Abstract
The objective of this pilot study was to determine the usability of stereophotogrammetry (SP) as a non-invasive technique for obtaining linear measures and anatomical data of the torso in people with osteogenesis imperfecta (OI) in comparison to clinical observations. Ten participants were recruited from subjects enrolled in ongoing IRB-approved OI protocols at the National Institute of Child Health and Human Development (NICHD). Using a Gulick tape measure, anthropometer, and the SP system proprietary software, linear measurements of the torso were taken. In addition, the presence or absence of specific torso deformities was documented from both clinical observation and evaluation of SP images.. Measurements of torso diameter and circumference by SP demonstrated strong agreement with the manual measurements (ICC=0.995, 0.964, respectively). Substantial and statistically significant agreement was present between SP image evaluation and clinical observation for pectus carinatum (κ = 0.52±0.23) as well as thoracic scoliosis (κ = 0.72±0.12). The κ values between clinical observation and SP evaluations of other torso deformities were not significant. The strong correlations and p values determined by this study demonstrate the potential value of SP in studying persons with truncal deformities. However, the weak agreement between SP and some clinical observations suggests that further development of SP image analysis tools is required before SP can be used as a standard method of diagnosis or assessment of treatment success.
Keywords: Stereophotogrammetry, Anthropometry, Scoliosis, Osteogenesis Imperfecta
INTRODUCTION AND BACKGROUND
Stereophotogrammetry (SP) is a digital image capture system that integrates information from multiple cameras and computer processing to create three-dimensional (3D) surface images. At 50 milliseconds, SP image capture time is much shorter than magnetic resonance imaging (MRI) and computed tomography (CT) and can be used in repeated measurements without adding significant cost or the use of ionizing radiation. Using SP, images can be captured in a standing, gravity-influenced, functional position. SP has many potential benefits over other imaging modalities including providing a method to quantify rotational components of scoliosis and chest-wall deformities not available on standard scoliosis x-ray studies.
The reliability, validity, and precision of both the image capture and image analysis processes of a commercially available SP system obtained by the National Institutes of Health (NIH) Clinical Center Rehabilitation Medicine Department were recently studied in imaging simple geometric solids and a human form mannequin1. Excellent intra- and interrater reliability of the system existed for linear, surface area and volume measurements (r > 0.99, P < 0.001); no overall significant difference was found between SP and manual measurements (F = 4.23, P > 0.06). The system exhibited excellent stability in images of the mannequin over time (r > 0.99). The limit of precision (error > 5%) of the system to detect objects on the surface of the mannequin was estimated at an object size of with surface area of 23.5 cm2 and volume of 32 mL. This study and corroborative data from other research studies2–7 support the development of SP outcome measures to study deformities of the torso.
Osteogenesis imperfecta (OI) is a heritable disorder occurring in about one in 100,000 births that affects the connective tissue matrices of bones and soft tissues and ranges in severity of phenotype. Scoliosis is particularly common in OI and thoracic deformities (such as pectus excavatum and pectus carinatum) are also prevalent. Due to the structural limitations of the bone in persons with OI, such deformities cannot be treated or braced in the same ways as idiopathic scoliosis8. As research into treatment of patients with OI continues, there is a growing need for a non-invasive method of quantifying these truncal deformities and their progression over time. At present, such deformities are often monitored using x-ray or CT, both of which require ionizing radiation. Due to increased incidence of fractures, severity of disease, and, often, participation in research protocols, patients with OI are subject to repeated radiation exposure throughout their growth and development. A method of quantifying and assessing these structural deformities with reduced cost and testing time and without radiation would be highly desirable for OI patients and their families.
SP is a safe, relatively inexpensive technique with potential for research and clinical assessment of OI. It may also offer new information on the three-dimensional qualities of torso deformities in OI and other conditions. The aim of this study was to examine the system’s usability as a non-invasive technique for obtaining linear measures and anatomical data of the torso and to compare SP to current clinical examination techniques for the assessment of truncal deformities by piloting its use in subjects with OI.
