Abstract
Purpose
The purpose of this study was to describe the use of operating room (OR) time for pediatric dental procedures performed under general anesthesia (GA) at a regional children’s hospital over a 2-year period.
Methods
A cross-sectional review of a pediatric dental GA records was performed at Seattle Children’s Hospital. Data were collected for 709 0- to 21-year-old patients from January 2008 to December 2009. Demographic data, dental and anesthesia operator types, and procedures were recorded. Utilization of OR time was analyzed.
Results
The mean age of patients was 7.1 years (±4.2 SD), and 58% were male. Distribution by American Society of Anesthesiology (ASA) classifications were: ASA I 226 (32%); ASA II 316 (45%); ASA III 167 (24%). Cases finished earlier than the scheduled time by an average of 14 minutes (±28). Overrun time was significantly associated with: patient age (P=.01); ASA classification (P=.006); treatment type (P<.001); number of teeth treated (P<.001); and dentist operator type (P=.005).
Conclusions
Overall, 73% of dental procedures under GA finished early or on time. Significant variables included patient age, medical status, treatment type and extent, and dentist operator type. Assessing factors that impact the time needed in GA may enhance efficiency for pediatric dental procedures.
Keywords: PEDIATRIC DENTISTRY, AMBULATORY SURGICAL PROCEDURES, GENERAL ANESTHESIA, DENTAL CARE FOR DISABLED, TIME FACTORS
Pediatric dental treatment and general anesthesia
Comprehensive dental rehabilitation under general anesthesia is a treatment modality for many pediatric dentists. General anesthesia (GA) is utilized for pediatric dental patients to provide comprehensive and high quality dental care when conventional dental treatment is not an option. Routine dental procedures for children are performed under GA for various reasons, including for patients: of a very young age; with complex medical/physical/mental conditions; with a need for extensive treatment; with a need for oral surgery treatment; with a need for emergency treatment that is extensive; who require safety considerations; who have language barriers preventing communication; who travel long distances to receive specialty care.1,2
The American Academy of Pediatric Dentistry (AAPD) endorses GA for pediatric dental patients who: are unable to cooperate; experience ineffective local anesthesia; are extremely fearful, anxious, or uncommunicative; require significant surgical procedures; can benefit from GA protecting them from psychological trauma and/or reducing medical risks; and require immediate, comprehensive oral care.1,3 Furthermore, many medical conditions present with oral disease that must be managed in an inpatient setting, and the operating room (OR) is often the best place to provide such care. Pediatric dentists are trained to recognize the need for hospital-based dental treatment and to work with an anesthesia team to provide optimal care for their patients.4 The AAPD definition of medically necessary care includes services of GA and use of surgery facilities.5
ASA classification and risk
The American Society of Anesthesiology (ASA) classifies patients according to their physical status as follows: (I) a normal healthy patient; (II) a patient with mild systemic disease; (III) a patient with severe systemic disease; (IV) a patient with severe systemic disease that is a constant threat to life; (V) a moribund patient who is not expected to survive without the operation; and (VI) a patient declared brain-dead whose organs are being removed for donor purposes.6 Patients at higher medical risk during sedation are often more safely treated in the OR.
Pediatric dentistry patients with an ASA classification of I or II are often treated on an outpatient basis with mild to moderate sedation, although GA is an appropriate treatment modality when treatment needs are extensive and cooperation is poor. Patients with an ASA classification of III or higher are usually not suitable candidates for moderate sedation and are more safely treated under GA supervised by a licensed, trained, and credentialed medical and dental team in an appropriately equipped facility.1,4
Attitudes toward GA
Despite the risk of adverse events inherent in GA, dental treatment performed in a hospital OR is generally considered safe.7 Pediatric dentists report a favorable attitude toward dental treatment under GA for pediatric patients, and many report an increasing interest in utilizing this modality more frequently in their practices.8
Parental attitudes toward behavior management techniques have changed over time.9–11 Previous studies report that parents were less accepting of GA as a treatment method for children receiving dental care. In 1984, Murphy et al., investigated parental attitudes toward behavior management techniques and found the greatest acceptance of “tell-show-do” and the least acceptance of GA and use of the Papoose Board.10 In 2005, Eaton et al., surveyed parents after showing a video of behavior management techniques, and found that the most accepted techniques, in decreasing order, were: (1) tell-show-do; (2) nitrous oxide sedation; (3) GA; (4) active restraint; (5) oral premedication; (6) voice control; (7) passive restraint; and (8) hand over mouth.11 This study notes a trend toward increasing acceptability of GA from 1984 to 2004. After children with extensive dental disease are treated under GA, the quality of life improvements and overall satisfaction with the treatment experience have been reported favorably.12 Parents of children who received dental care under GA to treat early childhood caries have reported satisfaction with treatment experience and perception of improved quality of life and improved health status for their children, mainly regarding improvements in pain levels, eating, sleeping, and behavior.12,13
Comprehensive dental care under GA is often more efficient and cost effective than repeated dental visits for restorative care utilizing other sedation methods.14 Dental restorations performed under GA, especially for treatment of early childhood caries, are reported to have greater quality and durability than restorations placed under conscious sedation.15,16 There is also some evidence that children who receive dental treatment under GA before 36 months old exhibit more positive behavior at future dental visits.17
Operating room utilization
Problems inherent to dental treatment in a hospital setting include: long waiting lists for treatment in the OR; difficulty scheduling dental patients vs patients with other medical needs; risk of cancellations due to staffing shortages or patient failures; poor utilization of OR time; and inefficient OR scheduling.4,18–20 The average waiting time for complex dental care in the OR with GA in US pediatric dentistry programs has been reported as an average of 28 days for children experiencing pain and 71 days for children without pain.21
Furthermore, treatment in a hospital OR is costly for both families and the health care system. Costs associated with this type of treatment have been studied by numerous investigators.2,12,18–20,22 In addition to the medical and dental costs directly associated with treatment, there are other associated costs involved in OR treatment (eg, lost wages, children missing school).23 For hospitals, the ORs assume a large portion of resources, including capital, medical equipment, pharmacologic agents, and staff.
