History
Proximal humerus fractures are the third most common fracture type in individuals older than 65 years, after distal radius and proximal femur fractures [8]. In 1970, Charles Neer described his four-segment classification system [18]. He believed the existing classifications were inadequate for research purposes, as they did not differentiate between injuries of varied severity nor did they group like fractures [5, 12, 18]. The classification systems at that time were based on the mechanism of injury or level of the fracture line, but did not consider many surgically important aspects or pathologic features of injury such as tuberosity displacement [18]. Forty years later, surgeons continue to use Neer’s four-segment fracture classification system for proximal humerus fractures because it is useful in guiding treatment, grouping similar fracture patterns for research purposes, and explaining pathologic features of injury.
Neer’s classification was based on careful analysis of radiographs and surgical findings from 300 proximal humerus fractures he treated at the New York Orthopaedic Hospital-Columbia Presbyterian Medical Center between 1953 and 1967 [18] . His classification system was based on an observation made much earlier by Codman, that all proximal humerus fractures were composed of four major segments: the lesser tuberosity, greater tuberosity, articular surface, and humeral shaft [7]. Neer added categories for articular surface fractures and dislocations, as he correctly observed these to be important prognostic factors. He sought to provide a conceptual framework to explain the pathoanatomy of proximal humerus fractures by accounting for displaced bone fragments, rotator cuff attachments, and vascular supply. His secondary aim was to catalogue the most common injury patterns for research purposes. In his original article, he described how characteristic patterns of displacement occur with each fracture type, and he explained how these result from the attached bone segments and the deforming forces generated by the rotator cuff [18].
It has now been more than four decades since Charles Neer first introduced his classification system, and it has endured with relatively minor modifications. Neer noted that when the classification was first published in the Journal of Bone and Joint Surgery, the editor Dr. Thornton Brown insisted that he provide defined criteria for determining if a fragment was displaced [18, 20]. In response, Neer set 45° angulation and 1-cm separation as the thresholds for displacement. Ironically, these criteria have become the most recognizable and quotable features of the classification system. Neer acknowledged that these were somewhat arbitrary but embraced the editor’s viewpoint that definitions were necessary for universal application. Aside from changes in the nomenclature of categories, the only other major modification was the addition of the valgus impacted four-part fracture category in 2002 [20].
Classification System
The four-segment classification system defines proximal humerus fractures by the number of displaced segments or parts, with additional categories for articular fractures and dislocations (Fig. 1). The potential segments involved are the greater tuberosity, lesser tuberosity, articular surface, and humeral diaphysis. A segment is defined as displaced if there is greater than 1 cm separation or 45° angulation.
Fig. 1.
The Neer four-segment classification system for proximal humerus fractures is shown. This diagram includes the valgus impacted four-part fracture (A) and the classic displaced four-part fracture (B). (Reprinted with permission from Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089.)
One-Part Fractures
No fragments meet the criteria for displacement; a fracture with no fragments considered displaced is defined as a one-part fracture regardless of the actual number of fracture lines or their location.
Two-Part Fractures
One segment is displaced, which may be the greater tuberosity, lesser tuberosity, or articular segment at the level of the anatomic neck or surgical neck.
Three-Part Fractures
With a three-part fracture, one tuberosity is displaced and the surgical neck fracture is displaced. The remaining tuberosity is attached, which produces a rotational deformity.
Four-Part Fractures
All four segments (both tuberosities, the articular surface, and the shaft) meet criteria for displacement. The articular segment typically is laterally displaced and out of contact with the glenoid (Fig. 2). This is a severe injury and carries a high risk of avascular necrosis.
Fig. 2A–B.

The four-part fracture occurs in two forms. In the (A) classic four-part fracture, the articular surface of the head is no longer in contact with the glenoid. In the (B) valgus impacted fracture, the humeral head is driven down and the tuberosities splay out. (Reprinted with permission from Elsevier from Neer CS 2nd. Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elbow Surg. 2002;11:389–400.)
