Abstract
Objectives
As osteoporotic fractures are becoming a major health care problem in countries characterized by an increasing number of older adults, in this study we aimed to compare the incidence and costs of hip fragility fractures in Italian elderly people versus those of major cardiovascular diseases (strokes and acute myocardial infarctions [AMI]) occurring in the whole adult population.
Methods
We analyzed hospitalization records maintained at the national level by the Italian Ministry of Health for the diagnosis of hip fractures (ICD-9-CM codes 820–821), AMI (code 410), hemorrhagic (codes 430, 431, 432) and ischemic strokes (codes 433–434), and TIA (code 435) between 2001–2005. Cost analyses were based on diagnosis-related groups.
Results
The incidence of hip fractures in elderly people has increased (+12.9% between 2001 and 2005), as well as that of AMI (+20.2%) and strokes (hemorrhagic: +9.6%; ischemic: +14.7) occurring in the whole adult population; conversely, hospitalization due to TIA decreased by a rate of 13.6% between 2001 and 2005. In 2005, the hospital costs across the national health care system that were associated with hip fragility fractures in the elderly were comparable to those of strokes (both hemorrhagic and ischemic), which occurred in the whole Italian adult population. Moreover, these costs were higher than those generated by AMI and TIA. Rehabilitation costs following strokes reached about 3 billion Euros in 2005, but rehabilitative costs of hip fractures and AMI were comparable (about 530 million Euros in 2005).
Conclusion
The burden of hip fragility fractures in Italy is comparable to that of AMI and strokes.
Keywords: hip fractures, strokes, acute myocardial infarction, incidence, hospital costs, rehabilitation costs
Introduction
Demographic trends from the last 50 years have indicated an increased life expectancy in developed countries. Among those countries, Italy has one of the highest life expectancies, which has increased up to 77.9 years for men and 87.4 years for women in 2010.1–3 For these reasons, Italy represents an interesting international case study about the effects of aging on chronic, degenerative illnesses such as hip fractures, cardiovascular diseases (CVD), and cerebrovascular accidents (CVA), which currently pose major health care challenges in many countries. Both acute myocardial infarctions (AMI) and strokes are known to be a relevant cause of morbidity, mortality, and disability, with their incidence progressively increasing in the oldest age groups.4–16 CVD are the primary causes of morbidity and mortality in Italy,2 with AMI representing a leading cause of hospitalizations and health care costs, as shown by our previous research.17
CVA, including transient ischemic attacks (TIA), as well as ischemic and hemorrhagic strokes, represent the second most prevalent causes of mortality worldwide,4,5 and are considered to be the main cause of disability in the elderly.6–8 One-third of patients experiencing a stroke show high levels of disability after 1 year.9,10 About 7%–12% of patients who experienced a previous TIA will experience an ischemic stroke within 1 year (with an additional 4%–7% of patients experiencing strokes after 5 years from the initial TIA).10,18 AMI and strokes are associated with a 15%–25%11–16 and 30%–60%9 1-year mortality rate, respectively. The risk of recurrence is remarkable for strokes.9 The Italian Longitudinal Study on Aging (ILSA) has estimated an annual incidence of 196,000 strokes, of which 20% represent relapsing episodes.19
On the other hand, hip fractures in the elderly Italian population are progressively increasing, with a 15%–25% 1-year mortality rate,20,21 and a high risk of disability.22–25 In Italy, about 18,000 elderly people per year become completely disabled as a consequence of hip fractures.2 For these reasons, the World Health Organization considers osteoporosis and osteoporotic fractures to be as critical a health problem as AMI and strokes.3 In our previous research, we have shown how the incidence and costs of hip fractures are comparable to those of AMI.26 As osteoporotic fractures are becoming a major health care problem in countries characterized by an increasing number of older adults, in this study we aimed to compare the incidence and costs of hip fragility fractures suffered by elderly people in Italy versus major cardiovascular events (strokes and AMI) occurring in the whole adult population.
