Abstract
Background
Wear of total knee polyethylene has been quantified gravimetrically with thickness measurements and evaluation of surface wear modes. However, these techniques do not localize volumetric wear.
Questions/Purposes
We used micro-CT scans of retrieved total knee liners and unworn, new liners to determine the volume and location of wear.
Methods
We retrieved 12 fixed and 12 rotating-platform bearings after a mean 52 months of use. Inserts were weighed and thickness was measured. Micro-CT scans of retrieved and matched new liners were superimposed to compare the location and magnitude of wear.
Results
The average total wear was 254 ± 248 mm3. The average wear rate was 58 ± 41 mm3/year. Wear was 69% of penetration, demonstrating the contribution of deformation to knee wear. Rotating-platform wear rate was 43 ± 25 mm3/year and the fixed-bearing rate was 74 ± 49 mm3/year. Five percent of the rotating-platform wear rate came from the backside compared with 14% of the fixed-bearing wear rate.
Conclusions
Micro-CT can determine the volume and location of wear of retrieved tibial liners. Because the magnitude of the manufacturing tolerances was approximately half the magnitude of the total wear on average, accounting for the potential influence of tolerances is important to accurately measure volumetric wear if the unworn (preimplantation) geometry of the insert is unknown. Without accounting for tolerances, this technique may not be applicable for retrievals with a short followup that have low wear. However, application of micro-CT could be of value in determining the exact location of wear in knee simulator studies in which the same insert is measured repeatedly and manufacturing tolerances are not a concern.
Introduction
Analysis of in vivo and in vitro total knee wear is critical for developing better TKAs. In vivo radiographic measurements of condylar penetration over time have been correlated to various patient characteristics [6, 10, 13]. However, measures of condylar penetration do not allow an analysis of penetration volume and are not necessarily an accurate measure of true wear because penetration does not account for creep or deformation. Analysis of retrieved components either at revision or postmortem allows the analysis of surface damage and changes in polyethylene thickness [4, 7, 8, 10–12, 16]. Retrieval analysis is inherently more accurate and detailed than radiographic analysis of condylar penetration and does provide more insight into wear. Unfortunately, volumetric analysis of retrieved tibial polyethylene components is rarely performed. When three-dimensional retrieval analysis is performed, it has been limited in the ability to separate wear from penetration because the volumetric calculation is typically based on shapes generated from multiple penetration measurements [1, 2, 9, 14, 15].
High-resolution micro-CT has been used to evaluate articular surface penetration of in vivo worn hip polyethylene [5]. Micro-CT has also been used and validated as a tool to measure simulator worn tibial polyethylene components [21]. Micro-CT scans of polyethylene before and after knee simulator wear were used to create three-dimensional models of the polyethylene liner. An additional biomedical imaging software program then allowed comparison of the unworn and worn three-dimensional images. The technique was validated by comparing the weight difference of the unworn and worn polyethylene with the calculated wear determined by the three-dimensional micro-CT image and matching software. The advantage of this technique over a gravimetric method is the ability to analyze the location and pattern of wear. Gravimetric techniques only determine weight change and used alone cannot determine the location of wear. A technique that overlaid micro-CT-generated three-dimensional models of retrieved worn and matched new tibial inserts could allow the separate determination of articular surface and backside polyethylene wear. This technique could have application to analysis of both retrieved and simulator worn liners focusing on the effect of locking mechanisms and varied articular surface congruence on the wear occurring at both sides of a tibial polyethylene.
Although simulator wear analysis is important, it represents a well-controlled environment. On the other hand, analysis of retrieved polyethylene represents real-life patient use and is generally agreed to be more helpful than simulator studies. One difficulty applying micro-CT and three-dimensional matching software to retrieval wear analysis is the availability of an unworn control polyethylene to be compared with a retrieved polyethylene. If unworn polyethylene or a three-dimensional model of an unworn liner was used as a control, there would still be the issue of manufacturing tolerances, which could influence the determination of wear volume. The magnitude of differences in volume as a result of manufacturing tolerances may or may not influence the application of micro-CT analysis of in vivo worn, retrieved tibial polyethylene inserts.
We used micro-CT to determine the location and magnitude of wear from revision retrieved fixed-bearing and rotating-platform tibial polyethylene inserts. First we wanted to determine the influence manufacturing tolerances would have on the determination of wear in revision retrieved inserts with this technique. We also wanted to compare rotating-platform and fixed-bearing retrieved tibial inserts. Specifically we compared condylar penetration, polyethylene deformation, and wear of the two types of knee bearings. We also compared articular surface and backside wear for the two types of bearings.
