Abstract
Objective
To determine the care pathways and implications of offering mothers the choice of external cephalic version (ECV) at term for singleton babies who present with an uncomplicated breech pregnancy versus assisted breech delivery or elective caesarean.
Design
A prospective observational audit to construct a decision analysis of uncomplicated full term breech presentations.
Setting
The North Staffordshire NHS Trust.
Subjects
All women (n = 176) who presented at full term with a breech baby without complications during July 1995 and June 1997.
Main outcome measures
The study determined to compare the outcome in terms of the costs and cost consequences for the care pathways that resulted from whether a women chose to accept the offer of ECV or not. All the associated events were then mapped for the two possible pathways. The costs were considered only within the hospital setting, from the perspective of the health care provider up to the point of delivery.
Results
The additional costs for ECV, assisted breech delivery and elective caesarean over and above a normal birth were £186.70, £425.36 and £1,955.22 respectively. The total expected cost of the respective care pathways for "ECV accepted" and "ECV not accepted" (including the probability of adverse events) were £1,452 and £1,828 respectively, that is the cost of delivery through the ECV care pathways is less costly than the non ECV delivery care pathway.
Conclusions
Implementing an ECV service may yield cost savings in secondary care over and above the traditional delivery methods for breech birth of assisted delivery or caesarean section. The scale of these expected cost savings are in the range of £248 to £376 per patient. This converts to a total expected cost saving of between £43,616 and £44,544 for the patient cohort considered in this study.
Introduction
The incidence of breech presentation at term is between 3-4%.[1] Breech presentations are at a greater risk of perinatal and neonatal mortality and morbidity than cephalic presentations, [2] with an excess risk of neonatal death quoted of 4/1,000.[3]
Currently 70-80% of breech presentations are dealt with by caesarean section.[4,5] This is the third highest contribution to the rise in caesarean births seen in the past two decades.[6]
Two standard strategies remain widely accepted for the management of breech presentations;
(i) assisted vaginal delivery for selected low risk patients and
(ii) elective caesarean section.
More recently, external cephalic version (ECV), the manipulative transabdominal conversion of the breech to cephalic presentation, has come to be recognised as a third alternative for uncomplicated breech presentations at 37+ weeks for low risk patients. Evidence suggests that ECV is a safe and successful method for correcting breech presentations.[7] Success rates vary between 48 and 77%.[1,8]
The Royal College of Obstetricians and Gynaecologists recommends that all women with an uncomplicated breech presentation at term should be offered ECV.[9]
Methods
The Setting
A good practice standard that "100% of women with an uncomplicated breech presentation at term should be offered ECV", was introduced by the North Staffordshire NHS Trust (ASQUAM Project) in 1995.[10] Women who presented with an uncomplicated pregnancy at term were offered the choice of an ECV in the ante natal clinic or community, this will be 80% of the number of breech presentations. ECV was done in early or late pregnancy none of the cases were in labour or were repetitions. ECV is a low risk procedure to both the fetus and the mother. There is less than a 1% risk to the fetus and an even smaller risk to the mother in terms of fetal complications.
This work presents a prospective audit of practice during a two year period: July 1995 to June 1997. It considers two options whether patients accept ECV management of a breech pregnancy or not and the resultant care pathway. The study design was observational cohort analysis.
"Changing Childbirth"(l 1) placed considerable emphasis on patient choice, therefore a randomised controlled trial was inappropriate. The UK Changing Childbirth initiative was created to increase women's participation in the decision making process relating to pregnancy. All patients who were offered ECV at the North Staffordshire Hospital during the period from July 1995 to June 1997 were recorded in the cohort - 176 in total. The viewpoint chosen was from the secondary care sector.