Materials and methods
Hospitalizations
Information concerning all hospitalizations that have occurred in Italy is registered in hospital discharge records maintained at the Italian Ministry of Health. This information is anonymous and includes patients’ age, diagnosis, procedures performed, and length of hospital stay. In the present study we have analyzed the number of hospitalizations occurring in Italy because of hip fractures, AMI, and strokes, considering also the direct costs related to hospitalization and rehabilitation. As these were observational analyses of anonymous numerical data, no approval from an ethical committee was required.27 We focused on the hospitalization data available for consultations, which corresponded with the period from 2001 to 2005.
Some data concerning hip fractures and AMI partially overlapped with those presented in our previous studies about these topics (from the years 2001 to 2005, both for hip fractures and AMI), with the number of hospitalizations and their associated costs being consistent with some previously published figures.17,28–30 Hip fractures were defined by the following ICD-9-CM diagnosis codes for major diagnosis: 820.0–820.1 (femoral neck fractures); 820.2–820.3 (pertrochanteric femoral fractures); and 820.8, 820.9, and 821.1 (other femoral fractures). Given that we intended to assess the burden of femoral fragility fractures, we excluded patients aged 45 to 64 from the analysis of hip fractures, which represented no more than 8% of all hip fractures. Strokes were defined by ICD-9-CM diagnosis codes 430, 431, 432 (hemorrhagic strokes); 433 and 434 (ischemic strokes); and 435 (TIA). AMI was defined by the ICD-9-CM diagnosis code 410 (all extensions). We have only included patients with a primary diagnosis of AMI.
Population data were obtained from the Italian Institute for Statistics for 2001–2005.1 All data were stratified by sex and age groups (45–64, 65–74, and ≥75 years; in the analysis of hip fractures, the youngest age group was not included as these fractures were not likely to be a consequence of osteoporosis), and were processed by using Stata (StataCorp, College Station, TX) and Excel (Microsoft Corporation, Redmond, WA) software programs. Descriptive statistical analyses were performed in order to calculate the incidence of each condition in each sex and age subgroup across the 5 examined years.
Cost analyses
The analysis of direct costs was based on diagnosis-related groups (DRGs), which were considered to be a proxy for computing hospitalization costs. Ministerial Decree DM 549/1997 defined the national DRG rate list that was adopted during the 5 years examined in our study. Italian regions are allowed to reduce these rates locally, by an average rate of 15%. For this reason, in our analysis we used the 1997 DRG rates reduced by 15%, in order to be more conservative.
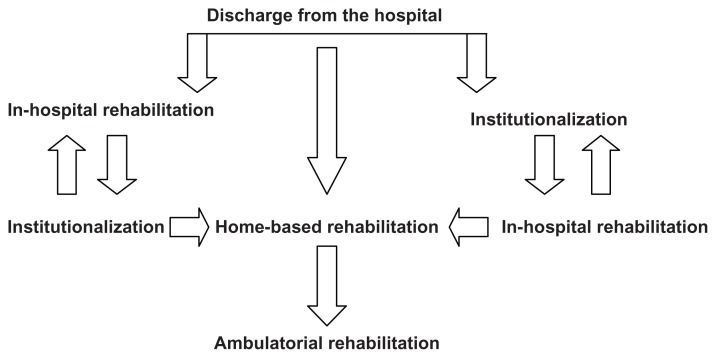
As was the case in our previous research,26,28–30 the DRGs that were considered relevant to hip fractures were: 209 (surgical procedures on major joints and hip replacement), 210–211 (hip and femur surgery), and 235–236 (hip, femur or pelvis fractures). Since not all patients that were assigned these DRGs had a main diagnosis of hip fracture (actually, osteoarthritis accounts for a substantial number of hip replacements), only 30% of costs ascribed to DRG 209 and 80% of costs ascribed to DRGs 210, 211, plus 100% of costs ascribed to DRGs 235 and 236 were attributable to a main diagnosis of hip fracture.26,28–30 We considered these rates to represent the weight of hip fracture-related costs for each DRG, based on national estimations provided by the Ministry of Health, which were confirmed by specific analyses performed on the whole hospitalization database from the Tuscany region (about 4 million inhabitants), and on those of the Local Health Authorities of Lecce (about 1 million inhabitants).26,28–30 As was the case in our previous studies, we also included rehabilitation costs following hip fractures in the analysis, assuming a 5% acute mortality rate.26,28–30 Detailed figures of the rehabilitation path following hip fractures have been published previously in separate articles and are summarized in Figure 1.26,30
Figure 1.