Study Design
Recruitment
Participants were enrolled under an NIH Clinical Center IRB approved protocol for piloting the assessment of new methods for patient evaluation in areas including scoliosis; subject accrual for projects in this protocol is limited to ten. Participants were recruited from subjects enrolled in ongoing IRB-approved OI protocols at the National Institute of Child Health and Human Development (NICHD) in which diagnoses and types were determined by employing Silence clinical criteria9–10 and confirmed with genetic or collagen testing. Recruitment was limited to those subjects in the available pool of OI patients who were able to sit without support in order to obtain SP images. Ten subjects with OI types III or IV between the ages of 4 and 27 years (5 males and 5 females) participated in the study. Adult subjects and parents of minor subjects provided written consent to participate. Written or verbal assent was obtained from minor subjects.
Materials
Images of the trunk were obtained with 3dMDtorso, a commercially available, FDA Class I approved, Windows PC based, active SP system including proprietary hardware and software. The system employs four “pods,” each of which consists of one stroboscopic flash, one speckle pattern projector, two black and white digital cameras, and one color digital camera. The projection of the speckle pattern on the subject’s surface is captured stereoscopically by the digital cameras in each of the pods. The color cameras are used to capture the surface texture of the subject. The system uses a proprietary active image capturing technique which can acquire all required images in about 1.5 ms. The images from the four pods are combined using proprietary software based on the Tsai algorithm11–12 to produce a 360 degree 3D image of the human torso.
A Gulick anthropometric tape measure and a Lafayette Instrument Company linear anthropometer were used to take the manual chest circumference and diameter measurements, respectively.
Methods
Participants received physical examinations as part of the regular protocol-specific data collection by two of the authors (S.P. and H.C.) who are associate investigators in the NICHD OI protocols. Authors S.P., H.C., E.L., and M.P. are all clinicians. S.P. and H.C. made the clinical observations and E.L. and M. P. evaluated the stereophotogrammetry images for this pilot study. Measurements of chest diameter (with the anthropometer) and circumference (with the Gulick anthropometric tape) of the subject’s torso were taken in a sitting position at the level of the xiphoid process. The xiphoid process was also marked with a surgical marking pen by author S.P. before the manual measurements were taken. Two authors (S.P. and H.C.) identified and agreed upon the presence or absence of pelvic asymmetry, pectus carinatum and excavatum, infraxiphoid and supraxiphoid depression, abdominal and thoracic protrusion, and scoliosis (thoracic, lumbar, and/or thoracolumbar) based on accepted clinical practices. Palpation was allowed as part of the clinical observations and scoliosis was determined from palpation and observation. Only asymmetries in the frontal plane were documented.
On the same day (subsequent to the above examination), four images were taken of the subject’s torso by SP cameras set in 360 degree mode (Figure 1). The subjects wore shorts and were seated with arms elevated to 90 degrees. Using the xiphoid landmark placed at the time of the clinical examination, author A.C. used the SP system software to take linear measurements of the anterior/posterior (AP) diameter and circumference of the subjects’ torso SP images. In addition, different evaluators (authors M.P and E.L), blinded to the clinical observations of S.P. and H.C. and to each other, made individual observations directly from the 3D image. Each identified the presence or absence of pelvic symmetry, pectus carinatum and excavatum, infraxiphoid and supraxiphoid depression, abdominal and thoracic protrusion, and scoliosis (thoracic, thoracolumbar, and/or lumbar) in the frontal plane (when applicable). Clinical observers and SP image evaluators were blinded to radiographs when diagnosing scoliosis. All evaluators are experienced clinicians with greater than ten years of experience in their field.
Figure 1.
