Abstract
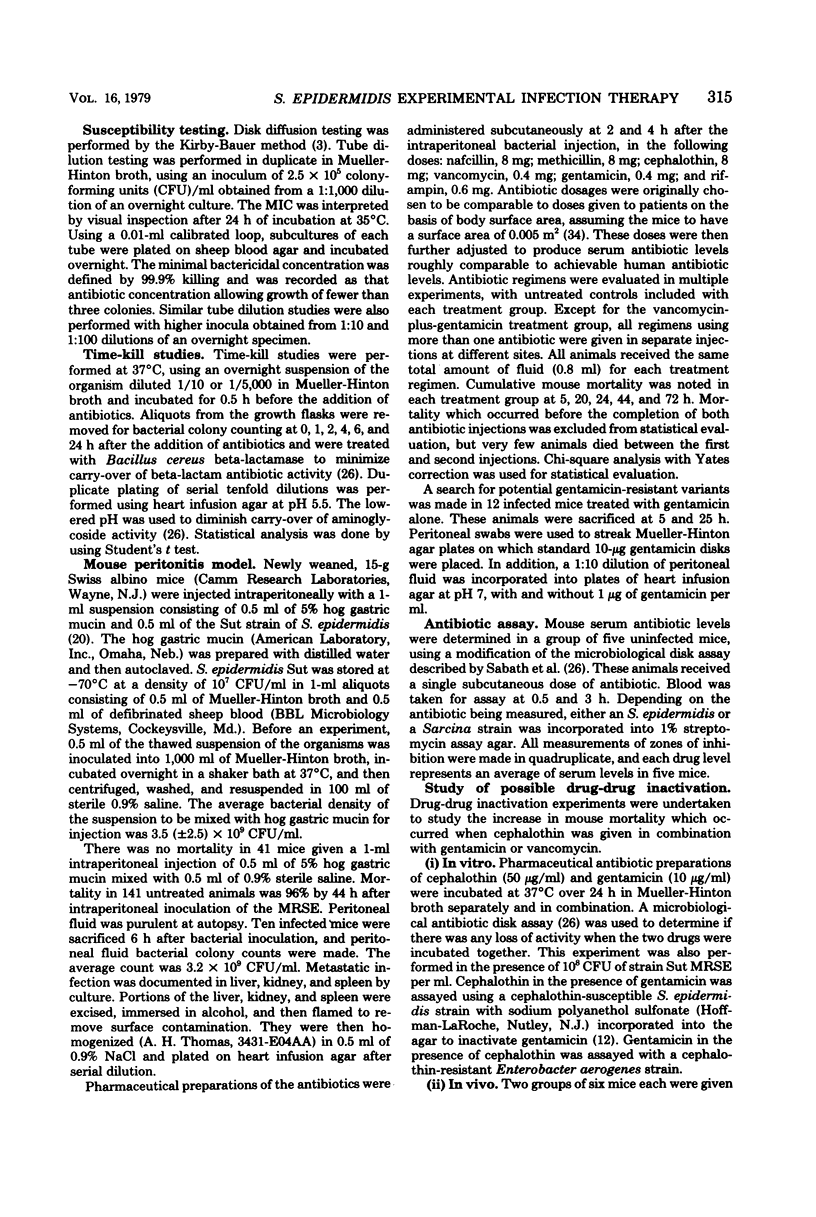
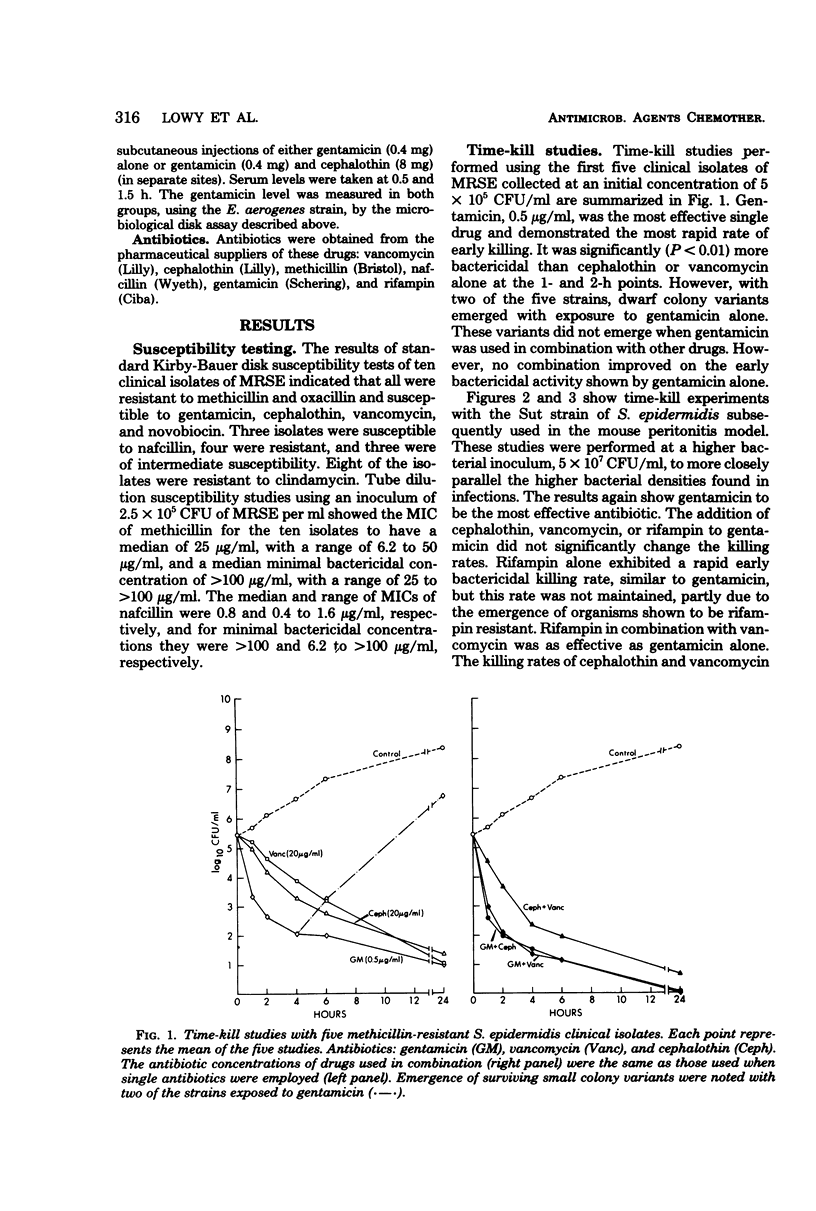
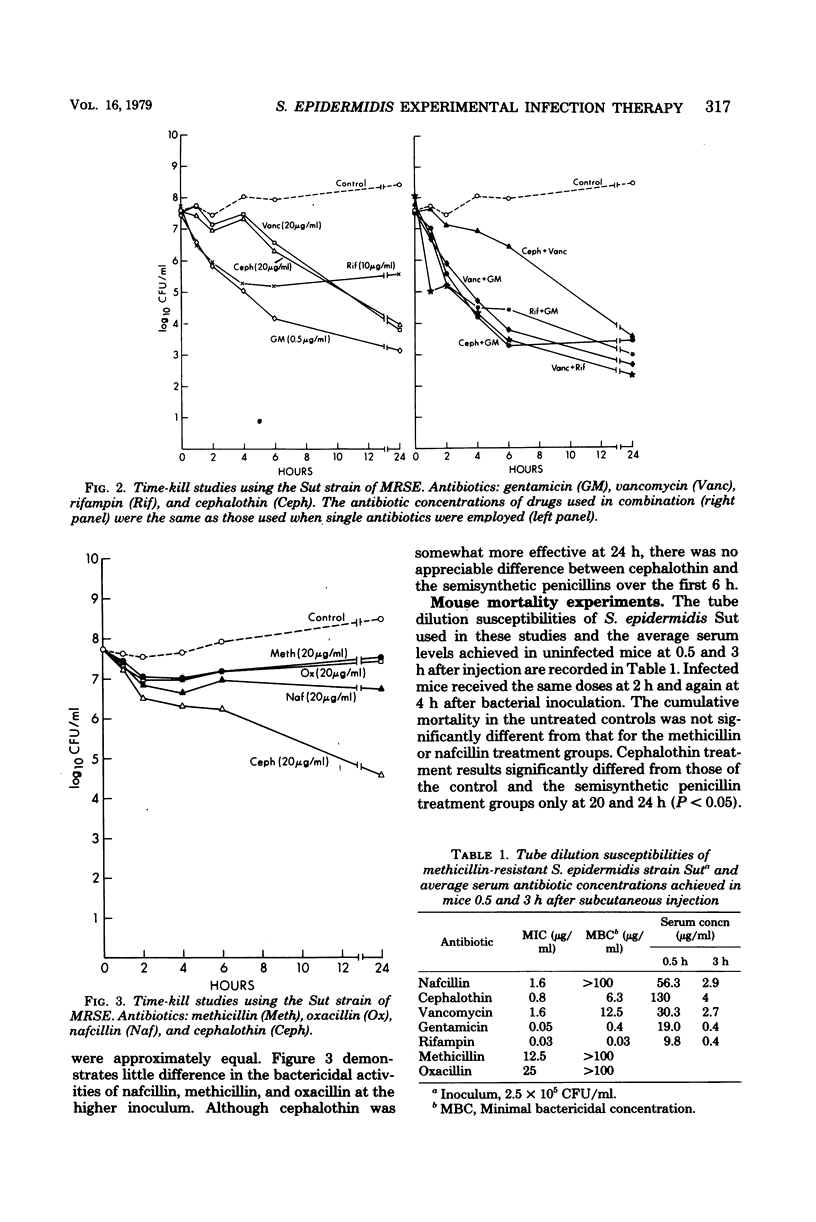
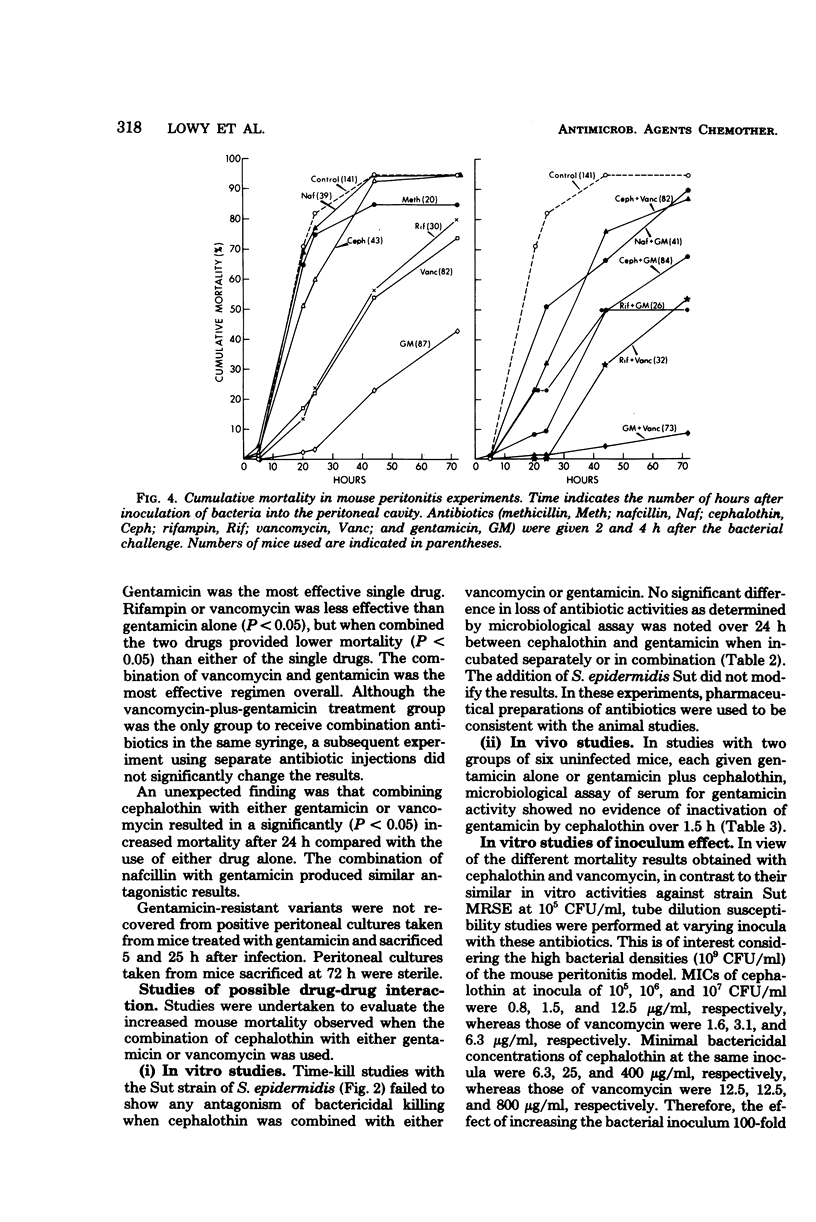
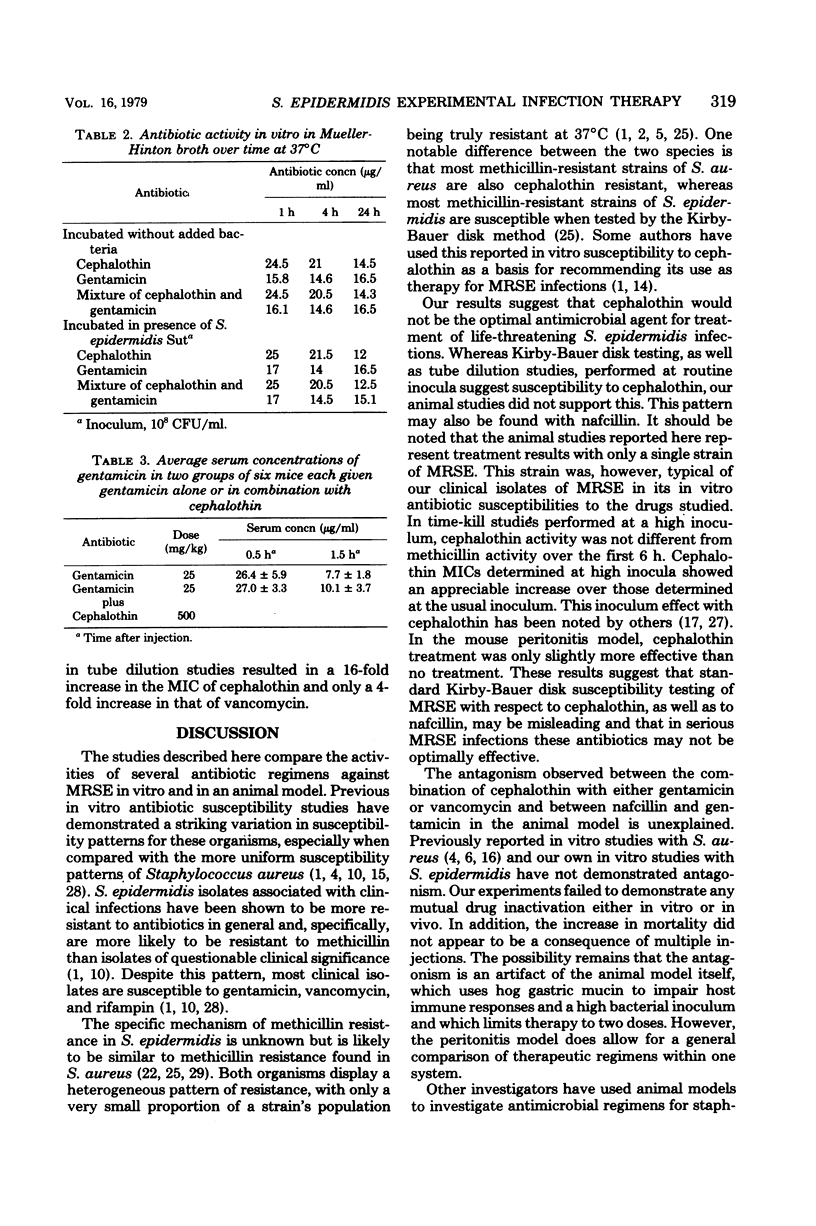
Staphylococcus epidermidis is a major pathogen in early prosthetic valve endocarditis and cerebrospinal fluid shunt infections. Approximately 10 to 15% of hospital isolates are methicillin resistant. Ten clinically significant isolates of the latter were collected for antibiotic studies in vitro and in an experimental infection in animals. Time-kill studies of five strains showed gentamicin to be the single most effective antibiotic; however, dwarf colony variants emerged as survivors with two of these strains when challenged with gentamicin alone. The addition of a second antibiotic to gentamicin did not significantly improve the bactericidal rate but prevented the emergence of variant strains. A blood culture isolate of methicillin-resistant S. epidermidis combined with 5% hog gastric mucin was used to establish an experimental intraperitoneal infection in mice. Neither methicillin nor nafcillin treatment reduced mortality below that of untreated animals. Cephalothin treatment delayed early mortality but did not diminish overall mortality. Gentamicin was the most effective single antibiotic, and gentamicin in combination with vancomycin was the most effective regimen overall. The combination of rifampin plus vancomycin was as effective as gentamicin alone. The combinations of cephalothin or nafcillin with gentamicin and cephalothin with vancomycin demonstrated antagonism. The antagonism was not due to multiple injections or drug-drug inactivation.
