutes, through a guiding catheter. Then intravenous tirofiban infusion was initiated at a rate of 0.15 µg/kg/min. Five minutes after the intracoronary administration was completed, we observed a Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow in the distal segment of the left circumflex coronary artery (Fig. 3). The patient was transferred to the intensive care unit, where the intravenous tirofiban infusion was maintained for 36 hours.

Fig. 2 Coronary angiogram shows thrombi causing total occlusion in the distal segments of the coronary arteries (left anterior descending and left circumflex coronary arteries and the first diagonal and obtuse marginal branches).
Real-time motion image is available at www.texasheart.org/journal.
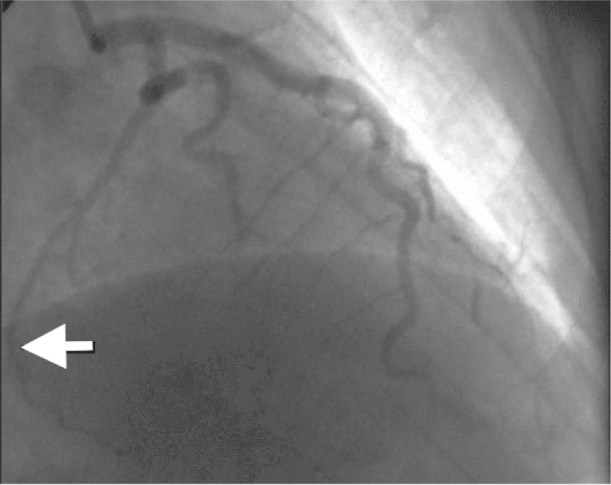
Fig. 3 Coronary angiogram reveals that the coronary thrombus in the left circumflex coronary artery was completely dissolved 5 minutes after intracoronary tirofiban administration.
Real-time motion image is available at www.texasheart.org/journal.
Elective angiography performed 72 hours after the patient's MI confirmed that the thrombi were dissolved in all arteries except the OM1 (Fig. 4). No flow was seen in the distal segment of the OM1; however, percutaneous coronary intervention (PCI) was not indicated, because the lesion was in the distal segment of the artery. The patient's chest pain had resolved, and echocardiography showed a marked improvement in left ventricular systolic function, with an ejection fraction of 0.58 and normalized regional wall motion in previously asynergic segments. Her platelet count was within the normal range. A small hematoma developed at the vessel puncture site, but it resolved before the patient was discharged. On the 5th day, the patient left the hospital, on a regimen of aspirin and clopidogrel.
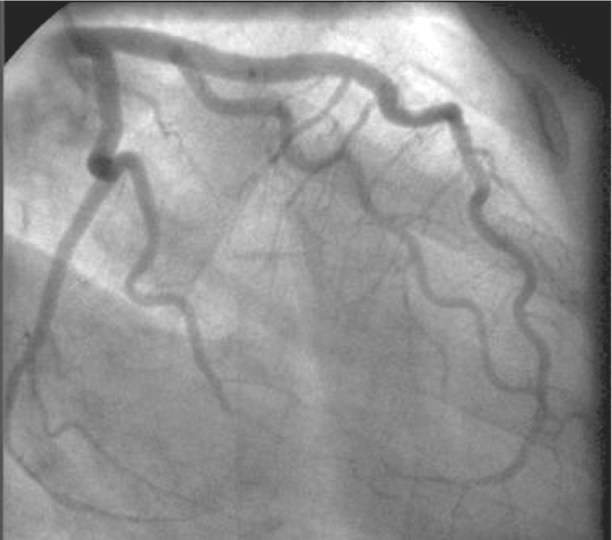
Fig. 4 Coronary angiogram after tirofiban infusion shows that the coronary thrombi in the left anterior descending coronary artery and first diagonal branch were completely dissolved.
Real-time motion image is available at www.texasheart.org/journal.
Discussion
Idiopathic thrombocytopenic purpura is the most common autoimmune blood disorder. In patients with ITP, thrombocytopenia appears to result from increased destruction of platelets by immunologic mechanisms, and bleeding is common.1,2 However, ITP has also been associated with thrombotic complications. The precise mechanism of arterial thrombosis in patients with ITP is unknown, but several possibilities have been identified. First, thrombosis may result from ITP itself: autoantibodies that are present on both platelet and coronary endothelial cells may cause endothelial damage because of the antigenic similarity between platelets and endothelial cells.2 Second, therapy for ITP with intravenous immunoglobulin or steroids can cause some degree of thrombosis.5 Third, thrombosis can occur if ITP is associated with hypercoagulative states such as antiphospholipid antibody syndrome.6
The optimal treatment for patients with ITP who have acute MI with ST-segment elevation is not clear. Generally, ITP increases the risk of bleeding and is, therefore, an obvious contraindication to antiplatelet therapy. Few articles have discussed the management of such patients; however, when PCI has been performed in patients with chronic ITP, concurrent administration of aspirin, clopidogrel, and unfractionated heparin has been successful, with no major bleeding complications reported.3,7 Yildiz and colleagues7 administered antiplatelet therapy in combination with PCI in a young woman who had ITP and acute MI, also without major bleeding complications. However, only 2 case reports have documented the administration of GPIIb/IIIa inhibitors in patients with ITP.8,9 Mendez and associates8 reported the case of a 70-year-old man with ITP who had a normal platelet count (170 ×109/L) and underwent PCI. The patient developed severe thrombocytopenia after abciximab administration. Those authors suggested that a history of ITP should be regarded as a contraindication to abciximab administration, even in patients with normal platelet counts. Stouffer and co-authors9 reported the case of a man with ITP who had a non-Q-wave MI caused by stent restenosis. The platelet count was 78 ×109/L. Eptifibatide was given for 18 hours, with no major bleeding noted on follow-up.
