Abstract
Background
Patient satisfaction has increasingly been recognized as an important measure after total knee arthroplasty (TKA). However, we do not know yet how and why the patients are satisfied or dissatisfied with TKA.
Questions/purposes
We asked: (1) After TKA, how satisfied are patients and which activities were they able to do? (2) Are patient-derived scores related to physician-derived scores? (3) Which factors affect patient satisfaction and function?
Methods
We retrospectively evaluated 375 patients who had undergone 500 TKAs between February 22, 2000 and December 1, 2009. We sent a questionnaire for The 2011 Knee Society Knee Scoring System to the patients. We determined the correlation of patient- and physician-derived scores and factors relating to the five questions relating to satisfaction and the 19 questions relating function. The minimum followup was 2 years (mean, 5 years; range, 2–11 years).
Results
The mean score for symptoms was 19 (74%), 23 (59%) for patient satisfaction, 10 (64%) for patient expectations, and 53 (53%) for functional activities. We found a poor correlation between the patient-derived and the physician-derived scores. Old age and varus postoperative alignment negatively correlated with the satisfaction. Varus alignment and limited range of motion (ROM) negatively correlated with the expectation. Old age, rheumatoid arthritis, and limited ROM negatively correlated with the functional activities.
Conclusions
Most patients did not report symptoms, but they experienced difficulty with activities of daily living after TKA. Patient satisfaction is difficult to measure, but avoiding varus alignment and achieving better ROM appear to be important for increasing satisfaction and meeting expectations.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA is one of the most effective surgical procedures for relieving pain and restoring function in patients with advanced osteoarthritis and rheumatoid arthritis of the knee. Pain relief is achieved in most patients after TKA, and advances in surgical technique and prosthesis design have improved its longevity. Recently, patient satisfaction has been recognized as an important measure of healthcare quality [1, 2, 5, 20]. Several studies have reported that patient satisfaction and function after TKA are lower than after a similar procedure, THA [4, 24, 34]. Increasingly, surgeons are paying more attention to how satisfied patients are after TKA.
Patient satisfaction and postoperative knee function have been difficult to evaluate. Quantifying satisfaction in a valid way is the challenge. Satisfaction is not straightforward to assess and unvalidated instruments can provide misleading data. Currently we do not have a gold standard method to measure patient satisfaction after TKA. Patient-derived outcome scales have become increasingly important [23, 25] because physician-based scores are poorly related to patient-derived measures [6, 19]. Patient satisfaction and knee function have been evaluated in the postoperative setting using disease-specific (WOMAC [3], Oxford-12 [11]) and patient-specific methods (MACTAS [32]), global health surveys (SF-36 [33]), and functional capacity instruments (KOOS [5]). Until recently there were no instruments to specifically measure patient satisfaction and knee function after TKA. In 2012 The Knee Society developed a new scoring system to better characterize the expectations, satisfaction, and physical activities of patients who underwent TKA [27, 30].
Many factors could affect satisfaction and function after TKA. A number of preoperative and postoperative factors, including infection, postoperative alignment, and soft tissue balancing, have been related to prosthesis failure [7, 13]. However, relatively few studies have evaluated the effect of postoperative knee alignment on patient satisfaction, and several have shown age and ROM correlate with satisfaction and function [5, 10, 26, 28].
Therefore, we asked the following questions: (1) After TKA, how satisfied are patients and which activities were they able to do? (2) Are patient-derived scores related to physician-derived scores? (3) Which factors affect patient satisfaction and function?
