Synopsis
This article uses the Disablement Model conceptual framework to guide an analysis of the importance of OA in the development of disability. The Disablement Model describes the development and progression of disablement from impairments to specific functional limitations and disability, and the hypothesized role of predisposing risk factors, extra-individual factors, and intra-individual factors. A wide range of population and clinical studies have characterized the unequivocal contribution of arthritis to the development of functional limitations and disability. Evidence overwhelmingly supports a significant, moderate independent contribution of arthritis to the onset and progression of functional limitations and disability. With respect to important risk factors for the development of functional limitations and disability among those with OA, the evidence provides strong support for the role of physical impairments along with other predisposing and intra-individual factors such as age; body mass index, obesity, lack of exercise, comorbid conditions, depression; and depressive symptoms. Extra-individual factors included need for aids and assistance, and lack of access to public or private transportation. Future disablement research must clarify the causal mechanisms behind a potential risk factor’s impact on disability and delineate the interplay between and among the various hypothesized steps in the disablement process.
Keywords: osteoarthritis, arthritis, function, disability, activity, participation, disablement
Introduction
It is widely stated that arthritis is the leading cause of disability among adults.[1-9] Indeed, there is no question that osteoarthritis (OA) in particular is related to disability as adults age. The risk of OA increases with age, so that by the age of 80 radiographic evidence of joint degeneration is found in nearly everyone. [10] However, there is much that remains unknown about the specific contributions of osteoarthritis and intervening variables to the development of disability. Ferrucci et al. revealed that as people age, a larger proportion of disability occurs along a slower, progressive course as compared to more rapid onset, “catastrophic disability.” [11] Research supports the characterization of OA as one example of a condition that is characterized by the slow progression of disability. [12-15]
OA pathology results in the degeneration of cartilage, bone and soft tissues integral to joints; most commonly the hand, knee, hip, spine and foot. Discordance between OA pathology and resultant disability highlight opportunities to identify modifiable factors in the pathway from pathology to disability. While OA is associated with joint-related symptoms such as pain and stiffness, there is wide variation in symptoms for those with radiographic evidence of joint degeneration changes, and many with radiographic changes report no pain.[16]
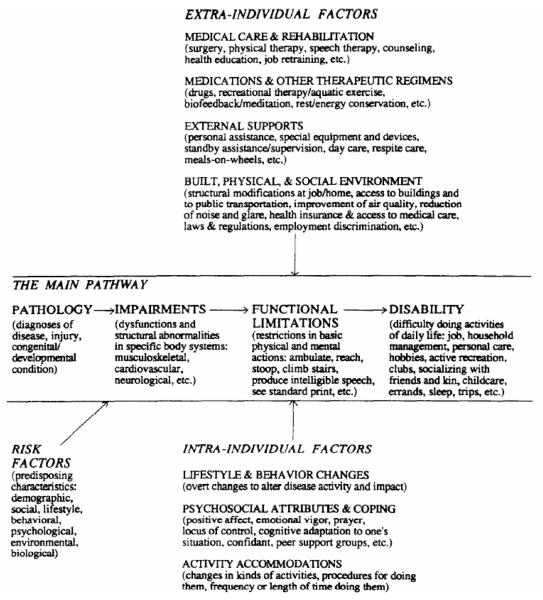
Studies of OA and disability use a range of definitions for OA and for disability, and this presents challenges to summarizing and interpreting the literature. Often, diagnosis of OA is made based on both radiographic signs and joint symptoms; however, and the former is considered to be associated with later stages of disease. In prior work, investigators have highlighted the importance of a disablement conceptual framework to guide the investigation of disability and its determinants.[17] Therefore, to guide this analysis of the importance of OA in the development of disability, we will use the Disablement Model developed by Verbrugge and Jette based on the seminal work by Nagi.[18-20] The Disablement Model (figure 1) presents the main pathway for the development of disability with factors affecting progression including risk factors, extra-individual factors, and intra-individual factors. Since the pathway represents a continuum from cellular to societal level effects, the threshold for transition from one element to another is debatable. We review the pathway below, and relate elements of OA to the levels of the pathway to facilitate our review and discussion.
Figure 1.
Verbrugge and Jette’s Disablement Model
From Verbrugge LM, Jette AM. The Disablement Process. Social Science and Medicine. 1994;38(1):Figure 2: Page 4.
The Main Pathway
The main disablement pathway progresses from pathology to impairments, to functional limitations, and finally to disability.
“Pathology refers to biochemical or physiological abnormalities that are detected and labeled as disease, injury, or congenital/developmental conditions.”[20] OA pathology would include biological and physiological changes to the hyaline cartilage and neighboring bone, synovial fluid and soft tissue, ligaments and muscle. The development of sclerotic changes in subchondral bone tissue, osteophyte growth and synovial tissue proliferation are examples of pathology in OA.
“Impairments are dysfunctions and significant structural abnormalities” that occur at the level of the body systems or organs, and are “the functional consequence of pathology.”[20] Abnormalities related to OA that reach the level of impairment may include joint swelling, deformity or malalignment, decreased strength, limitations in range of motion, and abnormalities of gait, and symptoms such as pain and stiffness.