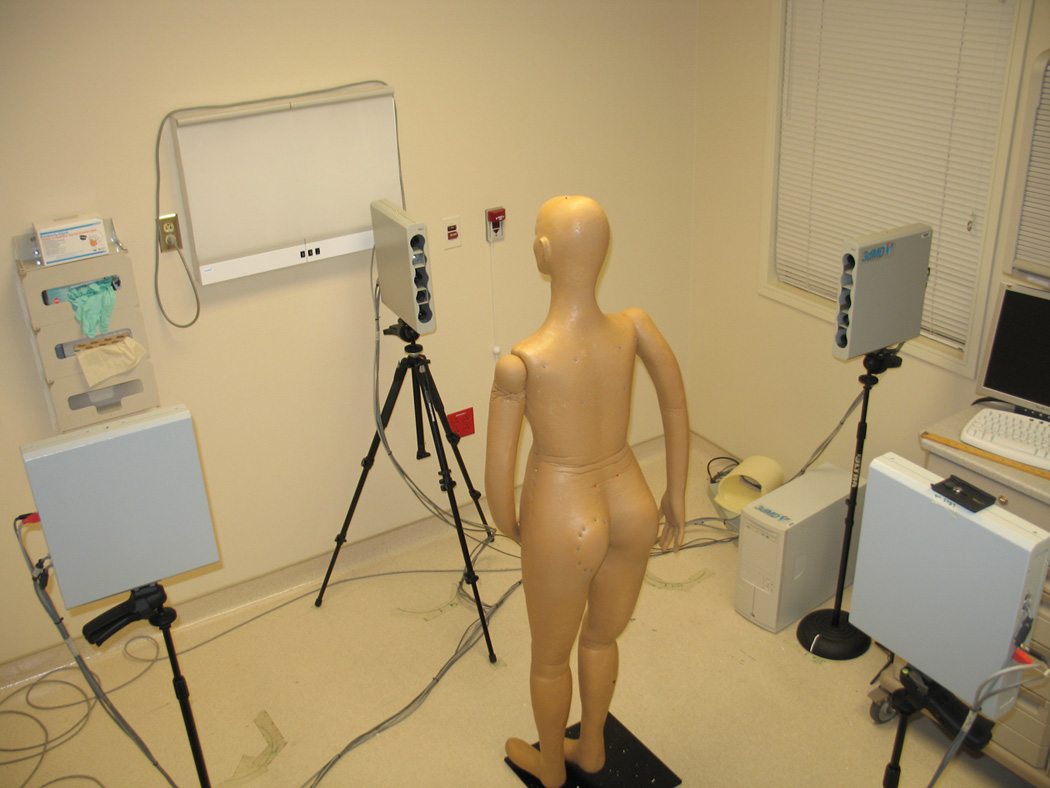
SP system in torso image capture assembly (360 degree)
Statistical Analyses
Four images of each patient’s torso were captured; average values of the data from each patient were used for statistical analyses. Intra-class correlation coefficients (ICC) were calculated to determine the inter-method agreement between manual and calculated measurements for both circumference and diameter. Paired t-tests were performed to determine if significant differences existed between the manual and SP calculated measurements. Comparison of the image evaluations to the clinical observations were performed using Cohen’s kappa (κ) correlation. Significant agreement was defined as a κ ≥ 0.40.
RESULTS
The ten patients ranged in age from 4 to 27 years, with an equal number of males and females and OI types III and IV. Images of all patients were obtained quickly, without incident or discomfort, and required no sedation for subjects as young as 4 years old. SP produced the 3D images without confining patients or exposing them to ionizing radiation. Measurements of torso diameter by SP showed very strong correlation with the manual measurement (ICC=0.9238, p<0.0001, Figure 2, Table 1). However, an average difference of 1.3 centimeters was noted between the two measures (ICC=0.001, Figure 3). In each subject, the result obtained by SP was the larger one. SP calculated torso circumference also showed strong correlation with the manual measurements (ICC=0.9458, p<0.0001 Figure 4, Table 1). Here, too, there was a difference, averaging 3.2 centimeters (p=0.022), between manual measurements and those derived by SP (Figure 3). SP derived data was greater than manual measurements in 8 of the 10 subjects.
Figure 2.