Patients and Methods
We reviewed data on 375 patients who underwent 500 primary TKAs between February 22, 2000 and December 1, 2009. We excluded 34 patients with revision arthroplasties, patients bedridden as a result of reasons other than knee surgery, and those who underwent another surgical procedure during the study period. We mailed a questionnaire to 543 patients, 375 (69%) of whom returned the completed questionnaire (Table 1). The questionnaire was sent to each patient 1 month before her or his office visit. Four hundred ten knees (82%) had a cruciate-substituting design; 90 knees (18%) had a cruciate-retaining design. The cruciate-retaining design was mainly indicated for the patients with small deformities (approximately less than 10°). All patients had patellar resurfacing. The minimum followup was 2 years (mean, 5 years; range, 2–12 years). No patients were recalled specifically for this study; all data were obtained from medical records and the questionnaires. Our institutional review board approved this survey.
Table 1.
Demographic and preoperative clinical data
| Characteristics | Number |
|---|---|
| Mean age ± SD (years) | 71 ± 10 |
| Female sex (%) | 83 |
| Mean body mass index ± SD (kg/m2) | 26 ± 4 |
| Primary diagnosis | Osteoarthritis (312), rheumatoid arthritis (56), other (7) |
| Mean preoperative extension angle ± SD (degrees) | −9 ± 9 |
| Mean preoperative flexion angle ± SD (degrees) | 118 ± 19 |
| Mean preoperative Knee Society total knee score ± SD | 45 ± 16 |
| Mean pain score ± SD | 18 ± 9 |
| Mean stability score ± SD | 22 ± 7 |
| Mean preoperative Knee Society function score ± SD | 31 ± 24 |
| Mean hip-knee-ankle angle ± SD (degrees) | 186 ± 4 |
We sent all patients questionnaires containing all patient-derived components of two scores: The 1989 Knee Society Clinical Rating System [18] and The 2011 Knee Society Scoring System [30]. The knee score and functional score of the Knee Society Clinical Rating System (Table 2), which was introduced in 1989 [18], were assessed by the surgeon using a scoring sheet. Hip-knee-ankle (HKA) angle was measured on the full leg-length standing radiograph, and ROM of the knee was measured with a goniometer. The new 2011 Knee Society Score questionnaire [30] has four categories: symptoms, patient satisfaction, patient expectations, and functional activities (Table 3). Patients are asked to grade their symptoms, expectations, and satisfaction for each question. These assessments and measurements were obtained at the last office visit.
Table 2.
Pain score and function score of The Knee Society Clinical Rating System© (1989)
| Pain score | 50 = none/mild or occasional/stairs only/walking and stairs Moderate (occasional)/moderate (continual)/severe |
| Functional score (100) | |
| Walking | 50 = unlimited/> 10 blocks/5-10 blocks/< 5 blocks/house-bound/unable |
| Stairs | 50 = normal up and down/normal up, down with rail/up and down with rail/up with rail; unable down/unable |
Reprinted with permission from The Knee Society, Copyright 2011 by The Knee Society.
Table 3.
The questionnaire for the patients in 2011 The Knee Society Scoring System© (2012)
| Symptoms (25) |
| 1. Pain with level walking (10 = none to severe [10 grades]) |
| 2. Pain with stairs or inclines (10) |
| 3. Does this knee feel “normal” to you? (5 = always/sometimes/never) |
| Patient satisfaction (40) |
| 1. Currently, how satisfied are you with the pain level of your knee while sitting? (8 = very satisfied/satisfied/neutral/dissatisfied/very dissatisfied) |
| 2. Currently, how satisfied are you with the pain level of your knee while lying in bed? (8) |
