Abstract
Fanconi anaemia (FA) is a rare autosomal recessive or X-linked inherited disease characterised by an increased incidence of bone marrow failure (BMF), haematological malignancies and solid tumours. Cells from individuals with FA show a pronounced sensitivity to DNA interstrand crosslink (ICL)-inducing agents, which manifests as G2-M arrest, chromosomal aberrations and reduced cellular survival. To date, mutations in at least 15 different genes have been identified that cause FA; the products of all of these genes are thought to function together in the FA pathway, which is essential for ICL repair. Rapidly following the discovery of FA genes, mutant mice were generated to study the disease and the affected pathway. These mutant mice all show the characteristic cellular ICL-inducing agent sensitivity, but only partially recapitulate the developmental abnormalities, anaemia and cancer predisposition seen in individuals with FA. Therefore, the usefulness of modelling FA in mice has been questioned. In this Review, we argue that such scepticism is unjustified. We outline that haematopoietic defects and cancer predisposition are manifestations of FA gene defects in mice, albeit only in certain genetic backgrounds and under certain conditions. Most importantly, recent work has shown that developmental defects in FA mice also arise with concomitant inactivation of acetaldehyde metabolism, giving a strong clue about the nature of the endogenous lesion that must be repaired by the functional FA pathway. This body of work provides an excellent example of a paradox in FA research: that the dissimilarity, rather than the similarity, between mice and humans can provide insight into human disease. We expect that further study of mouse models of FA will help to uncover the mechanistic background of FA, ultimately leading to better treatment options for the disease.
Introduction
Fanconi anaemia (FA) is a rare recessive disorder characterised by bone marrow failure (BMF), developmental abnormalities and an increased cancer risk. Anaemia as a consequence of BMF is usually the first life-threatening symptom with which individuals with FA present. More than two thirds of FA patients also present with a wide range of developmental abnormalities such as microcephaly, microphthalmia, abnormalities of the skeleton (thumb and/or radius), short stature, low birth weight and genital malformations (Tischkowitz and Hodgson, 2003). Later in life, individuals with FA also have a high risk of developing cancer, especially acute myeloid leukaemia (AML), squamous cell carcinoma (SCC) of the head and neck, SCC of the oesophagus, liver tumours, and gynaecological cancers (Kutler et al., 2003; Rosenberg et al., 2008). The cumulative probability in FA patients of developing leukaemia, solid tumours or liver tumours is almost 40% by age 30, ∼50% by age 45 and 76% by age 60 (Alter, 2003).
A total of 15 FA complementation groups have been identified thus far, representing 15 genes in which mutations cause FA or an FA-like disorder (D’Andrea, 2010; Stoepker et al., 2011; Vaz et al., 2010). Despite the genetic and phenotypic heterogeneity of FA, cells from individuals with FA of all complementation groups share a characteristic hypersensitivity to DNA interstrand crosslink (ICL)-inducing agents, owing to defects in an essential DNA repair pathway. The identification of the FA genes, and functional analyses of the proteins they encode, have uncovered the molecular details of this pathway, now known as the FA pathway.
Most FA proteins are found in a complex called the FA core complex. This complex consists of eight FA proteins (FANCA, FANCB, FANCC, FANCE, FANCF, FANCG, FANCL and FANCM), which are all known to cause FA in humans when defective, and four FA-associated proteins (FAAP24, FAAP100, MHF1 and MHF2) (Singh et al., 2010), which thus far have not been implicated in FA. The formation of the FA core complex is necessary for the efficient monoubiquitylation of the downstream-acting proteins FANCD2 and FANCI by the E3 ubiquitin ligase FANCL; UBE2T acts as the E2 ligase (de Winter and Joenje, 2009), but has not been associated with FA. The remaining FA proteins – FANCD1 (also known as BRCA2), FANCJ (BRIP1), FANCN (PALB2), FANCO (RAD51C) and FANCP (SLX4) – act downstream or in parallel to this monoubiquitylation step in the FA pathway to facilitate ICL repair (Deans and West, 2011).
Following the identification of FA genes in humans, blast searches for orthologues in other species were undertaken. The conservation of most FA proteins, especially the FA core complex members, seems limited to vertebrates (Blom et al., 2002), although orthologues of FANCD2 and FANCL are found in non-vertebrates (Arabidopsis) (Alpi et al., 2008). In Drosophila melanogaster and the urochordate Ciona intestinalis, only FANCD2, FANCL and FANCM exist, and it seems that FANCL can monoubiquitylate FANCD2 by itself and confer resistance to ICL-inducing agents in the fly (Marek and Bale, 2006; Titus et al., 2006). It remains enigmatic why so many FA core complex proteins are required for regulating FANCL ubiquitin ligase activity in vertebrates. This is a puzzle that is difficult to tackle given that most FA core complex members, apart from FANCL and FANCM, are orphan proteins lacking functional domains. Nevertheless, it is clear that the FA core complex has evolved in vertebrates, and that each member is essential for proper functioning of the FA pathway.
To study FA clinical phenotypes and develop a potential treatment for FA-associated symptoms, the laboratory mouse (Mus musculus) is a frequently used model system. In this Review, we discuss common and divergent phenotypes that are associated with FA gene disruptions in mice and humans. In addition, we demonstrate that the dissimilarity, rather than the similarity, between FA phenotypes in mice and humans provides important insight into FA pathology, which might contribute to the development of new treatments.
FA mouse models
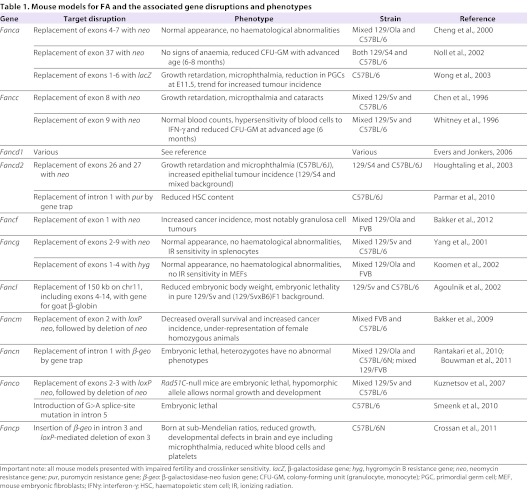
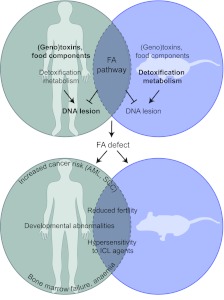
Targeted disruption of FA genes has been used to create several FA mouse models, which are detailed in Table 1. All FA mouse models show reduced fertility, and cells derived from all mutant mice are sensitive to ICL-inducing agents – the characteristic cellular phenotype of FA. However, FA phenotypes at the organism level were only observed in some models. In the following section, we provide an overview of phenotypes that are associated with FA gene disruptions in mice and compare them with human FA pathology. A summary of the discordance and similarity between humans with FA and FA mouse models is depicted in the lower panel of Fig. 1.