Previous reports estimate that ORs function during 70% of a regular working week and that 70% of available OR time is actually utilized.18 An optimal amount of utilization of 85% has been proposed.24 The classic definition of OR utilization is “the sum of the time it takes to perform each surgical procedure (including preparation of the patient in the OR, anesthesia induction, and emergence) plus the total turnover time, divided by the time available.” If cases extend beyond the scheduled time, the overtime may be counted as utilization, despite the increased staffing costs.23 Strum et al., define “overutilization” as the time used by scheduled cases beyond the scheduled time and “underutilization” as the time during scheduled operating hours that is not used for patient care.25 Difficulties in OR scheduling include inability to accurately predict case duration and variability of case time. Increasing variability causes a decrease in predictable optimum utilization. Overutilization incurs overtime costs and creates problems with staff morale and retention.24
Improvements in OR utilization for pediatric dental procedures may be identified to increase efficiency. This is desirable for several reasons, including: improved hospital resource allocation; an increased number of patients able to receive treatment; and a reduction of waiting time to receive dental rehabilitation in the OR under GA. Children whose dental treatment is delayed by waiting for GA suffer increased pain, require more analgesics and antibiotics, and experience life disturbances such as difficulty eating, sleeping, and going to school.23
To improve planning of OR scheduling and to better understand the GA time requirements for pediatric dental patients, this study investigated time utilized for pediatric dental procedures at a regional children’s hospital. The purposes of this study were to:
-
Assess operating room utilization by comparing the amount of dental operator time to the scheduled case time and ask if procedure time is affected by:
ASA status, dental treatment type, patient age, and no. of teeth treated?
anesthesia operator or dental operator types (attending doctor alone or in the presence of a resident/Fellow/certified registered nurse anesthesist [CRNA])?
Analyze data pertaining to the operating room visit regarding the use of: premedication; intraoperative narcotic use; wait time for surgery; type of anesthesia and dental operators; dental treatment type; number of teeth treated; and use of operating room time to perform perioperative tasks (preparing the patient for surgery, anesthesia induction and emergence, performing a timeout, etc.)
Methods
Seattle Children’s Hospital (SCH) is a tertiary care teaching hospital in Seattle, Wash., which serves as the largest pediatric and adolescent medical referral center of any region in the country. SCH is the primary teaching, research, and clinical setting for the Department of Pediatrics at the University of Washington School of Medicine. Numerous medical and dental specialists provide care in the ORs.
This descriptive, cross-sectional records review was approved by the hospital’s Internal Review Board. The study population consisted of the dentistry patients seen in the OR between January 1, 2008 and December 31, 2009. For all patients who were seen more than once during the study period, data were recorded for each encounter. Excluded from the study were any patients scheduled for nondental procedures, combination cases with nondental services, and cases performed by oral surgeons. A total number of 709 cases met the study requirements (Figure 1).
Figure 1.
