Abstract
Background
In a previously reported series of 51 patients with 62 cemented, fixed-bearing unicompartmental knee arthroplasties, we reported a 10-year, 98% survival rate with an average knee score of 92 points. The survivorship and modes of failure past 10 years are incompletely understood.
Questions/Purposes
At 15-year followup we sought to determine (1) the overall durability and survivorship of this design; (2) modes of failure; and (3) the progression of arthritis in the nonresurfaced compartments.
Methods
Nineteen knees in 16 patients were available for study with 34 patients lost to death and one lost to followup. At 15 years, we analyzed the Kaplan-Meier survivorship as well as durability with regard to radiographic loosening and knee scores, determined modes of failure, and assessed radiographs for degeneration in the nonresurfaced compartments.
Results
Fifteen-year survivorship was 93% and 20-year survivorship was 90%. Four of 62 knees were revised to total knee arthroplasty at a mean of 144 months. One knee was revised for patellofemoral and lateral compartment degeneration, one for lateral compartment degeneration, one for polyethylene disengagement and metallosis, and one for pain of unclear etiology. No patients had aseptic loosening or osteolysis. The mean knee score was 78 at latest followup. Arthritic progression in the nonresurfaced compartments was common although symptomatic in only two patients.
Conclusions
With this cemented, fixed-bearing design, the failure rates were low, there were no cases of failure secondary to wear or loosening, and the survivorship was similar to that reported for total knee arthroplasty.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Between 1998 and 2005, use of unicompartmental knee arthroplasty (UKA) increased at a rate nearly triple that of TKA [33]. Although early studies of UKA reported revision rates as high as 32% (seven of 22 knees) within 7 years of followup [11, 19], more recent studies have demonstrated survival rates of greater than 90% at 10 years [4, 7, 23, 39] and survivorship into the second decade ranging from 70% to 92% [10, 22, 24, 25, 37, 38, 40].
We previously reported the results of 51 patients with 62 fixed-bearing UKAs at a minimum of 6 years [6] and later 10 years [4, 5]. The 10-year survival rate was 98%, and the 13-year survival rate was 96% with revision for any reason or radiographic loosening as the end point. At a minimum of 10 years, the mean Hospital for Special Surgery knee score improved from 55 points (range, 30–79 points) preoperatively to 92 points (range, 60–100 points). No components appeared radiographically loose, although three knees had a complete tibial radiolucent line. These lines appeared after the initial postoperative radiographs but were nonprogressive in all cases.
The purposes of this report are to determine, at a minimum of 15 years of followup, (1) the overall durability and survivorship of this design; (2) modes of failure; and (3) progression of arthritis in the nonresurfaced compartments.
Patients and Methods
The original cohort of 62 knees included 34 women and 17 men with an average age of 58 years (range, 51–84 years). The diagnosis was osteoarthritis in 53 knees (85%) and osteonecrosis in nine knees (15%). Fifty-nine arthroplasties (95%) involved the medial compartment and three (5%) involved the lateral compartment.
The indications for this implant at the time were: (1) unicompartmental osteoarthritis or osteonecrosis; (2) radiographic evidence of preservation of the opposite compartment and only mild radiographic signs of deterioration of the patellofemoral joint; (3) ROM of at least 90° with a flexion contracture of < 15°; (4) minimal pain at rest; (5) a relatively sedentary lifestyle; (6) a weight of < 275 lb (124.7 kg); and (7) age older than 50 years. The contraindications were: (1) inflammatory arthritis; (2) anterior knee pain; (3) knee instability; and (4) intraoperative identification of greater than Outerbridge Grade 2 degeneration of the patellofemoral or adjacent tibiofemoral compartment [26]. Of the original cohort, 34 patients died and one was lost to followup, leaving 19 knees in 16 patients available for study at a minimum of 15 years. All of the patients who died had well-functioning knees at the followup before their death as confirmed by clinic notes and/or family members. The 16 remaining patients included four men and 12 women who had a mean age of 63 years (range, 58–73 years) at the time of the index procedure. The underlying diagnosis was osteoarthritis in 18 knees and osteonecrosis in one knee in those followed at a minimum of 15 years. The minimum followup was 15 years (mean, 19 years; range, 15–21 years). Three knees in three of these 16 living patients were revised, leaving 16 knees in 13 patients available for study (Table 1). We obtained institutional review board approval for this study.