Valgus-Impacted Four-Part Fractures
Neer added this pattern (Fig. 2B) as a separate category in 2002 [20]. In this situation, the head is rotated into a valgus posture and driven down between the tuberosities, which splay out to accommodate the head. Unlike in the classic four-part fracture, the articular surface maintains contact with the glenoid, and is not laterally displaced. This four-part fracture warranted its own category because the prognosis and treatment for this injury are different than those for the classic four-part fracture [20, 30].
Fracture Dislocations and Articular Surface Injuries
Separate categories were added for dislocations because they represent more severe injuries, and are more likely to have avascular necrosis and heterotopic ossification develop. Similarly, articular surface fractures were placed in a separate category because of their unique treatment considerations. These come in two varieties, head-splitting fractures and impaction fractures.
Reliability/Utility
Numerous studies have examined the interobserver and intraobserver reliabilities of fracture classification systems. Concordance between observers often is expressed as a kappa value; this statistic ranges from zero (agreement attributable to chance alone) to 1.0 (complete agreement) [15, 16].
The interobserver reliability of the Neer classification system has ranged between 0.21 and 0.64, while the intraobserver reliability is somewhat better between 0.5 and 0.8 [4, 24–26]. This is comparable to the reliability of the AO proximal humerus fracture classification system, and fracture classification systems pertaining to other areas such as the ankle, femur, and scaphoid [1, 6, 9, 25, 26]. Although interobserver reliability with Neer’s classification is variable, and tends to hover in the moderate range, we identified no other system for evaluating these fractures that is consistently more reliable than the Neer classification.
The reliability of the system is greater when more-experienced observers or shoulder specialists examine the radiographs [14, 24]. It has been suggested that some of the observed variability may be attributable to difficulty interpreting the patterns of complex three-dimensional (3-D) fractures on two-dimensional plain radiographs [23]. The addition of advanced imaging techniques improves the intraobserver reliability, however there is no clear evidence that interobserver reliability is increased. Brunner et al. reported a modest increase in the interobserver reliability with the addition of CT images [6], whereas other authors have reported minimal or no improvement [4, 26]. Likewise, investigators disagree regarding whether 3-D CT reconstructions improve reliability. Brunner et al. found 3-D CT analysis increased reliability to excellent (> 0.80) [6], whereas Sjoden et al. found no benefit [26].
Although inadequate radiographic representation likely confounds application of the classification system it cannot account for all observed inconsistency. Majed et al. found inadequate reliability between senior shoulder specialists even when they were presented with a physical model of the fracture [17]. This clearly shows that some of the problems are related to variable application of the classification system even among experienced shoulder surgeons.
Some have opined that the observed inconsistencies in reliability using Neer’s schema are a function of the large number of categories, and the difficulty of estimating whether a fragment meets the definition of displacement established by Neer [14, 23, 24]. Interestingly, though, the reliability did not improve in several studies when the classification was simplified to four categories (one part, two part, three part, and four part), or when the criteria for displaced fragments were removed [4, 14, 24]. The Neer classification system has a moderate degree of concordance between observers, which is comparable to other fracture classification systems, and there appear to be no reproducible strategies for increasing this degree of reliability.
