Abstract
Background
Humeral lengthening by distraction osteogenesis historically has relied on bulky circular external fixators. Advances in fixator technology have allowed for the use of monolateral frames. However, it is unclear whether and to what degree function is improved after humeral lengthening.
Questions/Purposes
We asked: (1) Does humeral lengthening performed with monolateral fixators improve function? (2) Does monolateral external fixation produce comparable restoration of length and complication rate when compared with historical results, using circular external fixation for humeral lengthening?
Methods
We retrospectively reviewed 11 patients who underwent 15 humeral lengthenings with monolateral external fixation. Clinical and radiographic data were collected, including preoperative and postoperative DASH scores as a metric of functional status. The minimum postremoval followup was 14 months (average, 38 months; range, 14–84 months).
Results
Fifteen humeri were lengthened an average of 7 cm (range, 4–9 cm), for a mean lengthening of 41% (range, 23%–52%). Lengthening required an average of 7 months (range, 5–8 months) of fixation, resulting in an external fixation index of 32 days/cm (range, 23–45 days/cm). The major complication rate (three of 15) and postoperative ROM (unchanged at the elbow and improved in seven of 15 shoulders) were comparable to those in previous studies using circular frames. In nine of 15 humeri for which DASH scores were available, the mean preoperative score improved from 14 to 9 after 1 year. The monolateral frame allowed the patient to keep their arm by the side without abducting the shoulder and without impinging the device into the chest wall.
Conclusions
Humeral lengthening with monolateral external fixation is well tolerated by patients and an effective means of improving patient function with a complication rate similar to that for traditional circular frames.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Circular external fixation of the upper extremity is a powerful tool for limb length equalization and deformity correction. Compared with the rich literature in lower extremity limb lengthening, there are relatively few related to upper extremity length equalization [1, 3, 6–9, 11, 14, 15, 22]. Upper extremity length discrepancies are less common than discrepancies of the lower extremities, and are better tolerated by patients when compared with discrepancies in the lower extremities [22]. In some cases upper extremity limb length discrepancy is principally a cosmetic issue [5, 14, 20]; nevertheless, functional limitations from upper extremity limb length discrepancies have been reported [14, 20].
The use of circular external fixation to restore humeral length has been reported in the literature [4, 9, 12, 13]. These series report mean lengthening of 8 to 9 cm with a total duration wearing the frame of 7 to 8 months to restore the upper extremity length discrepancy. They also reported complications including transient radial nerve paresis from 6% to 10%, refracture rate of 10% to 14%, and variable pin tract infection rate after circular external fixation but did not adequately address postoperative functional status. Although circular fixators can restore length, they require patients to abduct their shoulder to maintain clearance between the chest wall and medial aspect of the frame, and the diameter of the device makes clothing difficult. Classic wire-based circular external fixation is further limited by the need for tensioned wires. These wires cross through narrow safe zones and are particularly uncomfortable because of extensive soft tissue tethering. Use of modern monolateral frames in the lower extremity has shown correction of limb length discrepancies and deformity correction to near normal alignment with less patient discomfort [16, 18].
The literature on humeral lengthening with monolateral frames is limited to case reports [10, 17, 21]. These reports suggest that monolateral frames can mostly correct humeral length discrepancies and deformities. However, it is unclear whether and to what degree monolateral frames restore function and how and whether they compare with circular frames in terms of time wearing the device and complications.
We therefore: (1) determined function after humeral lengthening with monolateral external fixation, and (2) compared time spent wearing the frame, length restoration, and complications between a monolateral frame and a circular external fixator.