Functional limitations occur at the level of the person and represent limitations in executing specific mental or physical actions or tasks. Examples of functional limitations include restrictions in walking, picking up items from the floor, and climbing stairs.
Disability is defined as limitations, difficulty, or inability to do more complex behaviors or activities that are performed within a social, cultural, or physical context. Disability behaviors reflect what a person does in daily life and range from activities of daily living such as dressing, doing household chores and errands, to fulfilling social roles in such contexts of work, community, and family.
The Disablement Model includes outcomes beyond disability such as hospitalization, inability to live alone, and death, and pathways from disability to functional limitations, impairments and pathology as well. These are important considerations for researchers undertaking to investigate the causal mechanisms involved in the process.
The Factors
In order to facilitate understanding and investigation of the causal mechanisms in the progression from one stage of disablement to another, the Disablement Model identifies several categories of intervening factors: predisposing risk factors, intra-individual intervening factors, and extra individual intervening factors.
Predisposing Risk factors are pre-existing characteristics of the individual that can affect the presence of impairment, functional limitation, and disability, and its severity. These characteristics range from sociodemographic, lifestyle, psychological, and biological factors and exist before the onset of the disablement process.
Intra-individual intervening factors aim to impact the disease and its repercussions on degree of impairment, functional limitation, and disability, and include the following categories: lifestyle and behavior changes; psychosocial attributes and coping mechanisms; and individual accommodations to activity (changing the length of time spent doing an activity or the types of activities done).
Extra-individual intervening factors include “medical care and rehabilitation, medications & other therapeutic regimens, external supports, and built, physical, and social environment” factors.[20] The terms buffers and exacerbators are used to describe the potential positive or negative impacts of the existing environment or active interventions.
In arthritis research, “disability outcomes” may include variables ranging from the level of impairment (symptoms, weakness and malalignment) to that of disability (difficulty doing activities at the intersection of person and environment). Similarly, “OA” may be defined as joint pain, or joint pain associated with radiographic changes. It should be noted that arthritis as defined in large national studies often includes other conditions such as rheumatoid arthritis, spinal disorders, and arthropathies. This presents challenges for interpreting the literature as it relates to osteoarthritis. However, for the large majority of the persons in the larger “arthritis” category, the form of arthritis that they experience is osteoarthritis. We provide an example of the prevalence estimates from one national study to illustrate. Verbrugge et al. estimated that 43.7% of the US population has arthritis, and further stratified prevalence rates as follows: 34.8% of males over 55 have arthritis, and 32.7 % have osteoarthritis. Similarly the prevalence rates for females over the age of 55 were 50.6% for arthritis and 47.1 % for osteoarthritis. [21] Therefore, we have included relevant studies utilizing the broader definition of arthritis in our review when we found that they provided important information about the relationship between arthritis and functional limitations and disability that may guide future work specific to osteoarthritis. We use the term osteoarthritis or OA to represent the more specific diagnosis when appropriate, and use the term arthritis to denote the larger category that includes conditions other than osteoarthritis. We focus on the two elements to the right in the main pathway because together they represent what is meant by many when they refer to “disability.” In doing so, we will address risk factors, intra-individual factors, and extra--individual factors that impact the relationship between these elements. We will highlight gaps in knowledge, and propose directions for future inquiry.
The Contribution of Arthritis to Functional Limitations and Disability
Many cross-sectional studies have demonstrated a substantial relationship between arthritis and functional limitations and disability, a selection of which are highlighted here. Fewer studies address the contribution of osteoarthritis to disability.
Research indicates that the impact of arthritis on disability is greater on physical functional limitations than on more complex social and role activities. [22] Verbrugge et al. compared levels of functional limitation and disability for those with and without arthritis in a nationally representative sample living in the United States using data from the Supplement on Aging of the 1984 National Health Interview Survey. [21] This study investigated the relationship between over 20 indicators of functional limitation and disability including walking, “motions and strength” (e.g. reaching, lifting, standing), personal care and household activities among those with a range of arthritic conditions. Across all of these measures members of this sample with arthritis experienced more disability than those who did not, and that the impact of arthritis was greater on functional limitations than on disability, represented by more complex social role activities. Comparing the impact of various health conditions, Results from the Women’s Health and Aging Study also have revealed that women reporting “a physician with a diagnosis of arthritis” were significantly more likely to report difficulty in 13 of 15 functional tasks and activities.[23]
Employing the World Health Organization’s Disability Assessment Schedule, and the National Comorbidity Survey Replication, Merikangas et al. used regression analysis to estimate the effect of specific conditions on disability days. Arthritis more generally accounted for the third largest number of disability days (374.6 million days per year), following back/neck pain (1167.8 million days per year) and major depressive disorder (386.6 million days per year). [24]
Verbrugge et al. provided detail to the emerging picture of the contribution of arthritis to functional limitations and disability by analyzing the 1994-95 National Health Interview’s Disability Supplement Phase I.[25] In this “profile of arthritis disability,” arthritis (including osteo, rheumatoid, spinal, and other arthropathies). Those with arthritis had a slower progression of milder disabilities than persons with disabilities from other conditions. This “profile of arthritis disability” is consistent with Ferrucci et al.’s concept of “progressive disability” characterized by a slower, more progressive course as compared to more rapid onset seen in “catastrophic disability.