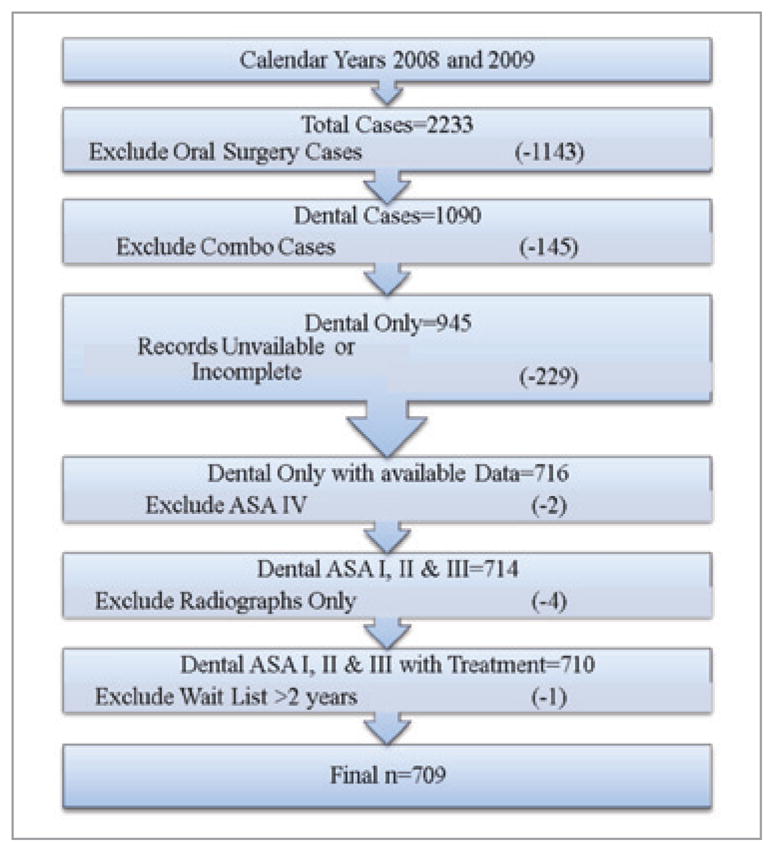
Records identification.
Data collection
Paper charts from SCH were accessed for the anesthesia record and perioperative record data. Computerized charting from SCH Computerized Information Systems and data previously existing in the SCH Dental Medicine clinic database were used for the dental record data collected. The following data for descriptive statistics were recorded: age; gender; weight; ASA classification; waiting list time; number of teeth treated; type of dental treatment; dentist operator type; premedication used; intraoperative use of narcotics; and anesthesia operator type.
The following times were recorded from the paper anesthesia and operative records: (1) patient checked in at hospital; (2) patient present in the OR; (3) patient “anesthesia ready”; (4) dentistry began; (5) dentistry concluded; (6) anesthesia completed (patient arrival in post anesthesia care unit [PACU]); and (7) patient discharged.
Based on the following formulas, the time required for these procedures was calculated: preprocedure anesthesia time= TIME 2 to TIME 3; anesthesia time=TIME 3 to TIME 6; postpocedure anesthesia time=TIME 5 to TIME 6; total dentist operator time=TIME 4 to TIME 5; total OR time utilized= TIME 2 to TIME 6; recovery time=TIME 6 to TIME 7.
Time estimates for scheduling dental cases that were planned during the study period were calculated using the guidelines described in Table 1. The scheduled dental case time was recorded from the surgical scheduling coordinator’s paper records located at SCH. A single calibrated dentist examiner collected all data from the dental and medical records. Ambiguities identified during data collection were resolved by cross referencing between the electronic and paper records. Any ambiguities not thus resolved resulted in the case being excluded from the study. All entries were checked twice by the examiner.
Table 1.
ESTIMATING CASE TIME
| Procedure | Time (mins) |
|---|---|
| Primary dentition:* | |
| 1 posterior quadrant | 15 |
| 1 anterior sextant restorative | 30 |
| Full-mouth coverage | 120 |
| Pulpotomy/pulpectomy | 5 |
| Permanent/late mixed dentition:† | |
| 1 posterior quadrant | 60 |
| 1 anterior sextant | 30 |
| Full-mouth debridement | 60 |
| Endodontic treatment (per tooth) | 60 |
| Extractions (per quadrant) | 15 |
| Additional time requirements:‡ | |
| Oral intubation | +30§ |
| Stent fabrication | +15§ |
| Impressions | +15§ |
| Direct space maintainer | +15§ |
| Restorations of severely crowded teeth | +15 for primary dentition§ +30 for permanent dentition§ |
Example: Dental treatment for 4 posterior quadrants (restorations, extractions, and stainless steel crowns) and 1 anterior sextant of maxillary incisors (esthetic full coverage crowns) would require (4×15)+(1×30)=90 minutes dentist operator time.
Example: Dental treatment for 4 posterior quadrants (restorations and stainless steel crowns) and 1 anterior sextant of maxillary incisors (esthetic full coverage crowns or restorations) would require (4×60)+(1×30)=270 minutes dentist operator time.
Example: For a patient estimated to require 90 minutes of treatment time (as calculated above) who also requires an oral endotracheal tube, another 30 minutes would be added to the scheduled time requested: 90+30=120 minutes planned for the dentist operator time.
Additional time required.