Patients and Methods
We retrospectively reviewed all 15 patients who had 19 humeri treated with a monolateral frame between 2001 and 2010. We excluded four patients treated but who did not have lengthening with monolateral external fixation for fracture nonunion and acute fracture, and those who underwent initial lengthening elsewhere. These exclusions left 11 patients with 15 lengthenings. The indications for a monolateral frame were: growth arrest caused by osteomyelitis or a tumor, achondroplasia, congenital short humerus, idiopathic short stature, and posttraumatic growth arrest. The contraindication to monolateral fixation would be a complex deformity more accurately and/or safely corrected with circular fixation. The minimum duration of followup after frame removal was 14 months (mean, 38 months; range, 14–84 months). The mean age of the patients was 24 years (range, 8–50 years) with five females and six males. Four of the 11 patients underwent bilateral humeral lengthening. Eight of 15 humeri had angular deformities and length discrepancies. The goal of lengthening in patients with unilateral humeral shortening was a postoperative discrepancy less than 3 cm, as compared with the unaffected side. In patients with bilateral humeral shortening, the goals of lengthening were to restore normal proportions, improve reach, and the ability to perform perineal personal hygiene. No patients were lost to followup. The minimum followup was 14 months (mean, 31 months; range, 14–60 months). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. We had prior institutional review board (IRB) approval.
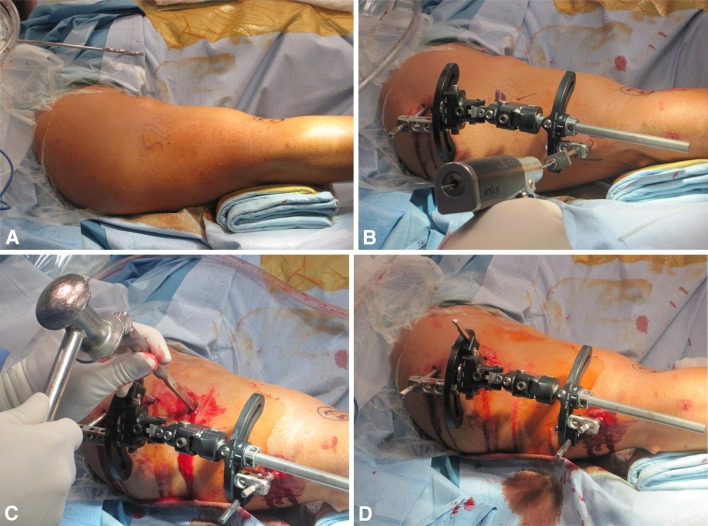
All surgeries were performed by the senior author (SRR). Frames were applied with the patient under regional anesthesia and sedation and supine on a radiolucent table (Fig. 1A). First, a 6-mm hydroxyapatite-coated half pin was inserted proximal to the olecranon fossa and perpendicular to the bone in its center as a distal reference. All half pins in all cases were inserted using fluoroscopic guidance and a cannulated wire technique to avoid neurovascular structures and ensure precise placement (Fig. 1B). During this procedure, an assistant carefully monitored the hand for evidence of nerve stimulation. (Regional anesthesia was used rather than general anesthesia with its associated paralytic agents.) The Biomet® Multi-Axial Correction external fixation system (MAC frame, EBI/Biomet® Trauma, Parsippany, NJ, USA) was used in eight patients, whereas a monolateral rail frame (EBI/Biomet® Trauma) was used in seven patients. The MAC frame is a monolateral frame that allows for multiplanar pin placement. In cases using the MAC frame (eight of 15 humeri), the proximal pins were placed laterally and anterolaterally, whereas the distal pins were placed anterolaterally and posterolaterally to avoid the radial nerve. When using the MAC frame the osteotomy is performed with the frame in place (Fig. 1C). The MAC frame allows for gradual correction of the deformity during the lengthening process. The monolateral frame (seven of 15 humeri) was applied to the distal reference pin, and a proximal pin was inserted using the frame to guide proper alignment. Next, the frame was further secured with an additional pin in the proximal and distal pin clusters (Fig. 1D). The frame then was removed and a percutaneous multiple drill-hole anterolateral osteotomy was performed, just distal to the deltoid tuberosity, taking care to avoid the neurovascular structures. Finally, the frame was reapplied to the pins, the osteotomy was left undisplaced, and the wounds were closed. Patients were mobilized the day after surgery. Active and passive ROM of the elbow was initiated without limitation of range. Shoulder physical therapy consisted of pendulum exercises and passive ROM as tolerated.