Patients and Methods
We evaluated 24 retrieved tibial components obtained from our implant retrieval laboratory. We chose implants that were in situ for more than 12 months from a single manufacturer that was able to provide matching new liners from their existing inventory. Selection of the implants was further influenced by the process of matching on patient sex, age, height, weight, revision diagnosis, and time in vivo. The selection process described was chosen to limit differences between manufacturers and patients allowing a better comparison of fixed-bearing and rotating-platform designs. The components included 12 rotating-platform and 12 fixed-bearing inserts (Table 1). New polyethylene inserts were obtained from the manufacturer based on product numbers. All inserts were cleaned and stored at room temperature. Twenty-four control and 24 retrieved tibial polyethylene inserts were scanned. Funding for the study was provided by DePuy (Warsaw, IN, USA). Institutional review board approval was obtained because protected patient data were used. All implants used for this study were FDA-approved.
Table 1.
Patient and implant data
| Parameter | Rotating platform | Fixed bearing | p value |
|---|---|---|---|
| Sex | 8 female 4 male |
8 female 4 male |
1.0 |
| Age at surgery (years)* | 59.1 ± 12.2 [57] (39–76) |
60.8 ± 12.6 [61] (40–79) |
0.59 |
| Age at revision (years)* | 63.4 ± 13.0 [62] (43–85) |
65.2 ± 13.1 [65] (45–84) |
0.65 |
| Time in situ (months) | 52 ± 31 [45] (13–107) |
53 ± 32 [59] (12–108) |
0.84 |
| Weight (kg)* | 85 ± 14 [89] (59–104) |
89 ± 23 [100] (54–112) |
0.32 |
| Height (cm)* | 168 ± 9 [168] (157–183) |
166 ± 9 [165] (150–178) |
0.61 |
| Bearing type | 9 cruciate-retaining 3 posterior-stabilized |
9 cruciate-retaining 3 posterior-stabilized |
1.0 |
| Retrieval type | 11 revision 1 postmortem |
12 revision | 1.0 |
| Reasons for revision | 3 loose tibia 3 loose femur 1 loose tibia and femur 2 stiffness 1 osteolysis 1 infection |
4 loose tibia 3 loose femur 3 failed patella 2 stiffness |
0.41 |
| Implant design | 9 LCS 3 Sigma RP |
12 PFC Sigma | < 0.001 |
| Sterilization | 3 gamma-barrier 9 gas plasma |
12 gamma-barrier | < 0.001 |
| Polyethylene resin | 3 GUR 1020 9 GUR 1050 |
12 GUR 1020 | < 0.001 |
| Tibial baseplate | Polished chrome-cobalt | Grit-blasted titanium | < 0.001 |
* Data include the mean ± SD [median] (range).
The inserts were scanned at 80 kVp and 450 μA with an isotropic voxel resolution of 92 μm (0.0036 inches) and a 1024 × 1024 in-plane image matrix at the Cleveland Clinic (ImageIQ, Cleveland, OH, USA) using a high-resolution micro-CT scanner (GE eXplore Locus; GE Healthcare, Waukesha, WI, USA). When the mediolateral dimension of an insert exceeded 9.4 cm, serial scans were obtained and subsequently stitched together to reconstruct the entire specimen geometry. Microview Image Analysis Software Version 2.2 (GE Healthcare) was used to filter the reconstructed image data using a 3 × 3 × 3 Gaussian smoothing filter. The DICOM-formatted image data were then imported into three-dimensional image analysis software developed by the Mayo Clinic’s Biomedical Imaging Resource (Analyze 9.0; AnalyzeDirect, Inc, Overland Park, KS, USA) that was used to reconstruct the three-dimensional insert geometry. Although the Gaussian smoothing filter is useful for suppressing normal image noise, it cannot eliminate image artifacts associated with metal pins that were embedded in the Low Contact Stress (DePuy) rotating-platform retrieved inserts. When present, these residual image artifacts were manually removed from each image slice.
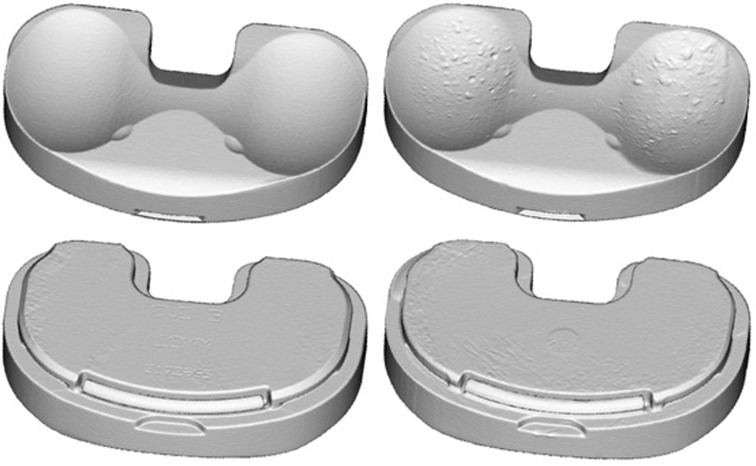
Three-dimensional geometries for the retrieved and control inserts were created by segmenting the polyethylene from the background using a threshold Hounsfield value that defined each voxel in the image as either polyethylene or background air (Fig. 1). The threshold value used for each image was chosen so that the volume of the polyethylene from the micro-CT image data matched the volume of the actual insert calculated by dividing the weight of the specimen by the nominal density of the polyethylene. A nominal density of 935 kg/m3 was used for extruded GUR 1020 inserts and 931 kg/m3 was used for extruded GUR 1050 inserts. The accuracy and error associated with this imaging technique have been previously reported [21].