| 3. Currently, how satisfied are you with your knee function while getting out of bed? (8) |
| 4. Currently, how satisfied are you with your knee function while performing light household duties? (8) |
| 5. Currently, how satisfied are you with your knee function while performing leisure recreational activities? (8) |
| Patient expectation (15) |
| 1. My expectations for pain relief were… (5 = too high/just right/too low) |
| 2. My expectations for being able to do my normal activities of daily living were… (5) |
| 3. My expectations for being able to do my leisure, recreational or sports activities were… (5) |
| Functional activities (100) |
| Walking and standing (30) |
| 1. Can you walk without any aids (such as a cane, crutches, or wheelchair)? (0 = yes/no) |
| 2. If no, which of the following aid(s) do you use? (−10) |
| 3. Do you use these aid(s) because of your knees? (0 = yes/no) |
| 4. For how long can you stand (with or without aid) before sitting as a result of knee discomfort? (15 = cannot stand/0–5 minutes/6–15 minutes/16–30 minutes/31–60 minutes/more than 1 hour) |
| 5. For how long can you walk (with or without aid) before stopping as a result of knee discomfort? (15) |
| Standard activities (30) |
| How much does your knee bother you during each of the following activities? |
| 1. Walking on an uneven surface (5 = no bother/slight/moderate/sever/very severe/cannot do) |
| 2. Turning or pivoting on your leg (5) |
| 3. Climbing up or down a flight of stairs (5) |
| 4. Getting up from a low couch or a chair without arms (5) |
| 5. Getting into or out of a car (5) |
| 6. Moving laterally (stepping to the side) (5) |
| Advanced activities (25) |
| How much does your knee bother you during each of the following activities? |
| 1. Climbing a ladder or step stool (5) |
| 2. Carrying a shopping bag for a block (5) |
| 3. Squatting (5) |
| 4. Kneeling (5) |
| 5. Running (5) |
| Discretionary activities (15) |
| Please check 3 of the activities below that you consider most important to you. (9 recreational activities [swimming, etc] and 8 workout and gym activities [weightlifting, etc]) |
| How much does your knee bother you during each of these activities? |
| 1. Activity A (5) |
| 2. Activity B (5) |
| 3. Activity C (5) |
Reprinted with permission from The Knee Society, Copyright 2011 by The Knee Society.
We used linear regression analysis to determine the relationship between the patient-derived symptom score of The 2011 Knee Society score (Table 2) and the physician-derived Knee Society pain score (Table 3) and between the patient-derived functional activities score of The 2011 Knee Society score (Table 2) and the physician-based Knee Society functional score (Table 3). We performed multivariate linear regression analyses to determine which factors affected symptoms, satisfaction, expectations, and function. In the multivariate linear regression, dependent variables included sex, age, BMI, primary diagnosis, postoperative HKA angle, and postoperative ROM. All statistical analyses were performed with JMP 9.0 (SAS Institute Inc, Cary, NC, USA).
Results
After TKA, the mean overall score for The 2011 Knee Society score [30] was 105 points, the mean satisfaction score was 23 of 40, and the mean expectation score was 10 of 15. These scores were lower than the symptom score of 19 of 25 (Table 4). In functional activities, patients feel difficulty for advanced activities such as running, kneeling, and squatting (Table 5). The physician-derived Knee Society pain score [18] was 47 of 50, and the physician-derived Knee Society functional score [18] was 82 of 100.
Table 4.
Postoperative scores (mean ± SD)
Table 5.