Data analysis
Data were recorded in spreadsheets (Microsoft Excel for Mac 2008, Microsoft Corp, Redmond, Wash., USA). The scheduled dental case time was subtracted from the actual dentist operator time to generate a new variable of “overrun time.” A positive value indicated that the case ran longer than scheduled. A negative value indicated that the case finished early. This new variable was utilized for comparisons between groups. Mean, median, and standard deviation were calculated for the following variables: patient age; patient weight; wait time for surgery; preoperative anesthesia time; anesthesia time; postoperative anesthesia time; total dental operator time; and total OR time. Data for the ASA classification groups, procedure type, age categories, and anesthesia operator type were analyzed using one-way analysis of variance (ANOVA). Data for patient gender, premedication used, narcotic use intraoperatively, number of teeth treated, and dentist operator type were analyzed using a 2-sample t test.
Perioperative management of the dental patient as well as anesthesia considerations must be considered when planning pediatric dental care under GA. Selected variables of ASA classification, premedication use, and narcotics intraoperatively were analyzed as they pertained to preprocedure anesthesia time (time required to prepare the patient for surgery and become “anesthesia ready”) and recovery time (time from arrival in the PACU to the time of patient discharge from the hospital). Data for the ASA classification groups were analyzed using one-way ANOVA. Data for premedication used and narcotic use intraoperatively were analyzed using a 2-sample t test.
Descriptive statistics, 2-sample t tests, and ANOVA were calculated using Stata 11.0 software (StataCorp LP, College Station, Texas, USA). The level of significance was predetermined at P<.05.
Results
A total of 709 cases were analyzed. Although 716 cases met the described inclusion criteria, 7 cases were excluded from the study for these reasons: 2 cases because the patients were categorized as ASA IV; 4 cases because no treatment other than a radiographic exam was rendered; and 1 case because the subject waited almost 2 years between initial examination and surgery date, during which time multiple cancellations and failed appointments occurred for various reasons.
When calculating the amount of wait time for surgery, 222 cases had to be excluded due to the fact that the patients were referred from an outside source and the initial evaluation date was not available in the hospital record. When calculating statistics for postoperative recovery time, only same-day surgeries were included, which resulted in an exclusion of 30 cases that were admitted postoperatively or received dental care with in-patient status.
In our study, the dental procedures finished earlier than the scheduled time by an average of 14 minutes (±28 SD) and overran the scheduled time in 27% of the cases. The average amount of dentist operator time required per case was 76 minutes (±37). The average amount of total OR time required per case (including anesthesia and dentistry) was 110 minutes (±40). The average wait list time was 90 days (±48). The mean age of patients was 7.1 years (±4.2; Table 2). Fifty-eight percent of patients were male. Age categories were created to account for average stages of dentition (primary, mixed, and permanent) by age, with 293 0- to 5-year-old patients (41%), 308 6- to 12- year-old patients (43%); and 108 patients who were at least 13 years old (15%). ASA classifications were distributed as follows: ASA I 226 (32%); ASA II 308 (45%); and ASA III 167 (24%; Table 3). Dental operators were classified as attending (37%) or attending with resident (63%). Anesthesia operators were classified as attending alone (13%), attending with resident or Fellow (53%), and attending with CRNA (35%; Table 4).
Table 2.
DESCRIPTIVE STATISTICS
| Mean (±SD) N=709 | Range | |
|---|---|---|
| Age (years, months) | 7.1 (4.2) | 1.1–21.8 |
| Weight (kg) | 26.1 (16.0) | 9.2–152.7 |
| Wait time (days)* | 90 (48) | 1–359 |
| Preop anesthesia time (mins) | 14 (9) | 0–96 |
| Anesthesia time (mins) | 96 (39) | 7–426 |
| Postop anesthesia time (mins) | 12 (10) | 0–151 |
| Total dentist operator time (mins) | 76 (37) | 9–365 |
| Total operating room time (mins) | 110 (40) | 38–443 |
| Scheduled dentist time (mins) | 91 (35) | 45–420 |
| Overrun time (mins) | −14 (28) | −102–161 |
N=487 due to 222 initial exam records unavailable.
Table 3.
OVERRUN TIME BY PATIENT DEMOGRAPHICS
| N=709 | Scheduled time (mins) | Actual time (mins) | Overrun time (mins) | P-value* | |
|---|---|---|---|---|---|
|
| |||||
| N (%) | Mean (±SD†) | Mean (±SD†) | Mean (±SD†) | ||
| Gender | .94 | ||||
| Male | 409 (58) | 90 (30) | 753(32) | −15 (28) | |
| Female | 300 (42) | 92 (41) | 77 (42) | −14 (28) | |
| Age (ys) | .01 | ||||
| 0–5 | 293 (41) | 86 (17) | 74 (24) | −11 (23) | |
| 6–12 | 308 (44) | 83 (20) | 68 (28) | −15 (26) | |
| 13+ | 108 (15) | 124 (70) | 103 (64) | −21 (41) | |
| ASA classification | .006 | ||||
| ASA I | 226 (32) | 87 (19) | 77 (32) | −10 (28) | |
| ASA II | 316 (45) | 91 (36) | 75 (34) | −16 (25) | |
| ASA III | 167 (23) | 96 (47) | 77 (45) | −19 (31) | |
Calculated using a 2-sample t test or analysis of variance.