Table 1.
The findings reported at each of the three followup periods
| Patient details | Minimum 6-year followup study | Minimum 10-year followup study | Minimum 15-year followup study |
|---|---|---|---|
| Total number followed | 51 knees (40 patients) | 49 knees (38 patients) | 19 knees (16 patients) |
| Mean duration of followup (years) | 7.5 (range, 6–10) | 12 (range, 10–13) | 19 (range, 15–21) |
| Died before minimum followup | 10 knees (10 patients) | 13 knees (13 patients) | 42 knees (34 patients) |
| Lost to followup | 1 knee (1 patient) | 0 knees | 1 knee (1 patient) |
A cemented, fixed-bearing Miller-Galante unicompartmental knee system (Zimmer, Warsaw, IN, USA) was implanted in all patients. Exposure was achieved through a medial parapatellar arthrotomy, and an intramedullary femoral cutting jig and an extramedullary tibial cutting jig were used in all knees.
We evaluated patients clinically using the Hospital for Special Surgery (HSS) knee scores [12] because this score was used in our prior reports. Patients were evaluated clinically at 3 weeks, 6 weeks, 3 months, 1 year, and every year thereafter and radiographically at 6 weeks and every year thereafter. Eight knees in eight patients who were unable to followup in the clinic were contacted by telephone by two observers (JRHF, NMB) not involved with the index procedures. We obtained standing AP, supine lateral, and merchant patellar views of the knee for radiographic analysis. Eight patients (nine knees) had radiographic evaluation at a minimum of 15 years. Three of us (JRHF, NMB, CJD) independently evaluated arthritic progression in the nonresurfaced compartments by comparing the 6-week and the most recent radiographs using the following grading system [6]: Grade 1, osteophytes without joint space narrowing; Grade 2, ≤ 25% joint space narrowing; Grade 3, 26% to 50% joint space narrowing; and Grade 4, > 50% joint space narrowing. Radiographic analysis of loosening was performed based on the method of the Knee Society [8]. The bone-cement interfaces and the prosthesis-cement interfaces were evaluated in each of 10 zones for radiolucencies [6]. Radiolucencies were considered progressive if there was an increase in size of the radiolucency or if the radiolucency progressed from one zone to an adjacent zone with time. Sequential radiographs were reviewed for evidence of component subsidence or position change. Definite loosening was defined as a change in position (subsidence) of > 2 mm or an angular change of > 3° relative to the surrounding bone as seen on sequential radiographs with the use of the early radiographs as a baseline [4, 35]. Osteolysis was evaluated using previously described methods [29].
We performed Kaplan-Meier survivorship analysis at 15 and 20 years using data from the entire cohort with revision for any reason or radiographic loosening as the end point. In cases in which revision surgery had been performed, we reviewed operative reports and the prerevision radiographs to determine the cause of failure. When possible, the explanted components and/or pathology reports were also obtained to confirm the cause of failure.
