Abstract
Maternal infection is a risk factor for autism spectrum disorder (ASD) and schizophrenia (SZ). Indeed, modeling this risk factor in mice through maternal immune activation (MIA) causes ASD- and SZ-like neuropathologies and behaviors in the offspring. Although MIA upregulates pro-inflammatory cytokines in the fetal brain, whether MIA leads to long-lasting changes in brain cytokines during postnatal development remains unknown. Here, we tested this possibility by measuring protein levels of 23 cytokines in the blood and three brain regions from offspring of poly(I:C)- and saline-injected mice at five postnatal ages using multiplex arrays. Most cytokines examined are present in sera and brains throughout development. MIA induces changes in the levels of many cytokines in the brains and sera of offspring in a region- and age-specific manner. These MIA-induced changes follow a few, unexpected and distinct patterns. In frontal and cingulate cortices, several, mostly pro-inflammatory, cytokines are elevated at birth, followed by decreases during periods of synaptogenesis and plasticity, and increases again in the adult. Cytokines are also altered in postnatal hippocampus, but in a pattern distinct from the other regions. The MIA-induced changes in brain cytokines do not correlate with changes in serum cytokines from the same animals. Finally, these MIA-induced cytokine changes are not accompanied by breaches in the blood-brain barrier, immune cell infiltration or increases in microglial density. Together, these data indicate that MIA leads to long-lasting, region-specific changes in brain cytokines in offspring—similar to those reported for ASD and SZ—that may alter CNS development and behavior.
Keywords: Neuroimmunology, maternal infection, autism, schizophrenia, chemokine, serum, microglia, poly(I:C), inflammation, development
1. Introduction
Autism spectrum disorder (ASD) and schizophrenia (SZ) are devastating disorders that each affect cognitive and social functions of approximately 1% of the population (Kogan et al., 2009). Although the etiology of these disorders is unclear, genetics and environmental factors appear to interact to increase risk (Nawa et al., 2000; Patterson, 2009). Indeed, many of the environmental insults linked to SZ and ASD involve the maternal-fetal environment. Large SZ and ASD twin studies highlight the fact that concordance for dizygotic twins is much greater than that for siblings (Brown and Patterson, 2011; Hallmayer et al., 2011; Patterson, 2007; Rosenberg et al., 2009; Szatmari, 2011) and concordance for SZ is also higher for monochorionic twins, who share a placenta, than for dichorionic twins, who do not (Davis et al., 1995). Together, these studies indicate a significant role for the fetal environment in these disorders. In addition, maternal infection greatly increases the risk for SZ and ASD in offspring (Brown and Derkits, 2010; Brown and Patterson, 2011; Patterson, 2011a), and maternal viral infection is associated with increased risk of ASD as well as a 3–7-fold increased risk of SZ in the offspring (Atladottir et al., 2010; Brown et al., 2004; Brown and Patterson, 2011). Since different types of viral, bacterial, and parasitic infections are associated with ASD and SZ, the critical link between prenatal maternal infection and postnatal brain and behavioral pathology appears to be the maternal immune response and factors that mediate that response, such as cytokines (Deverman and Patterson, 2009; Garay and McAllister, 2010).
These correlations from epidemiological studies are supported by work in rodent models of maternal infection. Adult offspring of pregnant mice given intranasal influenza virus exhibit behavioral abnormalities and changes in gene expression, neuroanatomy, and neurochemistry consistent with both SZ and ASD (Fatemi et al., 2002; Fatemi et al., 1998). Because these outcomes are also elicited in the absence of infection by maternal injection of synthetic dsRNA (poly(I:C)), which mimics the acute phase response to viral infection (Traynor et al., 2004), it is maternal immune activation (MIA) that drives the changes in fetal brain development (Shi et al., 2005). Offspring born to pregnant mice injected with poly(I:C) at embryonic day 12.5 (E12.5) display the three core behavioral symptoms of ASD: stereotyped and repetitive behaviors, deficits in social interaction, and deficits in communication (Malkova et al., 2012; Smith et al., 2007). These offspring also display behaviors that are consistent with both SZ and ASD, including elevated anxiety and deficits in prepulse inhibition (PPI), latent inhibition (LI), and working memory (Patterson, 2011b), some of which can be alleviated by treatment with anti-psychotic drugs (Meyer and Feldon, 2010; Meyer et al., 2010; Piontkewitz et al., 2009; Shi et al., 2003). Adult MIA offspring also exhibit abnormalities in gene expression and neurochemistry similar to those noted in SZ and ASD (Meyer et al., 2011). Finally, neuropathology is also seen in this model, including enlarged ventricles and a spatially-localized deficit in Purkinje cells, characteristic of SZ and ASD, respectively (Meyer et al., 2009; Piontkewitz et al., 2009; Shi et al., 2009). Related findings have also been reported in non-human primate models of maternal infection and poly(I:C) MIA (Bauman, 2011; Short et al., 2010).
Despite recent progress in developing and characterizing rodent MIA models, much remains to be studied about how MIA alters fetal brain development. Current evidence indicates that the maternal cytokine response is crucial (Patterson, 2009), which leads to immune activation and endocrine changes in the placenta (Hsiao and Patterson, 2011; Mandal et al., 2011). Interleukin (IL)-6 is necessary and sufficient to mediate these effects since the effects of MIA on neuropathology and behavior in the offspring are prevented by injection of pregnant dams with poly(I:C) combined with an anti-IL-6 antibody and are mimicked by a single maternal injection of IL-6 (Smith et al., 2007). Induction of maternal cytokines then alters cytokine expression in the fetal brain, including IL-1β, IL-6, IL-17, IL-13, MCP-1, and MIP1α, hours after MIA (Fatemi et al., 2008; Meyer et al., 2006b; Meyer et al., 2008), with only IL-1β remaining elevated in the fetal brain 24 hours following poly(I:C) injection (Arrode-Bruses and Bruses, 2012). However, it is unknown if MIA causes chronic changes in brain cytokines and/or immune cell infiltration in offspring during postnatal development and/or in adult offspring.
Here, we test this possibility using proteomic analysis of cytokine levels in the postnatal brain. The levels of 23 cytokines were measured in the blood and three brain regions from offspring of poly(I:C)- and saline-injected mice at five ages (postnatal day 0 (P0), P7, P14, P30, and P60) using multiplex technology. Perhaps surprisingly, in control brains, most of the 23 cytokines examined are detectable in serum and in all three brain regions (frontal cortex (FC), cingulate cortex (CC), and hippocampus (HC)) from birth through adulthood. The levels of individual cytokines are modulated in age- and region-specific patterns that have not been previously described. Most important, MIA induces striking, long-lasting changes in cytokine levels in the brains of offspring, many of which are region- and age-specific and include widespread decreases as well as increases, compared to controls. Our results indicate that MIA leads to chronic changes in brain cytokine levels in offspring that may mediate MIA-induced changes in CNS development and behavior.
2. Methods and Materials
2.1 MIA for cytokine measurements
Female C57BL/6J mice (Charles River; Wilmington, MA) were obtained from the Caltech breeding facility and housed on a 12:12 h light:dark cycle at 29 ± 1 °C with food and water available ad libitum. Mice were mated overnight, and the presence of a vaginal plug on the following morning was noted as E0.5. Pregnant mice were injected intraperitoneally (i.p.) on E12.5 with saline or poly(I:C) potassium salt (Sigma Aldrich; St. Louis, MO). E12.5 was chosen since this stage of gestation correlates with the late first trimester in humans (Clancy et al 2007)—the time that infections are most closely linked to increased incidence of SZ and ASD (Atladottir et al. 2010, Brown et al. 2004). Poly(I:C) was freshly dissolved in saline and administered i.p. at 20 mg/kg based on the weight of the poly(I:C) itself, not including the total weight of the potassium salts. Control mice were injected with saline alone at 5 μl per gram body weight. This concentration of poly(I:C) is higher than that used for intravenous injections (Meyer et al. 2006) and was selected because it is the optimal i.p. dose that causes MIA, while preserving viability of offspring (Ito et al. 2010).
2.2 Blood collection and brain dissections
Control and poly(I:C) offspring were sacrificed at 5 ages: P0, P7, P14, P30, and P60. Both male and female offspring were used in this study. Mice were deeply anesthetized with nembutal (10 μl/g). At least 150 μl of blood/animal was first collected by cardiac puncture and transcardial perfusion was then performed using 10–30 ml of sterile PBS (by weight). P0 offspring were processed without perfusion. Whole brains were quickly removed and placed in ice-cold Earle’s balanced salt solution for microdissection of the FC, CC, and HC. All tissues were snap-frozen in liquid nitrogen and stored at −80°C. Both blood and brains were sent overnight on dry ice to U.C. Davis for processing.
2.3 Sample processing
Blood was centrifuged (12,000 × g, 4°C, 20 min) to obtain serum, which was then stored at −80°C. Frozen tissues were thawed and disrupted in Bioplex cell lysis buffer (BioRad) containing factors 1 and 2 (protease and phosphatase inhibitors, respectively; BioRad) and the protease inhibitor phenyl-methylsulfonyl fluoride (500 mM; Sigma–Aldrich). A small plastic pestle was used to homogenize the samples. Tissue was further homogenized by trituration using 200 μl pipette tips. The homogenate was then agitated for 30–40 min on ice and centrifuged at 4°C and 6000 × g (Eppendorf centrifuge 5417R) for 20 min. The supernatant was removed and aliquots stored at −80 °C. The protein content of each sample was determined using the BioRad Protein Assay (BioRad), with bovine serum albumin as a standard, according to the manufacturer’s protocol. Sample absorbances were read at 560 nm using a spectrophotometer (Perkin Elmer HTS7000).
2.2 Cytokine measurements
BioRad (Hercules, CA) 23-plex mouse kits were used for all assays. Assays were performed according to the manufacturer’s instructions. Reagents were kept on ice until use, minimizing exposure of the beads to light. All samples were run in duplicate and were assayed with the BioRad cytokine reagent kit and either the diluent kit for serum samples or the cell lysis kit for tissue samples. All buffers and diluents were warmed to room temperature prior to use. Lyophilized cytokine standards (containing IL-1α, IL-1β, IL-2, IL-3, IL-4, IL-5, IL-6, IL-9, IL-10, IL-12 (p40), IL-12 (p70), IL-13, Eotaxin, G-CSF, GM-CSF, IFNγ, KC, MCP-1, MIP 1α, MIP1β, RANTES, and TNF-α) were reconstituted first to a master standard stock using 500 μl of diluent. Nine concentrations of the standards were made by eight, three-fold serial dilutions of the master standard stock in either cell lysis buffer (for brain tissue) or serum diluent. Samples were run at 200 μg protein/well for the mouse brain homogenates. Serum samples were diluted 1:3 prior to assay. All samples were held at 4°C for 10 min before the start of the assay. Corresponding buffer blanks were run to determine the level of background. All the wash steps were performed on a Bio-Plex Pro Wash Station at room temperature. The plates were then read in the Bio-Plex 200 System and the data analyzed using BioPlex Manager 4.1 software with 5-parameter logistic regression (5PL) curve fitting to determine the standard curve from the 8 standards in duplicate and extrapolate the sample concentrations from the standard curve. The goodness-of-fit for each point on the standard curve was determined by the BioPlex Manager software. The standard recovery, calculated by taking the ratio of the calculated concentration value divided by the expected amount of standard, was within an acceptable range of recovery of between 70–130% for all of the standards used. Only standards and samples with coefficients of variance under 5% were used. Readings were excluded if they were at or below the background value.