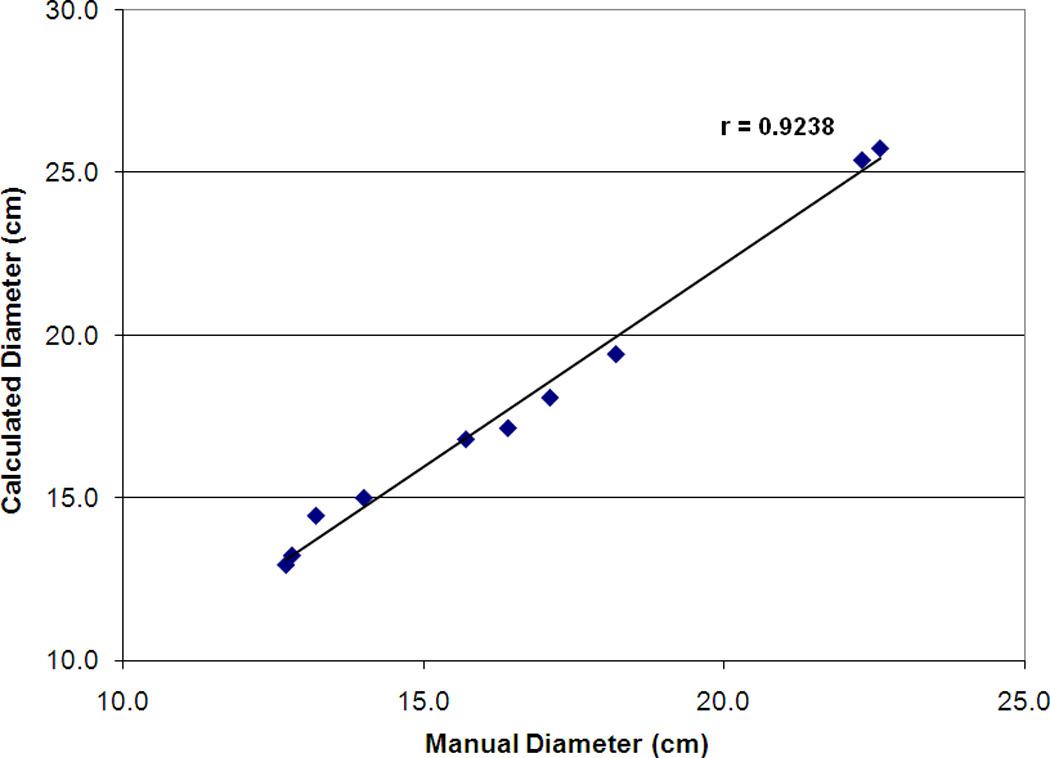
The correlation between the manual and SP measured torso diameter for the ten subjects
Table 1.
A summary of the clinical and SP measurement data and statistical analyses
| Measurements (cm) | Intra-class Correlation |
Paired t-test |
||
|---|---|---|---|---|
| Circumference | Manual | 63.9 ±16.1 (49.5–94.0) | 0.9458 (p < 0.001) | p=0.022 |
| Stereophotogrammetry | 67.1 ± 15.3 (50.9–93.4) | |||
| Diameter | Manual | 16.5 ± 3.7 (12.7–22.3) | 0.9238 (p < 0.001) | p=0.001 |
| Stereophotogrammetry | 17.8 ± 4.6 (13.0–25.8) |
Figure 3.