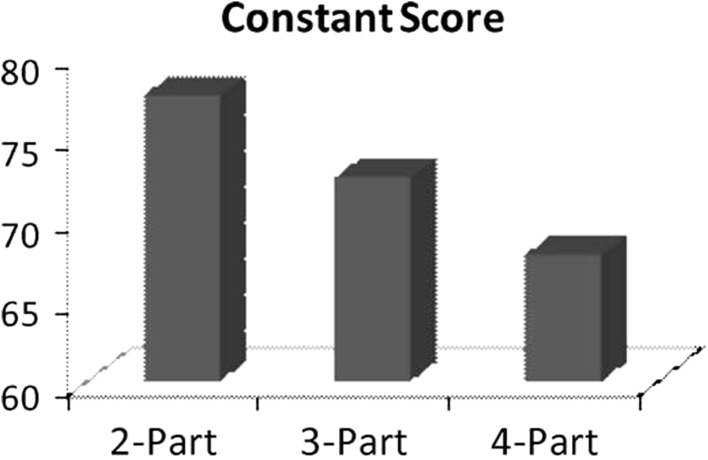
The utility of a fracture classification system may be measured by its ability to predict a clinical result or event such as fracture union, avascular necrosis, or restoration of painless function. In the case of proximal humerus fractures, this is difficult, because there are many variables other than the fracture pattern that influence the clinical outcome, including the patient’s age, comorbidities, bone quality, associated injuries, and reduction quality. Nevertheless, a couple studies have reported a correlation between the Neer classification and clinical outcome scores [29, 32] (Fig. 3). Two meta-analyses have shown that the Constant-Murley scores decrease as the number of Neer fracture parts increases [29, 32]. A regression analysis showed that this predictive value is largely explained by a correlation between intraoperative and postoperative complications and increased parts [31].
Fig. 3.
There is a correlation between functional outcome scores and the Neer classification system for patients undergoing open reduction internal fixation. The Constant score decreases with increasing fracture parts. (Reprinted with permission from Elsevier from Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408–413.)
Neer also believed that the four-segment classification system would help predict the incidence of avascular necrosis (AVN) because it focused on understanding the soft tissue attachments to the humeral head and the vascular supply. In particular, he believed that four-part fractures were especially prone to AVN because “in all four part lesions the blood supply to the humeral head has been severed” [18]. He found AVN in greater than 50% of these fractures and advocated for arthroplasty in their treatment [19, 20]. However, subsequent research has not found a four-part injury predicts AVN [10, 33]. In fact, no particular fracture characteristics consistently predict AVN [21]. Bastian and Hertel [3] and Hertel et al. [11] measured blood flow to the humeral head of proximal humerus fractures intraoperatively and found that a disrupted medial cortical hinge and short (< 8 mm) metaphyseal extension were correlated with poor perfusion, but even this did not predict the occurrence of avascular necrosis.
Limitations
The most commonly cited limitations of this fracture system are the arbitrary definition of displacement, the difficulty in estimating if a fragment is displaced, and limited interobserver reliability. The Neer classification system also is limited in its ability to differentiate among the many patterns of minimally displaced fractures. This group of fractures includes greater than 80% of proximal humerus fractures but, in fact, represent a variety of injury patterns and outcomes. Koval et al. reviewed 104 patients with minimally displaced fractures treated with physiotherapy [13]. Although most patients had a good outcome, 23% had a fair or poor result. There may be fracture and patient characteristics not included in the Neer classification system that predict these lesser outcomes. Bahrs et al. reviewed a series of one-part fractures and found intraarticular extension, tuberosity displacement greater than 5 mm, and 15° angulation were associated with decreased clinical outcomes [2]. These studies suggest that the Neer classification may not sufficiently predict prognosis in patients with the most common injury pattern.
The pattern of fracture displacement—as much or more than the number of parts as defined by Neer—likewise appears to affect prognosis. Solberg et al. found the direction of displacement (varus versus valgus) predicted functional outcome, with valgus fractures faring better than varus fracture patterns [28]. In addition, the length of the metaphyseal attachment to the articular surface may affect prognosis [11, 27, 28].
Conclusions
The Neer fracture classification system provides a useful framework for clinical assessment of and research for proximal humerus fractures. This classification system has moderate interobserver reliability, and correlates to a large degree (albeit not perfectly) with complications and functional results. There are limitations to the four-segment classification system, including limited ability to distinguish among the many patterns of one-part fractures, inconsistent application among observers, and an arbitrary (and perhaps insufficiently stringent) definition of displacement. Furthermore, the Neer system does not incorporate several variables such as the length of the metaphyseal hinge, magnitude of initial displacement, and varus displacement that predict clinical outcome scores.