Fig. 1A–D.
(A) Positioning and draping for frame application in the operating room is shown. (B) The cannulated drilling technique and (C) technique of the percutaneous osteotomy are shown in these intraoperative photographs. (D) The MAC frame is shown when in place.
Patients were discharged on postoperative Day 3. The frame adjustment started on postoperative Days 7 to 10 at the rate of a quarter turn four times a day for a total rate of 1 mm/day until the length goals were obtained. Electrical bone stimulation (EBI/Biomet®) was used in all cases as part of our typical postoperative care. Supervised physical therapy was advised but patients also engaged in a home program consisting of 15 repetitions four times per day. Active motion of the shoulder was initiated at 2 months. Resistance strengthening exercises including curls using dumbbells and wall pushups were started at 4 months.
Patients were followed every 2 weeks through lengthening, monthly during consolidation until removal, and biannually until the regenerate was fully healed, at which point patients were seen as needed. Preoperative and postoperative function were quantified using the DASH score [2]. The DASH outcome measure is a 30-item, self-report questionnaire designed to measure physical function and symptoms in people with musculoskeletal disorders of the upper limb. The DASH score has two components: the disability/symptom section (30 items, scored 1–5) and the optional high performance Sport/Music or Work section (four items, scored 1–5) [2].We did not administer the optional modules of the DASH measure because they increase patient burden and were not deemed relevant. Demographics including age, sex, etiology of deformity, device used (Table 1), and clinical features including duration of treatment, amount of lengthening, correction of deformity, shoulder and elbow ROM, and DASH scores were collected by chart review (Table 2). Special attention was paid to collecting adverse events during treatment, including pin tract infections, radial nerve injury, refracture, and/or stiffness of the shoulder and the elbow. Adverse events were categorized using Paley’s classification system as problems, obstacles, or complications [19].
Table 1.
Patient demographics
| Patient number | Humeri number | Side | Etiology | Age (years) | Technique |
|---|---|---|---|---|---|
| 1 | I | Right | Achondroplasia | 13 | Rail |
| II | Left | ||||
| 2 | III | Right | Achondroplasia | 12 | MAC |
| IV | Left | ||||
| 3 | V | Right | Ollier’s disease | 8 | MAC |
| VI | Left | ||||
| 4 | VII | Right | Ollier’s disease | 36 | MAC |
| VIII | Left | ||||
| 5 | IX | Right | Unicameral bone cyst | 17 | MAC |
| 6 | X | Left | Childhood growth arrest | 50 | Rail |
| 7 | XI | Right | Resection of malignant bone tumor | 13 | Rail |
| 8 | XII | Right | Childhood growth arrest | 31 | Rail |
| 9 | XIII | Left | Growth arrest as a result of septic arthritis | 36 | Rail |
| 10 | XIV | Left | Posttraumatic growth arrest | 34 | MAC |
| 11 | XV | Left | Childhood growth arrest | 39 | MAC |
MAC = Biomet® Multi-Axial Correction external fixation system.
Table 2.
Results and functional outcomes
| Patient number | Humeri number | EFI (days/cm) | Lengthening (%) | Adverse events (Paley classification [19]) | Preoperative DASH scores | DASH score after frame removal |
|---|---|---|---|---|---|---|
| 1 | I | 23 | 56 | |||
| II | 23 | 56 | ||||
| 2 | III | 39.9 | 57 | 15.74 | 2.77 | |
| IV | 39.9 | 57 | 15.74 | 2.77 | ||
| 3 | V | 30 | 35 | Pin tract infection (problem) | 2.73 | 2.58 |
| VI | 30 | 17 | 2.73 | 2.58 | ||
| 4 | VII | 23 | 31 | 2.5 | 2.7 | |
| VIII | 25 | 29 | Refracture (obstacle); pin tract infection (problem) | 2.5 | 2.9 | |
| 5 | IX | 26 | 33 | Pin tract infection (problem) | ||
| 6 | X | 28 | 42 | Radial nerve palsy (obstacle) | 7.5 | 1.66 |
| 7 | XI | 40 | 47 | Refracture (obstacle); radial nerve palsy (problem) | 42.5 | 26.66 |
| 8 | XII | 45 | 42 | |||
| 9 | XIII | 45 | 38 | |||
| 10 | XIV | 30 | 38 | |||
| 11 | XV | 30 | 32 | 34.82 | 33.92 | |
| Mean | 32 | 41 | 14.08 | 8.72 | ||
| Difference of means | 5.36; SD = 6 .75; p = .04 | |||||
EFI = external fixation index.