Fig. 1.
Three-dimensional rendered image of a control insert (left) and retrieved insert (right). Notice the visible implant identifiers on the backside of the control (lower left). Likewise, the absence of identifiers and the unworn central tray hole on the backside of the retrieval (lower right).
Using the Analyze software, one of the authors (RLZ) who was not a surgeon manually superimposed the worn and control insert geometries at the unworn intercondylar eminence on the femoral articulating side of both liners. The superimposed images were visually inspected to check for the conformity along other surfaces including the peripheral (lateral) edges and backside surface. To account for the possible influence of manufacturing tolerances and in vivo polyethylene expansion resulting from fluid absorption, if the peripheral edges of the control insert were uniformly outside or inside the boundaries of the retrieved insert, the control insert was dilated or eroded to match the geometry of the retrieved insert. Additionally, in three cases in which the backside of the control insert was uniformly larger or smaller than the retrieved insert and the machining marks on the backside surface of the retrieved insert were present or the uniform geometrical differences between the control and retrieval extended across contacting and noncontacting portions of the backside surface (such as chamfers), the backside surface of the processed control was uniformly dilated or eroded by a single slice (92 μm) to match the retrieved insert backside surface. The net change from this process resulted in 15 cases in which the control was dilated because it was slightly smaller than the retrieval and seven cases in which the control was eroded because it was slightly larger than the retrieval. Although we might erode or dilate the lateral edges and backside surfaces, the topside articular surface was never modified. The mean change in volume from this process was 0.4% ± 0.5% (range, 0.2% erosion to 1.1% dilation) of the control volume or 136 ± 142 mm3. Without this adjustment, 15 cases would have had decreased wear and seven would have had inflated wear.
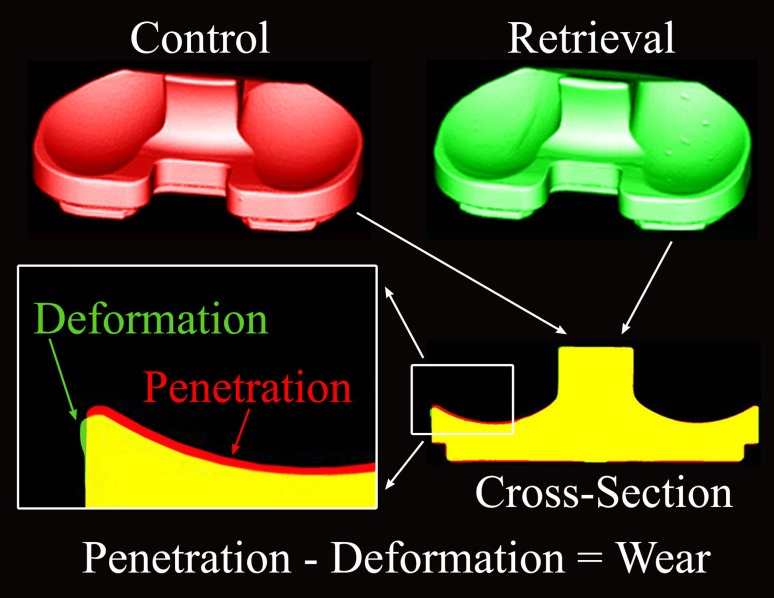
We defined penetration as the volume of polyethylene from the control insert that is outside the boundary of the retrieved insert. Deformation is defined as the volume of polyethylene from the retrieved insert that is outside the boundaries of the control. It follows that wear (material lost from the control) is defined as penetration minus deformation (Fig. 2).
Fig. 2.
Definitions of penetration, deformation, and wear are shown.