Full text
PDF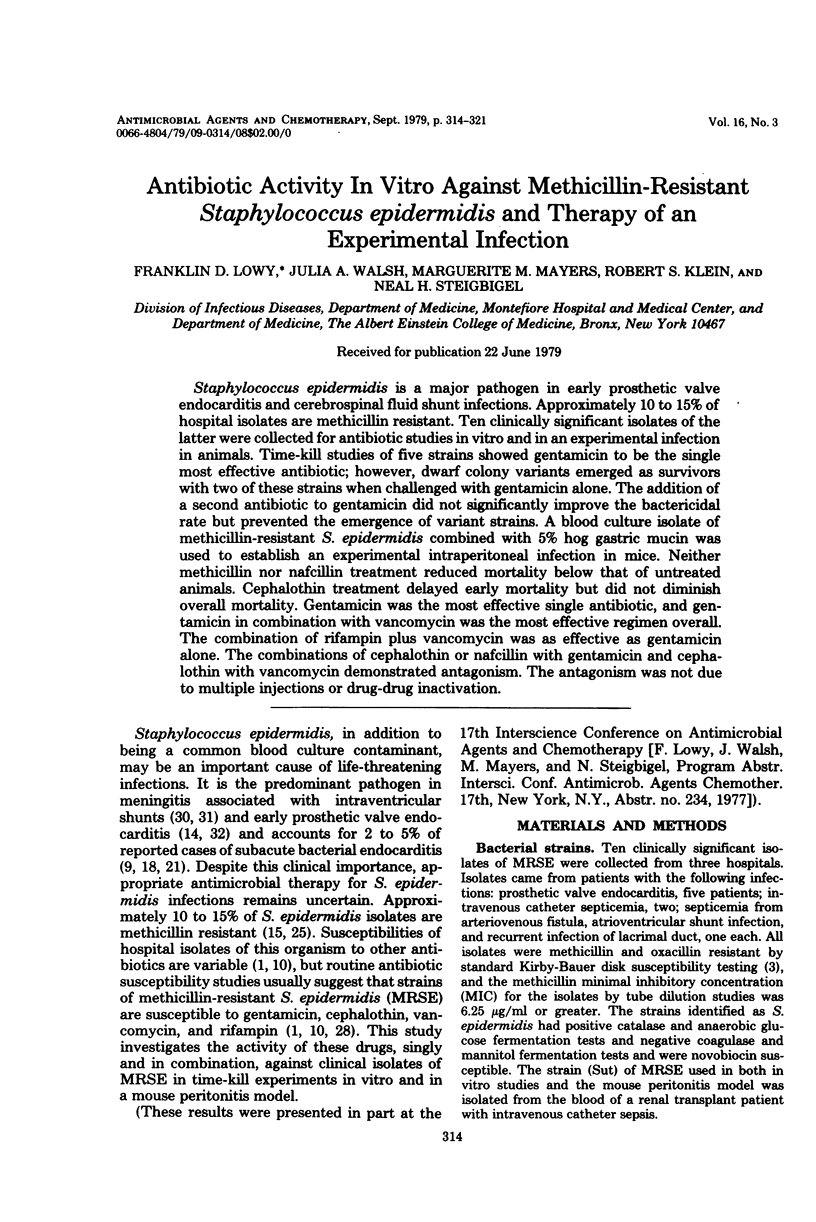
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andriole V. T., Lyons R. W. Coagulase-negative staphylococcus. Ann N Y Acad Sci. 1970 Oct 30;174(2):533–544. doi: 10.1111/j.1749-6632.1970.tb45579.x. [DOI] [PubMed] [Google Scholar]
- Archer G. L. Antimicrobial susceptibility and selection of resistance among Staphylococcus epidermidis isolates recovered from patients with infections of indwelling foreign devices. Antimicrob Agents Chemother. 1978 Sep;14(3):353–359. doi: 10.1128/aac.14.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Benner E. J., Morthland V. Methicillin-resistant Staphylococcus aureus. Antimicrobial susceptibility. N Engl J Med. 1967 Sep 28;277(13):678–680. doi: 10.1056/NEJM196709282771303. [DOI] [PubMed] [Google Scholar]
- Bentley D. W. Methicillin resistance in Staphylococcus epidermidis epidemiologic studies. Contrib Microbiol Immunol. 1973;1:650–658. [PubMed] [Google Scholar]
- Bulger R. J., Feigl P., Nielson K. Comparison of treatments with several antibiotics in experimental infections due to methicillin-resistant Staphylococcus aureus. J Infect Dis. 1972 Dec;126(6):674–678. doi: 10.1093/infdis/126.6.674. [DOI] [PubMed] [Google Scholar]
- Bulger R. J. In-vitro activity of cephalothin/kanamycin and methicillin/kanamycin combinations against methicillin-resistant Staphylococcus aureus. Lancet. 1967 Jan 7;1(7480):17–19. doi: 10.1016/s0140-6736(67)92422-1. [DOI] [PubMed] [Google Scholar]
- Campos M. E., Rabinovich S., Smith I. M. Therapy of experimental staphylococcal infection with antibiotic combinations. J Lab Clin Med. 1974 Feb;83(2):241–248. [PubMed] [Google Scholar]
- Cherubin C. E., Neu H. C. Infective endocarditis at the Presbyterian Hospital in New York City from 1938-1967. Am J Med. 1971 Jul;51(1):83–96. doi: 10.1016/0002-9343(71)90326-3. [DOI] [PubMed] [Google Scholar]
- Corse J., Williams R. E. Antibiotic resistance of coagulase-negative staphylococci and micrococci. J Clin Pathol. 1968 Nov;21(6):722–728. doi: 10.1136/jcp.21.6.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EAGLE H. Further observations on the zone phenomenon in the bactericidal action of penicillin. J Bacteriol. 1951 Nov;62(5):663–668. doi: 10.1128/jb.62.5.663-668.