Scores in functional activities (mean ± SD)
| Walking and standing (30) | 17 ± 10 (57%) |
| Standard activities (30) | 2 ± 7 (67%) |
| Walking on an uneven surface (5) | 3 ± 1 (66%) |
| Turning or pivoting on your leg (5) | 4 ± 1 (80%) |
| Climbing up or down a flight of stairs (5) | 3 ± 2 (62%) |
| Getting up from a low couch or a chair without arms (5) | 3 ± 1 (64%) |
| Getting into or out of a car (5) | 3 ± 1 (68%) |
| Moving laterally (stepping to the side) (5) | 4 ± 1 (76%) |
| Advanced activities (25) | 9 ± 17 (37%) |
| Climbing a ladder or step stool (5) | 3 ± 2 (54%) |
| Carrying a shopping bag for a block (5) | 4 ± 2 (70%) |
| Squatting (5) | 2 ± 2 (36%) |
| Kneeling (5) | 2 ± 2 (30%) |
| Running (5) | 2 ± 2 (30%) |
| Discretionary activities (15) | 7 ± 5 (45%) |
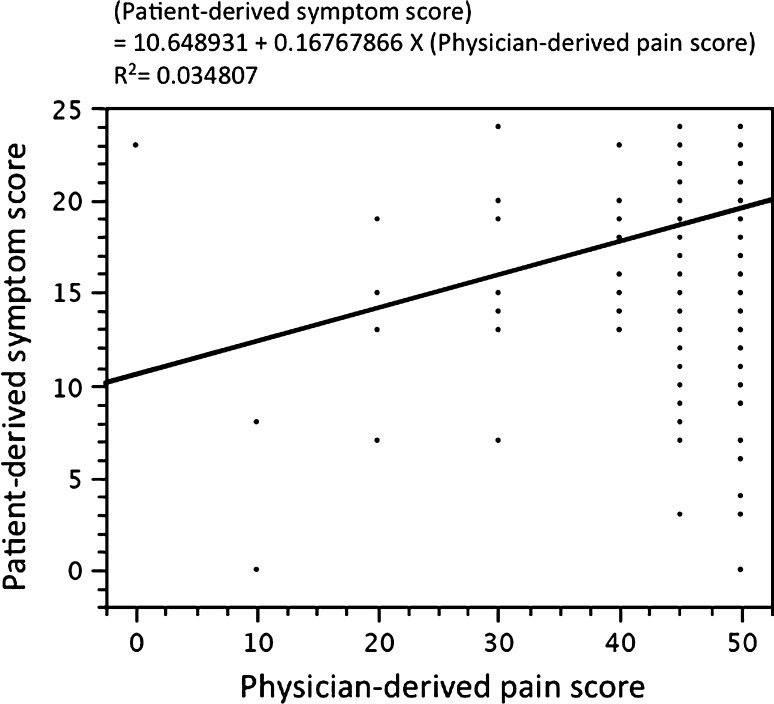
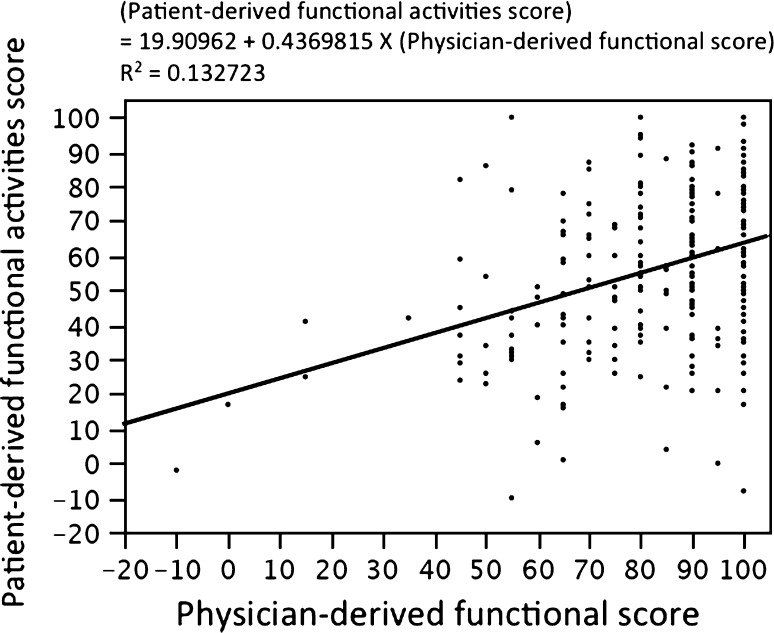
We found a poor correlation between the patient-derived symptom scores [30] and the physician-derived pain scores [18] (Fig. 1). There was a weak correlation between the patient-derived total functional score [30] and the physician-derived functional score [18] (Fig. 2).
Fig. 1.
