Abstract
Background
Computer navigation has improved accuracy and reduced the percentage of alignment outliers in TKA. However, the characteristics of outliers and the risk factors for limb malalignment after TKA are still unclear.
Questions/Purposes
We therefore addressed the following questions: (1) What is the incidence and characteristics of outliers for postoperative limb mechanical axis (hip-knee-ankle [HKA] angle outside the conventional 180° ± 3° range) and component alignment in TKA? And (2) what are the preoperative clinical or radiographic risk factors for limb mechanical axis malalignment in TKA?
Methods
We retrospectively reviewed the clinical and radiographic records of 1500 computer-assisted TKAs to identify outliers for postoperative HKA axis and component alignment and determined risk factors for malalignment. Full-length hip-to-ankle and knee radiographs were used to measure preoperative HKA angle, femoral coronal bowing, joint divergence angle, tibial subluxation, and tibial bone loss and postoperative HKA angle and femoral and tibial component angle.
Results
The incidence of outliers for postoperative limb mechanical axis, femoral component alignment, and tibial component alignment was 7% (112 of 1500 TKAs), 7%, and 8%, respectively, with 70% of limbs placed in excessive varus and 30% in excessive valgus. Preoperative varus deformity of more than 20° and femoral bowing of more than 5° were associated with increased risk of placing the limb mechanical axis outside the acceptable ± 3° range after computer-assisted TKA.
Conclusions
The presence of preoperative radiographic risk factors should alert the surgeon to increased chance of malalignment and every measure should be undertaken in such at-risk knees to ensure proper limb and component alignment and soft tissue balance.
Level of Evidence
Level II, prognostic study. See Instructions for Authors for a complete description of levels of evidence
Introduction
Several reports have emphasized the importance of restoring accurate alignment after TKA and the greater risk of implant failure with malalignment [6, 12, 23]. Ritter et al. [23] in a recent radiographic analysis of more than 6000 TKAs at a minimum followup of 2 years reported failure was most likely if the tibial or femoral component was placed outside the acceptable limit with respect to the tibial and femoral axes on short knee films.
Computer navigation has facilitated more accurate component placement and limb alignment restoration after TKA [5, 7, 9]. In three recent meta-analyses of randomized controlled trials comparing navigated versus conventional TKAs [5, 7, 9], 1119 to 2268 navigated TKAs from 21 to 41 trials were analyzed. They reported patients who underwent navigated TKA had a lower risk of limb and implant malalignment at more than 3° with respect to the mechanical axis and an outlier rate of 12% to 13% for the limb mechanical axis. Despite the accuracy, individual studies have reported an outlier rate of 0% to 29% with navigated TKA for limb mechanical axis [16, 17, 24, 28, 29]. This wide variation may be due to the small number of navigated knees (ranging from 32 to 282) included in most of these studies and the fact that most of these cases were part of an early series where surgeon experience might have played a role in the alignment outcome. Furthermore, none of these studies have analyzed the causes or risk factors for malalignment. Few [17, 24, 28] have attributed malalignment to reasons such as error during bone cuts, error during registration, displacement of the infrared arrays during the procedure, and errors that occur during obtaining and measuring postoperative radiographs.
We therefore addressed the following questions: (1) What is the incidence and characteristics of outliers for postoperative limb mechanical axis (hip-knee-ankle [HKA] angle outside the acceptable range of 180° ± 3°) and component alignment in TKA? And (2) what are the preoperative clinical or radiographic risk factors for limb mechanical axis malalignment in TKA?
Patients and Methods
We retrospectively reviewed the clinical and radiographic records of 1590 primary TKAs performed by the senior author (ABM) from 2005 to 2010. We included all primary TKAs performed for knee arthritis secondary to primary osteoarthritis, rheumatoid arthritis, or posttraumatic arthritis. We excluded patients whose radiographic records were incomplete for analysis (90 TKAs), leaving 1500 TKAs performed in 1196 patients (245 men, 951 women) for analysis. We used clinical records to obtain demographic details, including age, sex, BMI, and preoperative diagnosis (Table 1). A total of 226 knees (15%) had incomplete records to derive BMI and were therefore omitted for analysis of this variable. The primary diagnosis was osteoarthritis in 1460 knees, rheumatoid arthritis in 38 knees, and posttraumatic arthritis in two knees. One hundred seventeen knees (8%) had valgus deformity and 1383 knees (92%) had varus deformity preoperatively. A vast majority of knees (90%) had a combination of osteoarthritis with preoperative varus deformity whereas a small part of the knees (0.5%) had rheumatoid arthritis with preoperative valgus deformity (Table 2). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
Table 1.
