Abstract
A case of primary buccal squamous cell carcinoma arising in a patient with uterine papillary serous carcinoma after long-term pegylated liposomal doxorubicin treatment is presented.
Keywords: Pegylated liposomal doxorubicin, Endometrial cancer, Secondary malignancy, Squamous cell carcinoma
Dear Editor,
We read the article by Cannon et al. [1] with great interest. The authors reported five ovarian and fallopian tubal cancer patients who developed oromaxillary squamous cell carcinoma (SCC) during long-term maintenance therapy with pegylated liposomal doxorubicin (PLD) (range, 30–132 months; cumulative dose, 1,696–3,000 mg/m2). Notably, four of the five patients were positive for a BRCA mutation, suggesting a hereditary component to long-term PLD use and subsequent susceptibility to oromaxillary cancer in ovarian cancer patients.
Recently, a case of primary buccal SCC arising in a patient with uterine papillary serous carcinoma after long-term PLD treatment was seen in our institution. Briefly, a 56-year-old Hispanic woman without a family history of cancer or personal history of smoking was diagnosed with stage IV uterine papillary serous carcinoma. She received neoadjuvant chemotherapy with carboplatin and paclitaxel (three cycles) followed by interval tumor reduction. Postoperatively, she was given four additional cycles of carboplatin and paclitaxel, followed by whole pelvic radiotherapy (5,040 cGy) with weekly cisplatin. She developed vaginal cuff and retroperitoneal nodal recurrence 4 months after the completion of radiotherapy, and PLD treatment was therefore initiated. Brain metastases were detected 23 months after the initial surgical staging. The tumor was resected via craniotomy and she received whole brain radiotherapy thereafter (3,000 cGy). She continued to receive PLD (47 cycles total), with a cumulative dose of 3,924 mg until she progressed. The entire duration of PLD treatment was tolerated well without remarkable adverse events (intermittent grade 1 mucositis). Shortly after the discontinuation of PLD, she presented with a painful growing lump in her right cheek (Fig. 1). On exam there was a 3- to 4-cm palpable mass, which was diagnosed as an abscess and treated with oral antibiotics. However, her symptoms worsened and she underwent tooth extraction with adjacent soft tissue removal. Histopathology analysis revealed invasive moderately differentiated SCC. Imaging demonstrated a 4.5-cm mass involving the gingival mucosa and eroding into the mandible. She was staged cT4bN0 and received radiotherapy. The buccal tumor rapidly progressed despite the radiotherapy. Although she received additional chemotherapy with 5-fluorouracil, cisplatin, and cetuximab (two cycles), she deteriorated as the result of an inability to tolerate oral intake secondary to the expanding oromaxillary tumor. She expired 4 months after the diagnosis of buccal cancer.
Figure 1.
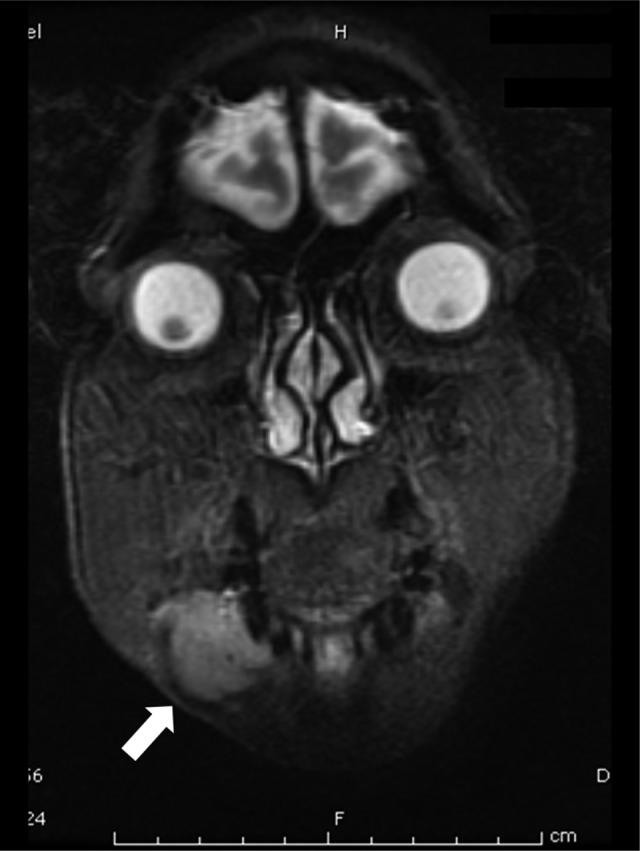
Imaging of an oromaxillary squamous cell carcinoma. Coronal view of magnetic resonance imaging is shown (white arrow points to the tumor).
In a literature review, with the exception of HIV-related Kaposi sarcoma, all patients who developed oromaxillary SCC after long-term use of PLD had mullerian cancer, suggesting a cancer-specific linkage [1, 2]. However our case was endometrial cancer, thus implying that this complication is also relevant to malignancies other than mullerian cancer. Notably, two patients in Cannon et al.'s report [1] who received radiotherapy developed tumor progression fairly soon after treatment. A similar finding was observed in our case experience, suggesting that oromaxillary SCC developing after long-term PLD use may be radiorefractory, a characteristic potentially exacerbated by a history of radiation to the brain. PLD is known to be one of the effective antitumor agents for ovarian cancer and is commonly used after recurrence [3]; hence, further investigation into the long-term adverse effects of PLD treatment is definitively warranted, and setting limitations on the maximum dose of PLD should be taken into consideration.
Editor's Note: We publish in this issue a brief series of related papers and letters that examine possible side effects of long-term exposure to pegylated liposomal doxorubicin (PLD). See pages 1534–1540 for a report of the occurrence of the renal thrombotic microangiopathy in ovarian cancer patients exposed to PLD; pages 1541–1546 for a report of squamous cell carcinoma (SCC) of the mouth in non-smoking women with recurrent ovarian cancer; and pages 1594–1597 for two additional Letters to the Editor that relate other cases of SCC of the oral cavity in patients with long-term PLD exposure.
Author Contributions
Conception/Design: Koji Matsuo, Erin A. Blake, Annie A. Yessaian, Lynda D. Roman
Provision of study material or patients: Lynda D. Roman
Manuscript writing: Koji Matsuo, Erin A. Blake, Annie A. Yessaian, Lynda D. Roman
Final approval of manuscript: Koji Matsuo, Erin A. Blake, Annie A. Yessaian, Lynda D. Roman
References
- 1.Cannon TL, Lai DW, Hirsch D, et al. Squamous cell carcinoma of the oral cavity in nonsmoking women: A new and unusual complication of chemotherapy for recurrent ovarian cancer? The Oncologist. 2012 May 23; doi: 10.1634/theoncologist.2011-0216. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ben-David Y, Leiser Y, Kachta O, et al. Does long-term treatment with Doxil predispose patients to oral cancer? Int J Clin Oncol. 2012 Mar 20; doi: 10.1007/s10147-012-0400-1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Matsuo K, Lin YG, Roman LD, et al. Overcoming platinum resistance in ovarian carcinoma. Expert Opin Investig Drugs. 2010;19:1339–1354. doi: 10.1517/13543784.2010.515585. [DOI] [PMC free article] [PubMed] [Google Scholar]