The graph shows the relationship between the patient-derived symptom score of the 2011 Knee Society score and the physician-derived Knee Society pain score. Linear regression analysis showed a poor correlation between the patient-derived symptom scores and the physician-derived pain scores.
Fig. 2.
The graph shows the relationship between the patient-derived functional activities score of the 2011 Knee Society score and the physician-based Knee Society functional score. Linear regression analysis showed a weak correlation between the patient-derived total functional score and the physician-derived functional score.
Regarding patient satisfaction, old age and varus postoperative HKA angle negatively correlated with the patient satisfaction score (Table 6) [4]. Varus alignment and limited ROM negatively correlated with the patient expectations score (Table 7). Old age, rheumatoid arthritis, and limited ROM negatively correlated with the functional activities score (Table 8). We identified no variables that related to the symptoms score (Table 9).
Table 6.
Multivariate analysis in patient satisfaction
| Factor | F-statistic | p value | Negative effect |
|---|---|---|---|
| Sex | 1.3797 | 0.2536 | |
| Age | 5.2091 | 0.0233 | Old age |
| BMI | 0.0670 | 0.7959 | |
| Primary diagnosis | 1.2395 | 0.2947 | |
| HKA | 4.1949 | 0.0416 | Varus |
| Postoperative ROM | 1.7432 | 0.1880 |
BMI = body mass index; HKA = hip-knee-ankle angle; ROM = range of motion of the knee.
Table 7.
Multivariate analysis in patient expectations
| Factor | F-statistic | p value | Negative effect |
|---|---|---|---|
| Sex | 2.7657 | 0.0649 | |
| Age | 0.0068 | 0.9341 | |
| BMI | 1.8102 | 0.1797 | |
| Primary diagnosis | 0.1321 | 0.9705 | |
| HKA | 7.6608 | 0.0061 | Varus |
| Postoperative ROM | 5.8741 | 0.0161 | Limited ROM |
BMI = body mass index; HKA = hip-knee-ankle angle; ROM = range of motion.
Table 8.
Multivariate analysis in functional activities
| Factor | F-statistic | p value | Negative effect |
|---|---|---|---|
| Sex | 1.3589 | 0.2589 | |
| Age | 28.6848 | < 0.0001 | Old age |
| BMI | 0.4681 | 0.4945 | |
| Primary diagnosis | 2.4622 | 0.0459 | Rheumatoid arthritis |
| HKA | 0.2291 | 0.6326 | |
| Postoperative ROM | 15.7567 | < 0.0001 | Limited ROM |
BMI = body mass index; HKA = hip-knee-ankle angle; ROM = range of motion.
Table 9.
Multivariate analysis in symptoms
| Factor | F-statistic | p value | Negative effect |
|---|---|---|---|
| Sex | 0.4445 | 0.6417 | |
| Age | 0.0169 | 0.8966 | |
| BMI | 0.0313 | 0.8597 | |
| Primary diagnosis | 1.0389 | 0.3877 | |
| HKA | 3.3771 | 0.0673 | |
| Postoperative ROM | 0.2036 | 0.6522 |
BMI = body mass index; HKA = hip-knee-ankle angle; ROM = range of motion.
Discussion
TKA is one of the most successful orthopaedic procedures considering its longevity and ability to relieve pain. Higher rates of success for this procedure have led younger and more active patients to undergo knee arthroscopy. Consequently, patients increasingly expect to be more active and pain-free after surgery. Therefore, it is important we evaluate patient satisfaction after TKA in more detail. The conventional Knee Society scoring system asked for patient input in only three aspects: pain, walking, and stairclimbing ability (Table 2). With this system, it has been difficult to comprehensively understand the postoperative condition [16] and the high inter- and intraobserver variations of the system were also reported [21]. The 2011 Knee Society scoring system was developed to better characterize the expectations, satisfaction, and physical activities of patients who underwent TKA. The new system is more patient-derived and much longer (30 questions) and more time-consuming to administer than the conventional system (Table 2). This scoring system was validated using standard statistical and psychometric procedures [27]. We used the questionnaire of The 2011 Knee Society Scoring System [30] to address the following questions: (1) After TKA, how satisfied were patients and which activities were they able to do? (2) Were patient-derived scores related to physician-derived scores? (3) Did postoperative knee alignment and ROM affect patient satisfaction and function?