Results
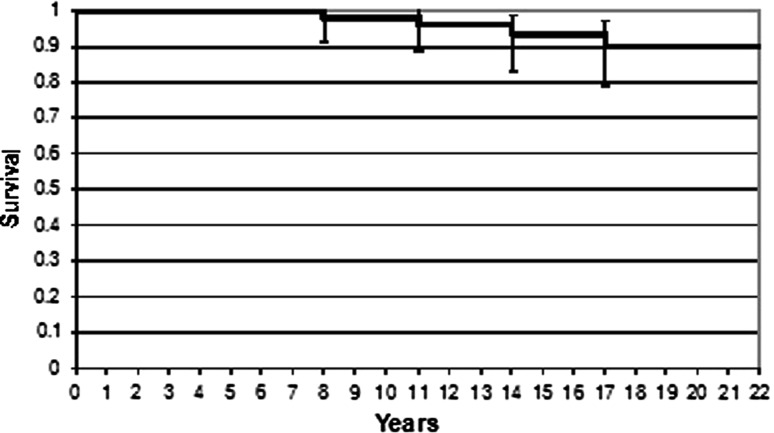
Kaplan-Meier survival analysis of all 62 knees in the original cohort revealed a 15-year survivorship free of revision for any reason of 93% (95% CI, 83%–98%) and a 20-year survivorship of 90% (95% CI, 79%–96%; Fig. 1). Four of 62 knees were revised at a mean of 144 months (range, 87–204 months).
Fig. 1.
Kaplan-Meier survivorship curve (and 95% CI) with revision for any reason as the end point. The cumulative survival rate is 93% (95% CI, 83%–98%) at 15 years and 90% (95% CI, 79%–96%) at 20 years.
At last followup, nine patients (11 knees) had > 85 points on the HSS scale, one patient (one knee) 76 points, and four patients (four knees) < 60 points (Table 2). Of the four patients with scores below 60, one had a neurological disorder, one had intractable back pain, and two had osteoarthritis in multiple joints.
Table 2.
A comparison of HSS scores at each of the three followup periods
| Clinical result (HSS score) | Minimum 6-year followup (N = 51) | Minimum 10-year followup (N = 49) | Minimum 15-year followup (N = 16) |
|---|---|---|---|
| 85–100 points | 40 (78%) | 39 (80%) | 11 (69%) |
| 70–84 points | 10 (20%) | 6 (12%) | 0 (0%) |
| 60–69 points | 1 (2%) | 4 (8%) | 1 (6%) |
| ≤ 59 points | 0 (0%) | 0 (0%) | 4 (25%)* |
* Each patient with an HSS ≤ 59 score had additional medical comorbidities that contributed to poor functional scores (see Results); HSS = Hospital for Special Surgery.
No patient had radiographic evidence of component loosening or osteolysis. In our prior report, three knees had a complete radiolucent line at the bone-cement interface of the tibial component; two of these knees were in one patient who died before 15 years without associated symptoms, and the third was in a patient with a knee score at most recent followup of 94 points who refused further radiographic evaluation. It is thus unknown if this knee was well fixed or loose but stable and asymptomatic.
Two of the five failures were described at a minimum of 10 years [4, 5]; however, further investigation into the reasons for revision was performed to confirm the mode of failure. The first revision was performed at 87 months at an outside hospital. The operative report and prior article identified persistent pain and patellofemoral arthritis as the causes of failure. Radiographs revealed Grade 1 changes of the patellofemoral and lateral compartments at both 3 and 84 months (no interval change); thus, the reason for revision is unclear. The operative report of the second patient revised at 127 months identified patellofemoral and lateral compartment arthritis as the reason for revision. Radiographs performed 56 months postoperatively showed evidence of metallosis that was confirmed with the pathology report from the revision procedure. Examination of the explanted components suggested the polyethylene liner had dislodged or had never been engaged properly, suggesting arthritis progression was not the cause of failure. Two knees were revised since the prior report at 157 months and 204 months. The revision at 157 months was performed for patellofemoral and lateral compartment degeneration that was confirmed radiographically with Grade 4 changes of the patellofemoral articulation and Grade 2 changes of the lateral compartment seen on prerevision radiographs. The patient revised at 204 months had a history of a prior high tibial osteotomy. Immediate postoperative radiographs showed a tibiofemoral mechanical axis of 7° of valgus, and prerevision radiographs confirmed Grade 3 lateral compartment progression; she had Grade 2 lateral compartment changes in our previous report. Although this suggests lateral compartment disease progression as the potential cause of failure, it also suggests a technical error in alignment at the time of the index surgical procedure. All components were well fixed at the time of revision.