The strength of the four-segment classification system is its ability to separate proximal humerus fractures into broad categories, which are intuitively understood and which have important differences. The classification is widely used by surgeons because, at least broadly speaking, it has been found useful to guide treatment, anticipate prognosis, and group similar fracture patterns for research purposes. The classification system also is pedagogically useful for orthopaedic trainees in that it helps explain how the deforming forces around the joint cause the observed patterns of fracture displacement.
When clinically applying the Neer classification system we find it helpful to consider a few additional factors such as the presence of varus displacement, medial comminution, and poor bone quality. These attributes contribute to decreased biomechanical stability after open reduction and internal fixation and consequently are associated with varus collapse, articular screw penetration, and lesser outcomes [22, 27, 28, 31]. None of the above factors are absolute contraindications to internal fixation, but the alternatives of hemiarthroplasty or nonoperative management might be more heavily considered in those situations.
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Andersen E, Jorgensen LG, Hededam LT. Evans’ classification of trochanteric fractures: an assessment of the interobserver and intraobserver reliability. Injury. 1990;21:377–378. doi: 10.1016/0020-1383(90)90123-C. [DOI] [PubMed] [Google Scholar]
- 2.Bahrs C, Rolauffs B, Dietz K, Eingartner C, Weise K. Clinical and radiological evaluation of minimally displaced proximal humeral fractures. Arch Orthop Trauma Surg. 2010;130:673–679. doi: 10.1007/s00402-009-0975-9. [DOI] [PubMed] [Google Scholar]
- 3.Bastian JD, Hertel R. Initial post-fracture humeral head ischemia does not predict development of necrosis. J Shoulder Elbow Surg. 2008;17:2–8. doi: 10.1016/j.jse.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 4.Bernstein J, Adler LM, Blank JE, Dalsey RM, Williams GR, Iannotti JP. Evaluation of the Neer system of classification of proximal humeral fractures with computerized tomographic scans and plain radiographs. J Bone Joint Surg Am. 1996;78:1371–1375. doi: 10.2106/00004623-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Bohler L. The Treatment of Fractures. 5. New York, NY: Grune and Stratton; 1956. [Google Scholar]
- 6.Brunner A, Honigmann P, Treumann T, Babst R. The impact of stereo-visualisation of three-dimensional CT datasets on the inter- and intraobserver reliability of the AO/OTA and Neer classifications in the assessment of fractures of the proximal humerus. J Bone Joint Surg Br. 2009;91:766–771. doi: 10.1302/0301-620X.91B6.22109. [DOI] [PubMed] [Google Scholar]
- 7.Codman EA. The Shoulder Rupture of the Supraspinatus Tendon and Other Lesion in or About the Subacromial Bursa. Boston, MA: Thomas Todd Co; 1934. [Google Scholar]
- 8.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 9.Dias JJ, Taylor M, Thompson J, Brenkel IJ, Gregg PJ. Radiographic signs of union of scaphoid fractures: an analysis of inter-observer agreement and reproducibility. J Bone Joint Surg Br. 1988;70:299–301. doi: 10.1302/0301-620X.70B2.3346310. [DOI] [PubMed] [Google Scholar]
- 10.Helwig P, Bahrs C, Epple B, Oehm J, Eingartner C, Weise K. Does fixed-angle plate osteosynthesis solve the problems of a fractured proximal humerus? A prospective series of 87 patients. Acta Orthop. 2009;80:92–96. doi: 10.1080/17453670902807417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427–433. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 12.Kocher T. Beitrage zur Kenntniss einiger praktisch wichtiger Fracturenformen. Basel, Switzerland: Carl Sollman; 1896. [Google Scholar]