AP and lateral radiographs of both upper extremities were available for all patients at each visit. After calibrating each image in the PACS viewer, the length and angular deformity of both humeri were measured in the sagittal and coronal planes. Percentage lengthening was calculated as distraction length or preoperative measured bone length. The external fixation index (EFI) was calculated by dividing the total number of days wearing the frame by the amount of lengthening achieved in centimeters (days wearing frame/cm lengthened).
PubMed, Medline, and Google Scholar were searched for suitable historical control reports on humeral lengthening. Search criteria such as ‘Humeral lengthening’ were used to identify 158 initial articles. The Boolean “and” and “or” were used to do an expanded search on ‘humeral lengthening and external fixation or deformity correction’. Finally three case series on humeral lengthening with external fixation were identified and all were included as controls (Table 3) [4, 9, 12]. The results of these control studies were aggregated using means weighted by the number of humeri in each study. The aggregate weighted mean was used as a summary of the historical controls for easier comparison with our results. The preoperative and postoperative (1 year after frame removal) DASH scores were obtained for nine patients and the data were compared using a two-tailed paired sample t-test. The distribution of preoperative to postoperative DASH scores met the assumption of normality necessary for parametric statistical testing (skewness statistic = −0.68, standard error of skewness = 0.71). All analyses were performed with SPSS® Statistics 20 (SPSS Inc, Chicago, IL, USA).
Table 3.
Comparison with historical controls
| Parameters | Kashiwagi et al. [12] | Cattaneo et al. [4] | Hosny [9] | Humeri weighted control means | Current study |
|---|---|---|---|---|---|
| Humeri lengthened | 20 | 43 | 16 | 26. | 15 |
| Number of patients | 10 | 29 | 16 | 11 | |
| Age of patients (years) | 13 | 18 | 13 | 16 | 24 |
| Operative technique | Ilizarov | Ilizarov | Hybrid | Monolateral | |
| Mean lengthening (cm) | 8 | 9 | 9 | 9 | 7 |
| Fixation time (months) | 7 | 8 | 8 | 8 | 7 |
| EFI (days/cm) | 30 | 27 | 28 | 28 | 32 |
| Pin tract infection (patients) | N/A | 6 | All patients | N/A | 2 |
| Transient radial nerve paralysis | 10% (n = 2) | 7% (n = 3) | 6% (n = 1) | 8% (n = 6) | 13% (n = 2) |
| Stiffness of elbow (patients) | 0 | 3 | 0 | 0 | |
| Refractures | 10% (n = 2) | 16% (n = 7) | 13% (n = 2) | 14% (n = 11) | 13% (n = 2) |
| Shoulder ROM (patients) | N/A | 3 decreased | No changes | 7 improved 8 unchanged | |
| Elbow ROM (patients) | No changes | 3 decreased | No changes | No changes | |
| Lengthening | 50% | N/A | N/A | 41% | |
| Deformity correction | None | N/A | None | 8 fully corrected |
N/A = not assessed; EFI = external fixation index.
Results
Humeral lengthening improved function. The mean preoperative DASH score was 14 (range, 3–43), which improved (p = 0.04) by 5 to 9 (range, 2–34) at followup 1 year after frame removal (Table 2). At 1 year followup all patients were free of shoulder and elbow stiffness (Table 3). This was an improvement in ROM in seven arms which were stiff preoperatively and a preservation of full baseline motion in the remaining eight arms.