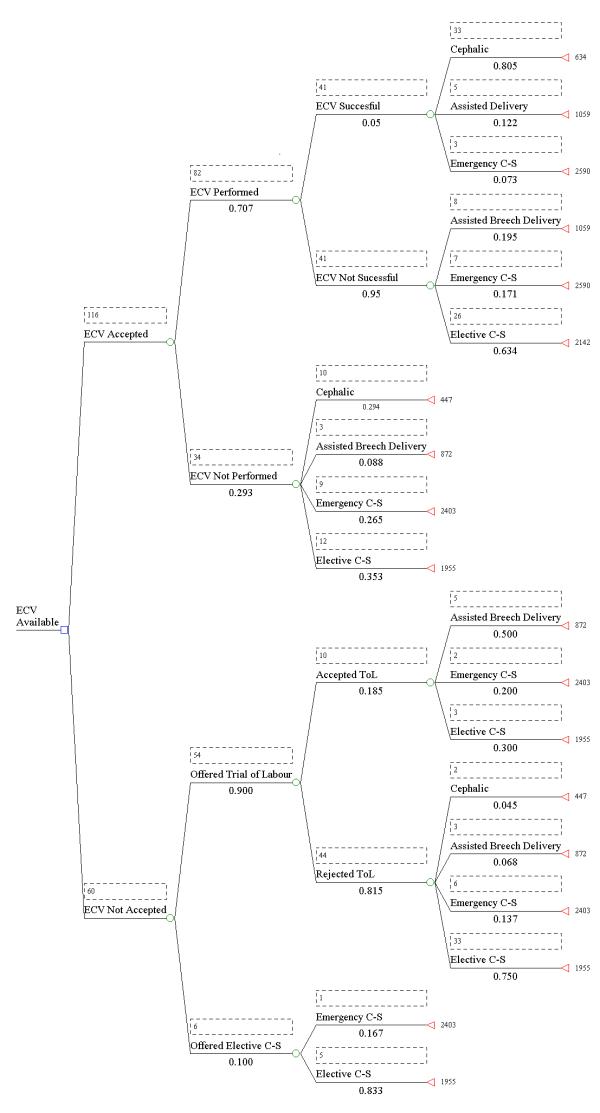
The analysis focused on comparing the cost consequences of "ECV offer accepted" and "ECV offer not accepted." Each event following this decision was plotted on a decision tree using a decision analytical approach. The resulting decision tree is presented in Figure 1.
Figure 1.
ECV Decision Tree
Decision analysis enables the service to be modelled and more importantly structured in a systematic fashion. The decision tree begins with "whether an ECV was successfully performed or not", and for both arms any subsequent interventions such as "whether an assisted delivery was required", or "whether an elective or emergency caesarean was performed" are recorded.
In this analysis the end point is delivery of the baby and the cost of that delivery. No consideration has been made of events beyond that point. The analysis of outcome is presented purely in terms of the cost consequences.
Any number or combination of events may occur in either arm of the decision tree leading to a sequence of events that may include assisted breech birth or result in an emergency caesarean being performed. In practice the five events that occurred were ECV, uncomplicated cephalic delivery, assisted vaginal delivery (breech or cephalic), elective caesarean or emergency caesarean. Each event incurred an attributable cost.
Economics requires the true cost of an intervention to be identified. It is therefore important to fully enumerate the whole process of care and not merely the single intervention. In the case of ECV all that happens to the patient from having an ECV performed or not, to delivery of the baby must be identified and fully costed. Whether for example, they have an uncomplicated ECV or end up having a caesarean section all needs to be costed into the final cost of the programme or the intervention. Economics further requires that the real resources of undertaking an intervention are quantified, that is the physical inputs are identified not merely the monetary value. Costs were calculated for each event based upon the staff, capital and consumables required for each intervention.
With regard to all costs a high and low figure is given depending upon whether the staff performing the intervention are minimum grade staff or higher grade staff. A staff cost per minute was used which included oncost. The actual timings for each procedure were obtained so an accurate cost for staff time could be imputed into the calculations. In all cases the structural breakdown of costs, i.e. the resources used, was gained in interviews with the consultant obstetrician, the senior midwife, the literature and from research at the North Staffordshire Trust. The resources used were enumerated using data from the North Staffordshire Hospital Trust's finance department. Overheads included an allocation to cover light, heating and administration.