Demographic data of the study population
| Parameter | Value |
|---|---|
| Number of TKAs/patients | 1500/1196 |
| Age (years)* | 67 ± 8 (39–94) |
| BMI* | 30 ± 5 (15–54) |
| Sex (number of patients) | |
| Male | 245 |
| Female | 951 |
| Diagnosis (number of knees) | |
| Osteoarthritis | 1460 |
| Rheumatoid arthritis | 38 |
| Posttraumatic arthritis | 2 |
| Procedure (number of patients) | |
| Unilateral | 892 |
| Simultaneous/staged bilateral | 304 |
* Values are expressed as mean ± SD, with range in parentheses.
Table 2.
Outlier rate for postoperative HKA axis and femoral and tibial component alignment in groups based on preoperative diagnosis and type of deformity
| Groups | Number of knees | Outliers for HKA axis | Outliers for femoral component alignment | Outliers for tibial component alignment | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | > 3° varus | > 3° valgus | Total | > 3° varus | > 3° valgus | Total | > 3° varus | > 3° valgus | ||
| OA varus | 1353 | 100 | 60 (60%) | 40 (40%) | 87 | 40 (46%) | 47 (54%) | 107 | 28 (26%) | 79 (74%) |
| OA valgus | 107 | 7 | 1 (14%) | 6 (86%) | 9 | 3 (33%) | 6 (67%) | 13 | 1 (8%) | 12 (92%) |
| RA varus | 28 | 4 | 3 (75%) | 1 (25%) | 4 | 1 (25%) | 3 (75%) | 4 | 2 (50%) | 2 (50%) |
| RA valgus | 10 | 1 | 1 (100%) | 0 | 1 | 0 | 1 (100%) | 0 | 0 | 0 |
| Total | 1498 | 112 | 65 | 47 | 101 | 44 | 57 | 124 | 31 | 93 |
HKA = hip-knee-ankle; OA = osteoarthritis; RA = rheumatoid arthritis.
All TKAs were performed by one surgeon (ABM) using the image-free Ci Navigation System (Brainlab AG, Munich, Germany). All procedures were performed with the tourniquet inflated using an anterior longitudinal incision and a medial parapatellar arthrotomy. All patients underwent TKA using a cemented, posterior cruciate-substituting design and all patients had resurfacing of the patella. During navigation, registration was performed in the standard fashion using proximal tibial and distal femoral arrays to which three reflector spheres were affixed. The mechanical axis of the lower limb was obtained by navigation, using the center of femoral rotation, the center of the intercondylar notch, and the center of the ankle plafond (defined as the midpoint between the outermost prominence of the medial and the lateral malleolus). Cutting blocks were navigated into position to perform the appropriate bone cuts where the tibial and femoral cuts were performed at 90° relative to their mechanical axes in the coronal plane and the tibial slope and femoral flexion at approximately 3° with respect to their mechanical axes in the sagittal plane. The degree of soft tissue release was governed by the amount of soft tissue tightness assessed using a tensioning device and medial and lateral gap imbalance as quantified by navigation. Medial release for varus knees and lateral release for valgus knees were performed to achieve rectangular balanced gaps and a fully restored mechanical axis.
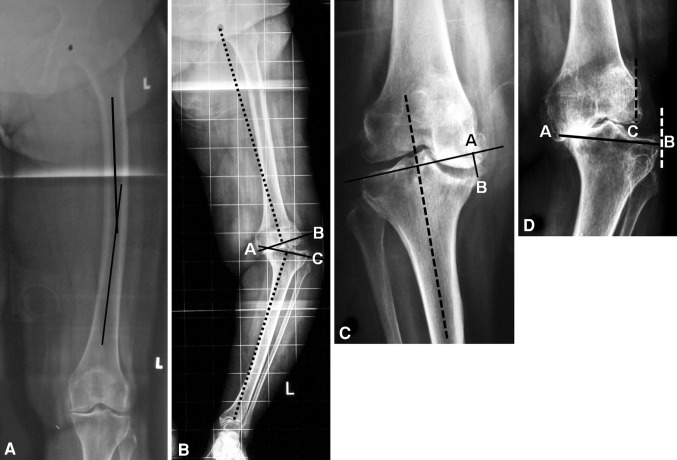
One of the authors (GMS) screened all full-length radiographs before analysis for excessive rotation of the limb or improper exposure, which may make the radiograph unsuitable for analysis. To determine excessive rotation of the limb on radiographs, the appearance of the lesser trochanter and the fibular head profile were used as landmarks. Radiographs that showed one of these two profiles in excess meant the limb was malrotated and those limbs were excluded from the study. Angles measured on full-length hip-to-ankle radiographs are reportedly reliable [25]. Hence, two of us (APL, SB), who had not operated on any of the patients from this study, performed the radiographic assessment using pre- and postoperative full-length standing hip-to-ankle and standing AP and lateral radiographs. The radiographs taken preoperatively and at latest followup were used for analysis in this study. All digital radiographic images were analyzed using ImageJ image processing and analysis software (Version 1.41; NIH, Bethesda, MD, USA). The degree of pre- and postoperative knee deformity or HKA angle was determined on the standing full-length radiographs as the angle between the mechanical axis of the femur (center of the femoral head to the center of the knee) and the mechanical axis of the tibia (center of the knee to the center of the ankle plafond). Postoperatively, coronal alignment of femoral and tibial components was measured using their respective mechanical axes on full-length radiographs. We also analyzed radiographs to determine the following parameters (Fig. 1): (1) amount of femoral shaft bowing in the coronal plane measured by the method described by Yau et al. [27], with angulation of more than 5° considered clinically important; (2) amount of lateral or medial soft tissue laxity in a varus or valgus knee as determined by the joint divergence angle (JDA), which was the angle made by the distal femur and proximal tibial joint lines plotted perpendicular to the femoral and tibial mechanical axes; (3) depth of medial or lateral tibial bone defect as determined by the method described by Aglietti et al. [1]; and (4) amount of lateral or medial subluxation of the tibia.