Humeral lengthening using monolateral external fixation yielded EFIs, radial nerve paralysis and regenerate refracture rates, and ROM comparable to those previously reported using circular external fixation (Table 3). The mean lengthening in this series was 7 cm (range, 4–9 cm), which required an average of 7 months (range, 5–8 months), resulting in an EFI of 32 days/cm (range, 23–45 days/cm). Although statistical comparison is not appropriate, these results were clinically comparable to those of the historical control studies [4, 9, 12]. The aggregated mean, weighted by humeri lengthening in the control studies, was 9 cm (range, 8–9 cm), which required an average of 8 months (range, 7–8 months), resulting in an EFI of 28 days/cm (range, 27–30 days/cm). In this series two of 15 patients had refractures (rate, 0.13); this was comparable to the historical control trials in which 11 of 79 patients had refractures (rate, 0.14) (Table 3). One of the two refractures (Patient 7), however, occurred after lengthening of a vascularized fibular graft. This suggested that monolateral fixation had a similar or potentially lower refracture rate in routine use. Although eight of 15 humeri in this series lengthened with monolateral fixation had concurrent deformity correction, none of the 36 humeri reported in two of the historical control papers that addressed deformity had concurrent correction. Transient radial nerve paralysis occurred in six of 79 control lengthenings (rate, 0.08 paralysis/humeri) and two of 15 lengthenings in this series (rate, 0.13 paralysis/humeri). Whether this represented a real difference in transient radial nerve paralysis was unclear, given the small sample size and presence of complex angular deformity in eight of 15 patients in this series. In all cases normal radial nerve function was regained.
Patients 3, 4, and 5 had superficial pin tract infections that resolved with oral antibiotics (Table 2). Patients 6 and 7 had transient radial nerve palsy that presented as numbness of the middle finger or forearm. These were treated by relocating a half pin and continuing lengthening (Patient 6) or watchfully waiting after planned removal (Patient 7). Both patients recovered fully within 4 weeks. Patients 4 and 7 had refractures through the regenerate shortly after frame removal. Patient 4 was treated with reapplication of the frame for an additional 3 months. Patient 7’s refracture occurred through regenerate, formed by lengthening a vascularized fibular graft and treated with open reduction and internal fixation with a 12-hole locked small fragment plate (Synthes®, Paoli, PA, USA). Followup radiographs showed a united fracture site and hypertrophy of the previously narrow regenerate. These adverse events resulted in a stratified adverse event rate of four problems, three obstacles and no true complications in 15 humeri (Table 2).
Discussion
The literature on humeral lengthening was generally sparse, but particularly so when one considers improvements in frame design. The largest existing case series [4, 9, 12] used traditional circular external fixation, which is uncomfortable for patients when used on the proximal upper extremity. Monolateral frames offered obvious advantages from a patient comfort standpoint [16, 18]; however, the essential literature for clinical decision making, that reporting the safety and efficacy of these constructs to traditional circular designs, was limited to case reports [10, 21]. Additionally it is unclear whether and to what degree lengthening restores function and how and whether monolateral frames compare with circular frames in terms of time wearing the device and complications. We therefore: (1) determined function after humeral lengthening with monolateral external fixation, and (2) compared time wearing the frame, length of restoration, and complications between a monolateral frame and a circular external fixator.
This retrospective case series was not without limitations. First, the sample was small and heterogeneous when compared with series on more common conditions. Second, because the DASH scores were not collected as part of a prospective trial, they were not available for all patients. Although it is essential that our conclusions be viewed through the lens of these limitations we believe our data are sufficiently representative to accept the resultant conclusions pending further study. A prospective study quantifying functional outcome after upper extremity limb length equalization could add to the results reported here. Such an effort would be aided by validated measures of functional impairment arising from limb length discrepancy. Finally, because all surgeries were performed at a subspecialty orthopaedic hospital with expert anesthesiologists, all the patients received regional anesthesia with intraoperative monitoring. The rate of radial nerve injury may not be generalizable to facilities that do not provide intraoperative monitoring.