The total cost of the two options "ECV accepted" and "ECV not accepted" depends on the probability of each event occurring. This yields a total cost figure for each arm of the decision tree. Probabilities for each event occurring were entered into the decision tree, using data of actual practice between July 1995 and June 1997.
Results
Activity
Figure 1 illustrates from the original 176 patients in the study, the actual number of patients following each branch of the decision tree and the probability associated with each event.
Cost Data
The following presents the costs of each of the five events ECV, uncomplicated cephalic birth, assisted vaginal delivery (breech or ventouse), elective caesarean and emergency caesarean, based on the staff, capital and consumables associated with each event.
Figures are presented based on the minimum grade of staff acceptable to perform an intervention i.e. E grade midwife and senior registrar, and also for higher grade staff, i.e. G grade senior midwife and consultant.
Cost of an ECV
Staff Costs
A doctor and midwife are present during the ECV. The midwife was present for 90 minutes, whilst the doctor was present for 30 minutes. In the low cost scenario this gives staff costs of:
£0.23 per minute * 90 minutes - £20.72 - midwife
£0.43 per minute * 30 minutes - £12.97 - senior registrar
resulting in a total staff cost for the procedure of £33.68
Capital Costs
The procedure is performed at the maternity unit and utilises a delivery suite and a back up operating theatre. Capital costs are included as part of the trust overheads to staff time. The £0.23 per minute midwife cost includes a £0.08 allowance for overheads. Overheads included an allocation to cover light heating and administration.
Specialist equipment also incurs a capital cost. These are as follows: Fetal Monitoring Cardiotacograph (CTG) - cost per minute of £0.26 (£15.88 cost per hour); Ultrasound scan before and after - cost per scan of £50 (£100 for 2). Equipment costs are converted into a unit cost by discounting to an annual equivalent cost and then dividing that figure by the number of units performed per year, i.e. an expected lifespan of 7 years discounted by a rate of 6% per year.
Consumable Costs
Certain items can be used once only or for a single patient, these items are consumables. In ECV the consumables used are: Almond Oil (£0.56) to enable the doctor to manipulate the patient's abdomen, an injection of salbutamol (a tocolytic agent) (£1.35) to relax the patients uterus (drug and syringe), and Saline solution (£3.01) to maintain fluid balance (litre of saline solution, an IV line, and tubes) and swabs (£1.22). This results in a total consumable cost of £6.14.
Other Costs
One additional outpatient appointment at £31.00 is required by all patients receiving an ECV.
To summarise the cost of an ECV is:
Cost of a Normal Vaginal Delivery
The cost of a normal vaginal delivery data has been obtained from a secondary source using work conducted by Clark and co-workers at the John Radcliffe Hospital in Oxford 1991.[12] The figure given is inflated to 1997 prices, to give a cost of £447. The figure has been validated by the North Staffordshire Trusts Finance directorate. It was felt that effort in this study should be concentrate on obtaining the incremental costs of delivery. Ingredient costs were obtained for the ECV, the cost of assisted delivery and the caesarean section. The figures obtained by the Oxford group represent a detailed and generally applicable national baseline cost for normal cephalic birth. It was assumed that this cost would be incurred as a baseline and additional cost for assisted delivery occur and emergency caesarean.
Cost of an Assisted Delivery
The cost of an assisted delivery was the same for both assisted breech delivery or assisted cephalic delivery. Assisted cephalic deliveries at the North Staffordshire Trust are usually performed by the ventouse method. The cost of assisted delivery was an additional incremental cost over and above normal cephalic birth.
Either an assisted breech or ventouse delivery is expected to require: a midwife, a doctor and a nurse practitioner and an anaesthetist on standby. Interventions prior to and following delivery are included in the cost. The cost of failure and second attempts including complications such as maternal tears have been included based upon data from the North Staffordshire Trust. In addition a probabilistic cost of proceeding to caesarean section based upon meta-analysis was added, at a rate of 1.92 %.[13] this is in recognition that this cost may be incurred over and above that of an assisted delivery.