We acknowledge limitations to our study. First, patient satisfaction is difficult to evaluate. The 2011 Knee Society score has not been validated for satisfaction in part because there is no gold standard for measuring patient satisfaction after TKA against which a new score could be validated. We asked the five questions in the scoring system, but they would not capture everything about patient satisfaction. Furthermore, results would vary depending on who and how the questionnaire is administered and how the questions are posed. Second, we did not evaluate patient expectations and functional activities before surgery. Patient satisfaction has been closely related to their expectations [9, 14, 29, 31], but we only retrospectively asked whether their expectations were met. Functional activities should be evaluated in changes by the surgery. Third, the questionnaire was mailed to the patients 1 month before their office visit and the physician-derived evaluation was obtained at their office visit. Therefore, the time difference at which the two scores were obtained is within 1 month but not completely the same. This time difference would possibly be one of the reasons for discrepancy in patient-based and physician-based scores. Fourth, mental health is an important aspect in patient satisfaction [22, 29], but we were unable to evaluate this factor. Lastly, we asked the patients about their functional activities by questionnaire, but we did not clarify if these scores are related to their actual ability to perform the activities.
We found most patients did not report symptoms, but satisfaction and expectation scores were relatively low. In previous studies, approximately 80% of the patients expressed overall satisfaction with their primary TKA [5], but it was difficult to compare our results with those from earlier studies because few scored the degree of satisfaction. Measuring functional status after knee surgery has also been an important part of the postoperative evaluation. This study showed the average functional activities score [30] was 53% in patients with an average age of 71 years. Dahm et al. [10] reported that the UCLA function score was 7.1 out of 10 in patients with an average age of 67 years at TKA. In addition to the fact that these two scoring systems are not identical, this difference might have been partly explained by the difference in age. Functional status varied with age; therefore, comparison against preoperative status would be more relevant than the absolute value of the postoperative functional status score.
Physicians tend to overestimate outcomes compared with patients [8, 19, 35]. Poor correlation between patient-derived and physician-derived scores has been reported after TKA [6, 17, 18]. We also showed that surgeons overestimated symptoms and function and there was a weak relationship between the patient-derived [30] and physician-derived scores [18] on postoperative pain and function. One of the reasons for discrepancy is that the physician overestimated the symptom and functional activities after TKA, as reported before [19]. The other possible causes are differences in the two scoring systems. Therefore, we cannot determine that the value of each system is identical. The findings of this study confirmed that patient-derived outcome scales are important for measuring improvements in function and satisfaction after surgery.
Determining which factors affect patient satisfaction and knee function has been a very important clinical issue. We found older patients and those with knees in varus alignment were less satisfied with the surgery. Previous studies also showed that younger patients were more satisfied with TKA [5, 26]. One of the possible reasons has been that younger patients tend to have less difficulty during postoperative rehabilitation, whereas older patients tend to have more complications. In the current study, expectations were less frequently met in patients with a more restricted ROM and with varus alignment. Devers et al. [12] also reported that increased ROM had a positive association with achievement of expectations but not with satisfaction. To our knowledge, few studies evaluated the effect of postoperative knee alignment on patient satisfaction. Although one study suggests patients are not able to judge alignment correctly [15], we found postoperative varus alignment results in lower patient satisfaction and fewer expectations met by TKA. These findings are difficult to be correctly explained, but these suggest that patients would not prefer varus knees. We also showed postoperative functional activities correlated with patient age, primary diagnosis, and postoperative ROM. Previous studies also found that age and ROM correlated with functional status [12, 28]. However, postoperative knee alignment was not related to functional activities. Although malalignment reportedly increases the risk of implant failure [7, 13], our data suggest that although patients dislike malalignment, it does not affect knee function in midterm followup.