Fig. 1A–D.
(A) Femoral bowing in the coronal plane is measured on a full-length hip-to-ankle radiograph as the angle made by the middiaphyseal lines of the proximal ½ and distal ½ of the femoral shaft. (B) JDA (Angle BAC) is measured as the angle made by the distal femur and proximal tibial cuts (solid lines) plotted perpendicular to the femoral and tibial mechanical axes (dotted lines). (C) Depth of tibial bone loss (Distance AB) is measured on standing knee AP radiographs as the distance between the tangential line (solid line) drawn to the top of the intact lateral tibial plateau perpendicular to the proximal tibial mechanical axis (dotted line) and the lowest point of the defect. (D) Amount of tibial subluxation is measured as a percentage of the distance between the lateral-most point of the distal femoral condyle to the lateral-most point of the tibial condyle (Distance CB) with respect to the mediolateral length of the tibial plateau at the level of the articular surface (Distance AB), ie, amount of tibial subluxation = Distance CB × 100/Distance AB.
Limbs with a postoperative HKA angle outside the conventional ± 3° range from a neutral alignment of 180° were considered outliers for limb alignment. Similarly, components outside the conventional ± 3° range from a neutral alignment of 90° in the coronal plane were considered outliers for component alignment. To determine the pattern of outliers for limb mechanical axis, we analyzed them further to determine the number of limbs in excessive postoperative varus or valgus in the subgroups based on the type and severity of preoperative knee deformity. Among the outliers for limb alignment, the number of tibial and femoral components that were malaligned was also determined.
For statistical analysis, we subgrouped demographic and radiographic parameters as follows: age at surgery (< 60 years, 60–70 years, > 70 years), BMI (< 30, ≥ 30), preoperative knee deformity (< 10° varus, 10°–20° varus, > 20° varus, < 10° valgus, > 10° valgus), amount of femoral shaft bowing (≤ 5°, > 5°), JDA (≤ 15°, > 15°), depth of tibial bone loss (≤ 20 mm, > 20 mm), and tibial subluxation (≤ 20%, > 20%). The chi-square test was used for comparison between groups during bivariate analysis. Demographic and radiographic factors found to be significant for unacceptable postoperative limb mechanical alignment on bivariate analysis (Table 3) were then included in a multivariate logistic regression analysis to analyze the effect of each significant factor adjusted for others (keeping other variables constant). An odds ratio for the increased chance of limb malalignment was calculated for all risk factors from the multivariate analyses.
Table 3.