A second profile of arthritis disability used the National Health Interview’s Disability Supplement Phase II to compare a range of functional limitations and disability for persons who attributed their disability to arthritis (including osteo, rheumatoid, spinal, and other arthropathies) against those with disability attributed to other conditions.[9] They reported that those with arthritis were more likely to be older, and female, and to be less likely to be working than those with other disabling conditions, and to report that they are unable to work due to their health. Overall, ”arthritis-disabled“ persons experienced more disability across a wider range of activities than ”other-disabled“ persons. In regard to participation in social activities, arthritis-disabled persons reported traveling long distances less often, using a vehicle for transportation less often, going out fewer days per week, and were less likely to report working at a job. This study provided new knowledge about the functional course for those with arthritis in middle age, and revealed that they experienced functional limitations and disability earlier than those without arthritis.
In longitudinal research, Song et al. estimated the population impact of arthritis using data from the nationally representative National Health and Retirement Survey.[8] Arthritis was identified when respondents answered yes to the question, ”Have you ever had or has a doctor ever told you that you have arthritis or rheumatism?“ Investigators used multiple logistic regression analysis to compare the incidence of new functional limitation or disability (preparing meals, grocery shopping, managing money, taking medications, using the telephone). Consistent with prior studies, investigators noted that risk factors for incident disability among persons 65 years and older were: demographic factors, age, comorbid conditions, physical limitations, health behaviors (tobacco and alcohol use, and physical activity), and socioeconomic factors, and they adjusted for them in the analysis. Song et al. conclude from their findings, ”Almost 1 in every 4 new cases of ADL disability was due to arthritis (adjusted population attributable fraction 23.7%).“[8] In is editorial comment, Covinsky wrote, ”Although Song et al. demonstrated that in a statistical sense almost 25% of disability is attributable to arthritis, it would not be correct to claim that arthritis is the cause of disability in 1 of 4 individuals with ADL dependence. In contrast, a conclusion stating that arthritis is the contributing cause in 75% of patients with ADL disability, and on average accounts for one-third of the disability is clinically very plausible.“[1]
A recent longitudinal study with 10 year follow-up from the Health and Retirement Study addressed the need to investigate the role of arthritis (as defined by the response to the same general arthritis question used in Song et al. above) earlier in life in the later development of functional limitations (walking and climbing stairs) or disability (bathing, dressing, transfers, eating and toileting). [2] The baseline results indicated that those with arthritis were significantly more likely to be older, female, of lower socioeconomic status, and have comorbid conditions (e.g. hypertension, depressive symptoms, cancer, or diabetes). After adjusting for age, sex, socioeconomic status, comorbid conditions, body mass index, smoking, depression, physical activity, difficulty jogging one mile, and difficulty climbing stairs, investigators found that those with arthritis demonstrated significantly higher risk of developing functional limitations (30% vs 16%) or difficulty with ADL function (13% vs 5% ) over 10 years. The adjusted odds ratio for ”mobility or ADL difficulty“ for those with arthritis compared to those without arthritis was 1.63 (1.43-1.86). Investigators also calculated odds ratios for those with arthritis only and those without arthritis and at least one other condition compared to those with no arthritis or other conditions. The adjusted odds ratios for those with arthritis and those with at least one other condition were 1.91(1.59-2.44) and 1.74 (1.46-2.08) respectively. This study provided new knowledge about the course of functional limitations and disability over a long period in those who experience arthritis in middle age.
The Contribution of Osteoarthritis to Functional Limitations and Disability
Guccione et al. used logistic regression to estimate the odds of dependence in 7 functional tasks and activities. [26] They found that knee OA was among the most disabling conditions, and was associated with the most limitation in walking and climbing stairs. The adjusted percentage of disability attributable to OA was approximately 16%, and equal to or higher than nine other major conditions in four out of the seven functional items (walking, carrying, climbing stairs, and housekeeping).
One approach to estimating the overall burden of conditions on disability used by the World Health organization is the Disability Adjusted Life Year (DALY). DALYs take into account the length of life and time spent with disability, by estimating the duration of healthy life lost due to a condition. Using data from 1990, and projecting the impact of OA in 2000, Reginster and Khaltaev reported that OA had the fourth greatest impact on disability, following ischaemic heart disease, cerebrovascular disease, and all musculoskeletal disease. [27]
Using data from a nationwide survey in France, and Fautrel et al. used reported limitation rates to calculate standardized limitation rate ratios (SLRRs) for those with OA compared to age and sex-matched controls. [28] They found that persons with OA reported limitations in mobility 4.5 to 6 times more frequently than those without. Among those with OA, 61% reported limitation in mobility outside the home compared to 10.2 % reported by controls. Inside the home, 12.8% of those with OA reported mobility limitations compared to 2.8% of controls. Similar patterns with smaller differences were observed for activities of daily living such as shopping and housecleaning. SLRRs ranged from 1.6 for dressing and sports to 6.0 for mobility outside the home.
Zhang et al found persons with hand OA experienced significant functional limitations in functions involving the hands compared to those who did not have hand OA, including writing, gripping, and manipulating small objects.[29]
In summary, a range of approaches has been used to characterize the unequivocal contribution of the presence of arthritis generally and OA in particular, to the development of functional limitations and disability. Evidence overwhelmingly supports a significant, moderate independent contribution of arthritis to the onset and progression of functional limitations and disability. We now consider a range of important risk and intervening factors that have been shown to mediate the impact of arthritis to a greater or lesser degree on loss of function and the development of disability.