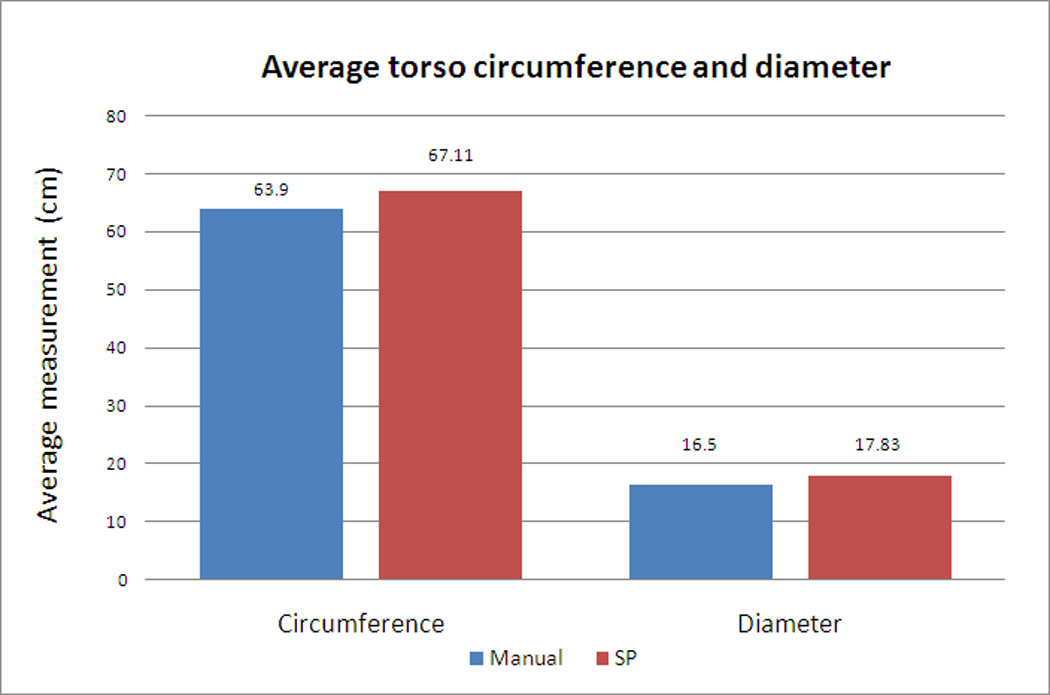
Comparison of average torso circumferences and diameters derived manually and by SP calculations
Figure 4.
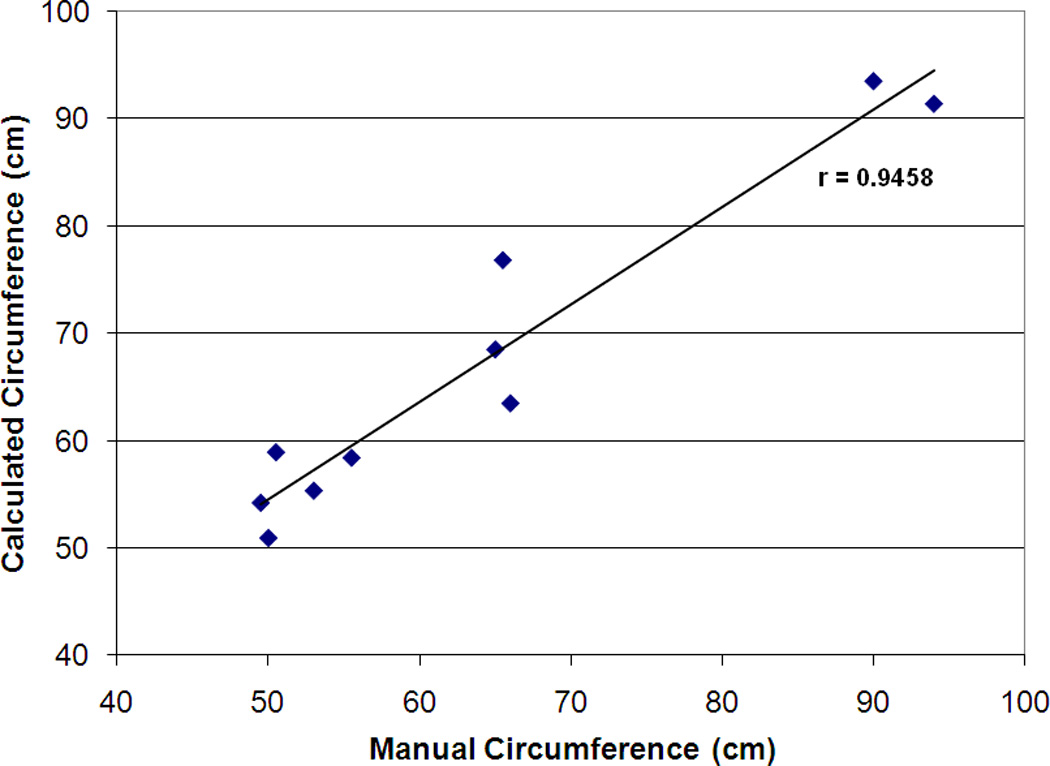
The correlation between the manual measurements and SP measured torso circumference for ten subjects
There was significant agreement between the evaluations based on SP images and those from clinical observation with regard to the presence or absence of pectus carinatum (κ = 0.52±0.23) as well as thoracic scoliosis (κ = 0.46±0.084). There was also significant agreement between the evaluators viewing the SP images for pectus excavatum (κ = 0.40±0.22), supraxiphoid depression (κ = 0.74±0.22), protruding abdomen (κ = 0.74±0.22), and thoracolumbar scoliosis (κ = 0.64±0.097). Significant agreement existed between evaluations based on SP images and those from clinical observation of thoracic scoliosis (κ = 0.72±0.12). Best overall agreement occurred between evaluators who made observations of the SP images. Limited overall agreement was present when comparing clinical observations (CO) of the evaluators to observations based on SP images (summary of values found in Table 2). Kappa values and the frequency of each finding on clinical exam are reported in Table 3.
Table 2.
Summary of observation type and kappa values
| Feature | Kappa | Agreement | CI (+/−) | |
|---|---|---|---|---|
| SP Image Evaluation Physical therapist vs. physiatrist |
Pelvis Hi | 0.00 | Slight | 0.00 |
| Pectis Carinatum | 0.00 | Slight | 0.00 | |
| Pectis Excavatum | 0.40 | Fair | 0.22 | |