2.3 MIA for immunohistochemistry
Female C57BL/6J mice (Charles River) were housed at U.C. Davis in accordance with the protocol approved by the Institutional Animal Care and Use Committee. Mice were mated overnight and the presence of a vaginal plug on the following morning was noted as day E0.5. Pregnant mice were injected (in the same fashion as for MIA for cytokine measurements described above) on E12.5 with saline or poly(I:C). Brains of offspring at the five ages were dissected into the three regions and post-fixed for 3 hrs in 4% paraformaldehyde in PBS. The paraformaldehyde was then replaced with 30% sucrose and left overnight at 4°C. The sucrose solution was changed twice until the brains sank. The brains were then frozen in OCT on dry ice and cut into 30 μm sections using a freezing microtome (Leica). The sections were blocked with 5% horse serum + 0.025% Triton in PBS for 2 hrs at room temperature, and then stained with primary antibodies, all at 1:1000: rabbit anti-IBA1 (WAKO, Japan), anti-CD45R (Abcam), rat anti-CD3 (R&D Systems), rat anti-GR1 (R&D Systems) at 4°C for 48 hrs. Sections were washed three times for 10 min each in PBS while shaking. Sections were incubated in secondary antibody for 90 min (1:200; Cy2 anti-rabbit, Cy3 anti-rabbit, and Cy2 anti-rat, Vector Laboratories) and mounted with Vectashield mounting media containing DAPI (Vector Laboratories) on 1% gelatin-coated slides.
2.4 Imaging
For assessing immune cell-infiltration, immunostaining was imaged with a 40× 1.2 NA objective on an epifluorescent microscope (Nikon E600, Nikon, Tokyo) under a mercury arc lamp using computer software to run the camera (a Spot View Advanced 2.0 (Diagnostic Imaging Inc.) For microglia, immunostaining was imaged using a 1.2 NA 40x oil objective on an Olympus Fluoview 2.1 laser-scanning confocal system.
2.5 Stereology
The density of Iba-1-positive microglia was quantified using stereological methods (Feng et al., 2011). Every third section (of nine sections) were used for a total of three sample sections per brain region. The Iba-1 cell counts were made on an epifluorescent microscope (Nikon E600, Nikon, Tokyo) and analyzed using Stereologer computer software (version 1.3, Systems Planning & Analysis, Inc., Alexandria, VA). Microglia cell counts were taken from FC layer 2–3, CC layer 2–3, and HC area CA1 of the stratum radiatum at five ages (P0, P7, P14, P30, P60). Microglia were identified by Iba-1-positive cell body staining. The brain region of interest was outlined using a 4× (0.67 NA) objective. Microglia identification and counting were performed with a 100x oil (1.2 NA) objective.
2.5 Blood-brain barrier integrity
25 mg/kg Evan’s blue dye was injected i.p. in offspring at the five ages examined. Four hours later, the brain was removed, rinsed in PBS, examined using a dissecting microscope (Olympus CK30-F100), and imaged using a digital camera (Olympus FE-370). Changes in the amount of Evans Blue signal were compared qualitatively.
2.6 Statistics
Unpaired t-tests were used to determine statistical significance (* = p< 0.05) using GraphPad Prism software.
2.7 Behavioral Testing
Behavioral tests were conducted on mice starting at six weeks of age according to previously published methods (Smith et al., 2007). Mice were tested for PPI of acoustic startle using SR-LAB startle chambers (San Diego Instruments). Mice were acclimated to the chambers for 5 minutes before exposure to 6, 120 db tones (startle stimulus). They were then subjected to 14 randomized blocks of either no startle, startle only, startle preceded by a 5 db pre-pulse, or startle preceded by a 15 db pre-pulse. PPI is defined as the percentage of (startle only – 5 or 15 db pre-pulse)/startle only. For LI testing, mice were placed in chambers with parallel-grid shock floors (Coulbourn Instruments). On the first day of testing, mice were presented with a pre-exposure to 40, 30 sec tones followed by three pairings of the tone with a mild foot shock. Non-pre-exposed mice are presented with the three pairings only. On the second day, mice were placed in the same chambers for 8 min to record freezing in response to the context. On the third day, mice were placed back in the same chambers and presented with an 8 min tone. LI is defined as the difference in freezing in response to the tone in pre-exposed mice compared to non-pre-exposed mice.
3. RESULTS
Several cytokines, including IL-1β, IL-6, IL-10, IFNγ, and TNFα, have been reported to be present in the healthy brain where they perform a wide range of functions (Deverman and Patterson, 2009; Garay and McAllister, 2010). However, it was unknown if other cytokines and chemokines are present in early postnatal development in the healthy brain, and if so, whether their levels change with age and following MIA. Here, we utilized the approach previously published for 3-plex BioRad luminex kits (Datta and Opp, 2008) for use with BioRad luminex mouse 23-plex bioplex kits. The high sensitivity of this approach allowed us to measure levels of 23 cytokines and chemokines from small regions of the developing mouse brain. The cytokines measured were IL-1α, IL-1β, IL-2, IL-3, IL-4, IL-5, IL-6, IL-9, IL-10, IL-12 (p40), IL-12 (p70), IL-13, IL-17, interferon gamma (IFNγ), tumor necrosis factor alpha (TNFα), granulocyte colony-stimulating factor (G-CSF), and granulocyte-macrophage colony-stimulating factor (GM-CSF). The chemokines measured included Eotaxin, keratinocyte chemoattractant (KC/CXCL1), monocyte chemoattractant protein-1 (MCP-1/CCL2), macrophage inflammatory protein-1α (MIP-1α/CCL3), MIP1β/CCL4, and regulated upon activation, normal T-cell expressed, and secreted (RANTES/CCL5).
Levels of these factors were measured in FC, CC, and HC at P0, P7, P14, P30, and P60. These brain regions were selected based on their involvement in ASD and SZ. The five ages represent periods before most synapses have formed (P0), the start of synaptogenesis (P7), the peak of synaptogenesis (P14), peak activity-dependent plasticity (P30), and early adulthood (P60). An average of six animals from at least two litters were used for each data point. Samples were run in duplicate and replicated on at least two arrays. Litters were obtained from pregnant mice injected at mid-gestation either with saline (typically-developing or control offspring) or with 20 mg/kg poly(I:C). We use maternal poly(I:C) injection at E12.5, since this stage of gestation correlates with the late first trimester in humans (Clancy et al 2007)—the time that infections are most closely linked to increased incidence of SZ and ASD (Atladottir et al. 2010, Brown et al. 2004).
3.1 Most cytokines are expressed in an age- and region-specific manner in the brain and blood of typically-developing offspring from birth to adulthood
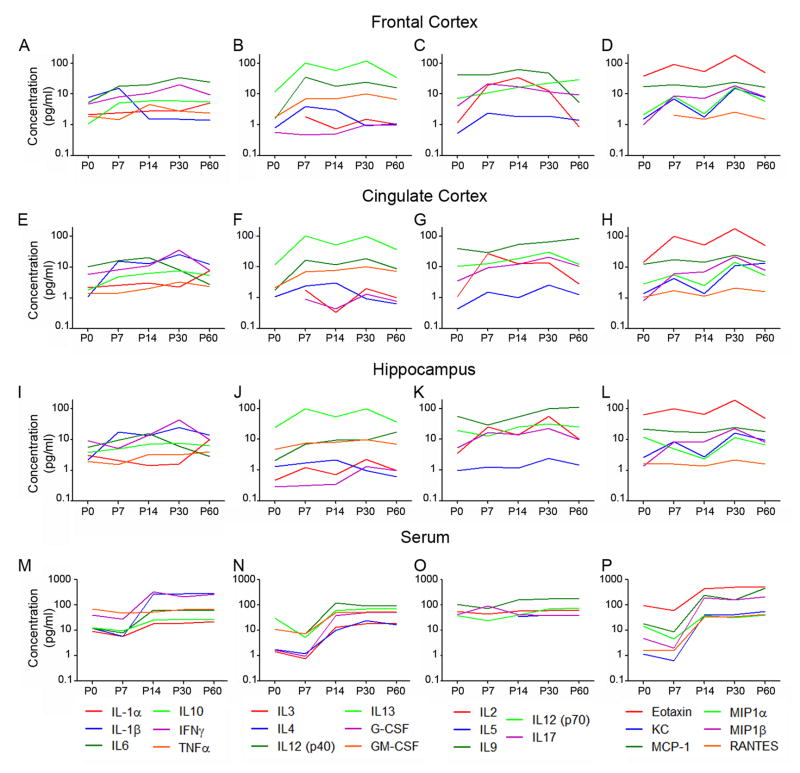
Surprisingly, most of the cytokines and chemokines examined are detectable in both brain and serum from control offspring, even at birth (Fig. 1). Although a few of the cytokines are undetectable in specific brain regions or serum during the first postnatal week, including IL-1α, IL-3, IL-4, IL-5, Eotaxin, G-CSF, and RANTES, all are detectable in brain and serum after the first postnatal week (Suppl. Tables 1–2). Most of the cytokine concentrations range from 1–100 pg/mg brain tissue. Cytokines with the lowest concentrations in multiple brain regions include IL-1α, TNFα, IL-3, IL-4, IL-5, G-CSF, and RANTES. Conversely, cytokines with the highest concentrations in multiple brain regions include IL-9, IL-13, and Eotaxin. Almost all cytokines are found at higher concentrations in serum (Fig. 1M–P) compared to brain (Fig. 1A–L; note that the scale is 10-fold greater for serum compared to brain regions).
Figure 1. Many cytokines are expressed in serum and brain throughout normal development.
Cytokine concentrations in the typically-developing brain change with age and some are region-specific. To illustrate changes in cytokine concentrations with age, the average values for each cytokine concentration are plotted at the five ages examined. Cytokine concentrations are plotted in pg/mg brain tissue (A–L) and pg/ml serum (M–P) for FC (A–D), CC (E–H), HC (I–L), and serum (M–P). The 23 cytokines are separated into 4 groups: (1) commonly-studied brain cytokines (A,E,I,M) including IL-1α, IL-1β, IL-6, IL-10, IFNγ, and TNFα, (2) a first set of additional cytokines with similar step-like changes in serum concentration with age (B,F,J,N) including IL-3, IL-4, IL-12(p40), IL-13, G-CSF, and GM-CSF, (3) a second set of additional cytokines with stable levels in serum (C,G,K,O) including IL-2, IL-5, IL-9, IL-12(p70), and IL-17, and (4) chemokines (D,H,L,P) including Eotaxin, KC, MCP-1, MIP1α, MIP1β, and RANTES. Error bars are not included in these graphs to enhance visibility of the trends in expression, however all values of mean ± SEM concentration are included in Suppl. Tables 1 and 2.
Cytokine concentrations in the typically-developing brain change with age and some changes are region-specific. To illustrate changes in cytokine concentrations with age, the average values for each cytokine concentration (pg/mg from brain and pg/ml from serum) are plotted at the five ages examined (Fig. 1). Error bars are not included in these graphs to enhance visibility of the trends in expression of each cytokine with age, however all values of mean ± SEM concentration are included in Suppl. Tables 1–2. For presentation, we separated the 23 cytokines into four groups: (1) commonly-studied cytokines, (2) a first set of additional cytokines with a similar step-like increase in serum concentration with age, (3) a second set of additional cytokines with stable levels in serum, and (4) chemokines.
Although the developmental profiles of these cytokines are diverse, some generalizations can be made. First, most cytokine profiles are similar across the three brain areas. This is most clearly seen for the chemokines, where the profiles for each chemokine in the three brain areas are nearly identical (Fig. 1D, H, L). There are, however, clear exceptions to this generalization, particularly in FC. For instance, IL-1β levels in HC and CC are similar with age, but quite different in FC where they are highest at P0 and P7 and then dramatically decrease at P14 (Fig. 1A, E, I). Levels of IL-9 are steadily high with age in CC and HC and are also relatively high in FC during the period of rapid synaptogenesis (P0–P14), but decrease in FC with maturity (Fig. 1C, G, K). Conversely, IL-6 decreases at P60 in HC and CC, but not in FC where it remains high in adulthood (Fig. 1A, E, I). A second point of interest is that some cytokines, including IL-4, IL-2, IL-17, are higher in mid-postnatal life, but lower at birth and in the adult (Fig. 1B–C, F–G, J–K). Third, several cytokines dip in concentration specifically at P14, a period of intense synaptogenesis; these include IL-3, IL-13, IL-12 (p40), Eotaxin, MIP1α, and KC in addition to IL-2 and IL-5 specifically in CC and HC (Fig. 1A–L). Fourth, another set of cytokines increase in concentration with age, including IL-6, IL-10, IFNγ, GM-CSF, IL-12 (p70), IL-17, and MIP1β (Fig. 1A–L). Finally, the concentration of a subgroup of cytokines does not change with age, including TNFα, G-CSF, MCP-1, and RANTES, in addition to IL-1α in FC and IL-10, IL-5, and GM-CSF in HC (Fig. 1A–L). Together, these results indicate that cytokines are expressed in the typically developing brain in an age- and region-specific manner.