Table 1.
Mouse models for FA and the associated gene disruptions and phenotypes
Fig. 1.
Discordance and similarity between humans with FA and FA mouse models. FA-associated phenotypes in humans and mice are illustrated in a Venn-like diagram. FA phenotypes (lower diagram) are depicted in the common area between the two circles when shared between humans and mice or further away from the common area when phenotypes only partially overlap. We propose that, due to environmental and genetic differences between humans and laboratory mice (upper diagram), humans rely on an effective FA pathway to ensure normal development and tumour suppression, whereas mice are less dependent on an active FA pathway.
Embryonic and perinatal lethality
Embryonic lethality caused by homozygous disruption of FA genes seems to be restricted to genes encoding proteins that are not members of the FA core complex, such as Fancd1, Fancn and Fanco. An exception is Fancl mice, which are embryonic lethal on a pure 129/Sv or C57BL/6 background but are viable on a mixed C57BL/6×FVB background (Agoulnik et al., 2002). Mice that are homozygous mutant for either Fancd1 or Fancn die early during embryonic development due to increased apoptosis; this phenotype is alleviated but not rescued in a p53-deficient background (Bouwman et al., 2011; Evers and Jonkers, 2006). The corresponding heterozygous mice do not show a strong tumour predisposing phenotype (Rantakari et al., 2010), even in a p53-deficient background (Bouwman et al., 2011). To bypass lethality, conditional models have been extensively used to study Fancd1 tumour suppressor function and have revealed a synergistic effect of combined Fancd1 and p53 deficiency on tumorigenesis (Jonkers et al., 2001).
Perinatal lethality has been described for several FA mouse mutants, including Fancc (Carreau, 2004), Fancd2 (Houghtaling et al., 2003; van de Vrugt et al., 2009), Fancl (Agoulnik et al., 2002), Fancm (Bakker et al., 2009) and Fancp (Crossan et al., 2011); however, the mechanism for this lethality has not been studied. Perinatal lethality has been found to depend strongly on genetic background. In particular, the C57BL/6J background leads to a more severe perinatal lethality phenotype, as was clearly demonstrated in a recent study in which Fancc- and Fancd2-deficient mice were under-represented in this background but not in a mixed 129S4 × C57BL/6J background (van de Vrugt et al., 2009). For Fancm-deficient mice, an under-representation of females was observed (Bakker et al., 2009), but this effect was also dependent on the genetic background (S.T.B. and H.t.R., unpublished results). These data suggest that FA pathway disruptions in mice affect viability when combined with the presence of modifier loci in certain genetic backgrounds (especially the C57BL/6J background). These loci will probably become apparent in the near future, when next-generation sequencing will reveal sequence variants between different strains.
Although perinatal lethality has not been reported for humans with FA, it is clear that some FA gene defects lead to a more severe phenotype. Similar to mice, complete loss of function of FANCD1 or FANCN is probably embryonic lethal in humans, whereas hypomorphic mutations in FANCD1 or FANCN are compatible with life, although affected individuals often die at a young age (Alter et al., 2007; Tischkowitz and Xia, 2010).
Developmental abnormalities
Most FA mouse models do not show any gross, FA-specific developmental abnormalities. There are a few exceptions, however: microphthalmia has been observed in Fanca (Wong et al., 2003), Fancc (Carreau, 2004), Fancd2 (Houghtaling et al., 2003) and Fancp (Crossan et al., 2011)-deficient mice in the C57BL/6J background. In addition, a proportion of Fancp-deficient mice were also reported to have an abnormally shaped and enlarged skull (Crossan et al., 2011).
Another notable exception is the gonadal abnormality and associated infertility that is also common in individuals with FA (Auerbach, 2009). This abnormality has been observed in all FA mouse models described thus far, independent of genetic background (Parmar et al., 2009; Tischkowitz and Winqvist, 2011) and has been attributed to a reduction in the number of primordial germ cells (PGCs) (Agoulnik et al., 2002; Nadler and Braun, 2000). The loss of pluripotent PGCs in FA-pathway-deficient mice is in agreement with the crucial role for the FA pathway in the derivation or maintenance of induced pluripotent stem (iPS) cells that has been reported recently (Raya et al., 2009). It still needs to be determined how the loss of PGCs and poor stem-cell self-renewal are related to FA pathway dysfunction. It is likely that the FA pathway is not only essential for viability after exposure to ICL-inducing agents, but also for the viability of stem cells. It has been reported that iPS cells acquire DNA damage and undergo p53-mediated apoptosis during reprogramming, and that p53 disruption results in more efficient reprogramming in the presence of DNA damage (Marión et al., 2009). These observations indicate that the FA pathway might function to maintain genomic stability and prevent DNA damage in pluripotent stem cells. In the absence of a functional FA pathway, these cells might acquire DNA damage and die by apoptosis. Thus, it is possible that the loss of pluripotent stem cells causes the growth retardation and short stature observed in humans with FA.
There is also evidence that the FA pathway plays an important role in meiotic recombination. Fanca (Wong et al., 2003) and Fancd2 (Houghtaling et al., 2003)-deficient mice show an increased incidence of mispaired chromosomes in pachytene spermatocytes, which is accompanied by increased apoptosis. Also, the expression of FA proteins is increased during mid-to-late pachytene (Wong et al., 2003). During this period, chromosomes are fully synapsed, and double Holliday junctions are formed that need to be resolved (Schwacha and Kleckner, 1995). The resolution of a double Holliday junction could be aided by the FA pathway, especially by FANCP (Svendsen and Harper, 2010; Wechsler et al., 2011). However, both Fancp-deficient male and female mice can produce offspring, indicating that meiosis takes place in these mice (Crossan et al., 2011).
Haematological abnormalities in FA mice
The absence of apparent haematological abnormalities in most FA mouse models studied thus far is in sharp contrast to the life-threatening anaemia that occurs in humans with FA. Notable exceptions are Fancp mutant mice, which have lower white blood cell counts and very low levels of platelets, and hypomorphic Fancd1 mice, which have a proliferation defect in haematopoietic progenitors (Crossan et al., 2011; Navarro et al., 2006). Therefore, studying the underlying molecular defects of haematopoietic failure in these two mouse models could aid in understanding haematological problems in individuals with FA.