Risk factors for postoperative limb mechanical axis alignment (bivariate analysis)
| Risk factor | Number of knees | p value | ||
|---|---|---|---|---|
| Total | Nonoutliers | Outliers | ||
| Age | 0.83 | |||
| < 60 years | 293 (19%) | 274 (20%) | 19 (17%) | |
| 60–70 years | 721 (49%) | 667 (48%) | 54 (48%) | |
| > 70 years | 486 (32%) | 447 (32%) | 39 (35%) | |
| Sex | 0.43 | |||
| Male | 223 (15%) | 203 (14.6%) | 20 (18%) | |
| Female | 1277 (85%) | 1185 (85.4%) | 92 (82%) | |
| BMI | 0.05 | |||
| < 30 | 750 (59%) | 725 (59%) | 25 (46%) | |
| ≥ 30 | 524 (41%) | 495 (41%) | 29 (54%) | |
| Severity of preoperative knee deformity | < 0.001 | |||
| Varus < 10° | 519 (37.5%) | 485 (37.9%) | 34 (33%) | |
| Varus 10°–20° | 712 (51.5%) | 668 (52.3%) | 44 (42.7%) | |
| Varus > 20° | 150 (11%) | 125 (8.5%) | 25 (16.5%) | |
| Valgus < 10° | 76 (64%) | 70 (63.6%) | 6 (66.7%) | |
| Valgus > 10° | 43 (36%) | 40 (36.4%) | 3 (33.3%) | |
| Femoral bowing | < 0.001 | |||
| ≤ 5° | 1375 (91.7%) | 1283 (92.4%) | 92 (82.1%) | |
| > 5° | 125 (8.3%) | 105 (7.6%) | 20 (17.9%) | |
| Joint divergence angle | 0.002 | |||
| ≤ 15° | 816 (61.2%) | 768 (62.4%) | 48 (46.6%) | |
| > 15° | 518 (38.8%) | 463 (37.6%) | 55 (53.4%) | |
| Tibial bone loss | < 0.001 | |||
| ≤ 20 mm | 1455 (97%) | 1354 (97.6%) | 101 (90.2%) | |
| > 20 mm | 45 (3%) | 34 (2.4%) | 11 (9.8%) | |
| Tibial subluxation | 0.01 | |||
| ≤ 20% | 1364 (90.9%) | 1269 (91.4%) | 95 (84.8%) | |
| > 20% | 136 (9.1%) | 119 (8.6%) | 17 (15.2%) | |
Results
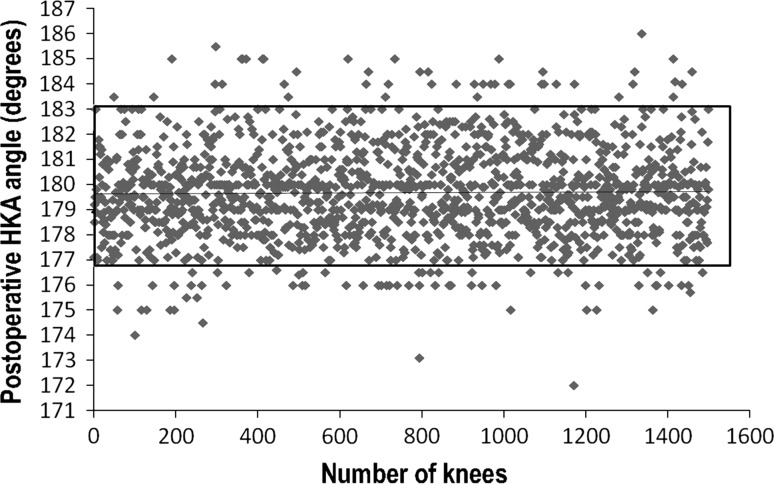
Among the 1500 TKAs analyzed, 112 knees (7%) in 109 patients were outliers for postoperative limb mechanical axis (Fig. 2). Sixty-five of these limbs (58%) were in excessive varus alignment and 47 limbs were in excessive valgus alignment. Postoperative limb malalignment was 5° or less in 107 limbs (96%) and greater than 5° in five limbs (two limbs in 5.1°–6° varus, one limb in > 6° varus, one limb in 6° valgus). A majority of the outliers in limbs with preoperative varus deformity (60%) were in excessive varus, implying undercorrection of deformity. Similarly, 75% of the outliers in limbs with preoperative valgus deformity were in excessive valgus, implying undercorrection postoperatively. However, a greater (p = 0.02) number of limbs were in excessive valgus malalignment postoperatively in outlier limbs having a preoperative varus deformity of 20° or less (44%) when compared to outlier limbs having a preoperative varus deformity of more than 20° (17%), suggesting limbs with lesser degrees of preoperative varus deformity had a tendency for overcorrection into valgus postoperatively. In contrast, irrespective of the degree of preoperative valgus deformity, 75% of limbs were in excessive valgus postoperatively, implying undercorrection. In both osteoarthritic and rheumatoid knees, a majority of the outliers (57% and 70%, respectively) were in excessive varus.
Fig. 2.
A scatterplot shows the postoperative HKA angle of all knees, with a rectangle around all knees within the acceptable ± 3° range from a neutral alignment of 180°. The horizontal line denotes the mean postoperative HKA angle.
The outlier rates were 7% (101 knees; 44 knees in excessive varus and 57 knees in excessive valgus) for femoral component alignment in the coronal plane and 8% (124 knees; 31 components in excessive varus and 93 components in excessive valgus) for tibial component alignment. A majority of the malaligned femoral and tibial components (56% and 75%, respectively) were placed in excessive valgus. Among the 112 knees that were outliers for postoperative limb mechanical axis, 57% (64 knees) had an associated component malalignment. Of these 64 knees, 31 knees each had either the femoral or the tibial component in malalignment and two knees had both components in malalignment. In the remaining 43% (48 knees), both the femoral and tibial components were well aligned in the coronal plane. Despite both components being well aligned, 75% of these knees had a postoperative mechanical limb alignment in excessive varus and 25% in excessive valgus. In osteoarthritic and rheumatoid knees, a majority of the malaligned femoral components (55% and 80%, respectively) were in excessive valgus. For malaligned tibial components, 75% in osteoarthritis knees and 50% in rheumatoid knees were in excessive valgus (Table 2).