Cytokine concentrations also change with age in serum (Fig. 1M–P), but the patterns are simpler than in brain and fall into just two distinct groups. Regardless of their starting concentration, 17 of the 23 cytokine levels are steady from P0 to P7 and then increase abruptly to a higher level at P14, where they remain through P60 (Fig. 1M–N,P). Importantly, this trajectory is not found in any area of the brain, indicating that the brain measurements are not significantly contaminated by blood cytokines and that changes in peripheral cytokines do not reflect the direction of cytokine changes in the CNS. The six other cytokines in the serum (TNFα, IL-2, -5, -9, -12, -17) remain at a constant level throughout development, a pattern that is also rare in the brain (Fig. 1O).
3.2 MIA alters brain cytokine profiles in an age-and region-specific manner
In order to determine if brain cytokines are altered in newborn MIA offspring and if these changes are developmentally regulated, pregnant mice were injected with poly(I:C) (MIA) or saline (control) in mid-gestation (E12.5) and FC, CC, and HC were collected from the offspring at P0, P7, P14, P30, and P60. The protein levels of 23 cytokines were measured as above on the same plates as the age-matched control samples. Average values were compared between saline and poly(I:C) offspring for each cytokine at each age in each brain region. Previous reports using ELISAs to measure cytokines in fetal brain of MIA offspring showed that some pro-inflammatory cytokines (IL-1β, IL-6, TNFα, and IFNγ) are increased in the brains of offspring during gestation within hours following MIA (Fatemi et al., 2008; Meyer et al., 2006b; Meyer et al., 2008). However, those studies did not determine if brain cytokines are chronically altered in postnatal MIA offspring and if so, what the trajectory of those changes is with age.
3.2.1 Frontal Cortex (FC)
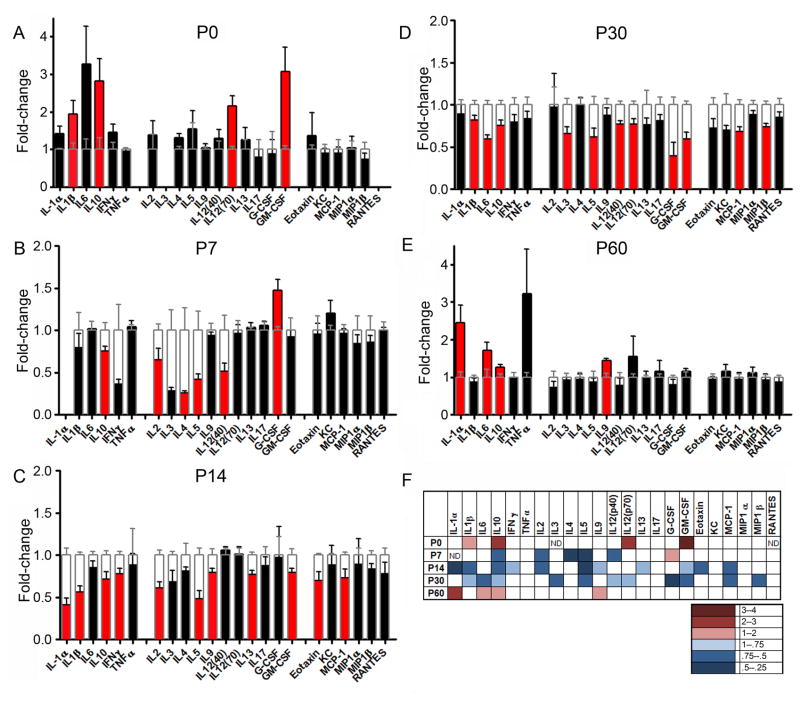
In FC, cytokine levels are altered at every age examined in MIA offspring (Figure 2A–F, Suppl. Table 1) and follow a clear pattern of elevations at birth, decreases throughout postnatal brain development (P7–P30), and elevations again in the adult. Compared to controls, many cytokines in MIA FC are higher at birth and in adulthood. At birth (Fig. 2A, F), four cytokines are significantly higher than controls: IL-1β (1.9-fold), IL-10 (2.8-fold), IL-12 (p70; 2.2-fold), and GM-CSF (3.1-fold). Although not statistically significant, IL-6 is dramatically higher (3.3-fold, p=0.09), and IL-1α (1.4-fold; p=0.07) and IL-4 (1.3-fold; p=0.09) trend toward higher levels. A somewhat different subset of cytokines is also higher in the adult FC (Fig. 2E–F), including IL-1α (2.5-fold), IL-6 (1.7-fold), IL-9 (1.4-fold), and IL-10 (1.3-fold).
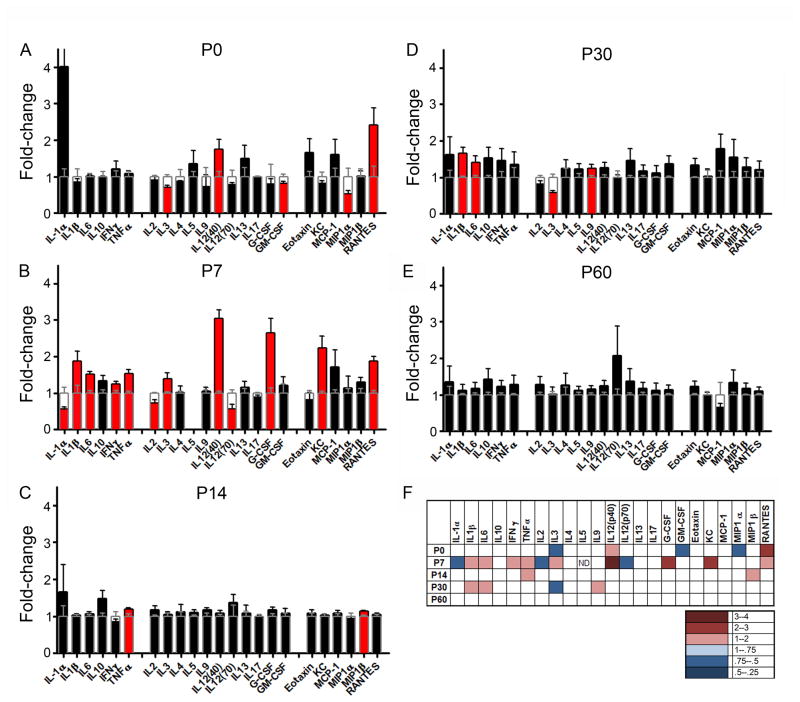
Figure 2. MIA induces long-lasting changes in cytokines in frontal cortex throughout development.
The fold-change ± SEM in cytokine concentration in MIA brain regions compared to control values is plotted. Values from MIA brains are either black or red, and the control values are superimposed in clear bars outlined in grey. Red bars indicate statistically significant changes compared to controls (p < 0.05). Increases are shown above 1 and decreases, below 1. (A) At P0, MIA-induced increases are found for four cytokines. IL-3 and RANTES are below the level of detection at this age. (B, C, D) At P7, P14 and P30, many cytokines in MIA FC are lower compared to controls. (E) At P60, fewer cytokines in MIA FC are altered and all of these are elevated. (F) A heat map is used to summarize the results for MIA-induced changes in cytokines at all ages examined. Statistically significant changes are indicated in color: red indicates increases, and blue decreases, in cytokine levels compared to controls. The degree of change is indicated by the depth of color as indicated in the lower panel. ND = below the level of detection. n = 5–6 brains per treatment group (pooled from at least two independent litters).
In contrast to the increased levels in MIA FC cytokines at birth and in the adult, many cytokines are lower than controls during the period of synaptogenesis and remodeling (P7, P14, and P30). Most of the cytokines that are elevated at P0 are not altered at P7 except for IL-10, which changes from being elevated 2.8-fold at P0 to being decreased (0.8-fold) at P7 (Fig. 2B,F). Including IL-10, six cytokines are significantly altered at P7. IL-2 (0.7-fold), IL-4 (0.3-fold), IL-5 (0.4-fold), and IL-12 (p40; 0.5-fold) are lower, while G-CSF is the lone cytokine that is higher at P7 (1.5-fold). Several additional cytokines trend toward significantly lower levels than controls, including IL-3 (0.2-fold, p=0.08) and IFNγ (0.4-fold, p=0.09). At P14 (Fig. 2C,F), several of these cytokines remain lower, including IL-2 (0.6-fold), IL-5 (0.5-fold), and IL-10 (0.7-fold) and an additional eight cytokines are lower at this age, including IL-1α (0.4-fold), IL-1β (0.6-fold), IL-9 (0.8-fold), IL-13 (0.8-fold), Eotaxin (0.7-fold), GM-CSF (0.8-fold), IFNγ (0.8-fold), and MCP-1 (0.7-fold). At P14, there are also trends toward significantly lower levels than controls (MIP-1β (0.8-fold, p=0.07) and IL-3 (0.7-fold, p=0.06)). Many cytokines remain lower than controls at P30 (Fig. 2D,F) including IL-1β (0.8-fold), IL-5 (0.6-fold), IL-10 (0.8-fold), GM-CSF (0.6-fold), and MCP-1 (0.7-fold), and an additional six cytokines are also lower at this age, including IL-3 (0.7-fold), IL-6 (0.6-fold), IL-12 (p40; 0.8-fold), IL-12 (p70; 0.8-fold), G-CSF (0.5-fold), and MIP-1β (0.7-fold).
Together, these results indicate that cytokines are indeed chronically altered in the FC of postnatal MIA offspring in a distinct developmental pattern. Both the subsets of cytokines that are altered and the direction of change are age-dependent. Perhaps most surprising, many cytokines are altered in the MIA FC and the majority of these cytokines are significantly decreased during the periods of circuit formation and plasticity within the FC (Fig. 2F).
3.2.2 Cingulate Cortex (CC)
In CC, cytokine levels are also changed at every age examined in MIA offspring compared to controls (Figure 3A–F, Suppl. Table 1) in a pattern similar to that found in FC. As in FC, cytokines are generally higher at birth and in adulthood and lower during the periods of synaptogenesis and plasticity (P7, P14, and P30). At birth (Fig. 3A,F), three cytokines are significantly higher than controls: IFNγ (1.4-fold), IL-12 (p70; 1.6-fold), and MCP-1 (1.4-fold). Although not statistically significant, IL-1α (1.9-fold, p=0.07) and IL-10 (1.7-fold, p=0.06) are also higher in the CC at birth. A somewhat different subset of cytokines is higher in the adult CC (Fig. 3E,F), including IL-10 (1.4-fold) and IFNγ (1.5-fold). MIP1α (1.45-fold) and RANTES (1.6-fold) are also close to significance and TNFα and IL-2 are dramatically higher (3.4- and 2.9-fold, respectively) but not statistically significant in the adult MIA CC.
Figure 3. MIA induces long-lasting changes in cytokines in cingulate cortex throughout development.
Data is plotted as in Fig. 2. (A) At P0, MIA induces increases in three cytokines. (B) At P7, five cytokines are lower than controls, while IL-17 is the only elevated cytokine at this age. IL-1α, IL-3, and IL-4 are below the level of detection. (C) At P14, eight cytokines are also lower. (D) At P30, eleven cytokines remain lower than controls. (E) At P60, fewer cytokines are altered and both are higher than controls. (F) A heat map is used to summarize the results for MIA-induced changes in cytokines at all ages examined. Statistically significant changes are indicated in color: red indicates increases and blue decreases in cytokine levels compared to controls. The degree of change is indicated by the depth of color as indicated in the lower panel. ND = below the level of detection. n = 5–6 brains per treatment group (pooled from at least two independent litters).