| Infraxiphoid Dep. | 0.20 | Slight | 0.13 | |
| Supraxiphiod Dep. | 0.74 | Substantial | 0.22 | |
| Protuding Abdomen | 0.74 | Substantial | 0.22 | |
| Thorasic Protrusion Ant | −0.01 | Poor | 0.17 | |
| Thorasic Protrusion Pos | 0.32 | Fair | 0.13 | |
| Scoliosis Thoracic | 0.27 | Fair | 0.062 | |
| Scoliosis T-L | 0.64 | Substantial | 0.097 | |
| Scoliosis Lumbar | 0.07 | Slight | 0.087 | |
| Clinical observation vs. SP image evaluation Physical therapist |
Pelvis Hi | 0.00 | Slight | 0.00 |
| Pectis Carinatum | 0.52 | Moderate | 0.23 | |
| Pectis Excavatum | 0.09 | Slight | 0.20 | |
| Infraxiphoid Dep. | 0.02 | Slight | 0.050 | |
| Supraxiphiod Dep. | 0.00 | Slight | 0.00 | |
| Protuding Abdomen | −0.25 | Poor | 0.23 | |
| Thorasic Protrusion Ant | 0.18 | Slight | 0.14 | |
| Thorasic Protrusion Pos | 0.22 | Fair | 0.23 | |
| Scoliosis Thoracic | 0.46 | Moderate | 0.084 | |
| Scoliosis T-L | 0.14 | Slight | 0.17 | |
| Scoliosis Lumbar | 0.26 | Fair | 0.17 | |
| Clinical observation vs. SP image evaluation Physiatrist |
Pelvis Hi | 0.02 | Slight | 0.087 |
| Pectis Carinatum | 0.00 | Slight | 0.00 | |
| Pectis Excavatum | −0.40 | Poor | 0.18 | |
| Infraxiphoid Dep. | −0.20 | Poor | 0.13 | |
| Supraxiphiod Dep. | 0.00 | Slight | 0.00 | |
| Protuding Abdomen | 0.21 | Fair | 0.22 | |
| Thorasic Protrusion Ant | 0.35 | Fair | 0.20 | |
| Thorasic Protrusion Pos | 0.22 | Fair | 0.15 | |
| Scoliosis Thoracic | 0.72 | Substantial | 0.12 | |
| Scoliosis T-L | 0.27 | Fair | 0.18 | |
| Scoliosis Lumbar | 0.38 | Fair | 0.18 |
Table 3.