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edberg S. C., Bottenbley C. J., Gam K. Use of sodium polyanethol sulfonate to selectively inhibit aminoglycoside and polymyxin antibiotics in a rapid blood level antibiotic assay. Antimicrob Agents Chemother. 1976 Mar;9(3):414–417. doi: 10.1128/aac.9.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KJELLANDER J. O., KLEIN J. O., FINLAND M. IN VITRO ACTIVITY OF PENICILLINS AGAINST STAPHYLOCOCCUS ALBUS. Proc Soc Exp Biol Med. 1963 Aug-Sep;113:1023–1031. doi: 10.3181/00379727-113-28563. [DOI] [PubMed] [Google Scholar]
- Klastersky J. Antibiotic susceptibility of oxacillin-resistant staphylococci. Antimicrob Agents Chemother. 1972 May;1(5):441–446. doi: 10.1128/aac.1.5.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laverdiere M., Peterson P., Verhoef J., Williams D. N., Sabath L. D. In vitro activity of cephalosporins against methicillin-resistant, coagulase-negative staphylococci. J Infect Dis. 1978 Mar;137(3):245–250. doi: 10.1093/infdis/137.3.245. [DOI] [PubMed] [Google Scholar]
- Lerner P. I., Weinstein L. Infective endocarditis in the antibiotic era. N Engl J Med. 1966 Jan 27;274(4):199–contd. doi: 10.1056/NEJM196601272740407. [DOI] [PubMed] [Google Scholar]
- Olitzki L. MUCIN AS A RESISTANCE-LOWERING SUBSTANCE. Bacteriol Rev. 1948 Jun;12(2):149–172. doi: 10.1128/br.12.2.149-172.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier L. L., Jr, Petersdorf R. G. Infective endocarditis: a review of 125 cases from the University of Washington Hospitals, 1963-72. Medicine (Baltimore) 1977 Jul;56(4):287–313. [PubMed] [Google Scholar]
- Plorde J. J., Sherris J. C. Staphylococcal resistance to antibiotics: origin, measurement, and epidemiology. Ann N Y Acad Sci. 1974 Jul 31;236(0):413–434. doi: 10.1111/j.1749-6632.1974.tb41507.x. [DOI] [PubMed] [Google Scholar]
- Quinn E. L., Cox F., Fisher M. The problem of associating coagulase-negative staphylococci with disease. Ann N Y Acad Sci. 1965 Jul 23;128(1):428–442. doi: 10.1111/j.1749-6632.1965.tb11652.x. [DOI] [PubMed] [Google Scholar]
- Richards F., McCall C., Cox C. Gentamicin treatment of staphylococcal infections. JAMA. 1971 Feb 22;215(8):1297–1300. [PubMed] [Google Scholar]