All nine knees with radiographic evaluation at a minimum of 15 years had evidence of deterioration in the adjacent tibiofemoral compartment and/or the patellofemoral compartment (Tables 3, 4). One patient who had Grade 4 adjacent compartment changes had an HSS knee score of 76 points at 252 months. Two patients had Grade 4 changes of the patellofemoral compartment. They had HSS scores of 91 and 86 at 204 and 234 months of followup, respectively.
Table 3.
The rate of radiographic patellofemoral arthritic progression at each of the three followup periods
| Grade | Minimum 6-year followup (N = 51) | Minimum 10-year followup (N = 49) | Minimum 15-year followup (N = 9) |
|---|---|---|---|
| No progression | 36 (71%) | 28 (57%) | 1 (11%) |
| Grade 1 | 12 (24%) | 13 (27%) | 3(33%) |
| Grade 2 | 3 (6%) | 1 (2%) | 3 (33%) |
| Grade 3 | 0 (0%) | 3 (6%) | 0 (0%) |
| Grade 4 | 0 (0%) | 4 (8%) | 2 (22%) |
Table 4.
The rate of radiographic adjacent tibiofemoral compartment arthritic progression at each of the three followup periods
| Adjacent compartment progression | Minimum 6-year followup (N = 51) | Minimum 10-year followup (N = 49) | Minimum 15-year followup (N = 9) |
|---|---|---|---|
| No progression | 31 (61%) | 21 (43%) | 3 (33%) |
| Grade 1 | 12 (24%) | 19 (39%) | 2 (22%) |
| Grade 2 | 4 (8%) | 6 (12%) | 1 (11%) |
| Grade 3 | 1 (2%) | 3 (6%) | 2 (22%) |
| Grade 4 | 0 (0%) | 0 (0%) | 1 (11%) |
Discussion
Our goal was to determine, at a minimum followup of 15 years, (1) the overall durability and survivorship of this UKA design; (2) modes of failure; and (3) the progression of arthritis in the nonresurfaced compartments. Studies examining the results of UKA into the second decade of use have reported failure rates ranging from 3% to 35% (Table 5), whereas we report a failure rate of 6% (four of 62). Although we observed no failures resulting from aseptic loosening, others have reported long-term aseptic loosening rates ranging from 0.5% to 18% [4, 7, 10, 13, 21, 24, 25, 31, 37–40]. Finally, although we found that all patients with radiographic followup had arthritic progression in the nonresurfaced compartments, in only two cases (4%) did this progression require revision. In comparison, other long-term series have reported failure resulting from arthritic progression to range from 3% to 9% [4, 7, 10, 13, 21, 24, 25, 31, 37–40].
Table 5.
Studies of unicompartmental knee arthroplasty with minimum 10-year followup
| Study | Year | Number of UKAs | Minimum followup (years) (mean) |
Prosthesis design | Bearing | Number of failures (%) | Reason for failure | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Patellofemoral | Adjacent tibiofemoral | Aseptic loosening | Other* |
|||||||
| Marmor [21] | 1988 | 60 | 10 (11) | Marmor | Fixed | 21 (35%) | 2% | 3% | 18% | 12% |
| Weale and Newman [40] | 1994 | 42 | 12 (N/A) | St George Sled | Fixed | 5 (12%) | N/A | N/A | N/A | N/A |
| Cartier et al. [7] | 1996 | 60 | 10 (12) | Marmor | Fixed | 9 (15%) | 0 | 3% | 2% | 10% |
| Squire et al. [37] | 1999 | 140 | 15 (17) | Marmor | Fixed | 14 (10%) | 0 | 5% | 4% | 1% |
| Svard and Price [39] | 2001 | 124 | 10 (13) | Oxford | Mobile | 6 (5%) | 0 | 0 | 2% | 3% |
| Hernigou and Deschamps [10] | 2002 | 99 | 10 (14) | Lotus | Fixed | 22 (22%) | 1% | 3% | 17% | 1% |
| Khan et al. [13] | 2004 | 30 | 10 (N/A) | St George Sled | Fixed | 2 (7%) | 0 | 0 | 3% | 3% |
| Price et al. [31] | 2005 | 114 | 10 (N/A) | Oxford | Mobile | 24 (21%) | 0 | 9% | 5% | 7% |
| Berger et al. [4] | 2005 | 62 | 10 (N/A) | Miller-Galante | Fixed | 2 (3%) | 3% | 0 | 0 | 0 |
| O’Rourke et al. [25] | 2005 | 136 | 21 (N/A) | Marmor | Fixed | 19 (14%) | N/A | 7%† | 6% | 1% |
| Steele et al. [38] | 2006 | 203 | 10 (15) | St George Sled | Fixed | 16 (8%) | 0.5% | 3% | 0.5% | 4% |
| Newman et al. [24] | 2009 | 24 | 15 (15) | St George Sled | Fixed | 4 (17%) | 0 | 8% | 4% | 4% |
| Foran et al. (current study) | 2011 | 62 | 15 (19) | Miller-Galante | Fixed | 4 (6%) | 2% | 2% | 0 | 4% |