Multivariate analysis showed preoperative varus deformity of more than 20° and femoral bowing of more than 5° were associated with increased risk for postoperative mechanical axis malalignment (Fig. 3, Table 4).
Fig. 3A–B.
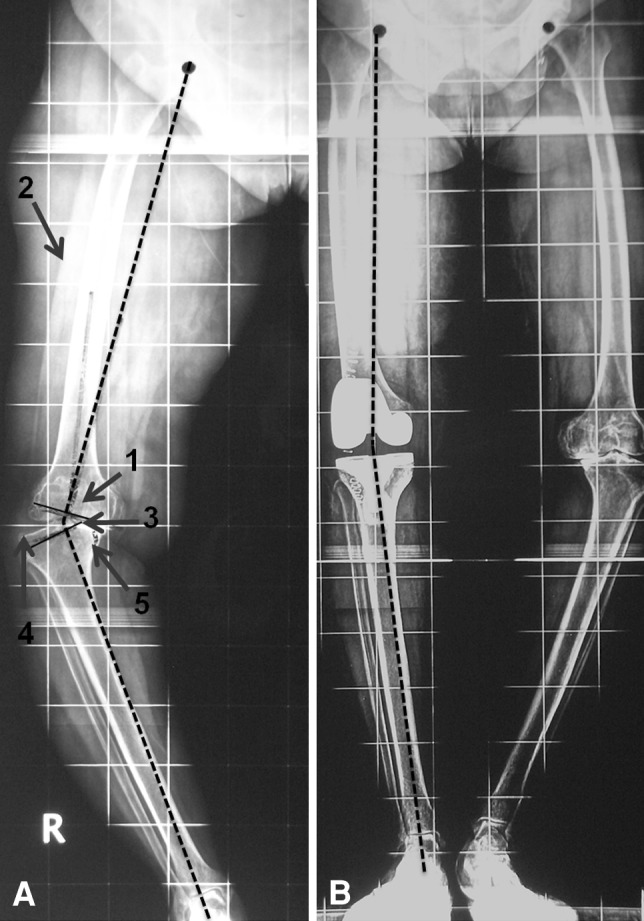
(A) A preoperative full-length hip-to-ankle radiograph shows a typical at-risk knee with the two risk factors for limb malalignment, (1) preoperative varus deformity of 34° and (2) severe femoral bowing in the coronal plane, along with other radiographic features such as (3) large JDA, (4) lateral tibial subluxation, and (5) medial tibial bone loss. (B) A postoperative full-length hip-to-ankle radiograph of the same patient shows the limb in excessive varus of 7°.
Table 4.
Risk factors for postoperative limb mechanical axis alignment (multivariate analysis)
| Risk factor | p value | Odds ratio | 95% CI for odds ratio |
|---|---|---|---|
| Preoperative knee deformity | |||
| Varus < 10° | Reference | Reference | Reference |
| Varus 10°–20° | 0.06 | 0.20 | 0.04–1.06 |
| Varus > 20° | 0.03 | 0.16 | 0.03–0.85 |
| Valgus < 10° | 0.15 | 0.27 | 0.04–1.60 |
| Valgus > 10° | 0.15 | 0.27 | 0.02–1.82 |
| Femoral bowing | |||
| < 5° | Reference | Reference | Reference |
| > 5° | 0.05 | 0.55 | 0.30–1.0 |
| Joint divergence angle | |||
| < 15° | Reference | Reference | Reference |
| > 15° | 0.18 | 0.67 | 0.38–1.19 |
| Tibial bone loss | |||
| < 20 mm | Reference | Reference | Reference |
| > 20 mm | 0.57 | 0.44 | 0.19–1.02 |
| Tibial subluxation | |||
| < 20% | Reference | Reference | Reference |
| > 20% | 0.86 | 0.94 | 0.50–1.77 |
Discussion
Although numerous studies have stressed the importance of a well-aligned limb mechanical axis after TKA [6, 13, 23], it is unclear what clinical and radiographic factors can increase the risk of limb malalignment after TKA. Based on our large series of 1500 computer-assisted TKAs, we sought to answer the following questions: (1) What are the incidence and characteristics of outliers for postoperative limb mechanical axis (HKA angle outside the conventionally acceptable range of 180° ± 3°) and component alignment in TKA? And (2) what are the preoperative clinical or radiographic risk factors for limb mechanical axis malalignment in TKA?