Factors Influencing the Course of Disablement
Overview of Factors
In their paper summarizing a 1999 NIH Scientific Conference, Felson et al. highlighted the differences in risk factors for OA pathology and the development of functional limitations and disability succinctly: ”Whereas osteoarthritis is associated with increasing age, obesity, injury, previous deformity, and ligamentous laxity, the broader clinical problem, of musculoskeletal pain and disability is predicted by increasing age; osteoarthritis; obesity; lack of exercise; low personal self-efficacy; comorbid conditions caused by smoking, alcohol, and other risk factors; depression; low educational level; and poor socioeconomic status.“ [5] Indeed, a more recent review identifies structural manifestations of pathology and symptoms (e.g. knee joint laxity, decreased muscle strength, decreased range of motion); visual and cognitive deficits; comorbidity; overweight; psychological and social factors including anxiety, depression, fatigue, poor self-efficacy, and social support; health behaviors and sociodemographic factors as predictive factors.[30] This report is consistent with prior work except that van Dijk et al. note that increased level of aerobic exercise is a protective factor.[15] We review selected individual studies that support these findings below, and focus more on modifiable factors.
Predisposing and Intra-individual Risk Factors
Dunlop et al. used longitudinal data from a national probability sample and multiple logistic regression to investigate risk factors for functional decline. [31] Functional decline was associated with female gender and race for those with arthritis. Additional risk factors included age, cognitive and visual impairment, symptoms of depression, stroke, and physical limitations. The chief finding was that lack of regular vigorous exercise could predict an important increased risk of decline. [31]
Impairment-level Factors
In cross-sectional analysis of data from a community sample Wilkie et al. used logistic regression to investigate the association between a range of risk factors and disability. Their findings indicated that self-reported joint-level impairment was associated with both functional limitations and disability, and that a stronger association existed between functional limitations and disability than between impairment and disability. [32] Other cross-sectional analyses support the relationship between knee pain and functional limitations. [33-35]
Sharma et al. used multiple measures of physical function and logistic regression to investigate factors predictive of functional decline over 3 years in this study of community-dwelling adults with knee osteoarthritis. [14] They found that baseline knee laxity, knee pain intensity, and baseline to 18-month increase in knee pain increased risk of functional decline as measured by the Western Ontario McMaster University Osteoarthritis Index. Impaired position sense was associated with decline in the ability to perform sit-to-stand from a chair. In other studies, baseline pain and increase in pain predicted functional limitations. [12, 36] In their recent longitudinal study of adults with hip and knee OA, van Dijk et al found little overall change in physical function, but important variation at the individual level. Factors predictive of decline included decrements of strength and range of motion, and increased pain.
Ling et al found that knee extensor strength was predictive of transition to new functional limitations in a longitudinal cohort of women using data from the Women’s Health and Aging Study.[7] Miller et al. used mixed effects repeated measures analysis of covariance to investigate the relationship between baseline radiographic evidence of OA, knee strength, and knee pain, and functional outcomes (ambulation test, transfer test, and self-report of physical function.[37] They reported that while initially, baseline radiographic evidence of OA was associated with decline in all measures of physical function; this relationship was not significant when baseline levels of knee pain and knee strength were included in the model. This study could not address the temporal pattern of these three impairment level factors. Jinks et al found that in spite of resolved knee pain at 3 year follow-up, physical function had made minimal improvement [38]
Research into the relationship between joint pain, depression and physical function illustrates the opportunities for improved understanding of the relative contribution to functional limitations and disability and timing of its effects. Machado et al reported that the relationship between baseline pain and downstream disability was mediated by depressive symptoms.[39] They demonstrated that physical symptoms impact higher level disability through lower level physical functional limitations and depressive symptoms.
In summary, with respect to important risk factors for the development of functional limitations and disability among those with OA, the evidence provides strong support for the role of physical impairments in the development of functional limitations and disability. Impairments noted include those associated with age, and those specific to OA pathology. More work has been done in knee OA, where increased pain, decreased range of motion, joint laxity, and decreased position sense have been identified as significant predictors.
Comorbidity
Verbrugge et al. and Merikangas et al found that the impact of arthritis on functional limitations and disability was strongly increased in those who had other chronic conditions.[21] Merikangas et al. found that coefficients for regression models adjusting for comorbidity were decreased by one half. [24] Song et al also estimated that 20% of the excess risk for new disability in performing activities of daily living related to arthritis could be attributed to the presence of comorbid conditions, and Ayis et al. estimated an odds ratio of 3.6 for those with 3 or more comorbidites in their study of adults with lower extremity pain.[40] Further studies support the important role of comorbidities in the development and progression of disability. [2, 12, 13, 15, 41]
Since OA is strongly associated with age, many with OA have comorbidities, and therefore understanding the specific contribution of arthritis, comorbidities, and related modifiable factors offers important opportunities to intervene. In particular, based on the evidence to date, interventions to decrease the risk of development of for example, cardiac disease, obesity, depression, and stroke, would have more than an additive effect on future disability.