FA mice have been used to study the role of the FA pathway in haematopoietic homeostasis. Blood homeostasis is maintained by haematopoietic stem cells (HSCs), which are long-lived cells that can self-renew and differentiate to give rise to all blood cell lineages. HSCs are defined by their ability to reconstitute the bone marrow of lethally irradiated mice in the long term. It has been shown that HSCs from several different mouse mutants (Fancc, Fancd2 and Fancg) have a reduced repopulating ability compared with wild-type HSCs (Barroca et al., 2012; Haneline et al., 1999; Zhang et al., 2008). In addition, BMF can be induced by treating Fancc-deficient mice with a single high dose of mitomycin C (MMC) or by chronic exposure to MMC (Carreau et al., 1998). This demonstrates that, although Fancc-deficient HSCs can maintain haematopoietic homeostasis under normal conditions, they fail to do so under conditions of stress, when HSCs need to be mobilised and replicate. More recent data demonstrate that Fancg-deficient HSCs also show defects in mobilisation and homing to the bone marrow (Barroca et al., 2012). Thus, the absence of anaemia in most FA mouse models might indicate that FA mutant mice housed in laboratory conditions are protected from stressful environmental cues that might contribute to BMF in humans with FA. Intriguingly, lipopolysaccharide and tumour necrosis factor-α (TNF-α) also suppress hematopoiesis in FA mice, suggesting that other stress inducers in addition to DNA-damaging agents can influence the phenotype (Sejas et al., 2007).
To identify compounds that improve HSC fitness in mouse models of FA, competitive repopulation assays have been used in combination with drug treatment. For example, an improved repopulating ability of Fancc-deficient HSCs was demonstrated after treatment with a p38 MAP-kinase inhibitor (Saadatzadeh et al., 2009). The Fancd2 mouse mutant could be especially suitable for studying the contribution of the FA pathway in HSC biology. In addition to performing poorly in competitive repopulation, Fancd2-deficient HSCs were also reduced in number (Zhang et al., 2010). In 3-week-old Fancd2 mice, HSCs were already under-represented, indicative of an early defect in HSC development and/or maintenance. The more severe phenotype of Fancd2-deficient mice suggests that non-ubiquitylated FANCD2 functions in HSC maintenance (Zhang et al., 2010). Fancd2-deficient HSCs also showed increased cell cycle entry and loss of their normal quiescent state, as has also been described for Fancc-deficient HSCs (Li et al., 2003). It is tempting to speculate that the enhanced cell cycle entry of HSCs compensates for the lower number of HSCs and thus prevents BMF in the short term. However, in the long term, this accelerated HSC turnover could lead to HSC exhaustion and subsequent BMF.
The clear phenotype of Fancd2-deficient HSCs makes this mouse a suitable preclinical model to study compounds that could reverse this abnormal cell cycle state. For example, Zhang et al. have shown that the HSC phenotype and reduced repopulating ability could be partially rescued by resveratrol (Zhang et al., 2010), a polyphenol found in grapes and red wine.
The endogenous lesion targeted by the FA pathway
Despite the promising effect of resveratrol, advising individuals with FA to indulge in red wine to improve white blood cell counts is probably counterproductive, given recent data on the involvement of the FA pathway in acetaldehyde toxicity (Langevin et al., 2011). Aldehydes are reactive metabolites that can induce DNA-DNA and DNA-protein crosslinks, and are produced endogenously during normal metabolism or as a byproduct of ethanol metabolism. Aldehyde dehydrogenases (ALDHs) are responsible for the detoxification of aldehydes by oxidising them to carboxylic acids (Crabb et al., 2004). In mouse-crossing experiments, it was shown that Fancd2 mutant mice were not viable in the absence of fetal and maternal ALDH2. Double-mutant homozygous Fancd2−/− Aldh2−/− animals could be obtained from crosses in which at least the mother was Aldh2+/−, but these mice died within 3–6 months owing to the development of acute lymphoblastic leukaemia (ALL). In addition, when Fancd2−/− Aldh2−/− mutant embryos were exposed to ethanol in utero, most developed severe physical abnormalities and died. Surviving young Fancd2−/− Aldh2−/− mutant animals had a severe reduction in bone marrow cellularity and showed γH2AX induction, indicating DNA damage. These data collectively demonstrate that excess acetaldehyde from endogenous or exogenous sources results in severe toxicity in the absence of FANCD2 (Langevin et al., 2011). It is tempting to speculate that excess acetaldehyde exposure also contributes to human FA pathology. It remains to be determined whether acetaldehyde-mediated toxicity in FA mutant mice is caused by a specific lesion that needs to be repaired by the FA pathway. Determining whether acetaldehyde toxicity is also seen in other FA mouse models should clarify this issue. Mouse embryonic fibroblasts (MEFs) derived from other FA core complex mutant animals were not sensitive to formaldehyde, in contrast to Fancd2-deficient MEFs (Noda et al., 2011). However, primary splenocytes from Fancd2 mutant mice, or chicken-derived DT40 cells made deficient for the FA core complex, were sensitive to acetaldehyde (Langevin et al., 2011). Also, DT40 cells mutant for translesion synthesis (TLS) or homology-directed repair (HDR) were not sensitive to acetaldehyde, despite the fact that these pathways are thought to play an important role in repairing acetaldehyde-induced crosslinks.
The emerging data on the necessity of the FA pathway for acetaldehyde detoxification is especially interesting when studying mouse models of FA. It is possible that mice with FA pathway disruptions are better protected than humans against acetaldehyde toxicity, owing to either enhanced detoxification pathways or reduced production of acetaldehyde in mice.
Viability and cancer
The high incidence of BMF, myelodysplasia and cancer contribute to the reduced life expectancy of individuals with FA, which is on average about 30 years. Cancers that frequently arise are AML, SCC of the head and neck region, SCC of the oesophagus, liver tumours, and gynaecological cancers (Alter, 2003; Kutler et al., 2003; Rosenberg et al., 2008). FA mouse models do not recapitulate this pronounced reduction in life expectancy because they generally do not succumb to accelerated tumorigenesis. Long-term survival cohorts have been published for Fancc-, Fancd2-, Fancf-, Fancm- and Fancp-deficient mice. In Fancc-deficient mice, no tumours were observed after 600 days (Freie et al., 2003). By contrast, a statistically significant increase in the incidence of both adenomas and carcinomas of epithelial origin was reported in Fancd2-deficient mice (Houghtaling et al., 2003). Furthermore, statistically significant reductions in overall and tumour-free survival were found for Fancf- and Fancm-deficient mice. Fancf-deficient mice have been reported to develop late-onset ovarian tumours, which were potentially related to a deregulation of sex hormones as a consequence of hypogonadism (Bakker et al., 2012). Fancm-deficient mice also show a reduced lifespan and increased cancer incidence, without skewing to a particular tumour type. Fancm-deficient MEFs showed an increased sister-chromatid exchange (SCE) frequency, which was not observed in Fanca-deficient MEFs and could suggest an additional role for FANCM in genome maintenance (Bakker et al., 2009). Additional crosses with other FA core complex mutant mice are needed to clarify this potential non-epistatic relationship between FANCM and the FA core complex. Overall, the increased incidence of tumorigenesis in some FA mouse models is minor compared with the reduced life expectancy and increased tumour risk in FA patients.