SD=standard deviation.
Table 4.
OVERRUN TIME BY DENTAL TREATMENTS
| N=709 | Scheduled time (mins) | Actual time (mins) | Overrun time (mins) | P-value* | |
|---|---|---|---|---|---|
|
| |||||
| N (%) | Mean (±SD†) | Mean (±SD†) | Mean (±SD†) | ||
| No. of teeth treated | <.001 | ||||
| 1–10 | 326 (46) | 82 (21) | 61 (20) | −20 (23) | |
| >10 | 383 (54) | 98 (42) | 88 (42) | −10 (31) | |
| Treatment type | <.001 | ||||
| Operative only | 185 (26) | 92 (36) | 77 (40) | −14 (29) | |
| Extractions only | 29 (4) | 85 (22) | 46 (15) | −39 (24) | |
| Both operative and extractions | 495 (70) | 91 (35) | 78 (36) | −13 (27) | |
Calculated using a 2-sample t test or analysis of variance.
SD=standard deviation.
Overrun time was significantly lower as ASA classification increased (F [2,706]=5.2; P=.006). On average, patients with increasing ASA classification were more likely to finish earlier than scheduled. The significant difference was noted only between the ASA I and ASA III groups (P=.006). A significant difference was found between overrun time for age categories (F [2,706]=4.6; P=.01). On average, older patients tended to finish earlier than scheduled. (Table 3). There was a significant difference between overrun time for dental procedure type (F [2,706]= 12.31; P<.001). On average, “extraction only” cases had less overrun time than either “operative only” and “operative and extractions combined” cases. There was not a significant difference between “operative only” and “operative and extractions combined” cases. There was a statistically significant difference in overrun time for the number of teeth treated (P<.001), with an average of 10 minutes more overrun time when more than 10 teeth were treated (Table 5). Overrun time was significantly lower for dentist attending than attending with resident (P=.005), with an average of 6 minutes more time used when a resident was present (Table 4). There was no statistically significant difference in the amount of overrun time compared between groups of gender, premedication use, intraoperative narcotic use, and anesthesia operator type.
Table 5.
OVERRUN TIME BY OPERATOR TYPES
| N=709 | Scheduled time (mins) | Actual time (mins) | Overrun time (mins) | P-value* | |
|---|---|---|---|---|---|
|
| |||||
| N (%) | Mean (±SD†) | Mean (±SD†) | Mean (±SD†) | ||
| Dentist operator | .005 | ||||
| Without resident | 265 (37) | 91 (32) | 72 (36) | −18 (28) | |
| With resident | 444 (63) | 91 (37) | 78 (36) | −12 (27) | |
| Anesthesia operator | .42 | ||||
| Attending | 89 (12) | 88 (24) | 72 (24) | −16 (22) | |
| Resident/Fellow | 374 (53) | 89 (31) | 76 (36) | −13 (29) | |
| CRNA | 246 (35) | 94 (43) | 78 (40) | −16 (27) | |
Calculated using a 2-sample t test or analysis of variance.
SD=standard deviation.
There was a significant difference between preprocedure anesthesia time between ASA classification groups (F [2,706] =6.46; P=.002). The statistical significance was present when comparing ASA III and ASA I patients. On average, patients with increasing ASA classification severity were more likely to require more anesthesia preparation time. To analyze recovery time, we excluded 30 cases in the study sample of patients who were admitted postoperatively or were inpatient status at the time of their dental procedure. This resulted in a new 3=679 for recovery time analyses. There was a significant difference between recovery time between ASA classification groups (F [2,676]=16.5; P<.001). On average, patients with increasing ASA classification were more likely to require more recovery time postoperatively. There was no significant difference for preprocedure anesthesia time or recovery time when comparisons were made between groups that received premedication and between groups that received narcotics intraoperatively (Tables 6 and 7).
Table 6.
ANESTHESIA PREPROCEDURE TIME
| For all surgeries | N=709 | Preop time (mins) | P-value* |
|---|---|---|---|
|
| |||
| N (%) | Mean (±SD†) | ||
| ASA classification | .002 | ||
| ASA I | 226 (32) | 13 (9) | |
| ASA II | 316 (45) | 14 (8) | |
| ASA III | 167 (23) | 16 (11) | |
| Narcotics intraoperatively | .16 | ||
| Yes | 605 (85) | 14 (9) | |
| No | 104 (15) | 15 (7) | |
| Premedication | .86 | ||
| Yes | 347 (49) | 14 (10) | |
| No | 362 (51) | 14 (7) | |
Calculated using a 2-sample t test or analysis of variance.