Obesity
Among others, several studies reviewed here have demonstrated that overweight and obesity is not only a risk factor for OA, but it has both direct and indirect effects on the progression of functional limitations and disability. [7, 8, 15, 22, 34, 41] Mallen et al. conducted a study to determine prognostic factors for functional limitations and disability for persons with knee pain and OA. One of the four ”generic indicators“ identified was body mass index (BMI). [12] OA Studies such as those described below have begun to investigate the relationships among other factors, OA, disability and obesity.
Self Efficacy
Self-efficacy has been identified as a factor mediating the relationship between knee pain, OA and functional decline. In a longitudinal study of older adults with knee pain, low self-efficacy was a significant predictor of decline in stair climbing and self-reported physical function and disability (e.g. taking care of a family member and shopping) for those with low baseline knee strength.[42] Other studies have demonstrated the predictive nature of self-efficacy among adults with knee OA[14] and adults with knee OA and obesity.[43] Pells et al provided further evidence for the role of self-efficacy among overweight and obese adults with knee OA, and found that the role of self-efficacy depends on the specific aspect of OA examined. For example, self-efficacy for physical function was more strongly related to disability, and self-efficacy for pain was strongly related to reports of pain. Additional analyses were conducted to examine the relationship between self-efficacy for restraint in eating and actual restraint. This relationship was stronger than those for domain-specific self-efficacy related to pain and function.[44] Using structural equation modeling, investigators have identified an additional variable, resilience, which has an indirect effect on pain, through self-efficacy. [45]
Psychosocial Factors
The impact of psychological and social factors has been studied more extensively for knee OA than for OA involving other joints. However, as discussed above, in a model developed to identify prognostic indicators for functional outcome among those with knee pain and OA, anxiety was one of the four indicators.[12] Machado, reporting on results of 18 month follow-up with adults with physician-diagnosed OA found that depressive symptoms mediated the relationship between symptoms and functional limitations and disability. [39] Lamb et al. investigated the relationship between knee pain and walking speed and ability to rise form a chair among participants in the Women’s Health & Aging study with knee pain. In this cross-sectional study they found that depression modified the relationship between knee pain and functional mobility. [34]
Larger studies using the broader definition of arthritis concur with studies focused on OA. Song et al. found that depressive symptoms were significantly associated with functional limitations and disability in their longitudinal study of older adults with arthritis.[8] Additional studies have demonstrated that depression exerts an important influence on disability in large national studies of those with arthritis.[24, 31]
Parmelee et al. investigated the relationship between depression, pain, functional limitation, and disability, modeling depressive symptoms as the outcome in a sample of persons with knee OA. [46] Using linear and ordinary least squares regression analysis to develop path models of the associations between the variables, authors reported that pain was the main driver of the relationship between functional limitations and depressive symptoms. However, this was not the case for the relationships among pain, depressive symptoms and disability, where both pain and disability predicted depressive symptoms. [46] This study provided evidence that participation in desired activities is associated with decreased depressive symptoms.
Level of Exercise
Recent studies have found that exercise level is associated with functional limitations and disability, with aerobic and vigorous exercise providing a protective effect. [8, 14, 15, 31]
Extra-individual Risk Factors
Two studies by Verbrugge et al addressed factors impacting the development of functional limitation or disability for those with arthritis using the National Health Interview Survey Disability Supplement, and were discussed briefly above in relation to other factors. The results of the first study indicated that persons with arthritis use more mobility aids, and fewer accommodations and assistance. [25] Building on earlier work, Verbrugge et al explored buffers and barriers in a comparison of those with and without arthritis using the Phase II of the Disability Supplement and compared persons with disabilities primarily due to arthritis and those with disabilities primarily due to other conditions.[9] Arthritis-disabled persons reported more functional limitations, more buffers (medical devices and services, assistive equipment and accommodations), and more barriers to getting around within and outside the home. Similar results were reported in a comparison of arthritis disability to heart disease disability using the same data source.[47] In addition, Wilkie et al demonstrated that environmental factors such as need of aids and assistance, limited access to public transportation, and limited access to car were predictive of disability. [33]
Knowledge Gaps and Future Directions
One of the major limitations of the many studies of OA and its impact on disablement is the inclusion of risk factors cross-sectionally at baseline and the adjustment for these factors in analytic model. Most previous disablement research relies on single-equation systems in which hypothesized causes of disability are simultaneously entered into the analysis model to determine their effects on disability. While this approach addresses the question of impact or association of the pathology of OA and its relationship with subsequent functional limitations or disability outcomes, it has limited ability to elucidate the specific roles of the range of relevant risk or intervening factors that affect the progression of the disablement process across the continuum from pathology to disability, beyond and back through feedback loops. Future disablement research must clarify the causal mechanisms behind a potential risk factor’s impact on disability and delineate the interplay between and among the various hypothesized steps in the disablement process. In other words, to know the extent to which OA is associated with functional loss and disability is important; to understand the critical factors that mediate these associations is crucial if we are to design evidence based interventions aimed at retarding or preventing the disablement process for those with OA.