FA pathway and telomere function
Telomeres are repetitive DNA sequences that protect the ends of chromosomes from being recognised as DNA double-strand breaks, and are shortened during each cell division (Blackburn et al., 2006). Reduced telomere length has been correlated with increased cancer incidence (Willeit et al., 2010). In addition, anaemia has been associated with aberrant telomere maintenance and short telomeres (Ball et al., 1998; Calado and Young, 2009). Telomere length is maintained by the enzyme telomerase or through a recombination-dependent pathway called the alternative lengthening of telomeres (ALT) pathway (Cesare and Reddel, 2010). Notably, individuals with FA have shorter telomeres compared with controls (Ball et al., 1998; Leteurtre et al., 1999; Rhee et al., 2010) and several studies have indicated a role for the FA pathway in telomere biology, especially in the ALT pathway.
FANCD2 localises to ALT-associated promyelocytic leukaemia bodies in human keratinocytes, and knockdown of FANCD2 results in accelerated telomere dysfunction in cells relying on the ALT pathway (Spardy et al., 2008). The colocalisation of telomeres and FANCD2 occurred exclusively in cells relying on the ALT pathway for telomere length maintenance and depended on FANCD2 monoubiquitylation (Fan et al., 2009). This colocalisation was part of a DNA-damage response: it was increased by exposure to both hydroxyurea (HU) and MMC in a manner dependent on the key DNA-damage response protein, ATR (Fan et al., 2009; Spardy et al., 2008).
It is unclear whether other FA proteins play a role in telomere length maintenance, because FANCG-deficient human and mouse cells have normal telomere length (Franco et al., 2004). However, in general, telomere length is much greater in laboratory mice compared with humans (Frese and Tuveson, 2007). Consequently, the absence of characteristic human FA signs in currently available mouse models (such as haematopoietic problems or increased cancer incidence) could be because mice have longer telomeres than humans. To directly address the contribution of the FA pathway in regulating telomere length and the importance of telomere length on FA pathology in mice, Fancc-deficient mice with long (C57/BL/6 strain) or short (Tert+/− telomerase mutant strain) telomeres were studied. The results of this study suggest that the FA pathway does not regulate telomere length but rather is necessary for maintaining telomere length when bone marrow cells are stressed, for example in repopulation assays (Rhee et al., 2010).
Double-mutant FA mice
To determine whether different FA proteins have redundant or divergent functions in the FA pathway, mice carrying mutations in two different FA genes have been generated. In principle, a double mutant that phenocopies the single mutants reveals an epistatic relationship, whereas a broader phenotype dictates a non-epistatic relationship. In practice, however, interpreting the phenotype of double FA mutants is less straightforward. The first double-mutant mice reported, Fanca−/− Fancc−/−, show no evidence of an additive phenotype, suggesting an epistatic relationship between the two genes (Noll et al., 2002). However, Fancc−/− Fancg−/− double-mutant mice have a broader phenotype: the mice develop BMF, myelodysplasia and complex cytogenetic abnormalities, which are phenotypes that were not present in either single knockout mouse strain (Pulliam-Leath et al., 2010). It was suggested that this non-epistatic relationship between Fancc and Fancg revealed a unique function for Fancg, because an additive phenotype was not observed in Fanca−/− Fancc−/− double-mutant mice. Recent data have, however, complicated this interpretation. Mice mutant for both Fanca and Fancg showed no additive phenotype, suggesting an epistatic relationship between these genes (van de Vrugt et al., 2011). The different outcomes of epistasis analysis could again be explained by the presence of FA pathway modifiers in different mouse strains. The Fanca−/− Fancc−/− and Fanca−/− Fancg−/− mice were maintained on a 129S4 and a mixed 129Ola/FVB genetic background, respectively, whereas the Fancc−/− Fancg−/− mice were maintained on a C57BL/6J genetic background. As described above, FA core complex gene defects seem to have a stronger penetrance in C57BL/6J mice (van de Vrugt et al., 2009). Therefore, C57BL/6J-associated modifier genes might have contributed to the more severe phenotype of the Fanc−/− Fancg−/− mice. The generation of more double-mutant mice in the same genetic background should shed light on the (non-)epistatic relationships between different FA (core complex) genes.
In addition to double-mutant mice of FA core complex genes, double mutants that included Fancd2 knockout have been generated. A recent study reported a non-epistatic relationship between Fancd2 and Fancg: Fancd2−/− Fancg−/− mice were not viable in the C57BL/6J background (Reliene et al., 2010). Also, Fancd2 but not Fancg mutant mice showed an increased frequency of homologous recombination (HR)-mediated deletions at an endogenous locus, as well as more DNA damage and chromosomal instability (Reliene et al., 2010). This additional role of FANCD2 in genome stability could be related to its role in the intra-S-phase checkpoint. FANCD2 mutant patient cells continue DNA synthesis after ionizing radiation (IR), indicative of a defective intra-S-phase checkpoint. This phenotype was not observed in FANCC mutant patient cells, indicating that this role of FANCD2 is not dependent on FANCD2 monoubiquitylation (Taniguchi et al., 2002). Also, FANCD2 is phosphorylated by ATM and CHK1 independently of the FA core complex (Taniguchi et al., 2002; Zhi et al., 2009). It is clear that further studies are needed to determine which phenotypes found in the Fancd2-deficient mice extend to other mice carrying mutations in FA core complex genes, and to determine the function of non-ubiquitylated FANCD2. In view of the fact that FANCD2 and FANCI form a complex, the generation and characterisation of Fanci-deficient mice would be highly informative in determining the extent to which FANCI is really the ‘fraternal twin’ of FANCD2 in and outside the FA pathway, i.e. in tumour suppression, HSC maintenance and telomere biology (Grompe and van de Vrugt, 2007).