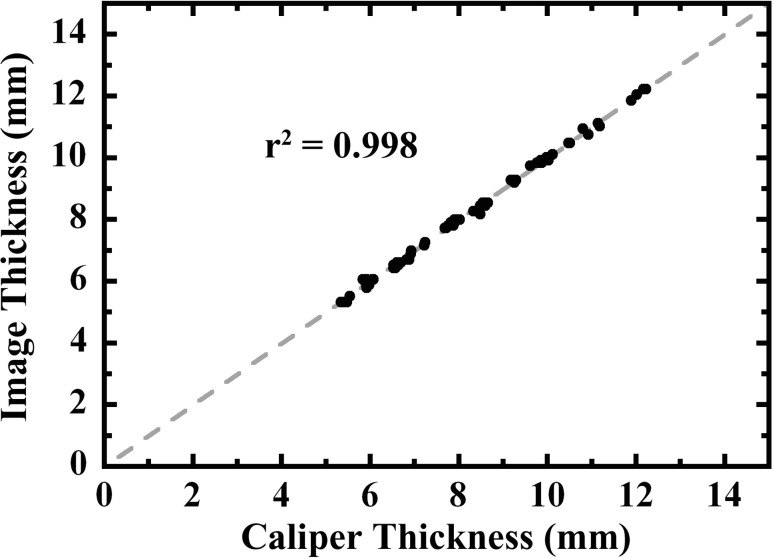
To validate the technique, physical measurements of the polyethylene liners were compared with measurements made with the micro-CT technique described. The thickness of each retrieved and control insert was measured by sampling the surface until the thinnest location in both the medial and lateral compartment was determined and measured with digital calipers (Mitoyo, Tokyo, Japan). The location of the measurement was recorded so that the same location could be measured on the micro-CT scan. We observed a very strong correlation (r2 = 0.998, p < 0.001) between all of the caliper and micro-CT thickness measurements (Fig. 3). The Bland and Altman Limits of Agreement [3], corresponding to an interval containing 95% of the differences between the physical caliper and micro-CT image measurements, ranged from −0.16 mm to 0.16 mm.
Fig. 3.
A strong correlation (p < 0.001) was found comparing insert thickness measured with calipers versus insert thickness based on three-dimensional reconstructions derived from micro-CT images. The dashed gray line represents perfect agreement. Ninety-five percent of the differences between the measurements fell within an interval ranging from −0.16 mm to 0.16 mm.
To apply the technique, we compared the total penetration, deformation, and wear values for the rotating-platform and fixed-bearing implants. Each registered three-dimensional image was divided into topside and backside regions to allow rotating-platform to fixed-bearing comparisons. Rates were determined by dividing volumetric measurements by time in vivo.
Linear regression was used to evaluate the relationship between the raw wear volumes (computed without accounting for manufacturing tolerances) and the adjusted wear volumes. Owing to the nonparametric distribution of wear data, comparisons of rotating-platform to fixed-bearing penetration, deformation, wear, and comparisons of topside and backside wear were evaluated using a Mann-Whitney U test. All statistical analyses were performed using SPSS (Statistical Package for the Social Sciences, Chicago, IL, USA).
Results
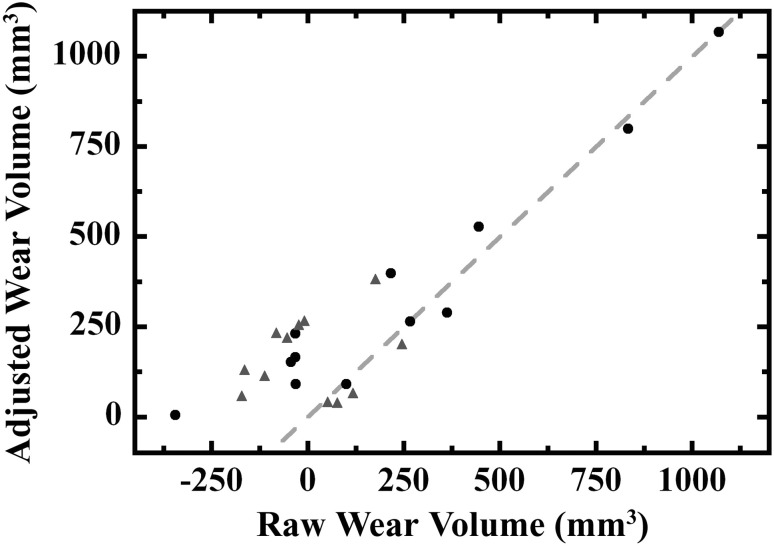
Because manufacturing tolerances required adjustments to the control shape and volume, we have included a comparison of the unadjusted or raw wear to the wear we calculated after accounting for tolerances, which allows readers to see how many cases would have had negative wear and the magnitude of the correction (Fig. 4). The regression equation for this comparison is - adjusted volume = 0.71*raw volume + 170 mm3, r2 = 0.81, p < 0.001.
Fig. 4.