Lawrence and Jette provide an example of one alternative analytic approach in their investigation of the relationship between risk factors, impairments, functional limitations and disability using data from a cohort of older adults. They used the Disablement Model as the conceptual model for the causal mechanisms involved, and structural equation modeling to test the hypotheses generated by the model. Their modeling underscored the important intervening role of lower extremity function in protecting against the subsequent onset of disability and also revealed the significant buffering role played by level of physical activity in the onset of future functional limitations and disability. Machado et al. also applied a hypothesized model of the relationship between impairment (symptom severity), and disability divided into activity limitations and participation restrictions specific to OA. [39] They utilized exploratory factor analysis to test their hypothesis that physical symptoms impact higher level disability through lower level physical functional limitations and depressive symptoms. Results supported this hypothesis, indicating that symptom severity causes limitations in specific functional tasks and depressive symptoms, and that persons with these limitations in turn limit their participation in social roles and activities. The authors posited that the subsequent limitations could be due to the fact that social roles and activities actually include these specific physical functions within their larger, more complex activities and that the depressive symptoms in turn cause limitations in the ability or desire to take part in social roles and activities. In providing detail for the causal mechanisms and relative contributions of physical symptoms and functional limitations, their results make an important contribution to understanding the disablement process in OA.
While there are many opportunities to improve our understanding of the specific role of risk factors, intra-individual factors, and extra-individual factors in the relationships among pathology, impairment functional limitations and disability, the analytic models employed need to be consistent with the objectives of this disablement research. We highlighted two examples of potential approaches to advancing our understanding of these factors. There are others in the OA literature, for example the use of ordinary least squares regression to model pathways, [46]. However, for most factors discussed the temporal pattern and relative impacts on key disability milestones are relatively unknown. Future work would use longitudinal data to test hypotheses about the relative impact of these factors rather than adjusting for them.
Acknowledgments
Dr. McDonough is supported by a New Investigator Fellowship Training Initiative in Health Services Research award from the Foundation for Physical Therapy. This work was supported, in part, by the Boston Claude D. Pepper Older Americans Independence Center (P30-AG031679).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Commercial Support/Conflicts Statement. None
References
- [1].Covinsky K. Aging, Arthritis, and Disability. Arthritis & Rheumatism (Arthritis Care & Research) 2006 Apr 15;55(2):175–6. doi: 10.1002/art.21861. [DOI] [PubMed] [Google Scholar]
- [2].Covinsky KE, Lindquist K, Dunlop DD, Gill TM, Yelin E, Covinsky KE, et al. Effect of arthritis in middle age on older-age functioning. Journal of the American Geriatrics Society. 2008 Jan;56(1):23–8. doi: 10.1111/j.1532-5415.2007.01511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Dunlop D, Hughes S, Manheim L. Disability in activities of daily living: Patterns of change and a hierarchy of disability. Am J Public Health. 1997;87:378–83. doi: 10.2105/ajph.87.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dunlop D, Manheim L, Song J, Chang R. Arthritis prevalence and activity limitations in older adults. Arthritis Rheum. 2001;44(1):212–21. doi: 10.1002/1529-0131(200101)44:1<212::AID-ANR28>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- [5].Felson D, Lawrence R, Dieppe P, Hirsch R, Helmick C, Jordan J. Osteoarthrits: new insights. Part 1: the disease and its risk factors. Annals of Internal Medicine. 2000;133(8):635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [Review] [120 refs] [DOI] [PubMed] [Google Scholar]
- [6].Institute of Medicine (IOM) The Future of Disability in America. Washington, DC: 2007. [Google Scholar]
- [7].Ling SM, Xue QL, Simonsick EM, Tian J, Bandeen-Roche K, Fried LP, et al. Transitions to Mobility Difficulty Associated With Lower Extremity Osteoarthritis in High Functioning Older Women: Longitudinal Data From the Women’s Health and Aging Study II. Arthritis & Rheumatism (Arthritis Care & Research) 2006 Apr 15;55(2):256–63. doi: 10.1002/art.21858. [DOI] [PubMed] [Google Scholar]
- [8].Song J, Chang RW, Dunlop DD. Population Impact of Arthritis on Disability in Older Adults. Arthritis & Rheumatism (Arthritis Care & Research) 2006 Apr 15;55(2):248–55. doi: 10.1002/art.21842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Verbrugge LM, Juarez L. Profile of Arthritis Disability: II. Arthritis & Rheumatism (Arthritis Care & Research) 2006 Feb 15;55(1):102–13. doi: 10.1002/art.21694. [DOI] [PubMed] [Google Scholar]