The current postoperative survey revealed most patients did not report symptoms but experienced difficulty with functional activities after TKA. We also confirmed patient-derived assessment is lower than surgeon-derived measurement. To increase satisfaction and meet patient expectations, surgeons should achieve proper postoperative knee alignment and to increase ROM.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Baumann C, Rat AC, Mainard D, Cuny C, Guillemin F. Importance of patient satisfaction with care in predicting osteoarthritis-specific health-related quality of life one year after total joint arthroplasty. Qual Life Res. 2011;20:1581–1588. doi: 10.1007/s11136-011-9913-8. [DOI] [PubMed] [Google Scholar]
- 2.Becker R, Doring C, Denecke A, Brosz M. Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1433–1441. doi: 10.1007/s00167-011-1621-y. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 4.Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res. 2010;468:542–546. doi: 10.1007/s11999-009-1046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16:740–747. [DOI] [PubMed]
- 7.Callaghan JJ, O’Rourke MR, Saleh KJ. Why knees fail: lessons learned. J Arthroplasty. 2004;19:31–34. doi: 10.1016/j.arth.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 8.Cohen SB, Strand V, Aguilar D, Ofman JJ. Patient- versus physician-reported outcomes in rheumatoid arthritis patients treated with recombinant interleukin-1 receptor antagonist (anakinra) therapy. Rheumatology (Oxford). 2004;43:704–711. doi: 10.1093/rheumatology/keh152. [DOI] [PubMed] [Google Scholar]
- 9.Culliton SE, Bryant DM, Overend TJ, Macdonald SJ, Chesworth BM. The relationship between expectations and satisfaction in patients undergoing primary total knee arthroplasty. J Arthroplasty. 2012;27:490–492. doi: 10.1016/j.arth.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Dahm DL, Barnes SA, Harrington JR, Sayeed SA, Berry DJ. Patient-reported activity level after total knee arthroplasty. J Arthroplasty. 2008;23:401–407. doi: 10.1016/j.arth.2007.05.051. [DOI] [PubMed] [Google Scholar]
- 11.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63–69. doi: 10.1302/0301-620X.80B1.7859. [DOI] [PubMed] [Google Scholar]
- 12.Devers BN, Conditt MA, Jamieson ML, Driscoll MD, Noble PC, Parsley BS. Does greater knee flexion increase patient function and satisfaction after total knee arthroplasty? J Arthroplasty. 2011;26:178–186. doi: 10.1016/j.arth.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Fitzgerald SJ, Trousdale RT. Why knees fail in 2011: patient, surgeon, or device? Orthopedics. 2011;34:e513–e515. doi: 10.3928/01477447-20110714-45. [DOI] [PubMed] [Google Scholar]
- 14.Gandhi R, Davey JR, Mahomed N. Patient expectations predict greater pain relief with joint arthroplasty. J Arthroplasty. 2009;24:716–721. doi: 10.1016/j.arth.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 15.Gandhi R, de Beer J, Petruccelli D, Winemaker M. Does patient perception of alignment affect total knee arthroplasty outcome? Can J Surg. 2007;50:181–186. [PMC free article] [PubMed] [Google Scholar]
- 16.Ghanem E, Pawasarat I, Lindsay A, May L, Azzam K, Joshi A, Parvizi J. Limitations of the Knee Society Score in evaluating outcomes following revision total knee arthroplasty. J Bone Joint Surg Am. 2010;92:2445–2451. doi: 10.2106/JBJS.I.00252. [DOI] [PubMed] [Google Scholar]