Our study has some limitations. First, this is a radiographic analysis in which improper radiographic technique may lead to errors of measurement. We tried to minimize this source of error by standardizing the technique of taking full-length hip-to-ankle and knee radiographs at our institution. Second, we found 43% of limbs, despite having well-positioned femoral and tibial components, had malalignment of the limb mechanical axis. This may indicate a mediolateral soft tissue imbalance in knee extension, which may cause the mechanical axis to deviate under weightbearing conditions. We have not included analysis of postoperative mediolateral soft tissue balance of TKA, which is relevant to this study. Third, we focused on the coronal plane alignment of limbs and components after TKA and did not analyze these in the sagittal and axial planes. Although the coronal plane has been the focus of attention in most studies on limb and component alignment, both the sagittal and axial planes may be equally important for long-term implant survival and function after TKA. Fourth, intraoperative factors such as error during registration of anatomic landmarks or accidental displacement of the pins or arrays during navigation may affect the accuracy of the procedure and contribute to outliers. The analysis of such factors as risks for malalignment was not part of our study. Finally, based on previously published studies that have also generally used this range, we have defined outliers as those outside the ± 3° range from 180° for limb mechanical axis and outside the ± 3° range from 90° for component alignment. However, we are fully cognizant of the fact that this is an arbitrary range and there is as yet inconclusive evidence to support its use [22].
Our study of 1500 TKAs showed an outlier rate of 7% for postoperative limb mechanical axis, 7% for femoral component alignment in the coronal plane, and 8% for tibial component alignment in the coronal plane, indicating navigation achieves accurate placement of femoral and tibial components and restoration of limb mechanical axis in the coronal plane. Our literature review of studies analyzing limb and component alignment using hip-to-ankle radiographs of least 100 navigated TKAs performed by individual surgeons/institutions revealed wide variations in the outlier rates (Table 5). Outlier rates were 5% to 21% for postoperative limb mechanical axis, 4% to 11% for femoral component alignment, and 3% to 11% for tibial component alignment. A higher outlier rate in some of these studies when compared to our results could be due to the fact that some of these studies involved multiple surgeons where individual experience with navigation could have played a role [8, 10] (in contrast to our single-surgeon study), had relatively smaller number of knees (maximum of 100–500 TKAs) [2, 8, 10, 11, 14, 17, 26], and were performed early during the evolution of navigation software and tools (1999–2003) [2, 8, 10, 11] (Table 5).
Table 5.
Comparison of outlier rates for postoperative HKA axis and component alignment between our study and studies in the literature published from 2007 to 2012 and having a minimum of 100 computer-assisted TKAs
| Study | Year | Study design | Navigation system | Number of TKAs | Outliers for postoperative HKA axis (%) | Outliers for femoral component alignment (%) | Outliers for tibial component alignment (%) | Minimum followup (months) |
|---|---|---|---|---|---|---|---|---|
| Anderson et al. [2] | 2005 | Retrospective, matched-pair case-control study, single surgeon | OrthoPilot® (Stryker Orthopaedics, Mahwah, NJ, USA) | 116 | 5 | NA | NA | NA |
| Haaker et al. [8] | 2005 | Retrospective, matched-pair case-control, 4 surgeons | OrthoPilot® (Stryker) | 100 | 21 | NA | NA | NA |
| Jenny et al. [10] | 2005 | Retrospective, matched-pair case-control study, 2 surgeons | OrthoPilot® (Stryker) | 235 | 8 | 11 | 11 | 3 |
| Mullaji et al. [17] | 2007 | RCT, single surgeon | Ci (Brainlab AG, Munich, Germany) | 282 | 9 | 9 | 9 | 12 |
| Martin et al. [14] | 2007 | RCT, 3 surgeons | VectorVision® (Brainlab) | 100 | 6 | 5 | 3 | 3 |
| Tingart et al. [26] | 2008 | Prospective | VectorVision® (Brainlab) and Ci™ System (DePuy Orthopaedics Inc, Warsaw, IN, USA) | 500 | 5 | 4 | 5 | NA |
| Kim et al. [11] | 2009 | Prospective, single surgeon in sequential bilateral TKAs | VectorVision® (Brainlab) | 160 | 13 | 11 | 9 | 36 |
| Current study | 2012 | Retrospective, single surgeon | Ci (Brainlab) | 1500 | 7 | 7 | 8 | 12 |
HKA = hip-knee-ankle; RCT = randomized controlled trial; NA = not available.