- [10].Saase, van Romunde L, Cats A, Vandenbrouke J, Valkenbourg H. Epidemiology of arthritis: Zoetermeer survey. Comparison of radiological arthritis in a Dutch population with that of 10 other populations. Ann Rheum Dis. 1989;20:351–69. doi: 10.1136/ard.48.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ferrucci L, Guralnik JM, Simonsick E, Salive ME, Corti C, Langlois J, et al. Progressive versus catastrophic disability: a longitudinal view of the disablement process. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 1996 May;51(3):M123–30. doi: 10.1093/gerona/51a.3.m123. [DOI] [PubMed] [Google Scholar]
- [12].Mallen CD, Peat G, Thomas E, Lacey R, Croft P, Mallen CD, et al. Predicting poor functional outcome in community-dwelling older adults with knee pain: prognostic value of generic indicators. Ann Rheum Dis. 2007 Nov;66(11):1456–61. doi: 10.1136/ard.2006.067975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Roos EM, Bremander AB, Englund M, Lohmander LS, Roos EM, Bremander AB, et al. Change in self-reported outcomes and objective physical function over 7 years in middle-aged subjects with or at high risk of knee osteoarthritis. Ann Rheum Dis. 2008 Apr;67(4):505–10. doi: 10.1136/ard.2007.074088. [DOI] [PubMed] [Google Scholar]
- [14].Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D, et al. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003 Dec;48(12):3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- [15].van Dijk GM, Dekker J, Veenhof C, van den Ende CH, Carpa Study G, van Dijk GM, et al. Course of functional status and pain in osteoarthritis of the hip or knee: a systematic review of the literature. Arthritis Rheum. 2006 Oct 15;55(5):779–85. doi: 10.1002/art.22244. [DOI] [PubMed] [Google Scholar]
- [16].Lawrence J, Bremner JM, F B. Prevalence in the population and relatonships between symptoms and x-ray changes. Ann Rheum Dis. 1966;25:1–24. [PMC free article] [PubMed] [Google Scholar]
- [17].Jette A. Disentangling the process of disablement. Social Science and Medicine. 1999;48:471–2. doi: 10.1016/s0277-9536(98)00371-2. [DOI] [PubMed] [Google Scholar]
- [18].Nagi S. Some conceptual issues disability and rehabiliation. In: Sussman M, editor. Sociology and rehabilitation. American Sociology Association; Washington, DC: 1965. pp. 100–13. [Google Scholar]
- [19].Nagi S. The concept and measurement of disability. In: ED B, editor. Disability policies and government programs. New York Praeger; 1979. [Google Scholar]
- [20].Verbrugge LM, Jette AM. The Disablement Process. Social Science and Medicine. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- [21].Verbrugge LM, Lepkowski JM, Konkol LL, Verbrugge LM, Lepkowski JM, Konkol LL. Levels of disability among U.S. adults with arthritis. Journal of Gerontology. 1991 Mar;46(2):S71–83. doi: 10.1093/geronj/46.2.s71. [DOI] [PubMed] [Google Scholar]
- [22].Verbrugge LM, Gates DM, Ike RW, Verbrugge LM, Gates DM, Ike RW. Risk factors for disability among U.S. adults with arthritis. Journal of Clinical Epidemiology. 1991;44(2):167–82. doi: 10.1016/0895-4356(91)90264-a. [DOI] [PubMed] [Google Scholar]
- [23].Hochberg MC, Kasper J, Williamson J, Skinner A, Fried LP, Hochberg MC, et al. The contribution of osteoarthritis to disability: preliminary data from the Women’s Health and Aging Study. Journal of Rheumatology - Supplement. 1995 Feb;43:16–8. [PubMed] [Google Scholar]
- [24].Merikangas K, Ames M, Cui L, Stang P, Ustun T, Von Korff M, et al. The impact of comorbidity of mental and physical conditions on role disability in the US adult household population. Arch Gen Psych. 2007;64(10):1180–8. doi: 10.1001/archpsyc.64.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Verbrugge LM, Juarez L, Verbrugge LM, Juarez L. Profile of arthritis disability. Public Health Reports. 2001;116(Suppl 1):157–79. doi: 10.1093/phr/116.S1.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Guccione A, Felson D, Anderson J, Anthony J, Zhang Y, Wilson P. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Amercian Journal of Public Health. 1994;84(3):351–8. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Reginster JY, Khaltaev NG, Reginster JY, Khaltaev NG. Introduction and WHO perspective on the global burden of musculoskeletal conditions. Rheumatology (Oxford) 2002 Apr;41(Supp 1):1–2. [PubMed] [Google Scholar]
- [28].Fautrel B, Hilliquin P, Rozenberg S, Allaert FA, Coste P, Leclerc A, et al. Impact of osteoarthritis: results of a nationwide survey of 10,000 patients consulting for OA. Joint, Bone, Spine: Revue du Rhumatisme. 2005 May;72(3):235–40. doi: 10.1016/j.jbspin.2004.08.009. [DOI] [PubMed] [Google Scholar]
- [29].Zhang Y, Niu J, Kally-Hayes M, Chaisson C, Aliabadi P, Felson D. Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly. Am J Epidemiol. 2002;156:1021–7. doi: 10.1093/aje/kwf141. [DOI] [PubMed] [Google Scholar]
- [30].Dekker J, van Dijk GM, Veenhof C, Dekker J, van Dijk GM, Veenhof C. Risk factors for functional decline in osteoarthritis of the hip or knee. Current Opinion in Rheumatology. 2009 Sep;21(5):520–4. doi: 10.1097/BOR.0b013e32832e6eaa. [DOI] [PubMed] [Google Scholar]