Similar to the pattern in FC, many cytokines are lower than controls during the periods of synaptogenesis and remodeling. By P7 (Fig. 3B,F), all of the cytokines that are higher at P0 return to control levels, but a new set of six cytokines is significantly altered: five are lower, including IL-2 (0.4-fold), IL-5 (0.6-fold), IL-6 (0.3-fold), IL-10 (0.7-fold), and Eotaxin (0.6-fold), while IL-17 is dramatically higher (2.2-fold). Although not statistically significant, IFNγ (0.3-fold, p=0.08), IL-12 (p70; 0.7-fold, p=0.07), and KC (1.5-fold, p=0.06) also trend away from controls in MIA CC. Of the cytokines altered at P7, IL-10 remains lower at P14 (0.7-fold) as does IL-17, but the direction of change in IL-17 is reversed (0.8-fold; Fig. 3C,F). In addition, five different cytokines are significantly lower in the P14 MIA CC, including IL-1β (0.6-fold), GM-CSF (0.63-fold), IFNγ (0.7-fold), KC (0.7-fold), MCP-1 (0.6-fold), and MIP-1β (0.7-fold). Although Eotaxin and MIP-1α are also lower in P14 MIA CC (Fig. 3C), they are not statistically different from controls. At P30, even more cytokines are lower in MIA CC compared to controls (Fig. 3D,F). Four cytokines that are lower at P14 remain lower than control levels at P30, including IL-1β (0.8-fold), IL-10 (0.7-fold), IL-17 (0.7-fold), and MCP-1 (0.8-fold) and seven additional cytokines are also lower at P30: IL-3 (0.7-fold), IL-4 (0.7-fold), IL-5 (0.7-fold), IL-6 (0.2-fold), IL-12 (p40; 0.8-fold), IL-12 (p70; 0.8-fold), and G-CSF (0.6-fold). IL-13 (0.7-fold, p=0.08), IFNγ (0.7-fold, p=0.08), and MIP1α (0.8-fold, p=0.08) are also close to significantly decreased at P30.
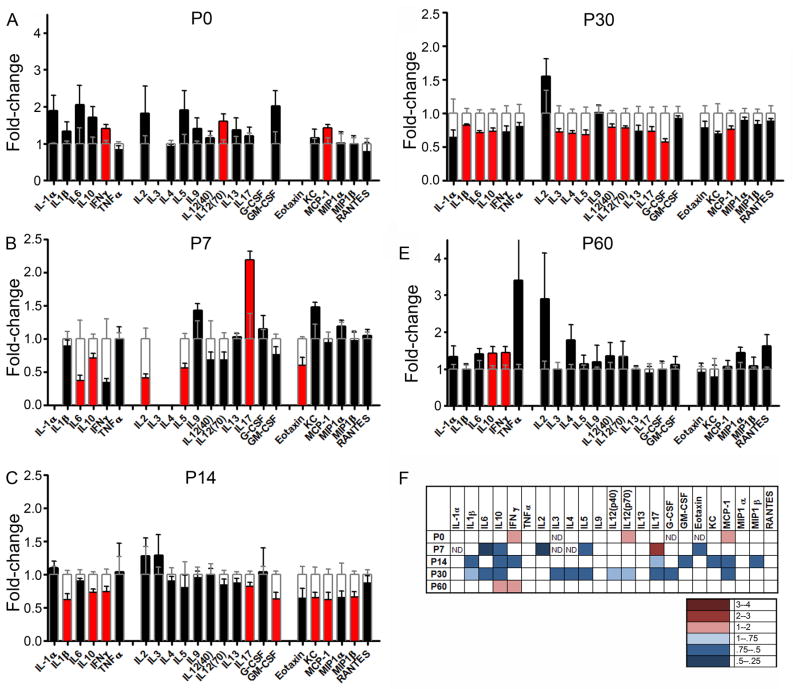
3.2.3 Hippocampus (HC)
In HC, MIA induces changes in the levels of cytokine at every age examined except for P60 (Fig. 4A–F, Suppl. Table 2) in a pattern distinct from that found in FC and CC. However, unlike the clear directional switch in MIA-induced changes in FC and CC in the first postnatal week, the direction of change in cytokine levels is mixed at most ages in HC. At birth (Fig. 4A,F), seven cytokines are altered in MIA HC. IL-6 (1.6-fold) is significantly elevated over controls, while IL-1β (0.7-fold), IL-2 (0.6-fold), IL-4 (0.8-fold), KC (0.7-fold), MCP-1 (0.7-fold), and MIP-1α (0.3-fold) are lower. Although not statistically significant, IL-13 is also lower at birth (0.7-fold, p=0.06). Of the cytokines altered at P0, only IL-4, KC, and MIP-1α remain changed at P7 (Fig. 4B,F): IL-4 remains lower (0.6-fold) and KC and MIP1α reverse direction towards a large elevation at P7 (1.6-fold; 1.6-fold). Four different cytokines are altered at P7 including IL-3 (0.4-fold), IL-5 (0.7-fold), IL-9 (1.6-fold), and IL-10 (0.8-fold). At P14, eight cytokines are significantly different in MIA HC compared to controls (Fig. 4C,F). Compared to the cytokines altered at P7, only IL-5 (0.4-fold) remains lower, and IL-9 is reversed in direction from being higher at P7 to being lower at P14 (0.7-fold). At P14, six different cytokines are altered in MIA HC: IL-1α (1.4-fold), IL-2 (0.4-fold), IL-6 (1.5-fold), Eotaxin (0.7-fold), MCP-1 (0.8-fold), and RANTES (0.6-fold). At this age, IL-10, IL-12 (p40), and MIP-1β are also lower than controls, although not significantly. Far fewer cytokines are altered in MIA HC at P30 (Fig. 4D,F). Only two cytokines are significantly lower than controls—IL-6 (0.6-fold) and MIP-1α (0.8-fold)—although several other cytokine changes approach significance including IL-1β (0.8-fold; p=0.09), IL-12 (p70; 0.7-fold; p=0.06), IL-13 (0.7-fold, p=0.08), G-CSF (0.6-fold, p=0.08), and RANTES (0.8-fold, p=0.09). Compared to controls, no cytokines are significantly altered in HC in adult MIA offspring (Fig. 4E, F).
Figure 4. MIA induces long-lasting changes in cytokines in hippocampus throughout development.
Data is plotted as in Fig. 2. (A) At P0, MIA induces higher levels of IL-6 and lower levels of six other cytokines, while MIP1α, IL-3, and RANTES are below the level of detection. (B) At P7, three cytokines are elevated, while four are lower than controls. IL-1α and G-CSF are below the level of detection. (C) At P14, IL-1α and IL-6 are higher and six other cytokines are lower than controls. (D) At P30, IL-6 and MIP1α are lower than controls. (E) At P60, no cytokines levels are changed relative to controls. (F) A heat map summarizes the results for MIA-induced changes in cytokines at all ages examined. Statistically significant changes are indicated in color: red indicates increases and blue, decreases in cytokine levels compared to controls. The degree of change is indicated by the depth of color as indicated in the lower panel. ND = below the level of detection. n = 5–6 brains per treatment group (pooled from at least two independent litters).
3.3 MIA alters cytokine profiles in serum in an age-specific manner
MIA also causes chronic changes in cytokine levels in the serum of offspring throughout postnatal development (Figure 5A–F, Suppl. Table 2). At birth, five cytokines are altered in MIA serum compared to controls. IL-12 (p40; 1.8-fold) and RANTES (2.4-fold) are higher, while IL-3 (0.7-fold), GM-CSF (0.8-fold), and MIPα (0.5-fold) are lower than controls (Fig. 5A,F). However, the most dramatic changes are one week after birth (P7), when twelve cytokines are altered in MIA serum (Fig. 5B,F). IL-1β (1.9-fold), IL-3 (1.4-fold), IL-6 (1.5-fold), IL-12 (p40; 3.0-fold), G-CSF (2.6-fold), IFNγ (1.3-fold), KC (2.2-fold), RANTES (1.9-fold), and TNFα (1.5-fold) are all higher, while IL-1α (0.6-fold), IL-2 (0.7-fold), and IL-12 (p70; 0.6-fold) are lower relative to controls at P7. By P14 (Fig. 5C,F), most of these widespread changes in MIA sera are back to control levels except for TNFα, which remains slightly higher (1.2-fold) and MIP-1β, which is significantly higher (1.1-fold). Although not statistically significant, IL-10 is also higher at P14 (1.5-fold, p=0.07). At P30, the cytokine profile is changed again, and four different cytokines are altered: IL-1β (1.7-fold), IL-6 (1.4-fold), and IL-9 (1.2-fold) are higher than controls, while IL-3 (0.6-fold) is lower (Fig, 5D,F). In adults, no significant differences in cytokine levels relative to controls are found in sera of MIA offspring (P60; Fig. 5E–F).
Figure 5. MIA induces long-lasting changes in cytokines in serum throughout development.
Data is plotted as in Fig. 2. (A) At P0, MIA increases two cytokines and decreases three. (B) At P7, MIA increases levels of nine cytokines and decreases three. IL-5 is below the level of detection at this age. (C) At P14, two cytokines are higher than controls. (D) At P30, three cytokines are increased and one is decreased. (E) At P60, no cytokines levels are changed relative to controls. (F) A heat map to summarize the results for MIA-induced changes in cytokines at all ages examined. Statistically significant changes are indicated in color: red indicates increases, and blue decreases, in cytokine levels compared to controls. The degree of change is indicated by the depth of color as indicated in the lower panel. ND = below the level of detection. n = 5–6 brains per treatment group (pooled from at least two independent litters).
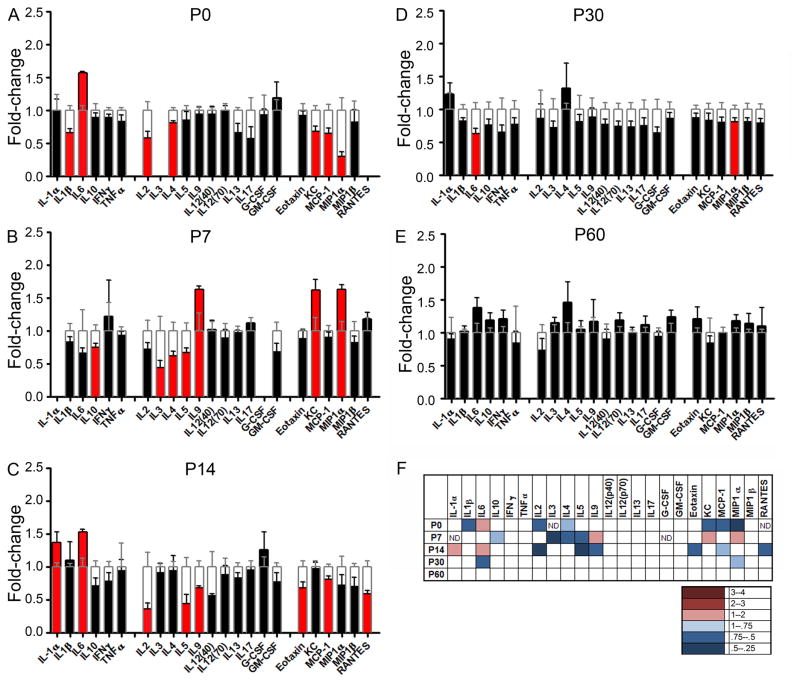
3.4 MIA-induced changes in serum cytokines do not correlate with changes in brain cytokines
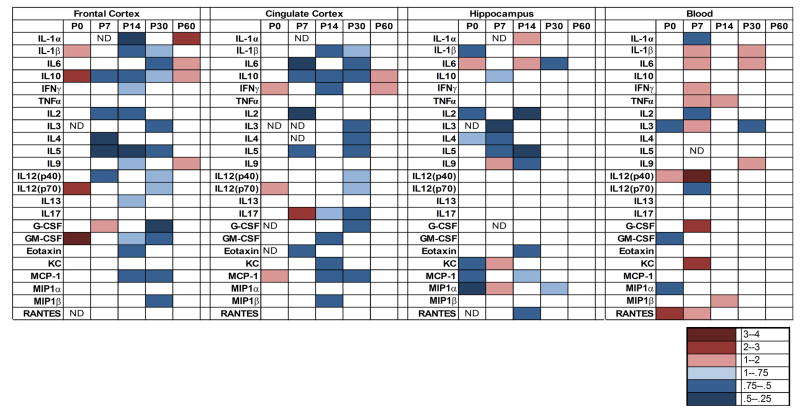
As illustrated in the summary Fig. 6, MIA causes changes in cytokine levels in brain and serum in offspring throughout postnatal development. In this figure, only statistically significant changes in cytokine levels are indicated by colored boxes; the direction and magnitude of change is indicated by red for higher, and blue for lower, levels than controls. These MIA-induced changes are complex, being both age- and region-specific, and involve significant changes at some point during development in levels of 22 of the 23 cytokines assayed in brain (the exception being TNFα). In striking contrast to the generally consistent cytokine profiles between brain regions in the control brain, at a given age, the nature and direction of MIA-induced changes in cytokines are different between brain regions. Moreover, within each brain region, the MIA-induced changes are different between ages. Although the changes are complex, they are not random; instead, they fall into a few, distinct patterns. In general, compared to controls, many cytokines in FC and CC are higher at P0, lower from P7–P30, and then higher again in the adult, although the specific cytokines that are altered at each age differ between these two regions. This general pattern of cytokine change is distinct from that in the HC, where fewer cytokines are altered and their direction of change is mixed at each age. Finally, the changes in cytokine levels observed in serum are also different at each age, but as in the control brains, these changes do not correlate with changes in cytokine levels in any brain region from the same animals. This supports the conclusion that our brain cytokine measurements are unlikely to be contaminated by serum cytokines. Finally, although cytokine levels are altered in all three brain regions and serum throughout postnatal development, they remain altered in the adult only in FC and CC, but not in HC or serum.