Our study replicated the finding of functional improvement after humeral lengthening with a MAC frame described in a previous case report [21] and extended it into a larger case series. Additionally, this study was a replication of large historical case series showing the safety and efficacy of humeral lengthening (Table 3), but it expands on those studies by reflecting modern frame design and including a validated functional end point, the DASH score [2]. That end point suggested that patients undergoing large (mean, 7 cm) humeral lengthenings experience improvements in function of 5 points as assessed by DASH score (Table 2) at 1 year. We believe the functional improvement arises from better reach for patients with bilateral shortening and near restoration of length in patients with unilateral humeral shortening. Patients frequently cite the ability to reach their perineum, and thus use the bathroom independently, as an important functional gain arising from lengthening. Deformity correction also restores the anatomic and mechanical axis of the upper extremity and thus contributes to these functional improvements.
Although historical controls reported occasional shoulder or elbow stiffness as a complication in 7% of patients [4], we observed no elbow or shoulder stiffness and occasionally observed shoulder motion improvement. This improvement may have reflected advances in physical therapy or frame design. We believe the less limited postoperative ROM may have reflected the reduced burden of transverse fixation around the shoulder and elbow, associated with monolateral frames built with half pins as compared with circular frames typically built with wires and/or half pins. It is also possible that the less cumbersome monolateral frame simply allowed for more normal limb use during treatment.
Our rate of transient radial nerve symptoms was similar to that of the historical control studies (two of 15 versus six of 79). One of our two patients (Patient 7) had a transient radial nerve palsy develop after refracture of a regenerate formed by lengthening a free fibular graft. Both of these patients were treated using a monolateral rail and both achieved complete resolution. As compared with wire-based circular frames, half-pin-based monolateral frames require fewer points of fixation in a region constrained by neurovascular structures. The modularity of the MAC frame offered some additional advantages over other rails. The standard monolateral rail required acute correction of the deformity and linear placement of the half pins, whereas the MAC frame system allowed pin clusters to be cantilevered off the frame, using arches, into anatomically safer positions and gradual correction of coronal and sagittal plane deformities by placing a hinge at the osteotomy site. Regardless of frame selection, the risk of radial nerve involvement could be reduced by placing the proximal half pins laterally and anterolaterally, and the distal pins anterolaterally and posterolaterally. We do this using fluoroscopic guidance and a cannulated wire technique with an assistant monitoring the hand for evidence of radial nerve stimulation.
Humeral lengthening and deformity correction with the Ilizarov method is difficult for the patient and surgeon and has real but mitigatable risks [4, 9, 12]. Our findings mirror those of previous studies and extended them by documenting postoperative functional improvement as measured by the DASH score. The severity and frequency of adverse events and restoration of humeral length observed in this series were comparable to those reported for circular frames. Armed with evidence of parity between monolateral and circular frames on these key end points, we are more confident using the frame design which is less difficult for patients in our experience. Future studies should more rigorously quantify the patient experience during and functional impact of humeral lengthening.