Rehabilitative path of hip-fractured patients.
Cost analysis concerning strokes was based on DRG 14 (hemorrhagic and ischemic strokes) and DRG 15 (TIA). We have also provided an estimation of the rehabilitation costs following strokes; actually, patients experiencing a stroke may be treated as an inpatient or outpatient in order to perform specific rehabilitative interventions. According to the ministerial guidelines for rehabilitative interventions approved on May 7, 1998, patients with stroke undergo intensive rehabilitation (in hospital settings or while institutionalized immediately after hospital discharge) for the recovery of major disabilities, and require at least 3 hours of specific exercises per day for a maximum of 60 consecutive days, including both in-hospital and day hospital rehabilitative programs (code number 56, rate fixed at 250 Euros per day). Patients who complete intensive rehabilitation usually start a 6-month ambulatorial or home-based rehabilitation program in order to recover residual disabilities or to preserve their achieved progress (this corresponds to a cost of 80 Euros per day for 180 consecutive days, according to the Ministerial Decree DM May 7, 1998).
To be conservative, we assumed that only one out of five patients do not perform in-hospital intensive rehabilitation because an ambulatorial or home-based rehabilitative program for 180 days usually begins immediately (at a rate of 80 Euros per day). We have not excluded readmissions of the same patients from our analysis because – as is the case of relapsing stroke – the path of rehabilitation is repeated as described above. Conversely, when computing rehabilitation costs, we have excluded patients with TIA because these kinds of CVAs are defined as events that do not result in residual disability, and therefore they do not need rehabilitative interventions. At the same time, we have taken into account an average 20% overall acute mortality rate following stroke (patients who have not started rehabilitative programs), as reported by the ILSA.19
As we did in our previous studies when we computed direct costs due to AMI,17,26 we have included DRG 121 (CVD with AMI and cardiovascular complications, patient alive), DRG 122 (CVD with AMI without cardiovascular complications, patient alive), and DRG 123 (CVD with AMI leading to death). We also included DRGs used for surgical procedures performed following AMI (bypass and angioplasties) on the basis of regional estimations from the Lazio region, and from the Local Health Authorities of Lecce in Southern Italy, as in our previous studies.17,26 These analyses showed that 1% of surgical DRG 107 (coronary bypass) and 15% of surgical DRG 112 (angioplasty) were attributable to a main diagnosis of AMI, whereas the majority of coronary bypasses and angioplasties were matched with other ICD-9-CM diagnosis codes, but not with AMI.17,26 Hospitalization costs were evaluated for all patients (≥45 years of age), as well as for elderly patients separately (≥75 years old). We also computed the costs associated with postoperative rehabilitation following AMI, while examining the rate fixed by the Italian Rehabilitation Guidelines for intensive rehabilitation (rate classified as code n.56; ie, 250 Euros per day). According to the Italian Ministry of Health guidelines for rehabilitative activities published on May 7, 1998, the average length of rehabilitation is 21 days, including both inpatient and outpatient, or home-based rehabilitative programs. We computed only rehabilitation costs for 85% of the patients, assuming a 15% acute mortality rate following AMI.11–16
Results
As shown in Table 1, a total of 85,762 hospitalizations due to hip fractures (17,597 men and 66,674 women) were recorded in 2005 for people ≥ 65 years old (+12.9% compared to 2001). As summarized in Table 1, the majority of hospitalizations due to hip fractures occurred in patients ≥ 75 years old (n = 72,072; 15,285 men and 56,787 women; +13.6% compared to 2001), particularly among women of this age group (n = 56,787; +12.2% compared to 2001). Hospitalizations due to hip fractures in men ≥ 75 years old (n = 15,285) increased by a rate of 19.0% from 2001, thus representing the highest increase observed in the subgroup analyses. Patients ≥ 85 years old (n = 29,308; 5661 men and 23,647 women) accounted for 37% of overall fractures among members of the population ≥ 65 years old (data not presented). As shown in Table 2, hospital costs were 467 million Euros in 2005 (+25.2% compared to 2001), with rehabilitation costs reaching 532 million Euros in the same year (+27.0% compared to 2001). Pooling all data together, hospitalizations due to hip fractures in the elderly resulted in expenditures of approximately 6.8 billion Euros over the 5-year period (including both hospital and rehabilitation costs).