Figure 6. Summary of cytokine changes in brain and serum across development.
A heat map is used to summarize the results for MIA-induced changes in cytokines at all ages examined. Statistically significant changes are indicated in color: red indicates increases and blue indicates decreases in cytokine levels compared to controls. The degree of change is indicated by the depth of color as indicated in the lower panel. This figure clearly shows the similar overall pattern in MIA-induced cytokine changes in FC and CC during development, characterized by increases in cytokines at birth (P0) and in the adult (P60), and dramatic decreases in many cytokines during periods of synaptogenesis and activity-dependent plasticity (P7–P30). This pattern is distinct from that in HC, where there are both increases and decreases in cytokine in MIA offspring at all ages examined. Finally, MIA-induced changes in serum cytokines do not correlate with changes in brain cytokines. ND = below the level of detection.
3.5 MIA-induced changes in brain cytokines are not due to immune cell infiltration through a leaky blood-brain barrier
Changes in brain cytokines in MIA offspring could be due to cytokines produced by infiltrating immune cells, which might gain access to the brain through MIA-induced breaches in the blood-brain barrier (BBB). To test this possibility, first BBB integrity was qualitatively assessed using Evans Blue (Suppl. Fig. 1); breaches in BBB integrity are typically indicated by dark blue staining of the brain. There is little to no BBB permeability detected at any postnatal age examined and no change in staining of MIA brains compared to controls at any age tested. Second, immune cell infiltration into the three brain regions was examined using immunohistochemistry with cell-type-specific antibodies to label B and T lymphocytes and neutrophils (Suppl. Fig. 2A). In general, there is virtually no staining for any of these immune cell types in any region of the brain at any age examined. This lack of staining is not due to an inability of our protocol to detect these cells, since we obtain clear labeling of these cells in spleens of control mice and spinal cord from EAE mice (Suppl. Fig. 2B). Taken together, these results support the interpretation that the MIA-induced changes in brain cytokines are most likely produced by brain-resident cells.
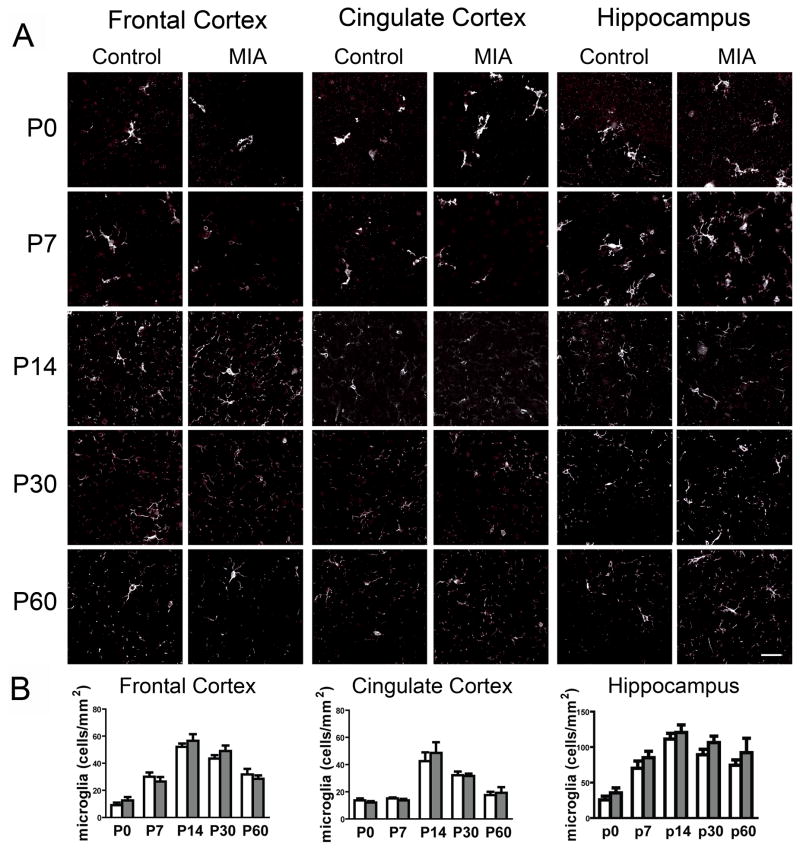
3.6 Microglial number is not altered by MIA
Microglia are present in the brain during all stages of development and are well-documented to increase in number and state of activation during neural inflammation (David and Kroner, 2011; Ransohoff and Perry, 2009). Because of the subjectivity inherent in classifying microglial activation morphologically, we chose to quantify only microglial density in sections from MIA and control brains. Microglia were labeled with the standard marker, Iba1, using immunohistochemistry and counted using Stereologer (Fig. 7). There are no qualitative changes in microglial morphology in any brain region from MIA offspring compared to controls (Fig. 7A). In general, the density of microglia in each brain region increases from low levels at birth to a peak at P14 and then decreases to intermediate levels in the adult brain (Fig. 7B). MIA does not cause any significant change in microglial density within any of the three brain regions at any of the five ages examined (Fig. 7B).
Figure 7. MIA does not alter microglial number or morphology.
The density of Iba1 + microglia (white) was quantified using Stereologer in each brain region at each age examined. (A) Representative images of coronal sections taken at 40X through FC, CC, and HC at five ages during postnatal development. (B) Quantification of the density of Iba1+ microglia for each brain region over age. The density generally increases from birth to P14 and then decreases to intermediate levels in the adult. There is no difference in microglial density between MIA and control brains. Open bars indicate control values and gray bars, MIA values.
3.7 Behavioral abnormalities in MIA offspring
Previous studies have documented ASD- and SZ-relevant abnormal behaviors in adult poly(I:C)-induced MIA offspring (Meyer and Feldon, 2010). To confirm that the MIA mice used in this study were likely to exhibit the expected behavioral changes, we tested two of these behaviors in a parallel cohort of animals that was raised alongside the cohort used for cytokine measurements. The two behavioral tests performed were LI and PPI. LI is a measure of the ability to ignore irrelevant stimuli and its disruption is considered to be pertinent for the cognitive deficits in SZ (Weiner, 2003). LI is disrupted in SZ subjects and in amphetamine-treated humans and rats, restored to normal levels in SZ by neuroleptic drugs, and enhanced in normal humans and rats by antipsychotic drugs (Weiner, 2003). PPI measures sensorimotor gating, and deficits are present in ASD, SZ and several other mental disorders. As in prior work (Meyer et al., 2009; Patterson, 2009) we find deficits in LI and PPI in the parallel cohort of mice used here (data not shown). MIA offspring exhibit increased freezing in response to a conditioned acoustic cue (LI) compared to controls when measured against the non-pre-exposed group [F(1, 23)=1.029, p=0.0149; n=28 saline, 24 poly(I:C)]. Compared to control offspring, MIA offspring also display decreased PPI when presented with either a 5 dB pre-pulse or 15 dB pre-pulse preceding a 120 dB pulse (PPI5 and PPI15, respectively) [F(1, 104)=4.830, p=0.0302; n=29 saline, 25 poly(I:C)].
4. Discussion
In order to determine if poly(I:C)-induced MIA leads to chronic changes in brain and blood cytokines in offspring throughout postnatal development, proteomic analysis of the cytokine response in the developing brains of offspring was performed. In typically-developing, control offspring, we find that most of the cytokines examined are present in serum as well as in the three brain regions examined from birth through adulthood. This data adds new evidence to the case that cytokines play a role in normal brain development and function (Deverman and Patterson, 2009; Garay and McAllister, 2010; Gilmore et al., 2004; Juttler et al., 2002; McAfoose and Baune, 2009; Stellwagen, 2011). Another striking observation from the control data is that the levels of 17 of the 23 cytokines assayed in serum increase abruptly on P14, and they remain at that level through P60. Although many aspects of immune system development occur during the second postnatal week in mice, the precise events that lead to this abrupt increase in serum cytokines are unknown. Importantly, this jump in cytokine levels is not found for any of the 23 cytokines in any of the brain areas, indicating that the measurements in the brain are not significantly contaminated by serum cytokines.
Remarkably, most of the 23 cytokines examined are altered in the brains of MIA offspring and these changes occur in a region- and age-specific manner. While several of the commonly studied, pro-inflammatory cytokines are altered by MIA, significant and widespread changes in anti-inflammatory cytokines and chemokines are also detected in brain and serum at every age examined. Although complex, MIA-induced changes in brain cytokines fall into a few, distinct patterns. In FC and CC, many pro- and anti-inflammatory cytokines are elevated in early postnatal MIA offspring, lower than controls in early adolescence, and a few cytokines are again elevated in the adult brain. The developmental pattern in HC is distinct from the other brain areas, with both increases and decreases in cytokines occurring at every age examined, except in the adult. Finally, these striking and complex changes in brain and serum cytokines are not accompanied by obvious changes in BBB permeability, immune cell infiltration, or increases in microglial density. Together, these data indicate that MIA leads to significant changes in brain cytokines in the postnatal offspring, which may alter CNS development and behavior in the absence of overt signs of neural inflammation.
The poly(I:C) MIA mouse model employed in this study has both face and construct validity for ASD and SZ, and predictive validity for at least SZ (Meyer and Feldon, 2010). Despite recent progress in developing and characterizing rodent MIA models, little is known about how MIA alters fetal brain development. Current evidence indicates that the maternal cytokine response is crucial (Patterson, 2009). Poly(I:C) injection at either mid- or late gestation leads to marked increases in levels of IL-1β, IL-6, IL-10, and TNF-α in the pregnant dam’s serum (Gilmore et al., 2005; Koga et al., 2009; Meyer et al., 2006b), which is reminiscent of similar increases in serum cytokines in mothers of children with ASD (Goines et al., 2011). Perturbation experiments indicate that IL-6 is necessary and sufficient to mediate the effects of the maternal immune response in the fetus (Smith et al., 2007). Induction of maternal cytokines then alters cytokine expression in the fetal brain, including IL-1β, -6, -10, -13, and -17, and MCP-1 and MIP1α, hours after MIA (Arrode-Bruses and Bruses, 2012; Meyer et al., 2006b), but it has been unclear if MIA causes changes in brain cytokines in postnatal offspring.