To Summarise the Cost of an Assisted Delivery
Higher staff grades yields a total expected cost of £455.60.
Cost of a Caesarean Section
A caesarean section can either be planned (elective) or unplanned (emergency), the assumption is an elective caesarean section will substitute the costs incurred in a normal vaginal delivery and a emergency caesarean section will be in addition to these costs.
A caesarean section involves: an advanced nurse practitioner, a midwife, a surgeon, an anaesthetist, and an operating theatre orderly. In addition during the recovery period a midwife will be in attendance with the mother on a one-to-one basis.
An operating theatre and recovery area are required. Overhead costs are apportioned on a staff basis.
To Summarise the Cost of an elective Caesarean Section
Allowing for high staff costs this figure becomes £1,992.47
To convert these figures into an emergency caesarean section £447, the vaginal delivery cost, is added.
An emergency caesarean section costs with low grade staff costs £2,403.22 and £2,439.47 with higher grade staff.
Table 1 provides a summary of the cost data for each procedure using low and high estimates of staff costs.
Table 1.
Cost per Procedure
| Low Staff Costs | High Staff Costs | |
|---|---|---|
| External Cephalic Version | £186.70 | £193.30 |
| Assisted Breech/Ventouse Delivery | £425.36 | £455.60 |
| Elective Caesarean Section | £1,955.22 | £1,992.47 |
| Emergency Caesarean Section | £2,403.22 | £2,439.47 |
| Normal Vaginal Delivery | £447.00 | £447.00 |
Inputting the two scenarios for the cost data above into the decision tree yields the following results.
With low staff cost the ECV branch of the decision tree yields an expected cost of £1,452 versus the non ECV branch of £1,828. Hence, to routinely conduct ECV on clinically suitable women with breech presentations results in an expected cost saving of £376 per breech presentation.
Higher staff costs yields an expected cost of £1,479 for the ECV branch of the tree and £1,863 for the non ECV branch of the tree. This converts into a cost saving of £384 per patient. These results are summarised in Table 2.
Table 2.
Summary of the cost implications of routine ECV
| Low Staff Costs | High Staff Costs | |
|---|---|---|
| ECV Offered | £1,452 | £1,479 |
| ECV Not Offered | £1,828 | £1,863 |
| ECV Cost Saving per Patient | £376 | £384 |
The results show that a maternity service in which ECV is routinely offered to patients presenting with a breech birth will be less expensive than a service in which ECV is not offered.
Sensitivity Analysis
Sensitivity analysis allows the key variables in the data to vary to test the reliability of the decision.[14] A threshold analysis was conducted, i.e. an approach whereby key variables are altered up until the point at which the decision would be reversed.
Two key variables were examined: the cost of ECV and the cost of caesarean section.
The first question was " to what must the cost of an ECV rise for the expected value of the ECV branch of the tree to increase to £1,828?" The answer is £718.40. This compares to the calculated ECV cost of £186.70. The cost of an ECV would have to increase by 285% for the conclusions to be reversed.
The second question was "to what must the cost of a caesarean section fall for ECV not offered to become the preferred alternative?" The answer is £856.70, compared to its expected cost of £1,955.22 (elective caesarean section). Hence, a Caesarean section would have to fall in cost by 56% for the conclusions to be reversed. Table 3 presents a summary of threshold values.
Table 3.
Summary of Threshold Values
| Expected Value | Threshold Value | Percentage Change | |
|---|---|---|---|
| External Cephalic Version | £186.70 | £718.40 | 285% |
| Normal Vaginal Delivery | £447 | £1,503.40 | 236% |
| Assisted Delivery | £425.36 | No Threshold | Not Applicable |
| Caesarean Section | £1,955.22 | £856.70 | 56% |
Hence, it can be seen that large scale changes will be required for the original conclusions of the study not to hold true.