Another important finding of our study is that limbs with lesser preoperative varus deformity had a tendency for overcorrection into valgus postoperatively. Hence, the surgeon should avoid overrelease of soft tissue medially and achieve adequate bone resection from the proximal tibia and distal femur to avoid overcorrection in such knees. Of the 112 limbs that were outliers for limb mechanical axis, 64 limbs had an associated component malalignment and the remaining 48 limbs had both the femoral and tibial components well aligned. Hence, a majority of malaligned limbs were probably a consequence of component malalignment. Although computer navigation allows for accurate placement of cutting blocks and verification of bone cuts intraoperatively, deviations can occur between the bone resection and the final implant position. This could be due to improper cementation and impaction of the components intraoperatively. Catani et al. [4] reported alignment deviations of more than 1° can occur in 20% of limbs for femoral component position in the coronal plane. Malaligned knees where both components were placed accurately were probably the result of mediolateral soft tissue imbalance. Although computer navigation is reportedly accurate and reliable for measuring soft tissue balance intraoperatively [15], the technique of soft tissue balance is complex and based on surgeon technique and subjective assessment. Although the senior author has ensured mediolateral soft tissue balance of within 2 mm at the end of each TKA, it is possible this balance may undergo change over time postoperatively. Bellemans et al. [3] reported all knees underwent increased mediolateral laxity by an average of 1 mm on the medial and lateral sides owing to stress relaxation immediately after the procedure. Furthermore, mediolateral soft tissue balance assessed intraoperatively in full extension is performed under nonweightbearing conditions, which may be different when the patient stands (as during postoperative full-length radiography) or walks.
Our study showed knees with a preoperative varus deformity of more than 20° and femoral bowing of more than 5° were at greater risk for postoperative mechanical axis malalignment. Usually knees with severe varus deformities (> 20°) have substantial associated femoral bowing, lateral soft tissue laxity (greater JDA and tibial subluxation), and tibial bone loss [19, 20] (Fig. 3). These factors may lead to distortion of bony landmarks, which may lead to errors in registration during navigation and consequently malposition of components and inaccurate assessment of limb alignment with navigation. Furthermore, substantial associated lateral soft tissue laxity may make soft tissue balance challenging. We have dealt with such substantial mediolateral imbalance by a graduated, stepwise substantial soft tissue release and judicious use of a sliding epicondylar osteotomy to achieve optimum soft tissue balance [18, 21].
We found computer navigation results in accurate limb and component alignment in the coronal plane in most TKAs. However, minor component malalignment and mediolateral soft tissue imbalance may still contribute to malalignment of limbs after TKA. The presence of a severe preoperative varus deformity (> 20°) and femoral bowing of more than 5° in the coronal plane on preoperative radiographs should alert the surgeon to increased risk of malalignment in such knees. Hence, every measure should be undertaken in such at-risk knees to ensure optimum limb and component alignment and soft tissue balance.
Acknowledgments
The authors thank Prof Harshad Thakur, MD, School of Health System Studies, TATA Institute of Social Sciences, Mumbai, India, and Mr Saket Tibrewal, MBBS, FRCS (Tr&Orth), Specialist Registrar, The Percival Pott Rotation, London, UK, for their help in statistical analysis.
Footnotes
The institution of one or more of the authors (APL, SB) has received, during the study period, funding from DePuy, India (Mumbai, India) for Joint Replacement Fellowships. One of the authors (ABM) certifies that he is a consultant for DePuy, India. Each of the remaining authors certifies that he or she, or a member of his or her family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Breach Candy Hospital, Mumbai, India.