Double-mutant mice: FA and non-FA genes
To further uncover genetic interactions between the FA pathway and other cellular pathways, mouse models of FA have been crossed to other mouse models. As demonstrated by the Fancd2−/− Aldh2−/− mouse study (Langevin et al., 2011), in vivo genetic interaction studies can shed light on the function of FA genes by enhancing their importance on a sensitised background. For example, it was demonstrated that mice that are mutant for Fancc and superoxide dismutase 1 (Sod1) have decreased red blood cell counts and colony-forming capacity of bone marrow cells. SOD1 metabolizes reactive oxygen species (ROS), which cause oxidative damage. Therefore, the aggravated phenotype in these double-mutant mice suggests that FANCC functions in counteracting superoxide-mediated genotoxicity (Hadjur et al., 2001).
Genetic interaction studies can also be extended to tumour-prone mouse models. By comparing tumour latency, multiplicity and type between mice with a sensitised background only versus mice also carrying a defect in an FA gene, it is possible to assess whether and how the tumour phenotype is modified. For example, it was demonstrated that both Fancc and Fancd2 deficiency decreased the latency of tumour development in p53 mutant mice (Freie et al., 2003; Houghtaling et al., 2005). p53 heterozygous mice are prone to developing sarcomas, whereas homozygous animals mainly develop thymic lymphomas, but also sarcomas and teratomas with a much shorter latency (Jacks et al., 1994). Fancc deficiency accelerates tumorigenesis in both the p53 mutant heterozygous and homozygous background (Freie et al., 2003). Moreover, Fancc−/− p53−/− mutant mice also develop tumours that were not observed in p53−/− single mutants. The combination of p53+/− with Fancd2 loss also resulted in a significant decrease in tumour-free survival, and female animals showed a high incidence of adenocarcinomas (Houghtaling et al., 2005). Potentially, these tumours were also stimulated by aberrant sex hormone levels as a consequence of hypogonadism, as has been suggested for the development of ovarian tumours in Fancf-deficient mice (Bakker et al., 2012). The accelerated tumour formation in p53/FA double-mutant mice suggests that the FA pathway prevents both spontaneous and genotoxin-induced chromosome instability, and that activation of p53 following this DNA damage limits cell proliferation to avoid tumour formation (Freie et al., 2003; Houghtaling et al., 2005).
p53/FA double-mutant mouse models might be suitable to study chemoprevention regimens with the potential of clinical use in individuals with FA. As an elegant example, tempol was shown to be a potent chemopreventive drug that specifically delayed the onset of epithelial tumours in Fancd2-deficient p53+/− female animals (Zhang et al., 2008).
Concluding remarks
In conclusion, most FA mouse models do not fully recapitulate the hallmark characteristics of FA, but most exhibit certain features of the disease at the phenotypic and/or molecular level. Thus, despite the apparent lack of gross FA symptoms in mouse models, studying them has allowed us to learn a great deal about the pathology of FA. The reduction in PGCs and consequent hypogonadism as a common phenotype of FA mouse models suggest that the FA pathway is important in early embryogenesis, probably for repairing replication-associated stress. Furthermore, the lower number of HSCs in young Fancd2-deficient mice suggests that also the development or maintenance of these stem cells is compromised in the absence of an active FA pathway. In particular, the Fancp mutant mouse model will probably be studied extensively in the future owing to the occurrence of a haematological phenotype resembling that of human FA.
An important and encouraging finding is the fact that FA pathway deficiency in mice does not jeopardise survival under normal circumstances. FA mice seem to thrive in the controlled environment of the laboratory (although the cellular phenotype of ICL-inducing agent sensitivity is maintained), and they display FA phenotypes only on exposure to genotoxic stress from either exogenous agents, such as MMC or ethanol, or endogenous molecules, such as acetaldehyde or ROS. That is, FA mutant mice seem to thrive because of the absence of harmful environmental stresses or owing to highly effective detoxification metabolisms (Fig. 1, upper panel). This suggests that it would be beneficial for individuals with FA to avoid certain environmental cues. Uncovering the nature of the environmental cues that trigger an FA phenotype in mice will undoubtedly stimulate the development of therapies for FA patients.
Footnotes
COMPETING INTERESTS
The authors declare no competing or financial interests.
FUNDING
Our work on FA mouse models is supported by the Fanconi Anaemia Research Fund and the Dutch Cancer Society (NKI 2006–3589).
REFERENCES
- Agoulnik A. I., Lu B., Zhu Q., Truong C., Ty M. T., Arango N., Chada K. K., Bishop C. E. (2002). A novel gene, Pog, is necessary for primordial germ cell proliferation in the mouse and underlies the germ cell deficient mutation, gcd. Hum. Mol. Genet. 11, 3047–3053 [DOI] [PubMed] [Google Scholar]
- Alpi A. F., Pace P. E., Babu M. M., Patel K. J. (2008). Mechanistic insight into site-restricted monoubiquitination of FANCD2 by Ube2t, FANCL, and FANCI. Mol. Cell 32, 767–777 [DOI] [PubMed] [Google Scholar]
- Alter B. P. (2003). Cancer in Fanconi anemia, 1927–2001. Cancer 97, 425–440 [DOI] [PubMed] [Google Scholar]
- Alter B. P., Rosenberg P. S., Brody L. C. (2007). Clinical and molecular features associated with biallelic mutations in FANCD1/BRCA2. J. Med. Genet. 44, 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach A. D. (2009). Fanconi anemia and its diagnosis. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis 668, 4–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker S. T., van de Vrugt H. J., Rooimans M. A., Oostra A. B., Steltenpool J., Delzenne-Goette E., van der Wal A., van der Valk M., Joenje H., te Riele H., et al. (2009). Fancm-deficient mice reveal unique features of Fanconi anemia complementation group M. Hum. Mol. Genet. 18, 3484–3495 [DOI] [PubMed] [Google Scholar]