* Other causes include: infection, arthrofibrosis, recurrent hemarthrosis, dislocation, instability, polyethelene wear, component fracture, unexplained pain; †the location of disease progression (patellofemoral versus tibiofemoral) not specified; N/A = not available.
There are several limitations of this study. First, because of the length of followup, a large proportion of the original cohort died. This large death rate inherently undermines the analyses that follow; however, we made every effort to understand the function of each knee at the time of death based on family member descriptions and latest progress notes. It is conceivable that this methodology may have missed radiographic loosening or subtle clinical failure based on poor observations and/or incomplete recollection by family members. The high death rate in this cohort also calls into question the generalizability of our findings to that of a younger, more active cohort of patients in which a higher percentage would be expected to be alive at 15 to 20 years of followup. Second, like any retrospective study, certain data points were incomplete. Some patients were interviewed by telephone only, and we were unable to obtain the latest radiographs for all patients. Third, AP and merchant patellar views of the knee are dependent on the degree of knee flexion as well as the angle of the xray beam, and therefore measurement of tibiofemoral and patellofemoral degeneration is inherently difficult to accurately interpret. Several authors independently evaluated the radiographs to help minimize this issue. The lack of complete radiographic followup on all patients is a major limitation of this study, and therefore the finding that there were no cases of radiographic loosening must interpreted with caution, because some cases of loosening may have been missed. Finally, there are inherent limitations in the HSS scoring system, because comorbidities are not well accounted for but can substantially affect the final scores.
We found 15- and 20-year survivorship free of revision of 93% and 90%, respectively, in this series using this cemented, fixed-bearing UKA design. With a mean followup of 15 years, four patients (6%) out of the original cohort of 62 underwent revision, and no knees failed secondary to aseptic loosening. The majority (67%) of patients in this series died with well-functioning knees, illustrating the durable long-term survivorship of UKA in this older patient population. The survivorship of this cohort compares favorably with the survivorship reported in recent long-term TKA studies [1, 17] as well as other long-term UKA studies [4, 7, 10, 13, 21, 24, 25, 30, 37–40] (Table 5). When comparing the results of this cohort with that of other TKA and UKA cohorts, it is important to take into account the key characteristics of the current population (including age and selection criteria), and as such, the generalizability of our findings should be undertaken with caution. Several factors likely contributed to the excellent long-term durability in this series. First was the conservative selection on the basis of the criteria of Kozinn and Scott [16]. Exclusion criteria included inflammatory arthritis, patients with anterior knee pain, knee instability, or intraoperative identification of greater than Outerbridge 2 degeneration of the patellofemoral or opposite tibiofemoral compartment. Additionally, the average age of patients in our cohort was relatively old (mean age, 68 years) and as such, activity levels, although not explicitly measured, were likely to be moderate in our population. Additionally, undercorrection of sagittal deformity and avoidance of anterior placement of femoral component (or oversizing the femoral component) to avoid patellofemoral impingement [10, 20, 36] likely played important roles as well. It is notable that all four knees with Grade 4 patellofemoral changes demonstrated evidence of impingement of the patella against the femoral component [10].