It has been suggested that brain cytokines would be altered in MIA offspring based on observations of neural inflammation and cytokine changes in blood, CSF, and postmortem brain tissue from individuals with ASD and SZ (Ashwood et al., 2011; Ashwood et al., 2011; Ashwood et al., 2010; Chez et al., 2007; Molloy et al., 2006; Pardo et al., 2005; Vargas et al., 2005). These human data predict that pro-inflammatory cytokines may be chronically increased in MIA brains and indeed, most of the few cytokines previously detected in the brains of MIA offspring were acute phase cytokines including IL-6, IL-1β, IFNγ, and TNFα (Gilmore et al., 2005; et al., 2006b; Meyer et al., 2008). Here, we took an unbiased approach to test this hypothesis and measured cytokine levels throughout postnatal development. Our results clearly demonstrate that MIA leads to dynamic changes in cytokine levels in the brains of offspring. Our results are also somewhat consistent with the expected pro-inflammatory changes in brain cytokines resulting from MIA in that there are increases in some of the acute phase cytokines at birth and in the adult MIA FC, CC, and HC, as well as in serum throughout development.
Although it is theoretically possible that these MIA-induced changes in brain cytokines in offspring could be influenced by changes in the dam’s behavior following MIA, there is little evidence supporting this possibility. The dosage of poly(I:C) administered results in an approximately three hour period of sickness behavior (lethargy, lack of grooming, etc.), after which the mother recovers fully. Consistent with this, levels of maternal and placental pro-inflammatory cytokines peak by 3 hours post injection and decline considerably by 24 hours post injection (Meyer et al. 2006). The dam loses weight (~1.0–1.5 g) by 24 hours post-injection, but recovers to levels comparable to controls by 48 hours post injection. We find no difference between poly(I:C) and saline-injected mothers in maternal care, as measured by equivalent time spent with pups and comparable latency to retrieve individual pups removed from the nest (Malkova and Patterson, personal communication). Although cross-fostering control offspring with immune-challenged mothers can alter behavior in control offspring (Meyer et al. 2006c), there is extensive evidence that cross-fostering MIA offspring with control mothers does not protect against the emergence of neuropathology and behaviors in the offspring (Meyer et al. 2008). Together, current data in the field is most consistent with the hypothesis that MIA causes changes in brain development that lead to ASD- and SZ-like behaviors in offspring.
Despite evidence for a pro-inflammatory brain cytokine profile at birth and in the adult MIA offspring, our results also reveal that MIA induces long-lasting changes in a surprisingly wide range of cytokines. These cytokines include both pro-inflammatory, anti-inflammatory, and regulatory cytokines, as well as several chemokines. In fact, most of the cytokines examined are significantly altered at some point in the MIA brain compared to controls. Perhaps most important, our results also reveal an unexpected and widespread decrease relative to controls in many brain cytokines during peak periods of synaptogenesis and plasticity (P7–P30). These decreases are in contrast to the expected pro-inflammatory phenotype and suggest that dramatically decreased cytokine signaling may be a critical variable causing altered brain connectivity and ASD and SZ-like behaviors in the offspring. Consistent with this idea, decreases in a few cytokines have been reported in postmortem brain tissue from individuals with ASD (Vargas et al., 2005) and SZ (Toyooka et al., 2003). The impact of widespread decreases in brain cytokines on the development and plasticity of cortical connections and synaptic transmission and plasticity will be the focus of future studies.
There is a rich complexity in the region- and age-specific changes in MIA brain cytokines. There are only a few reports of brain region-specific changes in cytokine levels following any manipulation, but our data and the few reports in non-MIA mouse models (Johnson and Kan, 2010; Kasten-Jolly et al., 2011) are consistent with the single report of region-specific changes in postmortem brain tissue from individuals with ASD (Vargas et al., 2005). Region-specific changes in overall gene expression have also been reported for SZ and ASD (Focking et al., 2011; Ji et al., 2011; Suda et al., 2011), suggesting that regional-specificity may contribute to both disorders. Detection of region-specificity of MIA-induced cytokine changes during development was made possible only recently due to the increased sensitivity of multiplex analysis from small amounts of tissue (Datta and Opp, 2008). The advantage of the Luminex x-map technology over traditional ELISAs is that the former requires only a small sample volume (50μl) to simultaneously measure multiple analytes. Luminex technology is being utilized to measure adult brain cytokines in an increasing number of reports (Abazyan et al., 2010; Dalgard et al., 2012; Datta and Opp, 2008; Erickson and Banks, 2011; Gandhi et al., 2007; Li et al., 2009; Mukherjee et al., 2011), and the greater sensitivity of the Bioplex system we used has been validated against both ELISA and other multi-plex systems (Fu et al., 2010; Mukherjee et al., 2011). Our results clearly demonstrate that a single, common maternal immune response (MIA during mid-gestation) can cause long-lasting changes in cytokines that are specific to particular brain regions. How this occurs is unknown, but may involve differential responses to MIA-induced cytokines elevated in fetal development mediated by well-documented region-specific differences in the distribution of cytokine receptors in the normal fetal brain (Bauer et al., 2007; Garay and McAllister, 2010). In the future, additional research is needed to determine if these region-specific patterns of changes in brain cytokines contribute to specific ASD- and SZ-like behaviors in offspring.
In addition to region-specific changes in brain cytokines, we also observe age-specific changes. Within a given brain region, the profile of cytokines that is altered in MIA offspring is distinct at each age. This dynamic response is not unexpected since cytokines are part of both positive and negative feedback loops that regulate each other’s expression and function to keep immune responses within a homeostatic range. Individual cytokines do not work in isolation, but rather in complex networks (Careaga et al., 2010). Interestingly, we find no obvious pattern in the age-specific changes in terms of alternating pro-or anti-inflammatory cytokines. However, classifying cytokines in this way is only partially useful as most cytokines can be either pro- or anti-inflammatory depending on the cellular context and the levels of other cytokines. Moreover, the biological effects of individual cytokine levels can vary widely—a small change in levels of some cytokines can cause dramatic physiological effects, while large changes in others may have minimal outcomes. Taken together, these properties caution against general conclusions about the effects of MIA-induced changes in cytokines on inflammation in the brain.
Another indication that cytokines may not have traditional pro- or anti-inflammatory roles in MIA brains is that there is no overt evidence of inflammation in any brain region at any age examined, even at times when traditionally pro-inflammatory cytokines are elevated. The lack of immune cell infiltration into the brain, combined with little evidence of changes in gross BBB permeability, suggests that poly(I:C) MIA does not cause inflammation in the postnatal brain in the classic sense. Consistent with this interpretation, there is also no change in microglial density in any of the three brain regions examined and there is no qualitative change in microglial morphology in MIA brains (Fig. 7). These results are also consistent with a lack of immune cell infiltration, but inconsistent with reports of microglial activation in postmortem brain tissue from ASD individuals (Vargas et al., 2005). Since increased brain cytokines cannot be attributed to infiltrating immune cells, it is possible that any of the cell types endogenous to the brain could be responsible. Prior work has shown that neurons, microglia, and astrocytes can produce cytokines during normal development in vivo (Deverman and Patterson, 2009). Although cytokines could in principle also come from the periphery by crossing the BBB, the postnatal BBB is relatively impermeable to most cytokines (Erickson and Banks, 2011) and MIA-induced changes in brain cytokines are region-specific and do not correlate with serum cytokines at any age (Fig. 6). Identifying the source and targets of the MIA-induced cytokines will be important for understanding the consequences of these changes on neuronal connectivity and potentially glial function.
Both epidemiological and experimental results indicate that the effect of MIA on neuropathology and behavior in offspring is determined by the timing of the infection. Maternal viral infection during the late first and early second trimesters, in particular, is associated with increased risk of ASD (Atladottir et al., 2010; Brown 2012; Hagberg et al., 2012; Patterson, 2011a). Similarly, infection during early to mid-pregnancy is related to an increase in risk for SZ in offspring (Brown et al., 2004; Brown 2012). Moreover, differential effects of poly(I:C) injection during early versus late gestation on neuropathology and behaviors in offspring have been found in the MIA mouse model (Meyer et al 2006b). Our experiments used poly(I:C) injection at E12.5, since this stage of gestation correlates with the late first trimester in humans (Clancy et al 2007)—the time that infections are most closely linked to increased incidence of ASD and SZ (Atladottir et al. 2010, Brown et al. 2004).
Remarkably, many of the cytokines altered in the MIA brains and serum are similar to those found to be altered in ASD and SZ (Bauer et al., 2007; Brown and Patterson, 2011; Careaga et al., 2010; Nawa et al., 2000). Significant increases in plasma cytokine levels (IL-1β, IL-6, TNFα, IFNγ, IL-8, IL-12p40) have been reported in children diagnosed with ASD when compared with children without a family history of ASD (Ashwood et al., 2011; Molloy et al., 2006; Vargas et al., 2005). Most of these cytokines are also increased at P7 in MIA offspring serum (Figs. 5,6). Chemokines, including Eotaxin, RANTES, and MCP-1, are also elevated in the serum of autistic children (Ashwood et al., 2011) and all of these are elevated in MIA serum at P7 (Fig. 6). Neural inflammation, marked by increased pro-inflammatory cytokines and chemokines, including IFN-γ, IL-1β, IL-6, IL-12p40, TNF-α, and MCP-1, is also found in postmortem brain tissue from individuals with ASD over a wide range of ages (Vargas et al., 2005). Although we found changes in many of these cytokines in the MIA mouse brain, it is difficult to directly compare these results because of the wide range of ages examined in the human study (4–45 years of age). Similar findings in SZ also indicate elevated levels of cytokines in the blood of patients, including elevations in IL-1β, IL-6, IL-12, IFNγ, TNFα, and RANTES (Kunz et al., 2011; Yao et al., 2003), although many of these studies did not control for secondary variables and often report conflicting results. The fact that the poly(I:C) model displays several cytokine changes in common with both SZ and ASD reinforces the construct validity of the model, given that these disorders share the risk factor of maternal infection and that their psychiatric and anatomical pathologies significantly overlap (Lord et al., 2000; Meyer et al., 2011; Rapoport et al., 2009). How the risk of these distinct disorders is increased in humans via a single environmental risk factor is currently unknown but is likely to involve genetic susceptibility and/or the timing and intensity of the infection (Fatemi et al., 2008; Meyer et al., 2006a,b). Identifying how this large family of signaling molecules, the cytokines, are altered over time in brain development by infection and other environmental risk factors may highlight targets for novel diagnostic tests and new immune-based therapies for ASD and SZ in the future.
Supplementary Material
Average concentrations (pg/ml for brain regions and pg/ml for serum) ± SEM for 23 cytokines are shown for saline (control) and poly(I:C) (MIA) conditions for each brain region at each age. The fold-change in cytokines resulting from MIA was calculated as the ratio of the average values for poly(I:C)/saline (P/S). P-values for t-tests between MIA and controls for each comparison are also indicated. Grey fills indicate cytokines that are significantly different between MIA and control values (p<0.05). ND = not detected.
Average concentrations (pg/ml for brain regions and pg/ml for serum) ± SEM for 23 cytokines are shown for saline (control) and poly(I:C) (MIA) conditions for HC and serum at each age. The fold-change in cytokines resulting from MIA was calculated as the ratio of the average values for poly(I:C)/saline (P/S). P-values for t-tests between MIA and controls for each comparison are also indicated. Grey fills indicate cytokines that are significantly different between MIA and control values (p<0.05). ND = not detected.
Representative brains from control and MIA offspring are shown for each of the four ages examined, following Evans Blue staining to detect BBB permeability. There is no qualitative difference in BBB permeability in MIA brains compared to controls at any age examined.
(A) Representative images of coronal sections taken at 10X through the three brain regions are shown at five different ages. Sections were stained with antibodies specific for B cells, T cells, and neutrophils. No immunoreactivity is seen over that detected in the no-primary antibody control. Adult spleen is included as a positive control and, as expected, all three cell types are visible in spleen. (B) Spinal cord sections from mice subjected to experimental autoimmune encephalitis (EAE) are included as a second positive control for our ability to detect immune cell infiltration. All immune cell types are stained, at the expected low levels, in EAE spinal cord.
Research Highlight.
As in autism and schizophrenia, maternal immune activation leads to chronic, region-specific changes in brain and serum cytokines in offspring throughout development.