SD=standard deviation.
Table 7.
ANESTHESIA RECOVERY TIME
| For day surgeries only | N=679* | Recovery time (mins) | P-value† |
|---|---|---|---|
|
| |||
| N (%) | Mean (±SD‡) | ||
| ASA classification | <.001 | ||
| ASA I | 222 (33) | 83 (44) | |
| ASA II | 311 (46) | 99 (60) | |
| ASA III | 146 (21) | 120 (85) | |
| Narcotics intraoperatively | .51 | ||
| Yes | 578 (85) | 99 (63) | |
| No | 101 (15) | 94 (63) | |
| Premedication | .36 | ||
| Yes | 338 (50) | 100 (55) | |
| No | 101 (50) | 96 (71) | |
Thirty cases omitted requiring postoperative patient hospital admission.
Calculated using a 2-sample t test or analysis of variance.
SD=standard deviation.
Discussion
Key aspects of OR use time that have been previously studied are the: planned vs actual start and finish times; type of operator; turnover and patient transport; and percentage of cancelled surgeries.18,24–26 Foley et al., in 2007 examined the “lost” OR time during pediatric dentistry GA procedures, and also the influence of operator type (experienced attending vs trainee) on the procedure length. These authors identified case cancellation and patient transportation between preoperative holding areas and the OR as major factors in “lost” OR time in a British teaching hospital. The same study reported a nonstatistically significant difference in procedure length for an experienced provider compared to a provider-in-training.18
While our study examined OR time utilization on a case-by-case basis, other studies have examined OR utilization and efficiency on a day-by-day basis, comparing the amount of time the OR was in use to the amount of available time for surgical procedures. Ogden et al., reported an OR utilization of 79% for dentoalveolar surgeries under GA.26 Tyler et al., used a simulated OR schedule to investigate efficiency and found a maximum efficiency of 85% to 90% when the goals of case starting and ending within 15 minutes of the scheduled time were met. The authors conceded, however, that this percentage may not be feasible “in the real world” of patient-related delays and inevitable case cancellations.24
The results of the present study describe characteristics of a pediatric dentistry population treated under GA in a hospital OR. This study reports utilization on a case-by-case basis over a 2-year period. We also reported the average amount of time required for perioperative patient management in addition to operator time. Seventy-three percent of cases finished early or on time, indicating a tendency to overestimate the time required when planning cases.
The main factors influencing the amount of dentist operator time were: patient ASA classification; dental treatment type; patient age; number of teeth treated; and presence of a dental resident. As ASA classification increased, overrun time decreased, indicating that more medically complex patients required less OR time than was scheduled for dental procedures. This finding may be due to the tendency for medically complicated patients to require a more agressive approach (less restorative treatment and more dental extractions). Patients in this category may be more likely to receive nutrition by gastrostomy tube, which would lower caries risk.
For patients with complex medical histories who also required extensive dental treatment (especially when a clinical exam was difficult), however, the scheduled time may have been significantly underestimated. This may account for the extensive overrun times that were observed for a small number of patients. Patients with complicated medical histories may be more likely to receive dental care under GA in combination with another medical or surgical procedure, and these cases were excluded from our study. The fact that ASA II and III patients comprised 69% of the study population may have skewed our results. As such, these findings from a hospital-based population may not be applicable to a surgery center or in-office anesthesia setting where mostly ASA I and II patients receive care.
It was also found that, as ASA classification increased, anesthesia time requirements for preoperative patient preparation and recovery time also increased. These findings reflect that increasing ASA classification for patients often necessitates more prolonged perioperative monitoring and patient management due to medical status. Thus, when planning dental treatment under GA for medically complex patients, the anesthesia and recovery time demands as well as the dental time demands must both be considered carefully.
Older patients tended to finish earlier than scheduled vs younger patients, with more of the scheduled time being utilized by younger patients. This finding may be due to the greater unpredictability in case planning for older children, especially children with special health care needs for whom a thorough dental examination is difficult. There may be a tendency to overestimate the amount of time required for patients with permanent dentition, especially when the initial exam has been of poor diagnostic value. Because an understimation of the operative time needed in patients with permanent dentition has a stronger impact in the OR schedule, these findings for age groups are understandable. Furthermore, older patients may be at increased risk for other oral problems such as periodontal disease and impacted third molars, which would change the types of oral procedures required by these patients.
Cases that required extraction treatment only, rather than operative dentistry or a combination of both treatment types, tended to finish earlier. This finding is consistent with the fact that extractions in general are less technically demanding and time consuming than restorations. In some cases, it may not be known whether a patient will require extractions only or extractions and restorations. Upon clinical and radiographic exam obtained on the day of treatment, it may be found that teeth cannot be restored and are indicated for extraction. Thus, a case that was planned with time allowed for restorations and requires extractions only will finish early. When patients had 1 to 10 teeth treated, they tended to finish earlier relative to the scheduled time than when patients had more than 10 teeth treated. This finding is intuitive in that treating more teeth usually takes more time for the same operator.