Various modes of failure of UKA have been reported [2, 9, 21, 24, 25, 38], including adjacent tibiofemoral compartment or patellofemoral compartment degeneration, aseptic loosening, polyethylene wear, mechanical failure, and infection. In many studies, unfortunately, the exact mode of failure is difficult for the reader to determine. In our present report, further review of prior reported failures revealed the stated causes of failure were not supported by the prerevision radiographs, pathology reports, and/or examination of the explanted components. Although we previously reported both failures as related to patellofemoral degeneration, in one case, degeneration of the nonresurfaced compartments could not be confirmed, and the patient seems to have been revised for pain alone, and in the second, disengagement of the polyethylene liner (possibly the result of technical error) occurred leading to metallosis. The available data from large registries [14, 15, 34] consistently show a higher rate of revision for UKA as opposed to TKA. This may be explained by surgeons and patients alike having a lower threshold for revising a partial as opposed to a TKA. In the two failures noted since the prior report, one was related to patellofemoral progression and the second appeared to have been associated with overcorrection of deformity in a patient with a prior high tibial osteotomy leading to lateral compartment disease. Previous literature has shown failure rates of UKA after high tibial osteotomy as high as 28%, particularly in the setting of valgus alignment of the extremity [32].
Progression of arthritis in the nonresurfaced compartments is a common concern for both patients and surgeons. The rates of patellofemoral progression in reported series of the Miller-Galante UKA range from 17% to 60% [3, 5, 18, 27, 28]. However, in long-term (> 10-year) studies of UKA of multiple designs, the failure rate resulting from arthritic progression of either the patellofemoral and/or adjacent tibiofemoral compartment is lower and ranges from 3% to 9% [4, 7, 10, 13, 21, 24, 25, 31, 37–40]. This indicates that arthritic progression does not necessarily portend poor outcomes. This is in keeping with our findings because although all knees with minimum 15-year radiographic followup had evidence of adjacent tibiofemoral compartment or patellofemoral compartment degeneration, most patients who had radiographic evidence of progression did not have associated clinical symptoms that necessitated further surgery. Only two failures (3%) in this cohort were secondary to arthritic progression. Furthermore, two patients who had Grade 4 changes (> 50% joint space loss) had knee scores greater than 90 points, and the third had a score of 76 points.
Based on our findings and a synthesis of the literature, we continue to use a cemented, fixed-bearing UKA with a metal-backed tibial component for patients who present with unicompartmental osteoarthritis or osteonecrosis. The 93% survivorship at 15 years reported in our series is likely in large part the result of our conservative indications. It remains to be determined how broadening the indications, especially with regard to age and adjacent and/or patellofemoral disease, affects the long-term survivorship.
Our findings suggest that, with conservative selection criteria, and in this older patient population (mean age, 68 years), the 15-year survivorship of fixed-bearing UKA is similar to that of TKA. Although arthritic progression in the nonresurfaced compartments appears common at long-term followup, most progression is low grade, and high-grade progression is not necessarily associated with clinical symptoms and thus does not necessarily lead to revision.
Footnotes
The institution of one or more of the authors (CJDV, RAB, JOG) has received, in any one year, funding from Zimmer (Warsaw, IN, USA), Smith & Nephew (Memphis, TN, USA), and Stryker (Kalamazoo, MI, USA). One of the authors (CJDV) certifies that he has or may receive payments or benefits, during the study period of an amount of less than $10,000 from Biomet (Warsaw, IN, USA), and less than $100,000 from Smith & Nephew. One of the authors (RAB) certifies that he certifies that he has or may receive payments or benefits, during the study period of an amount of $10,000–$100,000 from Medtronic (Memphis, TN, USA), more than $1,000,001 from Zimmer, less than $10,000 from Smith & Nephew, and less than $10,000 from DePuy (Warsaw, IN, USA). One of the authors (JOG) certifies that he certifies that he has or may receive payments or benefits, during the study period of an amount of less than $10,000 from Biomet and more than $1,000,001 from Zimmer.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Rush University Medical Center, Chicago, IL, USA.