Acknowledgments
We are grateful for the advice of several immunologists at U.C. Davis in the experimental design and interpretation of this study, including Drs. Judy van de Water, Paul Ashwood, and Nicole Baumgarth. Myka Estes also helped in editing the manuscript. This work was supported by an ARRA grant from the National Institutes of Mental Health (NIMH) R01-MH088879 (AKM), an R01 from the National Eye Institute (NEI) R01-EY13584 (AKM), a supplement to support Paula Garay (R01-EY13584-S1; AKM), NIMH grant 5R01 MH079299 (K. Mirnics and PHP), an NRSA pre-doctoral fellowship from NIMH (EYH), and a Dennis Weatherstone fellowship from Autism Speaks (EYH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abazyan B, Nomura J, Kannan G, Ishizuka K, Tamashiro KL, Nucifora F, Pogorelov V, Ladenheim B, Yang C, Krasnova IN, Cadet JL, Pardo C, Mori S, Kamiya A, Vogel MW, Sawa A, Ross CA, Pletnikov MV. Prenatal interaction of mutant DISC1 and immune activation produces adult psychopathology. Biol Psychiatry. 2010;68:1172–1181. doi: 10.1016/j.biopsych.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrode-Bruses G, Bruses JL. Maternal immune activation by poly(I:C) induces expression of cytokines IL-1beta and IL-13, chemokine MCP-1 and colony stimulating factor VEGF in fetal mouse brain. J Neuroinflammation. 2012;9:83. doi: 10.1186/1742-2094-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashwood P, Krakowiak P, Hertz-Picciotto I, Hansen R, Pessah I, Van de Water J. Elevated plasma cytokines in autism spectrum disorders provide evidence of immune dysfunction and are associated with impaired behavioral outcome. Brain Behav Immun. 2011;25:40–45. doi: 10.1016/j.bbi.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashwood P, Krakowiak P, Hertz-Picciotto I, Hansen R, Pessah IN, Van de Water J. Associations of impaired behaviors with elevated plasma chemokines in autism spectrum disorders. J Neuroimmunol. 2011;232:196–199. doi: 10.1016/j.jneuroim.2010.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashwood P, Nguyen DV, Hessl D, Hagerman RJ, Tassone F. Plasma cytokine profiles in Fragile X subjects: is there a role for cytokines in the pathogenesis? Brain Behav Immun. 2010;24:898–902. doi: 10.1016/j.bbi.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atladottir HO, Thorsen P, Ostergaard L, Schendel DE, Lemcke S, Abdallah M, Parner ET. Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. J Autism Dev Disord. 2010;40:1423–1430. doi: 10.1007/s10803-010-1006-y. [DOI] [PubMed] [Google Scholar]
- Bauer S, Kerr BJ, Patterson PH. The neuropoietic cytokine family in development, plasticity, disease and injury. Nat Rev Neurosci. 2007;8:221–232. doi: 10.1038/nrn2054. [DOI] [PubMed] [Google Scholar]
- Bauman MD, Losif A-M, Smith S, Bregere M, Zadran S, Amaral DG, Patterson PH. A nonhuman primate model of maternal immune activation. Annual Society for Neuroscience Meeting Abs. 2011 in press. [Google Scholar]
- Brown AS. Epidemiologic studies of exposure to prenatal infection and risk of schizophrenia and autism. Dev Neurobiol. 2012 doi: 10.1002/dneu.22024. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown AS, Begg MD, Gravenstein S, Schaefer CA, Wyatt RJ, Bresnahan M, Babulas VP, Susser ES. Serologic evidence of prenatal influenza in the etiology of schizophrenia. Arch Gen Psychiatry. 2004;61:774–780. doi: 10.1001/archpsyc.61.8.774. [DOI] [PubMed] [Google Scholar]
- Brown AS, Derkits EJ. Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. The American journal of psychiatry. 2010;167:261–280. doi: 10.1176/appi.ajp.2009.09030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown AS, Patterson PH. Maternal infection and schizophrenia: implications for prevention. Schizophr Bull. 2011;37:284–290. doi: 10.1093/schbul/sbq146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Careaga M, Van de Water J, Ashwood P. Immune dysfunction in autism: a pathway to treatment. Neurotherapeutics. 2010;7:283–292. doi: 10.1016/j.nurt.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chez MG, Dowling T, Patel PB, Khanna P, Kominsky M. Elevation of tumor necrosis factor-alpha in cerebrospinal fluid of autistic children. Pediatr Neurol. 2007;36:361–365. doi: 10.1016/j.pediatrneurol.2007.01.012. [DOI] [PubMed] [Google Scholar]
- Clancy B, Finlay BL, Darlington RB, Anand KJ. Extrapolating brain development from experimental species to humans. Neurotoxicology. 2007;28:931–937. doi: 10.1016/j.neuro.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalgard CL, Cole JT, Kean WS, Lucky JJ, Sukumar G, McMullen DC, Pollard HB, Watson WD. The cytokine temporal profile in rat cortex after controlled cortical impact. Front Mol Neurosci. 2012;5:6. doi: 10.3389/fnmol.2012.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta SC, Opp MR. Lipopolysaccharide-induced increases in cytokines in discrete mouse brain regions are detectable using Luminex xMAP technology. J Neurosci Methods. 2008;175:119–124. doi: 10.1016/j.jneumeth.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David S, Kroner A. Repertoire of microglial and macrophage responses after spinal cord injury. Nat Rev Neurosci. 2011;12:388–399. doi: 10.1038/nrn3053. [DOI] [PubMed] [Google Scholar]
- Davis JO, Phelps JA, Bracha HS. Prenatal development of monozygotic twins and concordance for schizophrenia. Schizophr Bull. 1995;21:357–366. doi: 10.1093/schbul/21.3.357. [DOI] [PubMed] [Google Scholar]
- Deverman BE, Patterson PH. Cytokines and CNS development. Neuron. 2009;64:61–78. doi: 10.1016/j.neuron.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Erickson MA, Banks WA. Cytokine and chemokine responses in serum and brain after single and repeated injections of lipopolysaccharide: multiplex quantification with path analysis. Brain Behav Immun. 2011;25:1637–1648. doi: 10.1016/j.bbi.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatemi SH, Emamian ES, Sidwell RW, Kist DA, Stary JM, Earle JA, Thuras P. Human influenza viral infection in utero alters glial fibrillary acidic protein immunoreactivity in the developing brains of neonatal mice. Mol Psychiatry. 2002;7:633–640. doi: 10.1038/sj.mp.4001046. [DOI] [PubMed] [Google Scholar]
- Fatemi SH, Reutiman TJ, Folsom TD, Huang H, Oishi K, Mori S, Smee DF, Pearce DA, Winter C, Sohr R, Juckel G. Maternal infection leads to abnormal gene regulation and brain atrophy in mouse offspring: implications for genesis of neurodevelopmental disorders. Schizophr Res. 2008;99:56–70. doi: 10.1016/j.schres.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatemi SH, Sidwell R, Kist D, Akhter P, Meltzer HY, Bailey K, Thuras P, Sedgwick J. Differential expression of synaptosome-associated protein 25 kDa [SNAP-25] in hippocampi of neonatal mice following exposure to human influenza virus in utero. Brain Res. 1998;800:1–9. doi: 10.1016/s0006-8993(98)00450-8. [DOI] [PubMed] [Google Scholar]
- Feng JF, Van KC, Gurkoff GG, Kopriva C, Olszewski RT, Song M, Sun S, Xu M, Neale JH, Yuen PW, Lowe DA, Zhou J, Lyeth BG. Post-injury administration of NAAG peptidase inhibitor prodrug, PGI-02776, in experimental TBI. Brain Res. 2011;1395:62–73. doi: 10.1016/j.brainres.2011.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Focking M, Dicker P, English JA, Schubert KO, Dunn MJ, Cotter DR. Common proteomic changes in the hippocampus in schizophrenia and bipolar disorder and particular evidence for involvement of cornu ammonis regions 2 and 3. Arch Gen Psychiatry. 2011;68:477–488. doi: 10.1001/archgenpsychiatry.2011.43. [DOI] [PubMed] [Google Scholar]
- Fu Q, Zhu J, Van Eyk JE. Comparison of multiplex immunoassay platforms. Clin Chem. 2010;56:314–318. doi: 10.1373/clinchem.2009.135087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi R, Hayley S, Gibb J, Merali Z, Anisman H. Influence of poly I:C on sickness behaviors, plasma cytokines, corticosterone and central monoamine activity: moderation by social stressors. Brain Behav Immun. 2007;21:477–489. doi: 10.1016/j.bbi.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Garay PA, McAllister AK. Novel roles for immune molecules in neural development: implications for neurodevelopmental disorders. Frontiers in synaptic neuroscience. 2010;2, 136:1–16. doi: 10.3389/fnsyn.2010.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore JH, Jarskog LF, Vadlamudi S. Maternal poly I:C exposure during pregnancy regulates TNF alpha, BDNF, and NGF expression in neonatal brain and the maternal-fetal unit of the rat. J Neuroimmunol. 2005;159:106–112. doi: 10.1016/j.jneuroim.2004.10.008. [DOI] [PubMed] [Google Scholar]
- Gilmore JH, Jarskog LF, Vadlamudi S, Lauder JM. Prenatal infection and risk for schizophrenia: IL-1b, IL-6, and TNFa inhibit cortcial neuron dendrtie development. Neuropsychopharmacology. 2004;29:1221–1229. doi: 10.1038/sj.npp.1300446. [DOI] [PubMed] [Google Scholar]
- Goines PE, Croen LA, Braunschweig D, Yoshida CK, Grether J, Hansen R, Kharrazi M, Ashwood P, Van de Water J. Increased midgestational IFN-gamma, IL-4 and IL-5 in women bearing a child with autism: A case-control study. Mol Autism. 2011;2:13. doi: 10.1186/2040-2392-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagberg H, Gressens P, Mallard C. Inflammation during fetal and neonatal life: implications for neurologic and neuropsychiatric disease in children and adults. Annals of Neurology. 2012;71:444–457. doi: 10.1002/ana.22620. [DOI] [PubMed] [Google Scholar]
- Hallmayer J, Cleveland S, Torres A, Phillips J, Cohen B, Torigoe T, Miller J, Fedele A, Collins J, Smith K, Lotspeich L, Croen LA, Ozonoff S, Lajonchere C, Grether JK, Risch N. Genetic Heritability and Shared Environmental Factors Among Twin Pairs With Autism. Arch Gen Psychiatry. 2011:1095–1012. doi: 10.1001/archgenpsychiatry.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao EY, Patterson PH. Activation of the maternal immune system induces endocrine changes in the placenta via IL-6. Brain Behav Immun. 2011;25:604–615. doi: 10.1016/j.bbi.2010.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito HT, Smith SEP, Hsiao E, Patterson PH. Maternal immune activation alters nonspatial information processing in the hippocampus of adult offspring. Brain Behav Immun. 2010;24:930–941. doi: 10.1016/j.bbi.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji L, Chauhan V, Flory MJ, Chauhan A. Brain region-specific decrease in the activity and expression of protein kinase A in the frontal cortex of regressive autism. PLoS One. 2011;6:e23751. doi: 10.1371/journal.pone.0023751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EA, Kan RK. The acute phase response and soman-induced status epilepticus: temporal, regional and cellular changes in rat brain cytokine concentrations. J Neuroinflammation. 2010;7:40. doi: 10.1186/1742-2094-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juttler E, Tarabin V, Schwaninger M. Interleukin-6 (IL-6): a possible neuromodulator induced by neuronal activity. Neuroscientist. 2002;8:268–275. doi: 10.1177/1073858402008003012. [DOI] [PubMed] [Google Scholar]
- Kasten-Jolly J, Heo Y, Lawrence DA. Central nervous system cytokine gene expression: modulation by lead. J Biochem Mol Toxicol. 2011;25:41–54. doi: 10.1002/jbt.20358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koga K, Cardenas I, Aldo P, Abrahams VM, Peng B, Fill S, Romero R, Mor G. Activation of TLR3 in the trophoblast is associated with preterm delivery. Am J Reprod Immunol. 2009;61:196–212. doi: 10.1111/j.1600-0897.2008.00682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Blumberg SJ, Schieve LA, Boyle CA, Perrin JM, Ghandour RM, Singh GK, Strickland BB, Trevathan E, van Dyck PC. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009;124:1395–1403. doi: 10.1542/peds.2009-1522. [DOI] [PubMed] [Google Scholar]