References
- 1.Aglietti P, Buzzi R, Scrobe F. Autologous bone grafting for medial tibial defects in total knee arthroplasty. J Arthroplasty. 1991;6:287–294. doi: 10.1016/S0883-5403(06)80178-6. [DOI] [PubMed] [Google Scholar]
- 2.Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: comparison with conventional methods. J Arthroplasty. 2005;20(7 suppl 3):132–138. doi: 10.1016/j.arth.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Bellemans J, D’Hooghe P, Vandenneucker H, Van Damme G, Victor J. Soft tissue balance in total knee arthroplasty: does stress relaxation occur perioperatively? Clin Orthop Relat Res. 2006;452:49–52. doi: 10.1097/01.blo.0000238790.29102.95. [DOI] [PubMed] [Google Scholar]
- 4.Catani F, Biasca N, Ensini A, Leardini A, Bianchi L, Digennaro V, Giannini S. Alignment deviation between bone resection and final implant positioning in computer-navigated total knee arthroplasty. J Bone Joint Surg Am. 2008;90:765–771. doi: 10.2106/JBJS.G.00293. [DOI] [PubMed] [Google Scholar]
- 5.Cheng T, Zhao S, Peng X, Zhang X. Does Computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc. 2012;20:1307–1322. doi: 10.1007/s00167-011-1588-8. [DOI] [PubMed] [Google Scholar]
- 6.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 suppl):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 7.Fu Y, Wang M, Liu Y, Fu Q. Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012;20:1075–1082. doi: 10.1007/s00167-011-1695-6. [DOI] [PubMed] [Google Scholar]
- 8.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 9.Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplasty. 2012;27:1177–1182. doi: 10.1016/j.arth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 10.Jenny JY, Clemens U, Kohler S, Kiefer H, Konermann W, Miehlke RK. Consistency of implantation of a total knee arthroplasty with a non-image-based navigation system: a case-control study of 235 cases compared with 235 conventionally implanted prostheses. J Arthroplasty. 2005;20:832–839. doi: 10.1016/j.arth.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Kim JS, Choi Y, Kwon OR. Computer-assisted surgical navigation does not improve the alignment and orientation of the components in total knee arthroplasty. J Bone Joint Surg Am. 2009;91:14–19. doi: 10.2106/JBJS.G.01700. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi AV, Jr, Berend KR, Ng VY. Neutral mechanical alignment: a requirement for successful TKA: affirms. Orthopedics. 2011;34:e504–e506. doi: 10.3928/01477447-20110714-40. [DOI] [PubMed] [Google Scholar]
- 13.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. 2009;24:570–578. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Martin A, Wohlgenannt O, Prenn M, Oelsch C, von Strempel A. Imageless navigation for TKA increases implantation accuracy. Clin Orthop Relat Res. 2007;460:178–184. doi: 10.1097/BLO.0b013e31804ea45f. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kurosaka M, Kuroda R. Soft tissue balance measurement in posterior-stabilized total knee arthroplasty with a navigation system. J Arthroplasty. 2009;24:358–364. doi: 10.1016/j.arth.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Molli RG, Anderson KC, Buehler KC, Markel DC. Computer-assisted navigation software advancements improve the accuracy of total knee arthroplasty. J Arthroplasty. 2011;26:432–438. doi: 10.1016/j.arth.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Mullaji A, Kanna R, Marawar S, Kohli A, Sharma A. Comparison of limb and component alignment using computer-assisted navigation versus image intensifier-guided conventional total knee arthroplasty: a prospective, randomized, single-surgeon study of 467 knees. J Arthroplasty. 2007;22:953–959. doi: 10.1016/j.arth.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 18.Mullaji A, Shetty GM. Extra-articular deformity: femur. In: Malhotra R, editor. Mastering Orthopedic Techniques: Total Knee Arthroplasty. New Delhi, India: Jaypee Brothers Medical Publishers; 2010. pp. 217–222. [Google Scholar]
- 19.Mullaji AB, Marawar SV, Mittal V. A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J Arthroplasty. 2009;24:861–867. doi: 10.1016/j.arth.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 20.Mullaji AB, Padmanabhan V, Jindal G. Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20 degrees. J Arthroplasty. 2005;20:550–561. doi: 10.1016/j.arth.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Mullaji AB, Shetty GM. Lateral epicondylar osteotomy using computer navigation in total knee arthroplasty for rigid valgus deformities. J Arthroplasty. 2010;25:166–169. doi: 10.1016/j.arth.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 23.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93:1588–1596. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- 24.Schmitt J, Hauk C, Kienapfel H, Pfeiffer M, Efe T, Fuchs-Winkelmann S, Heyse TJ. Navigation of total knee arthroplasty: rotation of components and clinical results in a prospectively randomized study. BMC Musculoskelet Disord. 2011;12:16–23. doi: 10.1186/1471-2474-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skyttä ET, Haapamäki V, Koivikko M, Huhtala H, Remes V. Reliability of the hip-to-ankle radiograph in determining the knee and implant alignment after total knee arthroplasty. Acta Orthop Belg. 2011;77:329–335. [PubMed] [Google Scholar]
- 26.Tingart M, Lüring C, Bäthis H, Beckmann J, Grifka J, Perlick L. Computer-assisted total knee arthroplasty versus the conventional technique: how precise is navigation in clinical routine? Knee Surg Sports Traumatol Arthrosc. 2008;16:44–50. doi: 10.1007/s00167-007-0399-4. [DOI] [PubMed] [Google Scholar]
- 27.Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong). 2007;15:32–36. doi: 10.1177/230949900701500108. [DOI] [PubMed] [Google Scholar]
- 28.Yau WP, Chiu KY, Zuo JL, Tang WM, Ng TP. Computer navigation did not improve alignment in a lower-volume total knee practice. Clin Orthop Relat Res. 2008;466:935–945. doi: 10.1007/s11999-008-0144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zorman D, Etuin P, Jennart H, Scipioni D, Devos S. Computer-assisted total knee arthroplasty: comparative results in a preliminary series of 72 cases. Acta Orthop Belg. 2005;71:696–702. [PubMed] [Google Scholar]