Contributor Information
Jared R. H. Foran, Email: jaredforan@yahoo.com.
Craig J. Della Valle, Email: craigdv@yahoo.com.
References
- 1.Abdeen AR, Collen SB, Vince KG. Fifteen-year to 19-year follow-up of the Insall-Burstein-1 total knee arthroplasty. J Arthroplasty. 2010;25:173–178. doi: 10.1016/j.arth.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Ansari S, Newman JH, Ackroyd CE. St. Georg sledge for medial compartment knee replacement. 461 arthroplasties followed for 4 (1–17) years. Acta Orthop Scand. 1997;68:430–434. doi: 10.3109/17453679708996257. [DOI] [PubMed] [Google Scholar]
- 3.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002;84:2235–2239. [PubMed] [Google Scholar]
- 4.Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006. doi: 10.2106/JBJS.C.00568. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Meneghini RM, Sheinkop MB, Della Valle CJ, Jacobs JJ, Rosenberg AG, Galante JO. The progression of patellofemoral arthrosis after medial unicompartmental replacement: results at 11 to 15 years. Clin Orthop Relat Res. 2004;428:92–99. doi: 10.1097/01.blo.0000147700.89433.a5. [DOI] [PubMed] [Google Scholar]
- 6.Berger RA, Nedeff DD, Barden RM, Sheinkop MM, Jacobs JJ, Rosenberg AG, Galante JO. Unicompartmental knee arthroplasty. Clinical experience at 6- to 10-year followup. Clin Orthop Relat Res. 1999;367:50–60. doi: 10.1097/00003086-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty. 1996;11:782–788. doi: 10.1016/S0883-5403(96)80177-X. [DOI] [PubMed] [Google Scholar]
- 8.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 9.Gioe TJ, Killeen KK, Hoeffel DP, Bert JM, Comfort TK, Scheltema K, Mehle S, Grimm K. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003;416:111–119. doi: 10.1097/01.blo.0000093004.90435.d1. [DOI] [PubMed] [Google Scholar]
- 10.Hernigou P, Deschamps G. Patellar impingement following unicompartmental arthroplasty. J Bone Joint Surg Am. 2002;84:1132–1137. doi: 10.2106/00004623-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Insall J, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am. 1980;62:1329–1337. [PubMed] [Google Scholar]
- 12.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 13.Khan OH, Davies H, Newman JH, Weale AE. Radiological changes ten years after St Georg Sled unicompartmental knee replacement. Knee. 2004;11:403–407. doi: 10.1016/j.knee.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V. Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop. 2008;79:499–507. doi: 10.1080/17453670710015490. [DOI] [PubMed] [Google Scholar]
- 15.Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128–135. doi: 10.1080/17453670610013538. [DOI] [PubMed] [Google Scholar]
- 16.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71:145–150. [PubMed] [Google Scholar]
- 17.Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement. A concise follow-up of a previous report. J Bone Joint Surg Am. 2009;91:1419–1423. doi: 10.2106/JBJS.H.01351. [DOI] [PubMed] [Google Scholar]
- 18.Li MG, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D. Mobile vs fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee. 2006;13:365–370. doi: 10.1016/j.knee.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Lindstrand A, Stenstrom A, Lewold S. Multicenter study of unicompartmental knee revision. PCA, Marmor, and St Georg compared in 3777 cases of arthrosis. Acta Orthop Scand. 1992;63:256–259. doi: 10.3109/17453679209154777. [DOI] [PubMed] [Google Scholar]
- 20.Marmor L. Marmor modular knee in unicompartmental disease. Minimum four-year follow-up. J Bone Joint Surg Am. 1979;61:347–353. [PubMed] [Google Scholar]