Table 1.
Number of hospitalizations due to hip fractures in the elderly Italian population (≥65 years old) by age group and sex (Italian Ministry of Health national hospitalization records, 2001–2005)
| Age group (years) | 2001 | 2002 | 2003 | 2004 | 2005 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| M | F | M | F | M | F | M | F | M | F | |
| 65–74 | 3619 | 9350 | 3630 | 9689 | 3560 | 9459 | 3923 | 10,010 | 3803 | 9887 |
| >75 | 12,837 | 50,604 | 13,315 | 52,639 | 14,352 | 53,916 | 14,205 | 54,157 | 15,285 | 56,787 |
| Total | 75,960 | 79,273 | 81,287 | 82,295 | 85,762 | |||||
Abbreviations: M, male; F, female.
Table 2.
Estimated direct hospital and rehabilitation costs following hip fractures occurring in people aged ≥ 65 years (Italy 2001–2005)
| Year | Hospital costs (€) | Rehabilitation costs (€) | Total costs (€) |
|---|---|---|---|
| 2001 | 373 | 419 | 792 |
| 2002 | 394 | 432 | 826 |
| 2003 | 433 | 480 | 913 |
| 2004 | 448 | 485 | 933 |
| 2005 | 467 | 532 | 999 |
Note: Values are expressed in million Euros.
The total hospitalizations for hemorrhagic and ischemic strokes (including TIA) were 187,883 in 2005 (97,941 men and 89,942 women), with a general increase of 5.1% when compared to 2001 (n = 178,703; men: 92,451; women: 86,252). This observed increase was due to a +19.4% rise in the number of ischemic and hemorrhagic strokes experienced by people ≥ 75 years old (12,198 additional hospital admissions in this age group occurred between 2001 and 2005). The total number of hospital admissions following hemorrhagic strokes was 30,263 in 2005 (men: 15,760; women: 14,503) and 27,613 in 2001 (men: 14,261; women: 13,352), showing a +9.6% increase over the 5-year period (Table 3). As shown in Table 3, the number of hospitalizations due to ischemic strokes and TIA was 109,707 (men: 59,065; women: 50,642), plus 47,913 (men: 23,116; women: 24,797) in 2005, and 95,613 (men: 51,614; women: 42,999) plus 55,477 (men: 26,576; women: 28,901) in 2001, respectively. Thus, while ischemic strokes increased by a rate of +14.7%, the number of hospitalizations that occurred as a result of TIA showed a −13.6% reduction over the 5-year period.
Table 3.
Number of hospitalizations following hemorrhagic or ischemic strokes and transient ischemic attacks, presented by age group and sex (Italian Ministry of Health national hospitalization records, 2001–2005)
| Age group (years) | 2001 | 2002 | 2003 | 2004 | 2005 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| M | F | M | F | M | F | M | F | M | F | |
| Hemorrhagic strokes | ||||||||||
| 45–64 | 4140 | 2921 | 4215 | 2931 | 3992 | 2776 | 4047 | 2728 | 4015 | 2729 |
| 65–74 | 4416 | 3233 | 4682 | 3292 | 4430 | 3147 | 4733 | 3346 | 4630 | 3346 |
| >75 | 5705 | 7198 | 6224 | 7607 | 6450 | 7829 | 6441 | 7757 | 7115 | 8428 |
| Total | 27,613 | 28,951 | 28,624 | 29,052 | 30,263 | |||||
| Ischemic strokes | ||||||||||
| 45–64 | 10,719 | 4712 | 11,317 | 5176 | 11,398 | 5050 | 12,032 | 5431 | 12,085 | 5463 |
| 65–74 | 19,064 | 11,058 | 19,434 | 11,798 | 19,857 | 11,656 | 20,927 | 12,244 | 20,482 | 12,059 |
| >75 | 21,831 | 28,229 | 24,186 | 30,939 | 25,415 | 32,344 | 25,298 | 31,905 | 26,498 | 33,120 |
| Total | 95,613 | 102,850 | 105,720 | 107,837 | 109,707 | |||||
| Transient ischemic attacks | ||||||||||
| 45–64 | 5690 | 3539 | 5394 | 3549 | 4901 | 3113 | 5038 | 3183 | 4489 | 2929 |
| 65–74 | 8060 | 6462 | 8029 | 6257 | 7367 | 5837 | 7157 | 5696 | 6876 | 5235 |
| >75 | 12,826 | 18,900 | 12,969 | 18,503 | 12,274 | 17,851 | 11,684 | 16,996 | 11,751 | 16,633 |
| Total | 55,477 | 54,701 | 51,343 | 49,754 | 47,913 | |||||
Abbreviations: M, male; F, female.