- 13.Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79:203–207. doi: 10.2106/00004623-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Kristiansen B, Andersen UL, Olsen CA, Varmarken JE. The Neer classification of fractures of the proximal humerus: an assessment of interobserver variation. Skeletal Radiol. 1988;17:420–422. doi: 10.1007/BF00361661. [DOI] [PubMed] [Google Scholar]
- 15.Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–374. doi: 10.2307/2529786. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 17.Majed A, Macleod I, Bull AM, Zyto K, Resch H, Hertel R, Reilly P, Emery RJ. Proximal humeral fracture classification systems revisited. J Shoulder Elbow Surg. 2011;20:1125–1132. doi: 10.1016/j.jse.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Neer CS., 2nd Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 19.Neer CS., 2nd Displaced proximal humeral fractures: Part I. Classification and evaluation. By Charles S. Neer, I, 1970. Clin Orthop Relat Res. 1987;223:3–10. [PubMed] [Google Scholar]
- 20.Neer CS., 2nd Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elbow Surg. 2002;11:389–400. doi: 10.1067/mse.2002.124346. [DOI] [PubMed] [Google Scholar]
- 21.Neviaser AS, Hettrich CM, Dines JS, Lorich DG. Rate of avascular necrosis following proximal humerus fractures treated with a lateral locking plate and endosteal implant. Arch Orthop Trauma Surg. 2011;131:1617–1622. doi: 10.1007/s00402-011-1366-6. [DOI] [PubMed] [Google Scholar]
- 22.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected] J Bone Joint Surg Am. 2008;90:233–240. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 23.Shrader MW, Sanchez-Sotelo J, Sperling JW, Rowland CM, Cofield RH. Understanding proximal humerus fractures: image analysis, classification, and treatment. J Shoulder Elbow Surg. 2005;14:497–505. doi: 10.1016/j.jse.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Sidor ML, Zuckerman JD, Lyon T, Koval K, Cuomo F, Schoenberg N. The Neer classification system for proximal humeral fractures: an assessment of interobserver reliability and intraobserver reproducibility. J Bone Joint Surg Am. 1993;75:1745–1750. doi: 10.2106/00004623-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Siebenrock KA, Gerber C. The reproducibility of classification of fractures of the proximal end of the humerus. J Bone Joint Surg Am. 1993;75:1751–1755. doi: 10.2106/00004623-199312000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Sjoden GO, Movin T, Guntner P, Aspelin P, Ahrengart L, Ersmark H, Sperber A. Poor reproducibility of classification of proximal humeral fractures: additional CT of minor value. Acta Orthop Scand. 1997;68:239–242. doi: 10.3109/17453679708996692. [DOI] [PubMed] [Google Scholar]
- 27.Solberg BD, Moon CN, Franco DP, Paiement GD. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23:113–119. doi: 10.1097/BOT.0b013e31819344bf. [DOI] [PubMed] [Google Scholar]
- 28.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009;91:1689–1697. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]
- 29.Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408–413. doi: 10.1016/j.injury.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 30.Stableforth PG. Four-part fractures of the neck of the humerus. J Bone Joint Surg Br. 1984;66:104–108. doi: 10.1302/0301-620X.66B1.6693466. [DOI] [PubMed] [Google Scholar]
- 31.Sudkamp NP, Audige L, Lambert S, Hertel R, Konrad G. Path analysis of factors for functional outcome at one year in 463 proximal humeral fractures. J Shoulder Elbow Surg. 2011;20:1207–1216. doi: 10.1016/j.jse.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg. 2009;18:837–844. doi: 10.1016/j.jse.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 33.Trupka A, Wiedemann E, Ruchholtz S, Brunner U, Habermeyer P, Schweiberer L. [Dislocated multiple fragment fractures of the head of the humerus: does dislocation of the humeral head fragment signify a worse prognosis?][in German] Unfallchirurg. 1997;100:105–110. doi: 10.1007/s001130050100. [DOI] [PubMed] [Google Scholar]