Kappa values between raters
| Kappa (κ) | ||||
|---|---|---|---|---|
| Finding | Frequency of finding on CO |
MD vs PT | PT vs CO | MD vs CO |
| Pelvis Hi | 7 | 0.00 | 0.00 | 0.087 |
| Pectus Carinatum | 3 | 0.00 | 0.23 | 0.00 |
| Pectus Excavatum | 2 | 0.40 | 0.20 | 0.18 |
| Infraxiphoid Dep. | 1 | 0.20 | 0.050 | 0.13 |
| Supraxiphiod Dep. | 0 | 0.74 | 0.00 | 0.00 |
| Protuding Abdomen | 2 | 0.74 | 0.23 | 0.22 |
| Thoracic Protrusion Ant | 0 | 0.42 | 0.14 | 0.20 |
| Thoracic Protrusion Pos | 2 | 0.31 | 0.23 | 0.15 |
| Scoliosis Thoracic | 4 | 0.20 | 0.084 | 0.12 |
| Scoliosis T-L | 1 | 0.20 | 0.17 | 0.18 |
| Scoliosis Lumbar | 0 | 1.0 | 0.17 | 0.18 |
MD = physiatrist as SP image evaluator
PT = physical therapist as SP image evaluator
CO = clinical observation
DISCUSSION
This study demonstrated strong, statistically significant agreement between two linear measures of the trunk obtained by direct physical measurement and SP. Although the measures were strongly correlated, the results calculated by SP were larger. The larger values derived from SP could be the result of the differences between techniques. Manual tools apply pressure to the patient, potentially creating deformation of soft tissues, whereas SP calculates the dimensions with no deformation of the image surface.
There was significant agreement between the SP raters and clinical observers only for a few of the nominal variables. Differences in agreement may be a function of the choice to place the patient in one position for SP, whereas clinical examinations could be made in a variety of positions. The presence of significant agreement in thoracic scoliosis between clinical observers and evaluations of SP images may be due to the feature’s position on the spine at the center of the SP system field of view. The absence of agreement between SP image evaluators for “pelvis high” feature is likely due to the feature’s location at the extreme end of the cameras’ field of view. Limited overall agreement for infraxiphoid depression, pectus excavatum, and supraxiphoid depression suggests difficulty resolving images with concave components, since there was better overall agreement for protruding abdomen and pectus carinatum. Differences in measurements could also be due to limits of the SP field of vision and differences between visualization of a model on a computer monitor and direct observation, which includes palpation of a patient. Discrepancies between evaluators may also be related to experience and/or professional definitions of the various findings. These results suggest that SP in its current form is not sufficiently developed for direct application (as an independent assessment) to telemedicine. However, the use of SP in conjunction with image analysis software offers potential to standardize the description of clinical features, although further research in this area is needed.
To achieve this goal, norms must first be developed using a healthy volunteer population and then compared to groups with scoliosis, sternal, or chest wall deformities. Based on the success of these studies, SP may also be directed to other clinical issues such as truncal fat distribution in obesity. Our group is beginning a clinical protocol to determine if a commercial SP system combined with computer-based analysis algorithms is capable of providing reliable, valid clinical outcome measures in scoliosis, chest deformities, and truncal obesity. We eventually plan to explore other clinical applications for SP including, but not limited to, quantifying limb edema and accurately describing diffuse skin lesions (such as those in neurofibromatosis type I or tuberous sclerosis). Results of such studies may also be used to develop algorithms to automate SP recognition of these findings for application in research and diagnostic settings.