Although the results reported here indicate a statistically significant difference in procedure time between dentist attending and attending with resident, the average amount of overrun time difference of 6 minutes may not be clinically significant. It is possible that this difference was observed because the presence of a resident requires greater attention to teaching on the part of the attending dentist and the resident lacks the expertise of an attending dentist. It is noteworthy, however, that, on average, cases finished earlier than scheduled whether there was a resident present or not. Furthermore, the value of learning in the OR for residents in a pediatric dentistry program is high, and a vital component of the educational experience.
This study had several limitations. There was lack of information regarding 222 initial examination records. These initial exams were performed at either the Odessa Brown Children’s Dental Clinic in Seattle, a local community health center affiliated with Seattle Children’s Hospital, or at the Department of Pediatric Dentistry of the School of Dentistry at the University of Washington. Accessing all of these initial records was beyond the scope of this project. Furthermore, the data were collected from an academic teaching hospital, which may not reflect trends in a private practice setting. A more detailed analysis of the number of dental procedures performed for each case would be beneficial in further assessing the adequacy of the scheduling guidelines previously described.
Documenting detailed procedure type (the number of stainless steel crowns, pulp treatments, composite and amalgam restorations, extractions, and primary vs permanent tooth procedures) was not chosen as a variable for this project, but a more detailed analysis of procedure type would be interesting and could help dentists better plan for effective use of OR time. Another variable that would have been interesting to examine is body mass index in relation to overrun time and time required for perioperative patient management. Additionally, overweight and obese patients require additional time and equipment when draping and preparing the patient for surgery and may require different dosing of medications and specific anesthesia concerns due to weight on the thoracic cavity. While patient weight was recorded, height was not included in the dataset, so BMI could not be calculated. Given the increasing number of pediatric patients with overweight and obesity conditions, this variable may be of interest when planning a dental case in the OR.
Conclusions
Based on this study’s results, the following conclusions can be made:
Seventy-three percent of dental procedures under general anesthesia finished early or on time in regard to dentist operator time.
Variables that influenced time utilization included: patient age (older patients tended to finish earlier than scheduled); American Society of Anesthesiology classification (more medically complex patients tended to finish earlier than scheduled); dentist operator type (cases in which a dental resident was present tended to utilize more dentist operator time than cases performed by an attending dentist alone); number of teeth treated (patients requiring a greater number of teeth treated tended to use more dentist operator time); and dental procedure type (patients requiring extraction treatment only tended to use less dentist operator time than patients requiring extraction and operative treatment, or operative treatment only).
Assessing factors that impact the time needed for pediatric dental cases performed under general anesthesia may enhance the efficiency of the operating room for pediatric dental procedures.
When planning future dental cases under general anesthesia, mindfulness of significant variables may increase efficiency of operating room utilization.
Acknowledgments
The authors wish to thank the staff at Seattle Children’s Hospital for their assistance in records review for this project. H. H. Lee is funded by the National Institutes of Health (grant T32GM086270 Department of Anesthesiology and Pain Medicine, University of Washington).
References
- 1.American Academy of Pediatric Dentistry. Policy on the use of deep sedation and general anesthesia in the pediatric dental office. Pediatr Dent. 2010;30:64–5. [PubMed] [Google Scholar]
- 2.Ba’akdah R, Frasi N, Boker A, Al Mushayt A. The use of general anesthesia in pediatric dental care of children at multi-dental centers in Saudi Arabia. J Clin Pediatr Dent. 2008;33:147–53. doi: 10.17796/jcpd.33.2.r6kl233707g20x30. [DOI] [PubMed] [Google Scholar]
- 3.AAPD. Guideline on behavior guidance for the pediatric dental patient. Pediatr Dent. 2010;30:132–40. [PubMed] [Google Scholar]