- Sabath L. D., Barrett F. F., Wilcox C., Gerstein D. A., Finland M. Methicillin resistance of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob Agents Chemother (Bethesda) 1968;8:302–306. [PubMed] [Google Scholar]
- Sabath L. D., Casey J. I., Ruch P. A., Stumpf L. L., Finland M. Rapid microassay of gentamicin, kanamycin, neomycin, streptomycin, and vancomycin in serum or plasma. J Lab Clin Med. 1971 Sep;78(3):457–463. [PubMed] [Google Scholar]
- Sabath L. D., Garner C., Wilcox C., Finland M. Effect of inoculum and of beta-lactamase on the anti-staphylococcal activity of thirteen penicillins and cephalosporins. Antimicrob Agents Chemother. 1975 Sep;8(3):344–349. doi: 10.1128/aac.8.3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabath L. D., Garner C., Wilcox C., Finland M. Susceptibility of Staphylococcus aureus and Staphylococcus epidermidis to 65 antibiotics. Antimicrob Agents Chemother. 1976 Jun;9(6):962–969. doi: 10.1128/aac.9.6.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabath L. D., Wallace S. J. The problems of drug-resistant pathogenic bacteria. Factors influencing methicillin resistance in staphylococci. Ann N Y Acad Sci. 1971 Jun 11;182:258–266. doi: 10.1111/j.1749-6632.1971.tb30662.x. [DOI] [PubMed] [Google Scholar]
- Schoenbaum S. C., Gardner P., Shillito J. Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis. 1975 May;131(5):543–552. doi: 10.1093/infdis/131.5.543. [DOI] [PubMed] [Google Scholar]
- Shurtleff D. B., Foltz E. L., Weeks R. D., Loeser J. Therapy of staphylococcus epidermidis: infections associated with cerebrospinal fluid shunts. Pediatrics. 1974 Jan;53(1):55–62. [PubMed] [Google Scholar]
- Slaughter L., Morris J. E., Starr A. Prosthetic valvular endocarditis. A 12-year review. Circulation. 1973 Jun;47(6):1319–1326. doi: 10.1161/01.cir.47.6.1319. [DOI] [PubMed] [Google Scholar]
- Smith I. M., Hazard E. C. Anomalous results of high dose chemotherapy in experimental peritonitis. Surg Gynecol Obstet. 1970 Jan;130(1):94–98. [PubMed] [Google Scholar]
- Steigbigel R. T., Greenman R. L., Remington J. S. Antibiotic combinations in the treatment of experimental Staphylococcus aureus infection. J Infect Dis. 1975 Mar;131(3):245–251. doi: 10.1093/infdis/131.3.245. [DOI] [PubMed] [Google Scholar]