A strong correlation (r = 0.90, p < 0.001) was found between the raw wear volume (calculated without adjusting the control insert geometry for manufacturing tolerances) and the adjusted wear volume (obtained after eroding or dilating the control to account for tolerances). Although 12 of 24 cases had negative raw wear volumes, the same trend toward lower wear with rotating-platform inserts (gray triangles) compared with fixed-bearing inserts (black circles) was observed whether manufacturing tolerances were accounted for or ignored. The dashed gray line represents equivalent raw and adjusted wear volumes that occurred when there was no net erosion or dilation of the control. Points above and to the left of the dashed line represent cases where the control was dilated. Points below and to the right of the dashed line represent cases where the control was eroded.
We found an average wear rate of 58 ± 41 mm3/year for all polyethylenes in the study (Table 2). On average, wear was 69% of penetration demonstrating the contribution of deformation to knee wear. Penetration correlated with (r = 0.73, p < 0.001) deformation. Although rotating-platform penetration (p = 0.01) and deformation (p < 0.001) were less than measured in fixed bearing, the wear was not statistically different (p = 0.16). These findings were the same when penetration (p = 0.004), deformation (p < 0.001), and wear (p = 0.14) were reported as rates based on the time in situ. Although the wear was not statistically different, Figure 4 shows the trend for lower rotating-platform wear and that the trend existed with or without adjustment for manufacturing tolerances. The backside rotating-platform and fixed-bearing wear rates were similar (p = 0.80, 2 ± 8 mm3/year and 10 ± 31 mm3/year, respectively). Evaluating the location of wear, we discovered average backside wear rate accounted for 5% of the rotating-platform wear and 5% of rotating-platform wear rate on average compared with 24% of fixed-bearing backside wear and 14% of fixed-bearing wear rate.
Table 2.
Micro-CT data for rotating platform, fixed bearing, and combined data
| Parameter | Rotating platform | Fixed bearing | p value | All | |
|---|---|---|---|---|---|
| Wear | Volume (mm3) | 167 ± 109 [166] (39–382) |
341 ± 316 [249] (6–1,069) |
0.16 | 254 ± 248 [211] (6–1,069) |
| Rate (mm3/year) | 43 ± 25 [43] (14–101) |
74 ± 49 [54] (6–152) |
0.14 | 58 ± 41 [49] (6–152) |
|
| Penetration | Volume (mm3) | 212 ± 127 [193] (60–487) |
524 ± 373 [382] (153–1,295) |
0.01 | 368 ± 315 [275] (60–1,295) |
| Rate (mm3/year) | 56 ± 28 [53] (19–107) |
135 ± 74 [127] (45–286) |
0.004 | 95 ± 68 [68] (19–286) |
|
| Deformation | Volume (mm3) | 45 ± 23 [41] (13–105) |
182 ± 115 [163] (49–468) |
< 0.001 | 114 ± 108 [60] (13–468) |
| Rate (mm3/year) | 13 ± 8 [11] (5–38) |
61 ± 60 [37] (12–211) |
< 0.0001 | 37 ± 49 [15] (5–211) |
|
| Topside wear | Volume (mm3) | 159 ± 110 [160] (33–314) |
260 ± 177 [216] (19–490) |
0.20 | 209 ± 153 [180] (19–490) |
| Rate (mm3/year) | 41 ± 28 [40] (12–101) |
63 ± 39 [60] (18–148) |
0.14 | 52 ± 35 [47] (12–148) |
|
| Backside wear | Volume (mm3) | 9 ± 32 [0] (−30–78) |
81 ± 188 [19] (−83–582) |
0.63 | 45 ± 137 [3] (−83–582) |
| Rate (mm3/year) | 2 ± 8 [0] (−6–26) |
10 ± 31 [5] (−30–80) |
0.80 | 6 ± 23 [1] (−30–80) |
|
Data include mean ± SD [median] (range).
Discussion
Wear has been studied using gravimetric techniques with knee simulators [13, 17–19]. Surface damage has been studied in worn polyethylene retrievals using visual assessment grading scales [4, 10–12, 16]. Condylar penetration has been measured radiographically [6, 20, 22]. However, these studies have rarely described the location and volume of wear nor have they identified the contributions of penetration and deformation to wear. We used micro-CT to compare new unworn and in vivo worn retrieved tibial polyethylene. Our purpose was to determine if micro-CT could measure the magnitude and location of wear from revision retrieved fixed-bearing and rotating-platform inserts. We also wanted to determine if there were differences in the location of wear for the two bearing types. We discovered that the location and magnitude of wear could be measured. However, small differences in the shapes of the control compared with the retrieval attributed to manufacturing tolerances made it difficult to apply the technique to cases with low wear.