- 21.Marmor L. Unicompartmental arthroplasty of the knee with a minimum ten-year follow-up period. Clin Orthop Relat Res. 1988;228:171–177. [PubMed] [Google Scholar]
- 22.Mercier N, Wimsey S, Saragaglia D. Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty. Int Orthop. 2010;34:1137–1143. doi: 10.1007/s00264-009-0869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80:983–989. doi: 10.1302/0301-620X.80B6.8177. [DOI] [PubMed] [Google Scholar]
- 24.Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009;91:52–57. doi: 10.1302/0301-620X.91B1.20899. [DOI] [PubMed] [Google Scholar]
- 25.O’Rourke MR, Gardner JJ, Callaghan JJ, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC. The John Insall Award: unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27–37. doi: 10.1097/01.blo.0000185451.96987.aa. [DOI] [PubMed] [Google Scholar]
- 26.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 27.Parratte S, Argenson JN, Pearce O, Pauly V, Auquier P, Aubaniac JM. Medial unicompartmental knee replacement in the under-50 s. J Bone Joint Surg Br. 2009;91:351–356. doi: 10.1302/0301-620X.91B3.21588. [DOI] [PubMed] [Google Scholar]
- 28.Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2003;85:1968–1973. doi: 10.2106/00004623-200310000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Peters PC, Jr, Engh GA, Dwyer KA, Vinh TN. Osteolysis after total knee arthroplasty without cement. J Bone Joint Surg Am. 1992;74:864–876. [PubMed] [Google Scholar]
- 30.Price AJ, Dodd CA, Svard UG, Murray DW. Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br. 2005;87:1488–1492. doi: 10.1302/0301-620X.87B11.16324. [DOI] [PubMed] [Google Scholar]
- 31.Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;435:171–180. doi: 10.1097/00003086-200506000-00024. [DOI] [PubMed] [Google Scholar]
- 32.Rees JL, Price AJ, Lynskey TG, Svard UC, Dodd CA, Murray DW. Medial unicompartmental arthroplasty after failed high tibial osteotomy. J Bone Joint Surg Br. 2001;83:1034–1036. doi: 10.1302/0301-620X.83B7.11827. [DOI] [PubMed] [Google Scholar]
- 33.Riddle DL, Jiranek WA, McGlynn FJ. Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty. 2008;23:408–412. doi: 10.1016/j.arth.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 34.Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L. Use of unicompartmental instead of tricompartmental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative. 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthop Scand. 1999;70:170–175. doi: 10.3109/17453679909011257. [DOI] [PubMed] [Google Scholar]
- 35.Schneider R, Freiberger RH, Ghelman B, Ranawat CS. Radiologic evaluation of painful joint prostheses. Clin Orthop Relat Res. 1982;170:156–168. [PubMed] [Google Scholar]
- 36.Scott RD, Cobb AG, McQueary FG, Thornhill TS. Unicompartmental knee arthroplasty. Eight- to 12-year follow-up evaluation with survivorship analysis. Clin Orthop Relat Res. 1991;271:96–100. [PubMed] [Google Scholar]
- 37.Squire MW, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Unicompartmental knee replacement. A minimum 15 year followup study. Clin Orthop Relat Res. 1999;367:61–72. doi: 10.1097/00003086-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Steele RG, Hutabarat S, Evans RL, Ackroyd CE, Newman JH. Survivorship of the St Georg Sled medial unicompartmental knee replacement beyond ten years. J Bone Joint Surg Br. 2006;88:1164–1168. doi: 10.1302/0301-620X.88B9.18044. [DOI] [PubMed] [Google Scholar]
- 39.Svard UC, Price AJ. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br. 2001;83:191–194. doi: 10.1302/0301-620X.83B2.10966. [DOI] [PubMed] [Google Scholar]
- 40.Weale AE, Newman JH. Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clin Orthop Relat Res. 1994;302:134–137. [PubMed] [Google Scholar]