- Kunz M, Cereser KM, Goi PD, Fries GR, Teixeira AL, Fernandes BS, Belmonte-de-Abreu PS, Kauer-Sant’anna M, Kapczinski F, Gama CS. Serum levels of IL-6, IL-10 and TNF-alpha in patients with bipolar disorder and schizophrenia: differences in pro- and anti-inflammatory balance. Rev Bras Psiquiatr. 2011;33:268–274. doi: 10.1590/s1516-44462011000300010. [DOI] [PubMed] [Google Scholar]
- Li X, Chauhan A, Sheikh AM, Patil S, Chauhan V, Li XM, Ji L, Brown T, Malik M. Elevated immune response in the brain of autistic patients. J Neuroimmunol. 2009;207:111–116. doi: 10.1016/j.jneuroim.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Cook EH, Leventhal BL, Amaral DG. Autism spectrum disorders. Neuron. 2000;28:355–363. doi: 10.1016/s0896-6273(00)00115-x. [DOI] [PubMed] [Google Scholar]
- Malkova NV, Yu CZ, Hsiao EY, Moore MJ, Patterson PH. Maternal immune activation yields offspring displaying mouse versions of the three core symptoms of autism. Brain Behav Immun. 2012;26:607–616. doi: 10.1016/j.bbi.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal M, Marzouk AC, Donnelly R, Ponzio NM. Maternal immune stimulation during pregnancy affects adaptive immunity in offspring to promote development of TH17 cells. Brain Behav Immun. 2011;25:863–871. doi: 10.1016/j.bbi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- McAfoose J, Baune BT. Evidence for a cytokine model of cognitive function. Neurosci Biobehav Rev. 2009;33:355–366. doi: 10.1016/j.neubiorev.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Meyer U, Feldon J. Epidemiology-driven neurodevelopmental animal models of schizophrenia. Prog Neurobiol. 2010;90:285–326. doi: 10.1016/j.pneurobio.2009.10.018. [DOI] [PubMed] [Google Scholar]
- Meyer U, Feldon J, Dammann O. Schizophrenia and autism: both shared and disorder-specific pathogenesis via perinatal inflammation? Pediatr Res. 2011;69:26R–33R. doi: 10.1203/PDR.0b013e318212c196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer U, Feldon J, Fatemi SH. In-vivo rodent models for the experimental investigation of prenatal immune activation effects in neurodevelopmental brain disorders. Neurosci Biobehav Rev. 2009;33:1061–1079. doi: 10.1016/j.neubiorev.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Meyer U, Feldon J, Schedlowski M, Yee BK. Immunological stress at the maternal-foetal interface: a link between neurodevelopment and adult psychopathology. Brain Behav Immun. 2006a;20:378–388. doi: 10.1016/j.bbi.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Meyer U, Knuesel I, Nyffeler M, Feldon J. Chronic clozapine treatment improves prenatal infection-induced working memory deficits without influencing adult hippocampal neurogenesis. Psychopharmacology (Berl) 2010;208:531–543. doi: 10.1007/s00213-009-1754-6. [DOI] [PubMed] [Google Scholar]
- Meyer U, Nyffeler M, Engler A, Urwyler A, Schedlowski M, Knuesel I, Yee BK, Feldon J. The time of prenatal immune challenge determines the specificity of inflammation-mediated brain and behavioral pathology. J Neurosci. 2006b;26:4752–4762. doi: 10.1523/JNEUROSCI.0099-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer U, Nyffeler M, Schwendener S, Knuesel I, Yee BK, Feldon J. Relative prenatal and postnatal maternal contributions to schizophrenia-related neurochemical dysfunction after in utero immune challenge. Neuropsychopharmacology. 2008;33:441–456. doi: 10.1038/sj.npp.1301413. [DOI] [PubMed] [Google Scholar]
- Meyer U, Schwendener S, Feldon J, Yee BK. Prenatal and postnatal maternal contributions in the infection model of schizophrenia. Exp Brain Res. 2006c;173:243–257. doi: 10.1007/s00221-006-0419-5. [DOI] [PubMed] [Google Scholar]
- Molloy CA, Morrow AL, Meinzen-Derr J, Schleifer K, Dienger K, Manning-Courtney P, Altaye M, Wills-Karp M. Elevated cytokine levels in children with autism spectrum disorder. J Neuroimmunol. 2006;172:198–205. doi: 10.1016/j.jneuroim.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Mukherjee S, Katki K, Arisi GM, Foresti ML, Shapiro LA. Early TBI-Induced Cytokine Alterations are Similarly Detected by Two Distinct Methods of Multiplex Assay. Front Mol Neurosci. 2011;4:21. doi: 10.3389/fnmol.2011.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawa H, Takahashi M, Patterson PH. Cytokine and growth factor involvement in schizophrenia--support for the developmental model. Mol Psychiatry. 2000;5:594–603. doi: 10.1038/sj.mp.4000730. [DOI] [PubMed] [Google Scholar]
- Pardo CA, Vargas DL, Zimmerman AW. Immunity, neuroglia and neuroinflammation in autism. Int Rev Psychiatry. 2005;17:485–495. doi: 10.1080/02646830500381930. [DOI] [PubMed] [Google Scholar]
- Patterson PH. Neuroscience. Maternal effects on schizophrenia risk. Science. 2007;318:576–577. doi: 10.1126/science.1150196. [DOI] [PubMed] [Google Scholar]
- Patterson PH. Immune involvement in schizophrenia and autism: etiology, pathology and animal models. Behav Brain Res. 2009;204:313–321. doi: 10.1016/j.bbr.2008.12.016. [DOI] [PubMed] [Google Scholar]
- Patterson PH. Maternal infection and immune involvement in autism. Trends Mol Med. 2011a;17:389–394. doi: 10.1016/j.molmed.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson PH. Modeling autistic features in animals. Pediatr Res. 2011b;69:34R–40R. doi: 10.1203/PDR.0b013e318212b80f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piontkewitz Y, Assaf Y, Weiner I. Clozapine administration in adolescence prevents postpubertal emergence of brain structural pathology in an animal model of schizophrenia. Biol Psychiatry. 2009;66:1038–1046. doi: 10.1016/j.biopsych.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Ransohoff RM, Perry VH. Microglial physiology: unique stimuli, specialized responses. Annu Rev Immunol. 2009;27:119–145. doi: 10.1146/annurev.immunol.021908.132528. [DOI] [PubMed] [Google Scholar]
- Rapoport J, Chavez A, Greenstein D, Addington A, Gogtay N. Autism spectrum disorders and childhood-onset schizophrenia: clinical and biological contributions to a relation revisited. J Am Acad Child Adolesc Psychiatry. 2009;48:10–18. doi: 10.1097/CHI.0b013e31818b1c63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg RE, Law JK, Yenokyan G, McGready J, Kaufmann WE, Law PA. Characteristics and concordance of autism spectrum disorders among 277 twin pairs. Arch Pediatr Adolesc Med. 2009;163:907–914. doi: 10.1001/archpediatrics.2009.98. [DOI] [PubMed] [Google Scholar]
- Shi L, Fatemi SH, Sidwell RW, Patterson PH. Maternal influenza infection causes marked behavioral and pharmacological changes in the offspring. J Neurosci. 2003;23:297–302. doi: 10.1523/JNEUROSCI.23-01-00297.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Smith SE, Malkova N, Tse D, Su Y, Patterson PH. Activation of the maternal immune system alters cerebellar development in the offspring. Brain Behav Immun. 2009;23:116–123. doi: 10.1016/j.bbi.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Tu N, Patterson PH. Maternal influenza infection is likely to alter fetal brain development indirectly: the virus is not detected in the fetus. Int J Dev Neurosci. 2005;23:299–305. doi: 10.1016/j.ijdevneu.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Short SJ, Lubach GR, Karasin AI, Olsen CW, Styner M, Knickmeyer RC, Gilmore JH, Coe CL. Maternal influenza infection during pregnancy impacts postnatal brain development in the rhesus monkey. Biol Psychiatry. 2010;67:965–973. doi: 10.1016/j.biopsych.2009.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SE, Li J, Garbett K, Mirnics K, Patterson PH. Maternal immune activation alters fetal brain development through interleukin-6. J Neurosci. 2007;27:10695–10702. doi: 10.1523/JNEUROSCI.2178-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellwagen D. The contribution of TNFalpha to synaptic plasticity and nervous system function. Adv Exp Med Biol. 2011;691:541–557. doi: 10.1007/978-1-4419-6612-4_57. [DOI] [PubMed] [Google Scholar]
- Suda S, Iwata K, Shimmura C, Kameno Y, Anitha A, Thanseem I, Nakamura K, Matsuzaki H, Tsuchiya KJ, Sugihara G, Iwata Y, Suzuki K, Koizumi K, Higashida H, Takei N, Mori N. Decreased expression of axon-guidance receptors in the anterior cingulate cortex in autism. Mol Autism. 2011;2:14. doi: 10.1186/2040-2392-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szatmari P. Is Autism, at Least in Part, a Disorder of Fetal Programming? Arch Gen Psychiatry. 2011;68:1091–1092. doi: 10.1001/archgenpsychiatry.2011.99. [DOI] [PubMed] [Google Scholar]
- Toyooka K, Watanabe Y, Iritani S, Shimizu E, Iyo M, Nakamura R, Asama K, Makifuchi T, Kakita A, Takahashi H, Someya T, Nawa H. A decrease in interleukin-1 receptor antagonist expression in the prefrontal cortex of schizophrenic patients. Neurosci Res. 2003;46:299–307. doi: 10.1016/s0168-0102(03)00093-2. [DOI] [PubMed] [Google Scholar]
- Traynor TR, Majde JA, Bohnet SG, Krueger JM. Intratracheal double-stranded RNA plus interferon-gamma: a model for analysis of the acute phase response to respiratory viral infections. Life Sci. 2004;74:2563–2576. doi: 10.1016/j.lfs.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol. 2005;57:67–81. doi: 10.1002/ana.20315. [DOI] [PubMed] [Google Scholar]
- Weiner I. The “two-headed” latent inhibition model of schizophrenia: modeling positive and negative symptoms and their treatment. Psychopharmacology (Berl) 2003;169:257–297. doi: 10.1007/s00213-002-1313-x. [DOI] [PubMed] [Google Scholar]
- Yao JK, Sistilli CG, van Kammen DP. Membrane polyunsaturated fatty acids and CSF cytokines in patients with schizophrenia. Prostaglandins, leukotrienes, and essential fatty acids. 2003;69:429–436. doi: 10.1016/j.plefa.2003.08.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Average concentrations (pg/ml for brain regions and pg/ml for serum) ± SEM for 23 cytokines are shown for saline (control) and poly(I:C) (MIA) conditions for each brain region at each age. The fold-change in cytokines resulting from MIA was calculated as the ratio of the average values for poly(I:C)/saline (P/S). P-values for t-tests between MIA and controls for each comparison are also indicated. Grey fills indicate cytokines that are significantly different between MIA and control values (p<0.05). ND = not detected.
Average concentrations (pg/ml for brain regions and pg/ml for serum) ± SEM for 23 cytokines are shown for saline (control) and poly(I:C) (MIA) conditions for HC and serum at each age. The fold-change in cytokines resulting from MIA was calculated as the ratio of the average values for poly(I:C)/saline (P/S). P-values for t-tests between MIA and controls for each comparison are also indicated. Grey fills indicate cytokines that are significantly different between MIA and control values (p<0.05). ND = not detected.
Representative brains from control and MIA offspring are shown for each of the four ages examined, following Evans Blue staining to detect BBB permeability. There is no qualitative difference in BBB permeability in MIA brains compared to controls at any age examined.
(A) Representative images of coronal sections taken at 10X through the three brain regions are shown at five different ages. Sections were stained with antibodies specific for B cells, T cells, and neutrophils. No immunoreactivity is seen over that detected in the no-primary antibody control. Adult spleen is included as a positive control and, as expected, all three cell types are visible in spleen. (B) Spinal cord sections from mice subjected to experimental autoimmune encephalitis (EAE) are included as a second positive control for our ability to detect immune cell infiltration. All immune cell types are stained, at the expected low levels, in EAE spinal cord.