When looking at the data by age group, the number of hospital admissions following TIA decreased in both younger and older patients, while there was a significant increase in patients over 75 years old with respect to both hemorrhagic and ischemic strokes. In 2005, the last year examined, among the subgroup of patients aged 45–64 years old, 20,589 men and 11,121 women (total: 31,710) were hospitalized following hemorrhagic or ischemic strokes (including TIA). In people aged 65–74, 31,988 hospital admissions among men and 20,640 hospitalizations among women were registered (total: 52,628), while in the oldest group (≥75) we recorded 45,364 and 58,181 hospitalizations (total: 103,545) following strokes in men and women, respectively. Men accounted for 52% of the total hospital admissions in 2005, but women ≥ 75 years old were the most represented affected population. The number of men hospitalized because of both hemorrhagic and ischemic strokes (including TIA) was always higher than women in each examined year, with the only exception being patients > 75 years old, where a higher number of hospital admissions among females versus males was always recorded both for hemorrhagic (8428 versus 7115 in 2005) and ischemic strokes (33,120 versus 26,498 in 2005), including TIA (16,633 versus 11,751 in 2005).
As shown in Table 4, the overall hospitalization costs sustained for strokes in adults ≥ 45 years of age decreased from 658 million Euros in 2001 to 640 million Euros in 2005 (−2.7%), with hemorrhagic and ischemic strokes showing an average cost per patient of 3515 Euros in 2005, and TIA generating costs of 3089 Euros per patient in the same year. Hospitalization costs totaled 3.3 billion Euros over the 5-year period, with people ≥ 75 year old accounting for about 60% of these expenditures (1.9 billion Euros). As summarized in Table 4, rehabilitation costs following strokes were estimated between 2.6 billion Euros in 2001 and about 3 billion Euros in 2005 (an increase of +13.6% over the 5 years), and rose from 1.3 billion Euros to 1.6 billion Euros (+19.3% in 5 years) when only data for patients ≥ 75 years old were examined. Total rehabilitation costs from 2001 to 2005 were estimated to be about 14 billion Euros, with people ≥ 75 years old accounting for 7.4 billion Euros. When considered together, hospitalization and rehabilitation costs reached a total of 3.6 billion Euros in 2005 alone. Rehabilitation costs per patient were estimated to be 15,733 Euros in the same year.
Table 4.
Estimated hospital and rehabilitation costs following strokes (including TIA, hemorrhagic and ischemic events) in the Italian population among those aged 45–100 years old
| Year | Overall adults ≥ 45 years old | Elderly people ≥ 65 years old | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Hospital costs | Rehabilitation costs | Total costs | Hospital costs | Rehabilitation costs | Total costs | |||
|
|
|
|||||||
| Strokes | TIA | Strokes | TIA | |||||
| 2001 | 486 | 172 | 2602 | 3260 | 285 | 94 | 1330 | 1709 |
| 2002 | 505 | 169 | 2783 | 3457 | 300 | 93 | 1456 | 1849 |
| 2003 | 506 | 159 | 2837 | 3502 | 306 | 89 | 1524 | 1919 |
| 2004 | 496 | 155 | 2891 | 3542 | 294 | 85 | 1508 | 1887 |
| 2005 | 492 | 148 | 2956 | 3596 | 299 | 84 | 1587 | 1970 |
Notes: Data concerning people aged > 65 years old are also presented separately. Values are expressed in million Euros.