The GPIIb/IIIa receptor antagonists prevent platelet aggregation and thrombus formation, improving the outcomes of patients with acute coronary syndrome. In clinical trials, intracoronary and intravenous administration of GPIIb/IIIa antagonists were compared in patients with acute myocardial syndrome. Intracoronary administration was associated with better myocardial reperfusion when evaluated by myocardial blush grade10 and TIMI frame count.11 Intracoronary administration of GPIIb/IIIa antagonists would be expected to increase the drug's concentration at the site of coronary thrombosis, which might, in turn, increase the binding of the drug molecules to both platelets and endothelial receptors, and increase bleeding. However, it is thought that existing autoantibodies bind to the GPIIb/IIIa receptors after they have undergone drug-induced structural changes, eventually causing thrombocytopenia.12 Therefore, treatment with these agents could lead to bleeding complications and thrombocytopenia.
Our patient had no risk factors for coronary artery disease. Her coagulation factor levels (protein C, protein S, and homocysteine) were within normal ranges, and no factor V Leiden mutation was present. After intracoronary administration of tirofiban, the thrombus in the left circumflex coronary artery was completely dissolved, and after intravenous tirofiban infusion, the thrombi in most of the other coronary arteries dissolved, without any complications.
To our knowledge, this is the first reported case of multivessel coronary thrombi in a patient with ITP. Because intracoronary and intravenous tirofiban dissolved our patient's coronary thrombi without bleeding complications, we believe that intracoronary and intravenous tirofiban infusion should be considered in those patients with no evidence of high bleeding risk. Nevertheless, the risks and benefits for each patient must be considered carefully to determine individualized treatment.
Supplementary Material
Footnotes
Address for reprints: Julide Yagmur, MD, Kardiyoloji Anabilim Dali, Inonu Universitesi Tip Fakultesi, Turgut Ozal Tip Merkezi Arastirma ve Uygulama Hastanesi, 44100 Malatya, Turkey
E-mail: julideyagmur@hotmail.com
References
- 1.Cines DB, Blanchette VS. Immune thrombocytopenic purpura. N Engl J Med 2002;346(13):995–1008. [DOI] [PubMed]
- 2.Fruchter O, Blich M, Jacob G. Fatal acute myocardial infarction during severe thrombocytopenia in a patient with idiopathic thrombocytopenic purpura. Am J Med Sci 2002;323 (5):279–80. [DOI] [PubMed]
- 3.Gracia MC, Cebollero IC, Lezcano JS, Osuna GG, Miguel JA, Peralta LP. Invasive treatment performed for acute myocardial infarction in a patient with immune thrombocytopenic purpura. Int J Cardiol 2008;127(3):e183–5. [DOI] [PubMed]
- 4.Rhee HY, Choi HY, Kim SB, Shin WC. Recurrent ischemic stroke in a patient with idiopathic thrombocytopenic purpura. J Thromb Thrombolysis 2010;30(2):229–32. [DOI] [PubMed]
- 5.Paolini R, Fabris F, Cella G. Acute myocardial infarction during treatment with intravenous immunoglobulin for idiopathic thrombocytopenic purpura (ITP). Am J Hematol 2000; 65(2):177–8. [DOI] [PubMed]
- 6.Moreno-Ruiz LA, Mendoza-Perez BC, Santillano-Gomez E, Jimenez-Arteaga S, Borrayo-Sanchez G, Alva-Espinosa C. Non-ST-elevation acute myocardial infarction secondary to antiphospholipid antibody syndrome in an adolescent female [in English, Spanish]. Cir Cir 2010;78(5):435–8. [PubMed]
- 7.Yildiz A, Coskun U, Batukan OE, Keskin K. Primary percutaneous coronary intervention for acute myocardial infarction in a young female with idiopathic thrombocytopenic purpura: a case report and review. Case Report Med 2010;2010: 854682. [DOI] [PMC free article] [PubMed]
- 8.Mendez TC, Diaz O, Enriquez L, Baz JA, Fernandez F, Goicolea J. Severe thrombocytopenia refractory to platelet transfusions, secondary to abciximab readministration, in a patient previously diagnosed with idiopathic thrombocytopenic purpura. A possible etiopathogenic link [in Spanish]. Rev Esp Cardiol 2004;57(8):789–91. [PubMed]
- 9.Stouffer GA, Hirmerova J, Moll S, Rubery B, Napoli M, Ohman EM, Simpson R. Percutaneous coronary intervention in a patient with immune thrombocytopenia purpura. Catheter Cardiovasc Interv 2004;61(3):364–7. [DOI] [PubMed]
- 10.Gu YL, Kampinga MA, Wieringa WG, Fokkema ML, Nijsten MW, Hillege HL, et al. Intracoronary versus intravenous administration of abciximab in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention with thrombus aspiration: the comparison of intracoronary versus intravenous abciximab administration during emergency reperfusion of ST-segment elevation myocardial infarction (CICERO) trial. Circulation 2010;122(25):2709–17. [DOI] [PubMed]
- 11.Deibele AJ, Jennings LK, Tcheng JE, Neva C, Earhart AD, Gibson CM. Intracoronary eptifibatide bolus administration during percutaneous coronary revascularization for acute coronary syndromes with evaluation of platelet glycoprotein IIb/IIIa receptor occupancy and platelet function: the Intracoronary Eptifibatide (ICE) Trial. Circulation 2010;121(6):784–91. [DOI] [PubMed]
- 12.Abrams CS, Cines DB. Thrombocytopenia after treatment with platelet glycoprotein IIb/IIIa inhibitors. Curr Hematol Rep 2004;3(2):143–7. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