Readers should be aware of limitations of our study. First is the wide range of measured wear values. We believe patient differences, revision diagnoses, baseplate surfaces, polyethylene type, and sterilization are contributors to the wide range in wear values. Lesser contributors to the variation are multiple surgeons and different surgical techniques for fixed-bearing and rotating-platform knees. We did our best to control for these variables (Table 1) but like other studies that evaluate revision retrievals, we could not control all variables [1, 2, 9, 14, 15]. Although this study only used one manufacturer, there were three designs evaluated. It is possible that tolerances vary with different designs and may also vary with the date of manufacture because more modern manufacturing techniques could improve tolerances. We believe the difference in tolerances is the reason one of the authors (RLZ) had to align the worn and unworn inserts and then slice by slice expand or contract the nonarticular peripheral volume of the unworn liner. It is important to note that the amount of manipulation was only 0.4% of the total control insert volume on average and that the articular surface was not changed. By comparing the raw total wear with the wear adjusted for manufacturing tolerances, it is easy to see the cases that would have had negative wear without an adjustment (Fig. 4). Unfortunately we did not perform either an intraobserver or intraobserver analysis of this aspect of the technique because of the technical, time-consuming, and tedious nature of adjusting many CT slices to account for tolerance differences. We were encouraged that despite the need to manually adjust for tolerances, the validation that compared physical thickness with micro-CT thickness was highly correlated and had limits of agreement on the order of 0.2 mm. Additionally, the values we obtained fell between volumes of wear reported for simulator studies (Table 3) and other retrieval studies (Table 4). A final limitation of the rotating-platform to fixed-bearing comparison was an inability to account for the wear that occurred on the central tibial rotation peg of rotating-platform retrievals because the peg is typically cut off to facilitate revision removal.
Table 3.
Simulator studies
| Study | Knee design | Polyethylene type | Wear |
|---|---|---|---|
| Muratoglu et al. [19] | FB CR | Gamma-inert | 9.6 ± 3.6 mm3/Mc |
| McEwen et al. [17] | FB CR | Gamma-inert | 23 ± 9.5 mm3/Mc |
| FB CR | Crosslinked | 13 ± 3.9 mm3/Mc | |
| MB | Gamma-inert | 5.2 ± 3.8 mm3/Mc | |
| Kester et al. [13] | FB PS | Gamma-inert | 35 ± 1.7 mm3/Mc |
| FB PS | Crosslinked | 8.2 ± 0.7 mm3/Mc | |
| Muratoglu et al. [18] | FB CR | Gamma-inert | 23 ± 6 mm3/Mc |
| FB CR | Crosslinked | 4.6 ± 2 mm3/Mc |
FB = fixed-bearing; CR = cruciate-retaining; MB = mobile-bearing; PS = posterior-stabilized; Mc = million cycles.
Table 4.
Retrieval studies
| Study | Knee design | Polyethylene type | Wear* |
|---|---|---|---|
| Kop and Swarts [14] | MB-APG | Not described | 85 mm3/year |
| MB-LCS | Not described | 77 mm3/year | |
| Benjamin et al. [2] | FB CR-flat | Gamma-air† | 959 mm3/year |
| FB CR-curved | Gamma-air† | 356 mm3/year | |
| Lavernia et al. [15] | FB CR-postmortem | Gamma-air† | 32 ± 43 mm3/year |
| Atwood et al. [1] | MB-LCS | Gamma-air | 54 mm3/year backside |
| Conditt et al. [9] | FB CR | Gamma-air | 138 mm3/year backside |
| Current study | MB | Gas plasma/gamma-inert | 43 ± 25 mm3/year |
| FB CR/PS | Gamma-inert | 74 ± 49 mm3/year |
* Volumes reported from other studies calculate wear based on multiple thickness measurements and do not account for creep or deformation; †polyethylene type assumed based on implant design; FB = fixed-bearing; CR = cruciate-retaining; MB = mobile-bearing; PS = posterior-stabilized.
The application of micro-CT to retrieved in vivo worn polyethylene liners provides additional data on retrievals, which have traditionally only been studied by characterization of surface wear modes [8, 10–12, 16]. Our average wear of 58 mm3/year falls between the wear reported for knee simulators (Table 3) and retrieval studies (Table 4). One might expect our wear rates to be similar to those reported in retrieval studies. There are two possible explanations for the lower wear seen in our retrievals. First is the absence of gamma-in-air polyethylene in our study compared with its presence in four of five retrieval studies [1, 2, 9, 15]. The second reason is the relationship among penetration, deformation, and wear. If we only reported the penetration value of 95 mm3/year as wear, our study would have found similar values to three of the retrieval studies [1, 14, 15]. Although the agreement seen between penetration values from our and other studies is reassuring, we do not believe penetration alone is a good measure of wear. One of the important aspects of the micro-CT technique is the finding that wear was just 69% of penetration, demonstrating the contribution of deformation or creep to the wear calculation. Comparing rotating-platform with fixed-bearing knees in this study, the mean wear rates were 43 mm3/year and 74 mm3/year, respectively. Although these values were not statistically different, there was a trend for a twofold reduction in wear comparing the rotating-platform with the fixed-bearing group. The magnitude of this reduction is the same twofold reduction seen in a simulator comparison of fixed-bearing with rotating-platform knees [17]. The same study determined that backside wear accounted for 30% of total wear in fixed-bearing knees, which is similar to the 24% of fixed-bearing wear attributed to the backside in our analysis.