Abbreviation: TIA, transient ischemic attack.
Table 5 presents the number of AMI cases that occurred in adults between 2001 and 2005. The total number of hospitalizations due to AMI among patients ≥ 45 years old were 97,913 in 2001, 106,842 in 2002, 113,315 in 2003, 116,303 in 2004, and 117,750 in 2005, showing an increase in hospitalizations of 20.3% over the 5-year period. In 2005, 75,586 men and 42,164 women were hospitalized with a primary diagnosis of AMI, with an increase of 17.2% and 26.2%, respectively, over the 5-year period. The number of patients hospitalized that were ≥65 years old constantly increased over this period, rising from 65,275 in 2001 to 82,382 in 2005, with a corresponding increase of 26.2%. In the youngest age group (45–64 years old), a total of 29,925 AMI hospitalizations in men and 6443 hospitalizations in women were recorded during 2005. In the same year, among the subgroup aged 65–74, 21,621 men and 10,145 women were hospitalized for AMI, with the number of hospitalizations among the oldest group (≥75 years old) being 24,040 and 26,576 in men and women, respectively. The increasing rates across the 5-year period among men and women were 9.4% and 22.0% in the youngest age group, 14.3% and 17.5% in people aged 65–74, and 31.8% and 36.3% in the oldest subgroup, respectively. It should be noted that among AMI patients ≥ 75 years old, the number of women hospitalized was always higher than the number of men, while almost 5000 AMI hospitalizations per year involved people under 45 years old (data not shown).
Table 5.
Number of hospitalizations following acute myocardial infarction in the Italian population aged ≥ 45 years old
| Age group (years) | 2001 | 2002 | 2003 | 2004 | 2005 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||
| M | F | M | F | M | F | M | F | M | F | |
| 45–64 | 27,359 | 5279 | 28,594 | 5673 | 29,434 | 5972 | 30,294 | 6400 | 29,925 | 6443 |
| 65–74 | 18,909 | 8637 | 20,109 | 9149 | 20,995 | 9543 | 21,476 | 10,080 | 21,621 | 10,145 |
| >75 | 18,234 | 19,495 | 20,804 | 22,513 | 22,908 | 24,463 | 22,935 | 25,118 | 24,040 | 26,576 |
| Total | 97,913 | 106,842 | 113,315 | 116,303 | 117,750 | |||||
Abbreviations: M, male; F, female.
Overall hospitalization costs incurred for AMI admissions and treatment for adults ≥ 45 years of age ranged between 305 million Euros in 2001 and 370 million Euros in 2005 (Table 6), with an average cost of 3142 Euros per patient in the latter year. Rehabilitation costs following AMI were estimated at between 437 million Euros in 2001 and 525 million Euros in 2005 (an increase of 20.1% over the 5-year period), which rose from 291 million Euros to 368 million Euros (+26.5%) from 2001 to 2005, when only data for patients ≥ 65 years old were examined.
Table 6.
Total hospitalization and rehabilitation costs due to acute myocardial infarction (2001–2005) in the overall population (≥45 years old) and among the elderly (≥65 years old)
| Year | Overall population ≥ 45 years old | Elderly ≥ 65 years old | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Hospital costs | Rehabilitation costs | Total costs | Hospital costs | Rehabilitation costs | Total costs | |
| 2001 | 305 | 437 | 742 | 195 | 291 | 486 |
| 2002 | 310 | 477 | 787 | 213 | 324 | 537 |
| 2003 | 324 | 506 | 830 | 229 | 348 | 577 |
| 2004 | 332 | 519 | 851 | 234 | 355 | 589 |
| 2005 | 370 | 525 | 895 | 274 | 368 | 642 |
Note: Values are expressed in million Euros.