- Bakker S. T., van de Vrugt H. J., Visser J. A., Delzenne-Goette E., van der Wal A., Berns M. A. D., van de Ven M., Oostra A. B., de Vries S., Kramer P., et al. (2012). Fancf-deficient mice are prone to develop ovarian tumours. J. Pathol. 226, 28–39 [DOI] [PubMed] [Google Scholar]
- Ball S. E., Gibson F. M., Rizzo S., Tooze J. A., Marsh J. C., Gordon-Smith E. C. (1998). Progressive telomere shortening in aplastic anemia. Blood 91, 3582–3592 [PubMed] [Google Scholar]
- Barroca V., Mouthon M. A., Lewandowski D., Brunet de la Grange P., Gauthier L. R., Pflumio F., Boussin F. D., Arwert F., Riou L., Allemand I., et al. (2012). Impaired functionality and homing of Fancg-deficient hematopoietic stem cells. Hum. Mol. Genet. 21, 121–135 [DOI] [PubMed] [Google Scholar]
- Blackburn E. H., Greider C. W., Szostak J. W. (2006). Telomeres and telomerase: the path from maize, Tetrahymena and yeast to human cancer and aging. Nat. Med. 12, 1133–1138 [DOI] [PubMed] [Google Scholar]
- Blom E., van de Vrugt H. J., de Winter J. P., Arwert F., Joenje H. (2002). Evolutionary clues to the molecular function of fanconi anemia genes. Acta Haematol. 108, 231–236 [DOI] [PubMed] [Google Scholar]
- Bouwman P., Drost R., Klijn C., Pieterse M., van der Gulden H., Song J. Y., Szuhai K., Jonkers J. (2011). Loss of p53 partially rescues embryonic development of Palb2 knockout mice but does not foster haploinsufficiency of Palb2 in tumour suppression. J. Pathol. 224, 10–21 [DOI] [PubMed] [Google Scholar]
- Calado R. T., Young N. S. (2009). Telomere diseases. N. Engl. J. Med. 361, 2353–2365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carreau M. (2004). Not-so-novel phenotypes in the Fanconi anemia group D2 mouse model. Blood 103, 2430. [DOI] [PubMed] [Google Scholar]
- Carreau M., Gan O. I., Liu L., Doedens M., McKerlie C., Dick J. E., Buchwald M. (1998). Bone marrow failure in the Fanconi anemia group C mouse model after DNA damage. Blood 91, 2737–2744 [PubMed] [Google Scholar]
- Cesare A. J., Reddel R. R. (2010). Alternative lengthening of telomeres: models, mechanisms and implications. Nat. Rev. Genet. 11, 319–330 [DOI] [PubMed] [Google Scholar]
- Chen M., Tomkins D. J., Auerbach W., McKerlie C., Youssoufian H., Liu L., Gan O., Carreau M., Auerbach A., Groves T., et al. (1996). Inactivation of Fac in mice produces inducible chromosomal instability and reduced fertility reminiscent of Fanconi anaemia. Nat. Genet. 12, 448–451 [DOI] [PubMed] [Google Scholar]
- Cheng N. C., van de Vrugt H. J., van der Valk M. A., Oostra A. B., Krimpenfort P., de Vries Y., Joenje H., Berns A., Arwert F. (2000). Mice with a targeted disruption of the Fanconi anemia homolog Fanca. Hum. Mol. Genet. 9, 1805–1811 [DOI] [PubMed] [Google Scholar]
- Crabb D. W., Matsumoto M., Chang D., You M. (2004). Overview of the role of alcohol dehydrogenase and aldehyde dehydrogenase and their variants in the genesis of alcohol-related pathology. Proc. Nutr. Soc. 63, 49–63 [DOI] [PubMed] [Google Scholar]
- Crossan G. P., van der Weyden L., Rosado I. V., Langevin F., Gaillard P. H., McIntyre R. E., Gallagher F., Kettunen M. I., Lewis D. Y., Brindle K., et al. (2011). Disruption of mouse Slx4, a regulator of structure-specific nucleases, phenocopies Fanconi anemia. Nat. Genet. 43, 147–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Andrea A. D. (2010). Susceptibility pathways in Fanconi’s anemia and breast cancer. N. Engl. J. Med. 362, 1909–1919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Winter J., Joenje H. (2009). The genetic and molecular basis of Fanconi anemia. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis 668, 11–19 [DOI] [PubMed] [Google Scholar]
- Deans A. J., West S. C. (2011). DNA interstrand crosslink repair and cancer. Nat. Rev. Cancer 11, 467–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evers B., Jonkers J. (2006). Mouse models of BRCA1 and BRCA2 deficiency: past lessons, current understanding and future prospects. Oncogene 25, 5885–5897 [DOI] [PubMed] [Google Scholar]
- Fan Q., Zhang F., Barrett B., Ren K., Andreassen P. R. (2009). A role for monoubiquitinated FANCD2 at telomeres in ALT cells. Nucleic Acids Res 37, 1740–1754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco S., van de Vrugt H. J., Fernández P., Aracil M., Arwert F., Blasco M. A. (2004). Telomere dynamics in Fancg-deficient mouse and human cells. Blood 104, 3927–3935 [DOI] [PubMed] [Google Scholar]
- Freie B., Li X., Ciccone S. L., Nawa K., Cooper S., Vogelweid C., Schantz L., Haneline L. S., Orazi A., Broxmeyer H. E., et al. (2003). Fanconi anemia type C and p53 cooperate in apoptosis and tumorigenesis. Blood 102, 4146–4152 [DOI] [PubMed] [Google Scholar]
- Frese K. K., Tuveson D. A. (2007). Maximizing mouse cancer models. Nat. Rev. Cancer 7, 654–658 [DOI] [PubMed] [Google Scholar]
- Grompe M., van de Vrugt H. (2007). The Fanconi family adds a fraternal twin. Dev. Cell 12, 661–662 [DOI] [PubMed] [Google Scholar]
- Hadjur S., Ung K., Wadsworth L., Dimmick J., Rajcan-Separovic E., Scott R. W., Buchwald M., Jirik F. R. (2001). Defective hematopoiesis and hepatic steatosis in mice with combined deficiencies of the genes encoding Fancc and Cu/Zn superoxide dismutase. Blood 98, 1003–1011 [DOI] [PubMed] [Google Scholar]
- Haneline L. S., Gobbett T. A., Ramani R., Carreau M., Buchwald M., Yoder M. C., Clapp D. W. (1999). Loss of FancC function results in decreased hematopoietic stem cell repopulating ability. Blood 94, 1–8 [PubMed] [Google Scholar]
- Houghtaling S., Timmers C., Noll M., Finegold M. J., Jones S. N., Meyn M. S., Grompe M. (2003). Epithelial cancer in Fanconi anemia complementation group D2 (Fancd2) knockout mice. Genes Dev. 17, 2021–2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houghtaling S., Granville L., Akkari Y., Torimaru Y., Olson S., Finegold M., Grompe M. (2005). Heterozygosity for p53 (Trp53+/−) accelerates epithelial tumor formation in Fanconi anemia complementation group D2 (Fancd2) knockout mice. Cancer Res. 65, 85–91 [PubMed] [Google Scholar]