Acknowledgments
We acknowledge the administrative assistance of Eugene Borst for making this project possible.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aldegheri R, Dall’Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B. 2001;10:238–247. [PubMed] [Google Scholar]
- 2.Beaton DE, Wright JG, Upper Extremity Collaborative Group Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 3.Cattaneo R, Catagni MA, Guerreschi F. Applications of the Ilizarov method in the humerus: lengthenings and nonunions. Hand Clin. 1993;9:729–739. [PubMed] [Google Scholar]
- 4.Cattaneo R, Villa A, Catagni MA, Bell D. Lengthening of the humerus using the Ilizarov technique: description of the method and report of 43 cases. Clin Orthop Relat Res. 1990;250:117–124. [PubMed] [Google Scholar]
- 5.Dal Monte A, Andrisano A, Manfrini M, Zucchi M. Humeral lengthening in hypoplasia of the upper limb. J Pediatr Orthop. 1985;5:202–207. [PubMed] [Google Scholar]
- 6.Damsin JP, Ghanem I. Upper limb lengthening. Hand Clin. 2000;16:685–701. [PubMed] [Google Scholar]
- 7.Dick HM, Petzoldt RL, Bowers WR, Rennie WR. Lengthening of the ulna in radial agenesis: a preliminary report. J Hand Surg Am. 1977;2:175–178. doi: 10.1016/s0363-5023(77)80067-1. [DOI] [PubMed] [Google Scholar]
- 8.Dick HM, Tietjen R. Humeral lengthening for septic neonatal growth arrest: case report. J Bone Joint Surg Am. 1978;60:1138–1139. [PubMed] [Google Scholar]
- 9.Hosny GA. Unilateral humeral lengthening in children and adolescents. J Pediatr Orthop B. 2005;14:439–443. doi: 10.1097/01202412-200511000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Ilizarov S, Blyakher A, Rozbruch SR. Lengthening of a free fibular graft after sarcoma resection of the humerus. Clin Orthop Relat Res. 2007;457:242–246. doi: 10.1097/BLO.0b013e31802c7932. [DOI] [PubMed] [Google Scholar]
- 11.Janovec M. Short humerus: results of 11 prolongations in 10 children and adolescents. Arch Orthop Trauma Surg. 1991;111:13–15. doi: 10.1007/BF00390185. [DOI] [PubMed] [Google Scholar]
- 12.Kashiwagi N, Suzuki S, Seto Y, Futami T. Bilateral humeral lengthening in achondroplasia. Clin Orthop Relat Res. 2001;391:251–257. doi: 10.1097/00003086-200110000-00029. [DOI] [PubMed] [Google Scholar]
- 13.Katz K, Goldberg I, Bahar A, Yosipovitch Z. Humeral lengthening for septic neonatal growth arrest. J Hand Surg Am. 1989;14:903–907. doi: 10.1016/S0363-5023(89)80100-5. [DOI] [PubMed] [Google Scholar]
- 14.Lee FY, Schoeb JS, Yu J, Christiansen BD, Dick HM. Operative lengthening of the humerus: indications, benefits, and complications. J Pediatr Orthop. 2005;25:613–616. doi: 10.1097/01.bpo.0000164868.97060.bb. [DOI] [PubMed] [Google Scholar]
- 15.Liu T, Zhang X, Li Z, Zeng W, Peng D, Sun C. Callus distraction for humeral nonunion with bone loss and limb shortening caused by chronic osteomyelitis. J Bone Joint Surg Br. 2008;90:795–800. doi: 10.2106/JBJS.H.00626. [DOI] [PubMed] [Google Scholar]
- 16.McCarthy JJ, Ranade A, Davidson RS. Pediatric deformity correction using a multiaxial correction fixator. Clin Orthop Relat Res. 2008;466:3011–3017. doi: 10.1007/s11999-008-0491-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLawhorn AS, Sherman SL, Blyakher A, Widmann RF. Humeral lengthening and deformity correction with the multiaxial correction system. J Pediatr Orthop B. 2011;20:111–116. doi: 10.1097/BPB.0b013e328341bc87. [DOI] [PubMed] [Google Scholar]
- 18.Noonan KJ, Leyes M, Forriol F, Cañadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation: a study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998;80:793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 20.Peterson HA. Surgical lengthening of the humerus: case report and review. J Pediatr Orthop. 1989;9:596–601. doi: 10.1097/01241398-198909010-00017. [DOI] [PubMed] [Google Scholar]
- 21.Tellisi N, Ilizarov S, Fragomen AT, Rozbruch SR. Humeral lengthening and deformity correction in Ollierʼs disease: distraction osteogenesis with a multiaxial correction frame. J Pediatr Orthop B. 2008;17:152–157. doi: 10.1097/BPB.0b013e3282f548dc. [DOI] [PubMed] [Google Scholar]
- 22.Tetsworth K, Krome J, Paley D. Lengthening and deformity correction of the upper extremity by the Ilizarov technique. Orthop Clin North Am. 1991;22:689–713. [PubMed] [Google Scholar]