Event Probability
It can be seen form the decision tree that once an ECV has been accepted the probability of an ECV being performed is high around 70% of the time. The results reported around whether an ECV is successful could be deemed to be somewhat conservative, with a success rate around 50%. A sensitivity analysis was performed around the success of an ECV. If the rate of successfully performed ECVs increases so to does the cost effectiveness. If, however, the success of an ECV is deemed to fall, the sensitivity analysis showed that the success of an ECV would have to fall to less than 5% for ECV accepted to be a less cost effective option than ECV not accepted.
Discussion
The conclusion of this study is that the use of ECV in the management of women with uncomplicated breech pregnancies at term will yield a cost saving over non ECV options. A key assumption around the whole analysis is that all births are equivalent with regard to neonatal outcome. Successful delivery is taken as the endpoint in this study. The study does not consider the health consequences of ECV nor does it consider a time frame beyond delivery method and associated costs. Given the levels of morbidity associated with caesarean sections[15] it is likely the results of the analysis would only be strengthened by extending the scope and time frame of the work here presented.
Although actual grade of staff subsequently made little difference to total cost of the different options, staffing and the cost of such staff are potentially important to the employing hospital Trust. This analysis shows that although its is possible to substitute a cheaper grade of staff to perform various interventions in obstetrics, this made little difference to the total cost of the care pathways of ECV versus no ECV. The actual resultant procedures in each care pathway are the more important cost drivers.
The results presented showing a potential saving of £376 per ECV per patient, do not yield the same large savings per ECV as those presented by Mauldin of $2462 (£1,501 pounds sterling) per ECV.[16] This difference can largely be explained by the relative costs for ECV, assisted delivery, caesarean section and cephalic birth in the British and American data. The challenge for both health economics and hospital management is to realise these savings in practice. In the case of ECV by avoiding procedures such as caesarean section, it should be possible to save the theatre time and staff, capital and consumable costs associated with this time. Savings in consumable can be realised into real resource savings and theatre time can potentially be used for other procedures.
Table 4 shows the relative costs of each procedure converted to sterling.
Table 4.
American and British Costs per Procedure
| Cost in £ Sterling | ||
|---|---|---|
| Procedure | American Data | British Data |
| Converted from Mauldin 1996 | James 1999 | |
| ECV | 174 | 186 |
| Caesarean Section | 6077 | 1955 |
| Assisted Delivery | 6575 | 425 |
| Cephalic Birth | 3404 | 447 |
It can be seen that whilst the cost of an ECV is approximately the same across the two countries, the cost for the other delivery modes are more expensive in the American data. Hence, any savings accrued from averting each of the procedures would be considerably greater in the American context. In the American context charges for procedures rather than costs are often quoted, caution must be expressed in directly translating savings in the American context into savings in the British context, such results are likely to overestimate true resource savings associated with ECV. The cost of caesarean delivery in the Gifford work is quoted at $10,000 (£6,250)[17] this is some £4,000 more expensive than the British figures reported here and would result in a higher reported financial saving from ECV.
In our study we presented the findings for all cases where ECV had been offered and accepted, or rejected, by the clients and all the subsequent care pathways for both groups. The American data concentrated solely upon those women who had accepted the offer of an ECV and only reported procedures performed following the ECV.[16] The British results are somewhat more conservative than the American. The American work does not consider the important element of patient choice. All eligible women will not by necessity choose ECV and indeed this negates the importance that is rightly attached to patient choice in childbirth.
Within the context of the study a maternity service in which ECV is routinely offered for breech pregnancies at term, will be less expensive per delivery than a maternity service where ECV is not routinely offered. At the same time the service here described preserves the patients right to choose their mode of delivery in childbirth.
Competing interests
None declared
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/content/backmatter/1472-6963-1-6-b1.pdf
Contributor Information
Marilyn James, Email: m.james@keele.ac.uk.
Kevin Hunt, Email: hma13@keele.ac.uk.