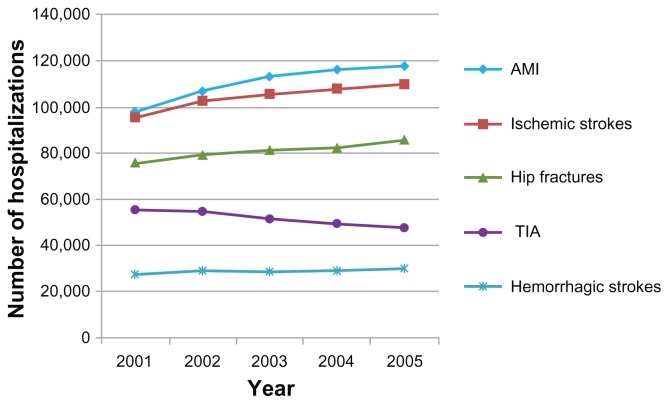
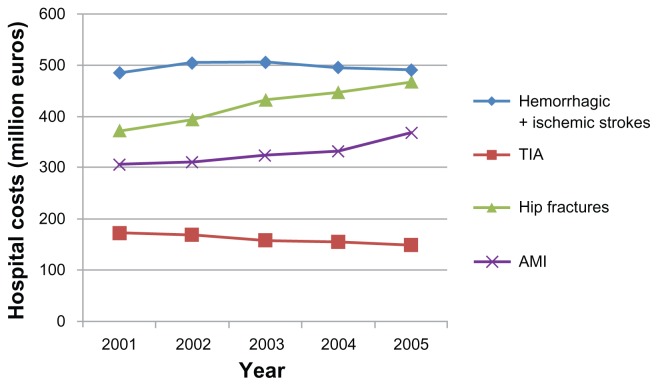
Figure 2 shows how the incidence of hip fractures among elderly people has increased between 2001 and 2005, and how the incidence of AMI and strokes occurring across the whole adult population also increased during this time; conversely, hospitalization due to TIA has decreased. Figure 3 shows that hospital costs incurred in 2005 by the national health care system for hip fragility fractures among the elderly were comparable to those associated with strokes (both hemorrhagic and ischemic), which occurred in the whole Italian adult population. These costs were higher than the costs resulting from AMI and TIA. Furthermore, rehabilitation costs following strokes reached about 3 billion Euros in 2005, but rehabilitative costs associated with hip fractures and AMI have been found to be comparable (about 530 million Euros in 2005).
Figure 2.
Number of hospitalizations following hip fractures in elderly people (>65 years old) versus strokes (both hemorrhagic and ischemic), TIA, and AMI occurring in the whole adult population (Italy 2001–2005).
Abbreviations: TIA, transient ischemic attack; AMI, acute myocardial infarction.
Figure 3.
Estimated direct hospital costs following hip fractures in elderly people (>65 years old) versus strokes (both hemorrhagic and ischemic), TIA, and AMI occurring in the whole adult population in Italy between 2001 and 2005.
Abbreviations: TIA, transient ischemic attack; AMI, acute myocardial infarction.
Discussion
This is the first study conducted that aimed to compare the incidence and costs of hip fractures in the elderly with those generated by strokes and AMI in Italy. This research is based on data from a reliable institutional database (national hospitalization records). The number of hospitalized patients with hip fractures has been presented, excluding patients who were readmitted, and specific figures have been provided regarding the oldest age groups (ie, people ≥ 75 and ≥85), where the higher prevalence of osteoporosis is acknowledged.
Our results concerning the incidence of strokes in Italy seem to be consistent with rates provided by the ILSA study group.19 The number of hospitalizations following hemorrhagic and ischemic strokes per 10,000 inhabitants has increased year over year between 2001 and 2005, with this trend being remarkable in people aged 75 years and over. Breakdown by age and sex confirmed the marked increase with age and the predominance of hospitalizations in men. Conversely, the number of hospitalizations for TIA decreased consistently over the 5-year period, possibly as an effect of medical efforts in the prevention of CVAs. However, many TIAs may go unreported (such as so-called silent strokes) in community dwelling people.31
Relevant differences (mostly due to rehabilitation costs) were found between our results and those of the Economic Longitudinal Incidence-based Project for Stroke Evaluation (EcLIPSE) study, which had previously assessed an overall cost of 11,600 Euros per patient within 6 months from hospital admission following stroke.32 Our findings concerning individual costs are higher, mostly due to a comprehensive evaluation of the rehabilitative process followed by the patients, and because the EcLIPSE study involved only 449 patients from eleven Italian hospitals.32 However, the EcLIPSE study estimated that the overall social burden of strokes in Italy costs up to 3 billion Euros per year, thus being close to the results of our analyses (3.6 billion Euros in 2005). Our estimations concerning individual costs generated by strokes in Italy (about 30,000 Euros per patient within 12 months) seem to also be consistent with findings from an international review, which considered values between 7975 USD and 54,546 USD as a reliable estimation of the annual cost per patient.33 Annual health care expenditures for each patient experiencing a stroke have been computed to be 17,800 Euros by a recent French study,34 while a multicenter study carried out in France, Germany, Sweden, and the UK reported a value of 9800 USD as being a minimum annual cost per patient.35
The main limitation of our study was represented by the fact that, for strokes, we were not able to detect readmissions of the same patients, although this did not influence the cost analysis. Actually, DRGs are entirely paid for if a person is hospitalized twice or more, and if the rehabilitation cycle is repeated for each CVA experienced by the patient. Another limit in this study is that rehabilitative paths followed by the patient may present with some regional differences.