- [31].Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW, et al. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005 Apr;52(4):1274–82. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Wilkie R, Peat G, Thomas E, Croft P, Wilkie R, Peat G, et al. Factors associated with participation restriction in community-dwelling adults aged 50 years and over. Quality of Life Research. 2007 Sep;16(7):1147–56. doi: 10.1007/s11136-007-9221-5. [DOI] [PubMed] [Google Scholar]
- [33].Wilkie R, Peat G, Thomas E, Croft P, Wilkie R, Peat G, et al. Factors associated with restricted mobility outside the home in community-dwelling adults ages fifty years and older with knee pain: an example of use of the International Classification of Functioning to investigate participation restriction. Arthritis Rheum. 2007 Dec 15;57(8):1381–9. doi: 10.1002/art.23083. [DOI] [PubMed] [Google Scholar]
- [34].Lamb SE, Guralnik JM, Buchner DM, Ferrucci LM, Hochberg MC, Simonsick EM, et al. Factors that modify the association between knee pain and mobility limitation in older women: the Women’s Health and Aging Study. Ann Rheum Dis. 2000 May;59(5):331–7. doi: 10.1136/ard.59.5.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Mottram S, Peat G, Thomas E, Wilkie R, Croft P, Mottram S, et al. Patterns of pain and mobility limitation in older people: cross-sectional findings from a population survey of 18,497 adults aged 50 years and over. Quality of Life Research. 2008 May;17(4):529–39. doi: 10.1007/s11136-008-9324-7. [DOI] [PubMed] [Google Scholar]
- [36].van Dijk GM, Veenhof C, Spreeuwenberg P, Coene N, Burger BJ, van Schaardenburg D, et al. Prognosis of limitations in activities in osteoarthritis of the hip or knee: a 3-year cohort study. Archives of Physical Medicine & Rehabilitation. 2010 Jan;91(1):58–66. doi: 10.1016/j.apmr.2009.08.147. [DOI] [PubMed] [Google Scholar]
- [37].Miller ME, Rejeski WJ, Messier SP, Loeser RF, Miller ME, Rejeski WJ, et al. Modifiers of change in physical functioning in older adults with knee pain: the Observational Arthritis Study in Seniors (OASIS) Arthritis Rheum. 2001 Aug;45(4):331–9. doi: 10.1002/1529-0131(200108)45:4<331::AID-ART345>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- [38].Jinks C, Jordan K, Croft P, Jinks C, Jordan K, Croft P. Osteoarthritis as a public health problem: the impact of developing knee pain on physical function in adults living in the community: (KNEST 3) Rheumatology (Oxford) 2007 May;46(5):877–81. doi: 10.1093/rheumatology/kem013. [DOI] [PubMed] [Google Scholar]
- [39].Machado GP, Gignac MA, Badley EM, Machado GPM, Gignac MAM, Badley EM. Participation restrictions among older adults with osteoarthritis: a mediated model of physical symptoms, activity limitations, and depression. Arthritis Rheum. 2008 Jan 15;59(1):129–35. doi: 10.1002/art.23259. [DOI] [PubMed] [Google Scholar]
- [40].Ayis S, Dieppe P, Ayis S, Dieppe P. The natural history of disability and its determinants in adults with lower limb musculoskeletal pain. Journal of Rheumatology. 2009 Mar;36(3):583–91. doi: 10.3899/jrheum.080455. [DOI] [PubMed] [Google Scholar]
- [41].Peters TJ, Sanders C, Dieppe P, Donovan J, Peters TJ, Sanders C, et al. Factors associated with change in pain and disability over time: a community-based prospective observational study of hip and knee osteoarthritis. British Journal of General Practice. 2005 Mar;55(512):205–11. [PMC free article] [PubMed] [Google Scholar]
- [42].Rejeski WJ, Miller ME, Foy C, Messier S, Rapp S, Rejeski WJ, et al. Self-efficacy and the progression of functional limitations and self-reported disability in older adults with knee pain. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2001 Sep;56(5):S261–5. doi: 10.1093/geronb/56.5.s261. [DOI] [PubMed] [Google Scholar]
- [43].Shelby RA, Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Blumenthal JA, et al. Domain specific self-efficacy mediates the impact of pain catastrophizing on pain and disability in overweight and obese osteoarthritis patients. Journal of Pain. 2008 Oct;9(10):912–9. doi: 10.1016/j.jpain.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Pells JJ, Shelby RA, Keefe FJ, Dixon KE, Blumenthal JA, Lacaille L, et al. Arthritis self-efficacy and self-efficacy for resisting eating: relationships to pain, disability, and eating behavior in overweight and obese individuals with osteoarthritic knee pain. Pain. 2008 Jun;136(3):340–7. doi: 10.1016/j.pain.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Wright LJ, Zautra AJ, Going S, Wright LJ, Zautra AJ, Going S. Adaptation to early knee osteoarthritis: the role of risk, resilience, and disease severity on pain and physical functioning. Annals of Behavioral Medicine. 2008 Aug;36(1):70–80. doi: 10.1007/s12160-008-9048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Parmelee P, Harralson T, Smith L, Schumacher H. Necessary and discretionary activities in knee osteoarthritis: Do they mediate the pain-depression relationship? Pain Medicine. 2007;8(5):449–61. doi: 10.1111/j.1526-4637.2007.00310.x. [DOI] [PubMed] [Google Scholar]
- [47].Verbrugge LM, Juarez L, Verbrugge LM, Juarez L. Arthritis disability and heart disease disability. Arthritis Rheum. 2008 Oct 15;59(10):1445–57. doi: 10.1002/art.24107. [DOI] [PubMed] [Google Scholar]