Acknowledgments
This study was performed under the Intramural Research Program at the National Institutes of Health. The 3dMDtorso is a commercially available, FDA Class I approved, Windows PC based, active stereophotogrammetry system including proprietary hardware and software. Portions of this study were previously presented at the 2008 Annual Assembly of the American Academy of PM&R, but have never been published in complete form.
Footnotes
Disclosures:
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
All of the authors are U.S. Federal Government employees without any conflicts of interest.
REFERENCES
- 1.Paul SM, Chamberlin AP, Hatt C, Nayak AV, Danoff JV. Reliability, validity, and precision of an active stereophotogrammetry system for three-dimensional evaluation of the human torso. Med Eng Phys. 2009 Oct;:9. doi: 10.1016/j.medengphy.2009.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ajemba P, Durdle N, Hill D, Raso J. Classifying torso deformity in scoliosis using orthogonal maps of the torso. Med Biol Eng Comput. 2007 Jun;45(6):575–584. doi: 10.1007/s11517-007-0192-z. [DOI] [PubMed] [Google Scholar]
- 3.Ajemba PO, Durdle NG, James Raso V. Clinical monitoring of torso deformities in scoliosis using structured splines models. Med Biol Eng Comput. 2008 Dec;46(12):1201–1208. doi: 10.1007/s11517-008-0399-7. [DOI] [PubMed] [Google Scholar]
- 4.Ajemba PO, Durdle NG, Hill DL, Raso VJ. Validating an imaging and analysis system for assessing torso deformities. Comput Biol Med. 2008 Mar;38(3):294–303. doi: 10.1016/j.compbiomed.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Jaremko JL, Poncet P, Ronsky J, Harder J, Dansereau J, Labelle H, Zernicke RF. Estimation of spinal deformity in scoliosis from torso surface cross sections. Spine (Phila Pa 1976) 2001 Jul 15;26(14):1583–1591. doi: 10.1097/00007632-200107150-00017. [DOI] [PubMed] [Google Scholar]
- 6.Jaremko JL, Poncet P, Ronsky J, Harder J, Dansereau J, Labelle H, Zernicke RF. Indices of torso asymmetry related to spinal deformity in scoliosis. Clin Biomech (Bristol, Avon) 2002 Oct;17(8):559–568. doi: 10.1016/s0268-0033(02)00099-2. [DOI] [PubMed] [Google Scholar]
- 7.Kumar A, Ajemba P, Durdle N, Raso J. Pre-processing range data for the analysis of torso shape and symmetry of scoliosis patients. Stud Health Technol Inform. 2006;123:483–487. [PubMed] [Google Scholar]
- 8.Basel D, Steiner RD. Osteogenesis imperfecta: recent findings shed new light on this once well-understood condition. Genet Med. 2009 Jun;11(6):375–385. doi: 10.1097/GIM.0b013e3181a1ff7b. [DOI] [PubMed] [Google Scholar]
- 9.Sillence D, Barlow K, Garber A, Hall J, Rimoin D. Osteogenesis imperfecta type II delineation of the phenotype with reference to genetic heterogeneity. Am J Med Genet. 1984;(17):407–423. doi: 10.1002/ajmg.1320170204. [DOI] [PubMed] [Google Scholar]
- 10.Sillence D, Senn A, Danks D. Genetic heterogeneity in osteogenesis imperfect. J Med Genet. 1979;(16):101–116. doi: 10.1136/jmg.16.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai RY. An efficient and accurate camera calibration technique for 3D machine vision. Proceedings of IEEE Conference on Computer Vision and Pattern Recognition; Miami Beach FL. 1986. pp. 364–374. [Google Scholar]
- 12.Tsai RY. A versatile camera calibration technique for high-accuracy 3D machine vision metrology using off-the-shelf TV cameras and lenses. IEEE Journal of Robotics and Automation. 1987 Aug;3(4):323–344. [Google Scholar]