- Jacks T., Remington L., Williams B. O., Schmitt E. M., Halachmi S., Bronson R. T., Weinberg R. A. (1994). Tumor spectrum analysis in p53–mutant mice. Curr. Biol. 4, 1–7 [DOI] [PubMed] [Google Scholar]
- Jonkers J., Meuwissen R., van der Gulden H., Peterse H., van der Valk M., Berns A. (2001). Synergistic tumor suppressor activity of BRCA2 and p53 in a conditional mouse model for breast cancer. Nat. Genet. 29, 418–425 [DOI] [PubMed] [Google Scholar]
- Koomen M., Cheng N. C., van de Vrugt H. J., Godthelp B. C., van der Valk M. A., Oostra A. B., Zdzienicka M. Z., Joenje H., Arwert F. (2002). Reduced fertility and hypersensitivity to mitomycin C characterize Fancg/Xrcc9 null mice. Hum. Mol. Genet. 11, 273–281 [DOI] [PubMed] [Google Scholar]
- Kutler D. I., Singh B., Satagopan J., Batish S. D., Berwick M., Giampietro P. F., Hanenberg H., Auerbach A. D. (2003). A 20-year perspective on the International Fanconi Anemia Registry (IFAR). Blood 101, 1249–1256 [DOI] [PubMed] [Google Scholar]
- Kuznetsov S., Pellegrini M., Shuda K., Fernandez-Capetillo O., Liu Y., Martin B. K., Burkett S., Southon E., Pati D., Tessarollo L., et al. (2007). RAD51C deficiency in mice results in early prophase I arrest in males and sister chromatid separation at metaphase II in females. J. Cell Biol. 176, 581–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langevin F., Crossan G. P., Rosado I. V., Arends M. J., Patel K. J. (2011). Fancd2 counteracts the toxic effects of naturally produced aldehydes in mice. Nature 475, 53–58 [DOI] [PubMed] [Google Scholar]
- Leteurtre F., Li X., Guardiola P., Le Roux G., Sergère J. C., Richard P., Carosella E. D., Gluckman E. (1999). Accelerated telomere shortening and telomerase activation in Fanconi’s anaemia. Br. J. Haematol. 105, 883–893 [DOI] [PubMed] [Google Scholar]
- Li X., Plett P. A., Yang Y., Hong P., Freie B., Srour E. F., Orschell C. M., Clapp D. W., Haneline L. S. (2003). Fanconi anemia type C-deficient hematopoietic stem/progenitor cells exhibit aberrant cell cycle control. Blood 102, 2081–2084 [DOI] [PubMed] [Google Scholar]
- Marek L. R., Bale A. E. (2006). Drosophila homologs of FANCD2 and FANCL function in DNA repair. DNA Repair (Amst.) 5, 1317–1326 [DOI] [PubMed] [Google Scholar]
- Marión R. M., Strati K., Li H., Murga M., Blanco R., Ortega S., Fernandez-Capetillo O., Serrano M., Blasco M. A. (2009). A p53-mediated DNA damage response limits reprogramming to ensure iPS cell genomic integrity. Nature 460, 1149–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadler J., Braun R. (2000). Fanconi anemia complementation group C is required for proliferation of murine primordial germ cells. Genesis 27, 117–123 [DOI] [PubMed] [Google Scholar]
- Navarro S., Meza N. W., Quintana-Bustamante O., Casado J. A., Jacome A., McAllister K., Puerto S., Surrallés J., Segovia J. C., Bueren J. A. (2006). Hematopoietic dysfunction in a mouse model for Fanconi anemia group D1. Mol. Ther. 14, 525–535 [DOI] [PubMed] [Google Scholar]
- Noda T., Takahashi A., Kondo N., Mori E., Okamoto N., Nakagawa Y., Ohnishi K., Zdzienicka M. Z., Thompson L. H., Helleday T., et al. (2011). Repair pathways independent of the Fanconi anemia nuclear core complex play a predominant role in mitigating formaldehyde-induced DNA damage. Biochem. Biophys. Res. Commun. 404, 206–210 [DOI] [PubMed] [Google Scholar]
- Noll M., Battaile K. P., Bateman R., Lax T. P., Rathbun K., Reifsteck C., Bagby G., Finegold M., Olson S., Grompe M. (2002). Fanconi anemia group A and C double-mutant mice: functional evidence for a multi-protein Fanconi anemia complex. Exp. Hematol. 30, 679–688 [DOI] [PubMed] [Google Scholar]
- Parmar K., D’Andrea A., Niedernhofer L. J. (2009). Mouse models of Fanconi anemia. Mutat. Res. 668, 133–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmar K., Kim J., Sykes S., Shimamura A., Stuckert P., Zhu K., Hamilton A., Deloach M., Kutok J., Akashi K., et al. (2010). Hematopoietic stem cell defects in mice with deficiency of Fancd2 or Usp1. Stem Cells 28, 1186–1195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulliam-Leath A. C., Ciccone S. L., Nalepa G., Li X., Si Y., Miravalle L., Smith D., Yuan J., Li J., Anur P., et al. (2010). Genetic disruption of both Fancc and Fancg in mice recapitulates the hematopoietic manifestations of Fanconi anemia. Blood 116, 2915–2920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantakari P., Nikkilä J., Jokela H., Ola R., Pylkäs K., Lagerbohm H., Sainio K., Poutanen M., Winqvist R. (2010). Inactivation of Palb2 gene leads to mesoderm differentiation defect and early embryonic lethality in mice. Hum. Mol. Genet. 19, 3021–3029 [DOI] [PubMed] [Google Scholar]
- Raya A., Rodríguez-Pizà I., Guenechea G., Vassena R., Navarro S., Barrero M. J., Consiglio A., Castellà M., Río P., Sleep E., et al. (2009). Disease-corrected haematopoietic progenitors from Fanconi anaemia induced pluripotent stem cells. Nature 460, 53–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reliene R., Yamamoto M. L., Rao P. N., Schiestl R. H. (2010). Genomic instability in mice is greater in Fanconi anemia caused by deficiency of Fancd2 than Fancg. Cancer Res. 70, 9703–9710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee D. B., Wang Y., Mizesko M., Zhou F., Haneline L., Liu Y. (2010). FANCC suppresses short telomere-initiated telomere sister chromatid exchange. Hum. Mol. Genet. 19, 879–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg P. S., Alter B. P., Ebell W. (2008). Cancer risks in Fanconi anemia: findings from the German Fanconi Anemia Registry. Haematologica 93, 511–517 [DOI] [PubMed] [Google Scholar]