- 4.AAPD. Oral health policy on hospitalization and operating room access for dental care of infants, children, adolescents, and persons with special health care needs. Pediatr Dent. 2010;30:68–9. [PubMed] [Google Scholar]
- 5.AAPD. Definition of medically necessary care. Pediatr Dent. 2010;30:14. [Google Scholar]
- 6.Hurford WE, editor. Clinical Anesthesia Procedures of the Massachusetts General Hospital. 6. Chapter 1. Philadelphia, Pa: Lippincott Williams and Wilkins; 2002. p. 10. [Google Scholar]
- 7.Lee JY, Roberts MW. Mortality risks associated with pediatric dental care using general anesthesia in a hospital setting. J Clin Pediatr Dent. 2003;27:381–3. doi: 10.17796/jcpd.27.4.e3gw10732q917757. [DOI] [PubMed] [Google Scholar]
- 8.Adair SM, 3Waller JL, 3Schafer TE, 3Rockman RA. A survey of members of the American Academy of Pediatric Dentistry on their use of behavior management techniques. Pediatr Dent. 2004;26:159–66. [PubMed] [Google Scholar]
- 9.Alammouri M. The attitude of parents toward behavior management techniques in pediatric dentistry. J Clin Pediatr Dent. 2006;30:310–3. doi: 10.17796/jcpd.30.4.m73568r0t74962m3. [DOI] [PubMed] [Google Scholar]
- 10.Murphy MG, Fields HW, Jr, Machen JB. Parental acceptance of pediatric dentistry behavior management techniques. Pediatr Dent. 1984;6:193–8. [PubMed] [Google Scholar]
- 11.Eaton JJ, McTigue DJ, Fields HW, Jr, Beck M. Attitudes of contemporary parents toward behavior management techniques used in pediatric dentistry. Pediatr Dent. 2005;27:107–13. [PubMed] [Google Scholar]
- 12.Anderson HK, 3Drummond BK, Thomson WM. Changes in aspects of children’s oral-health-related quality of life following dental treatment under general anaesthesia. Int J Paediatr Dent. 2004;14:317–25. doi: 10.1111/j.1365-263X.2004.00572.x. [DOI] [PubMed] [Google Scholar]
- 13.Acs G, Pretzer S, Foley M, Ng MW. Perceived outcomes and parental satisfaction following dental rehabilitation under general anesthesia. Pediatr Dent. 2001;23:419–23. [PubMed] [Google Scholar]
- 14.Lee JY, Vann WF, Roberts MW. A cost analysis of treating pediatric dental patients using general anesthesia vs conscious sedation. Pediatr Dent. 2000;22:27–32. [PubMed] [Google Scholar]
- 15.Eidelman E, Faibis S, Peretz B. A comparison of restorations for children with early childhood caries treated under general anesthesia or conscious sedation. Pediatr Dent. 2000;22:33–7. [PubMed] [Google Scholar]
- 16.Al-Eheideb AA, 3Herman NG. Outcomes of dental procedures performed on children under general anesthesia. J Clin Pediatr Dent. 2003;27:181–3. doi: 10.17796/jcpd.27.2.k3307186n7086r11. [DOI] [PubMed] [Google Scholar]
- 17.Fuhrer CT, III, Weddell JA, Sanders BJ, Jones JE, Dean JA, Tomlin A. Effect on behavior of dental treatment rendered under conscious sedation and general anesthesia in pediatric patients. Pediatr Dent. 2009;31:492–7. [PubMed] [Google Scholar]
- 18.Foley J, Soldani F. The use of theatre time for paediatric dentistry under general anaesthesia. Int J Paediatr Dent. 2007;17:29–33. doi: 10.1111/j.1365-263X.2006.00789.x. [DOI] [PubMed] [Google Scholar]
- 19.Stapleton M, Sheller B, Williams BJ, Mancl L. Combining procedures under general anesthesia. Pediatr Dent. 2007;29:397–402. [PubMed] [Google Scholar]
- 20.Pandit JJ, 3Westbury S, 3Pandit M. The concept of surgical operating list “efficiency”: A formula to describe the term. Anaesthesia. 2007;62:895–903. doi: 10.1111/j.1365-2044.2007.05174.x. [DOI] [PubMed] [Google Scholar]
- 21.Lewis CW, Nowak AJ. Stretching the safety net too far: Waiting times for dental treatment. Pediatr Dent. 2002;24:6–10. [PubMed] [Google Scholar]
- 22.Kanellis MJ, Damiano PC, Momany ET. Medicaid costs associated with the hospitalization of young children for restorative dental treatment under general anesthesia. J Public Health Dent. 2000;60:28–32. [PubMed] [Google Scholar]
- 23.North S, Davidson LE, Blinkhorn AS, Mackie IC. The effects of a long wait for children’s dental general anaesthesia. Int J Paediatr Dent. 2007;17:105–9. doi: 10.1111/j.1365-263X.2006.00790.x. [DOI] [PubMed] [Google Scholar]
- 24.Tyler DC, Pasquariello CA, Chen CH. Determining optimum operating room utilization. Anesth Angl. 2003;96:1114–21. doi: 10.1213/01.ANE.0000050561.41552.A6. [DOI] [PubMed] [Google Scholar]
- 25.Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning. Anesthesiology. 1999;90:1176–85. doi: 10.1097/00000542-199904000-00034. [DOI] [PubMed] [Google Scholar]
- 26.Ogden GR, Kershaw AE, Hussein I. Use of theatre time for dentoalveolar operations under general anesthesia. Br J Oral Maxillofac Surg. 2000;38:331–4. doi: 10.1054/bjom.2000.0309. [DOI] [PubMed] [Google Scholar]