In conclusion, we applied micro-CT to the measurement of wear in retrieved tibial polyethylene inserts. The unique and important aspect of the application is the ability to determine the magnitude of the penetration and deformation components of wear. The technique also allowed localization of wear to different regions of the liner, specifically top and backside. We had to overcome a difference in the shape of the control and retrieved inserts. We believe this difference represented manufacturing tolerances. Accounting for tolerances is particularly critical when the total amount of wear is relatively small because volumetric differences resulting from tolerances can exceed volume losses resulting from wear. We believe that the mean time in situ time of 52 months was short and thus the mean wear of 254 mm3 was not much larger than the mean difference in tolerance of 136 mm3. If we had retrievals that had been in situ for a longer duration with greater total wear, the influence of manufacturing tolerances would have been less of a factor. We noticed a trend for lower wear in the rotating-platform group compared with the fixed-bearing group whether or not we accounted for tolerances (Fig. 4). We believe that retrievals obtained with larger amounts of wear resulting from longer time in situ will determine if the trend we identified is real. Although manufacturing tolerances complicated the application of micro-CT to retrieval analysis, we speculate this technique could be valuable as a supplement to simulator studies. Simulator studies are well controlled and the same implant is measured gravimetrically over millions of cycles. An institution that had access to both micro-CT and knee simulators could easily scan the same implant before and at each interval the implant was weighed. The added data on location of penetration, deformation, and wear could help the development of new polyethylene components and knee designs. For instance, it may be possible to better evaluate the influence of polyethylene deformation and wear on the tibial locking mechanism. Developers would also be able to report the proportion of wear attributed to the backside surface.
Acknowledgments
We thank DePuy Orthopaedics, a Johnson & Johnson company (Warsaw, IN, USA), for providing the control inserts used for this study.
Footnotes
One author (CAE) certifies that he has or may receive payments or benefits, in any one year, an amount in excess of $100,000, from DePuy, a Johnson & Johnson company (Warsaw, IN, USA), related to this work. The institution (AORI) of the authors (CAE, RLZ, RHH, GAE) has received funding to support this research from DePuy, a Johnson & Johnson company, and Inova Health Services.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at Anderson Orthopaedic Research Institute, Alexandria, VA, USA, and Inova Center for Joint Replacement at Mount Vernon Hospital, Alexandria, VA, USA.
References
- 1.Atwood SA, Currier JH, Mayor MB, Collier JP, Van Citters DW, Kennedy FE. Clinical wear measurement on low contact stress rotating platform knee bearings. J Arthroplasty. 2008;23:431–440. doi: 10.1016/j.arth.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin J, Szivek J, Dersam G, Persselin S, Johnson R. Linear and volumetric wear of tibial inserts in posterior cruciate-retaining knee arthroplasties. Clin Orthop Relat Res. 2001;392:131–138. doi: 10.1097/00003086-200111000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 4.Blunn GW, Joshi AB, Minns RJ, Lidgren L, Lilley P, Ryd L, Engelbrecht E, Walker PS. Wear in retrieved condylar knee arthroplasties. A comparison of wear in different designs of 280 retrieved condylar knee prostheses. J Arthroplasty. 1997;12:281–290. doi: 10.1016/S0883-5403(97)90024-3. [DOI] [PubMed] [Google Scholar]
- 5.Bowden AE, Kurtz SM, Edidin AA. Validation of a micro-CT technique for measuring volumetric wear in retrieved acetabular liners. J Biomed Mater Res Part B Appl Biomater. 2005;75:205–209. doi: 10.1002/jbm.b.30318. [DOI] [PubMed] [Google Scholar]
- 6.Collier MB, Engh CA, Hatten KM, Ginn SD, Sheils TM, Engh GA. Radiographic assessment of the thickness lost from polyethylene tibial inserts that had been sterilized differently. J Bone Joint Surg Am. 2008;90:1543–1552. doi: 10.2106/JBJS.G.00651. [DOI] [PubMed] [Google Scholar]