- 17.Gioe TJ, Pomeroy D, Suthers K, Singh JA. Can patients help with long-term total knee arthroplasty surveillance? Comparison of the American Knee Society Score self-report and surgeon assessment. Rheumatology (Oxford). 2009;48:160–164. doi: 10.1093/rheumatology/ken439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 19.Khanna G, Singh JA, Pomeroy DL, Gioe TJ. Comparison of patient-reported and clinician-assessed outcomes following total knee arthroplasty. J Bone Joint Surg Am. 2011;93:e117.1–e117.7. doi: 10.2106/JBJS.J.00850. [DOI] [PubMed] [Google Scholar]
- 20.Kwon SK, Kang YG, Kim SJ, Chang CB, Seong SC, Kim TK. Correlations between commonly used clinical outcome scales and patient satisfaction after total knee arthroplasty. J Arthroplasty. 2010;25:1125–1130. doi: 10.1016/j.arth.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 21.Liow RY, Walker K, Wajid MA, Bedi G, Lennox CM. The reliability of the American Knee Society Score. Acta Orthop Scand. 2000;71:603–608. doi: 10.1080/000164700317362244. [DOI] [PubMed] [Google Scholar]
- 22.Lopez-Olivo MA, Landon GC, Siff SJ, Edelstein D, Pak C, Kallen MA, Stanley M, Zhang H, Robinson KC, Suarez-Almazor ME. Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis. 2011;70:1775–1781. doi: 10.1136/ard.2010.146423. [DOI] [PubMed] [Google Scholar]
- 23.Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011;2011:591253. doi: 10.1155/2011/591253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marx RG, Jones EC, Atwan NC, Closkey RF, Salvati EA, Sculco TP. Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J Bone Joint Surg Am. 2005;87:1999–2005. doi: 10.2106/JBJS.D.02286. [DOI] [PubMed] [Google Scholar]
- 25.Mizner RL, Petterson SC, Clements KE, Zeni JA, Jr, Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2011;26:728–737. doi: 10.1016/j.arth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 27.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, Chadha P, Daylamani DA, Scott WN, Bourne RB. Development of a new Knee Society scoring system. Clin Orthop Relat Res. 2012;470:20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Padua R, Ceccarelli E, Bondi R, Campi A, Padua L. Range of motion correlates with patient perception of TKA outcome. Clin Orthop Relat Res. 2007;460:174–177. doi: 10.1097/BLO.0b013e318046ccb7. [DOI] [PubMed] [Google Scholar]
- 29.Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92:1253–1258. doi: 10.1302/0301-620X.92B9.24394. [DOI] [PubMed] [Google Scholar]
- 30.Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new Knee Society knee scoring system. Clin Orthop Relat Res. 2012;470:3–19. doi: 10.1007/s11999-011-2135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan M, Tanzer M, Reardon G, Amirault D, Dunbar M, Stanish W. The role of presurgical expectancies in predicting pain and function one year following total knee arthroplasty. Pain. 2011;152:2287–2293. doi: 10.1016/j.pain.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 32.Tugwell P, Bombardier C, Buchanan WW, Goldsmith CH, Grace E, Hanna B. The MACTAR Patient Preference Disability Questionnaire—an individualized functional priority approach for assessing improvement in physical disability in clinical trials in rheumatoid arthritis. J Rheumatol. 1987;14:446–451. [PubMed] [Google Scholar]
- 33.Ware JE., Jr Sherbourne CD. The MOS 36-item Short-Form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Wylde V, Blom AW, Whitehouse SL, Taylor AH, Pattison GT, Bannister GC. Patient-reported outcomes after total hip and knee arthroplasty: comparison of midterm results. J Arthroplasty. 2009;24:210–216. doi: 10.1016/j.arth.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Zisapel N, Nir T. Determination of the minimal clinically significant difference on a patient visual analog sleep quality scale. J Sleep Res. 2003;12:291–298. doi: 10.1046/j.0962-1105.2003.00365.x. [DOI] [PubMed] [Google Scholar]