- Saadatzadeh M. R., Bijangi-Vishehsaraei K., Kapur R., Haneline L. S. (2009). Distinct roles of stress-activated protein kinases in Fanconi anemia-type C-deficient hematopoiesis. Blood 113, 2655–2660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwacha A., Kleckner N. (1995). Identification of double Holliday junctions as intermediates in meiotic recombination. Cell 83, 783–791 [DOI] [PubMed] [Google Scholar]
- Sejas D. P., Rani R., Qiu Y., Zhang X., Fagerlie S. R., Nakano H., Williams D. A., Pang Q. (2007). Inflammatory reactive oxygen species-mediated hemopoietic suppression in Fancc-deficient mice. J. Immunol. 178, 5277–5287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh T. R., Saro D., Ali A. M., Zheng X. F., Du C. H., Killen M. W., Sachpatzidis A., Wahengbam K., Pierce A. J., Xiong Y., et al. (2010). MHF1-MHF2, a histone-fold-containing protein complex, participates in the Fanconi anemia pathway via FANCM. Mol. Cell 37, 879–886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeenk G., de Groot A. J., Romeijn R. J., van Buul P. P., Zdzienicka M. Z., Mullenders L. H., Pastink A., Godthelp B. C. (2010). Rad51C is essential for embryonic development and haploinsufficiency causes increased DNA damage sensitivity and genomic instability. Mutat. Res. 689, 50–58 [DOI] [PubMed] [Google Scholar]
- Spardy N., Duensing A., Hoskins E. E., Wells S. I., Duensing S. (2008). HPV-16 E7 reveals a link between DNA replication stress, fanconi anemia D2 protein, and alternative lengthening of telomere-associated promyelocytic leukemia bodies. Cancer Res. 68, 9954–9963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoepker C., Hain K., Schuster B., Hilhorst-Hofstee Y., Rooimans M. A., Steltenpool J., Oostra A. B., Eirich K., Korthof E. T., Nieuwint A. W., et al. (2011). SLX4, a coordinator of structure-specific endonucleases, is mutated in a new Fanconi anemia subtype. Nat. Genet. 43, 138–141 [DOI] [PubMed] [Google Scholar]
- Svendsen J. M., Harper J. W. (2010). GEN1/Yen1 and the SLX4 complex: Solutions to the problem of Holliday junction resolution. Genes Dev. 24, 521–536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taniguchi T., Garcia-Higuera I., Xu B., Andreassen P. R., Gregory R. C., Kim S. T., Lane W. S., Kastan M. B., D’Andrea A. D. (2002). Convergence of the fanconi anemia and ataxia telangiectasia signaling pathways. Cell 109, 459–472 [DOI] [PubMed] [Google Scholar]
- Tischkowitz M. D., Hodgson S. V. (2003). Fanconi anaemia. J. Med. Genet. 40, 1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tischkowitz M., Winqvist R. (2011). Using mouse models to investigate the biological and physiological consequences of defects in the Fanconi anaemia/breast cancer DNA repair signalling pathway. J. Pathol. 224, 301–305 [DOI] [PubMed] [Google Scholar]
- Tischkowitz M., Xia B. (2010). PALB2/FANCN: recombining cancer and Fanconi anemia. Cancer Res. 70, 7353–7359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titus T. A., Selvig D. R., Qin B., Wilson C., Starks A. M., Roe B. A., Postlethwait J. H. (2006). The Fanconi anemia gene network is conserved from zebrafish to human. Gene 371, 211–223 [DOI] [PubMed] [Google Scholar]
- van de Vrugt H. J., Eaton L., Hanlon Newell A., Al-Dhalimy M., Liskay R. M., Olson S. B., Grompe M. (2009). Embryonic lethality after combined inactivation of Fancd2 and Mlh1 in mice. Cancer Res. 69, 9431–9438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Vrugt H. J., Koomen M., Bakker S., Berns M. A. D., Cheng N. C., van der Valk M. A., de Vries Y., Rooimans M. A., Oostra A. B., Hoatlin M. E., et al. (2011). Evidence for complete epistasis of null mutations in murine Fanconi anemia genes Fanca and Fancg. DNA Repair (Amst.) 10, 1252–1261 [DOI] [PubMed] [Google Scholar]
- Vaz F., Hanenberg H., Schuster B., Barker K., Wiek C., Erven V., Neveling K., Endt D., Kesterton I., Autore F., et al. (2010). Mutation of the RAD51C gene in a Fanconi anemia-like disorder. Nat. Genet. 42, 406–409 [DOI] [PubMed] [Google Scholar]
- Wechsler T., Newman S., West S. C. (2011). Aberrant chromosome morphology in human cells defective for Holliday junction resolution. Nature 471, 642–646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitney M. A., Royle G., Low M. J., Kelly M. A., Axthelm M. K., Reifsteck C., Olson S., Braun R. E., Heinrich M. C., Rathbun R. K., et al. (1996). Germ cell defects and hematopoietic hypersensitivity to gamma-interferon in mice with a targeted disruption of the Fanconi anemia C gene. Blood 88, 49–58 [PubMed] [Google Scholar]
- Willeit P., Willeit J., Mayr A., Weger S., Oberhollenzer F., Brandstätter A., Kronenberg F., Kiechl S. (2010). Telomere length and risk of incident cancer and cancer mortality. JAMA 304, 69–75 [DOI] [PubMed] [Google Scholar]
- Wong J. C., Alon N., Mckerlie C., Huang J. R., Meyn M. S., Buchwald M. (2003). Targeted disruption of exons 1 to 6 of the Fanconi Anemia group A gene leads to growth retardation, strain-specific microphthalmia, meiotic defects and primordial germ cell hypoplasia. Hum. Mol. Genet. 12, 2063–2076 [DOI] [PubMed] [Google Scholar]
- Yang Y., Kuang Y., Montes De Oca R., Hays T., Moreau L., Lu N., Seed B., D’Andrea A. D. (2001). Targeted disruption of the murine Fanconi anemia gene, Fancg/Xrcc9. Blood 98, 3435–3440 [DOI] [PubMed] [Google Scholar]
- Zhang Q. S., Eaton L., Snyder E. R., Houghtaling S., Mitchell J. B., Finegold M., Van Waes C., Grompe M. (2008). Tempol protects against oxidative damage and delays epithelial tumor onset in Fanconi anemia mice. Cancer Res. 68, 1601–1608 [DOI] [PubMed] [Google Scholar]
- Zhang Q. S., Marquez-Loza L., Eaton L., Duncan A. W., Goldman D. C., Anur P., Watanabe-Smith K., Rathbun R. K., Fleming W. H., Bagby G. C., et al. (2010). Fancd2−/− mice have hematopoietic defects that can be partially corrected by resveratrol. Blood 116, 5140–5148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhi G., Wilson J. B., Chen X., Krause D. S., Xiao Y., Jones N. J., Kupfer G. M. (2009). Fanconi anemia complementation group FANCD2 protein serine 331 phosphorylation is important for fanconi anemia pathway function and BRCA2 interaction. Cancer Res. 69, 8775–8783 [DOI] [PMC free article] [PubMed] [Google Scholar]