- 7.Collier MB, Engh CA, Mcauley JP, Engh GA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am. 2007;89:1306–1314. doi: 10.2106/JBJS.F.00667. [DOI] [PubMed] [Google Scholar]
- 8.Collier MB, Jewett BA, Engh CA. Clinical assessment of tibial polyethylene thickness: comparison of radiographic measurements with as-implanted and as-retrieved thicknesses. J Arthroplasty. 2003;18:860–866. doi: 10.1016/S0883-5403(03)00272-9. [DOI] [PubMed] [Google Scholar]
- 9.Conditt MA, Thompson MT, Usrey MM, Ismaily SK, Noble PC. Backside wear of polyethylene tibial inserts: mechanism and magnitude of material loss. J Bone Joint Surg Am. 2005;87:326–331. doi: 10.2106/JBJS.C.01308. [DOI] [PubMed] [Google Scholar]
- 10.Engh GA, Engh GA, Zimmerman RL, Zimmerman RL, Parks NL, Parks NL, Engh CA, Engh CA. Analysis of wear in retrieved mobile and fixed bearing knee inserts. J Arthroplasty. 2009;24:28–32. doi: 10.1016/j.arth.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Garcia RM, Kraay MJ, Messerschmitt PJ, Goldberg VM, Rimnac CM. Analysis of retrieved ultra-high-molecular-weight polyethylene tibial components from rotating-platform total knee arthroplasty. J Arthroplasty. 2009;24:131–138. doi: 10.1016/j.arth.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Kelly NH, Fu RH, Wright TM, Padgett DE. Wear damage in mobile-bearing TKA is as severe as that in fixed-bearing TKA. Clin Orthop Relat Res. 2011;469:123–130. doi: 10.1007/s11999-010-1557-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kester MA, Herrera L, Wang A, Essner A. Knee bearing technology: where is technology taking us? J Arthroplasty. 2007;22(Suppl 3):16–20. doi: 10.1016/j.arth.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 14.Kop AM, Swarts E. Quantification of polyethylene degradation in mobile bearing knees: a retrieval analysis of the Anterior-Posterior-Glide (APG) and Rotating Platform (RP) Low Contact Stress (LCS) knee. Acta Orthop. 2007;78:364–370. doi: 10.1080/17453670710013942. [DOI] [PubMed] [Google Scholar]
- 15.Lavernia CJ, Sierra RJ, Hungerford DS, Krackow K. Activity level and wear in total knee arthroplasty: a study of autopsy retrieved specimens. J Arthroplasty. 2001;16:446–453. doi: 10.1054/arth.2001.23509. [DOI] [PubMed] [Google Scholar]
- 16.Lu Y-C, Huang C-H, Chang T-K, Ho F-Y, Cheng C-K, Huang C-H. Wear-pattern analysis in retrieved tibial inserts of mobile-bearing and fixed-bearing total knee prostheses. J Bone Joint Surg Br. 2010;92:500–507. doi: 10.2106/JBJS.I.00833. [DOI] [PubMed] [Google Scholar]
- 17.McEwen HMJ, Barnett PI, Bell CJ, Farrar R, Auger DD, Stone MH, Fisher J. The influence of design, materials and kinematics on the in vitro wear of total knee replacements. J Biomech. 2005;38:357–365. doi: 10.1016/j.jbiomech.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 18.Muratoglu OK, Bragdon CR, Jasty M, O’Connor DO, Von Knoch RS, Harris WH. Knee-simulator testing of conventional and cross-linked polyethylene tibial inserts. J Arthroplasty. 2004;19:887–897. doi: 10.1016/j.arth.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 19.Muratoglu OK, Rubash HE, Bragdon CR, Burroughs BR, Huang A, Harris WH. Simulated normal gait wear testing of a highly cross-linked polyethylene tibial insert. J Arthroplasty. 2007;22:435–444. doi: 10.1016/j.arth.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 20.Sanzén L, Sahlström A, Gentz CF, Johnell IR. Radiographic wear assessment in a total knee prosthesis. 5- to 9-year follow-up study of 158 knees. J Arthroplasty. 1996;11:738–742. doi: 10.1016/S0883-5403(96)80014-3. [DOI] [PubMed] [Google Scholar]
- 21.Teeter MG, Naudie DDR, McErlain DD, Brandt J-M, Yuan X, Macdonald SJ, Holdsworth DW. In vitro quantification of wear in tibial inserts using microcomputed tomography. Clin Orthop Relat Res. 2011;469:107–112. doi: 10.1007/s11999-010-1490-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thadani PJ, Vince KG, Ortaaslan SG, Blackburn DC, Cudiamat CV. Ten- to 12-year followup of the Insall-Burstein I total knee prosthesis. Clin Orthop Relat Res. 2000;380:17–29. doi: 10.1097/00003086-200011000-00004. [DOI] [PubMed] [Google Scholar]