Robin Burr, Email: nicola@kogs.freeserve.co.uk.
Richard Johanson, Email: richard@kogs.freeserve.co.uk.
Acknowledgements
The authors would like to thank the West Midlands R&D Directorate, who funded the BOAT Study; Patients, midwives and consultants at the North Staffordshire Hospital who were involved in the study and Nicola Leighton for preparing the manuscript.
References
- Zhang J, Bowes WA, Fortney JA. Efficacy of external cephalic version: a review. Obstet Gynecol. 1993;82(2):306–12. [PubMed] [Google Scholar]
- Pritchard JA, MacDonald PC. Dystocia caused by abnormalities in presentation, position, or development of the fetus. In : Williams Obstetrics. Sixteenth ed. Appleton-Century-Crofts. 1980. pp. 787–96.
- Bingham P, Lilford R. Management of the selected term breech presentation: Assessment of the risks of selected vaginal delivery versus cesarean section for all cases. Obstet Gynecol. 1987;69(6):965–78. [PubMed] [Google Scholar]
- Philipson EH, Rosen MG. Trends in the frequency of cesarean births. Clin Obstet Gynecol. 1985;28(4):691–6. doi: 10.1097/00003081-198528040-00002. [DOI] [PubMed] [Google Scholar]
- Marieskind HI. Cesarean Section in the United States: Has it changed since 1979? Birth. 1989;16(4):196–202. doi: 10.1111/j.1523-536x.1989.tb00898.x. [DOI] [PubMed] [Google Scholar]
- Burr RW, Johanson RB. Breech presentation: Is external cephalic version worthwhile? In : Progress in Obstetrics and Gynaecology. Churchill Livingstone Press. 1996. pp. 87–97.
- Hofmeyr GJ. External cephalic version at term (Cochrane Review) The Cochrane Library.
- Bewley S, Robson SC, Smith M, Glover A, Spencer JAD. The introduction of external cephalic version at term into routine clinical practice. Eur J Obstet Gynecol Reprod Biol. 1993;52:89–93. doi: 10.1016/0028-2243(93)90233-3. [DOI] [PubMed] [Google Scholar]
- RCOG Audit Unit. Effective procedures in obstetrics suitable for audit. RCOG. 1995.
- Johanson RB, Rigby C. Clinical Governance in Practice. J Clin Effectiveness. 1999;1:19–22. [Google Scholar]
- Department of Health Expert Maternity Group. Changing Childbirth. London: HMSO. 1993.
- Clark L, Mugford M, Paterson C. How does the mode of delivery affect the cost of maternity care? Br J Obstet Gynaecol. 1991;98(6):519–23. doi: 10.1111/j.1471-0528.1991.tb10362.x. [DOI] [PubMed] [Google Scholar]
- Johanson RB, Menon V. Vacuum extraction vs forceps delivery (Cochrane Review) The Cochrane Library, Issue 1, 1999.
- Drummond MS, Obrien B, Stoddart GL. Methods for the economic evaluation of health care programmes. 2nd ed. Oxford: Oxford University Press; 1988.
- Hemminki E. Impact of caesarean section of future pregnancy - a review of cohort studies. Paediatric and Perinatal Epidemiology. 1996;10(4):366–79. doi: 10.1111/j.1365-3016.1996.tb00062.x. [DOI] [PubMed] [Google Scholar]
- Mauldin JG, Mauldin PD, Feng TI, Adams EK, Durkalski VM. Determining the clinical efficacy and cost savings of successful external cephalic version. Am J Obstet Gynecol. 1996;175:1639–44. doi: 10.1016/s0002-9378(96)70118-7. [DOI] [PubMed] [Google Scholar]
- Gifford DS, Keeler E, Kahn KL. Reductions in cost and cesarean section rate by routine use of external cephalic version: a decision analysis. Obstet Gynecol. 1995;85:930–6. doi: 10.1016/0029-7844(95)00044-R. [DOI] [PubMed] [Google Scholar]