In actuality, many people do not complete 60 days of intensive rehabilitation or 180 days of ambulatorial or home-based exercises. A cycle of extensive rehabilitation (including in-hospital, nursing home, ambulatory, or home-based rehabilitative programs) may be performed for the completion of a previous intensive rehabilitative cycle, or in the case of transient or minor functional restrictions. Extensive rehabilitation requires 1–3 hours of physical therapy per day for a maximum of 120 consecutive days (corresponding to a cost of 125 Euros per day, as defined by code n.60 in the Ministerial guidelines of May 7, 1998). After these 120 days, patients may enter home-based rehabilitation programs to recover residual disabilities or to preserve any achieved progresses. On the other hand, a proportion of patients (difficult to estimate) continue intensive rehabilitation cycles for more than 2 months per year, or they can prolong their outpatient rehabilitative program for more than 6 months. These cases, as well as the financial aids granted by the government (7500 Euros per year) for individuals with permanent disabilities following strokes, have not been considered in our cost analysis.
Sudden mortality has not been considered when computing AMI incidence,11,15 although this did not underestimate our cost analysis. The observed increase in the incidence of AMI may reflect the efficacy of the newly established emergency service (with a reduction of sudden deaths and the transfer of the same patients from a hospital to another hospital for angioplasty), but this increase could also result from the publication of new diagnostic criteria, which occurred in 2000. The very high increase of AMI cases occurring in women between 45 and 64 years old (almost double that of men in the same age group) is perhaps a consequence of new risk factors that are becoming more prevalent among younger women (ie, smoking), and highlights the need to implement preventive strategies among women in this younger age group. A complete evaluation of AMI consequences would also require the analysis of data concerning postacute phase costs (pharmacological treatments and long-term follow-up), as well as indirect costs, which represent an issue that is very difficult to assess. Some authors have suggested that these latter costs may have a high economic impact.36–40
Conclusion
The results of our study confirm the extremely high burden of hip fractures in Italy, which is actually comparable to that of strokes and higher than that of AMI, both in terms of hospitalizations and health care expenditures.
Footnotes
Disclosure
The authors report no conflicts of interest in this work. Disclosures concerning the past 5 years include: PP has received grants for consulting/speaking by Sanofi-Aventis, Amgen-Dompè, Servier, and Eli-Lilly. AM, MG, AM, AB, RG, RDB, LR, CG, FG, MLB, LM, DD, and GI have received research grants and funding for consulting/speaking by Merck, Sanofi-Aventis, Novartis, Stroder, Servier, Ely Lilly, Roche, Nicomed, and Amgen Dompè. AA, GC, CN, GM, MS, DD, MB, VM, SM, MG report no conflicts of interest.
References
- 1.Istat.it [webpage on the Internet]. [Annual Italian statistics 2010] Rome: Istituto nazionale di statistica; [Accessed November 14, 2012]. Available from: http://www3.istat.it/salastampa/comunicati/non_calendario/20101119_00/ Italian. [Google Scholar]
- 2.Italian Senate Health Commission, editor. Official Report of the Survey on Osteoporosis. Rome, Italy: Italian Senate; 2002. [Google Scholar]
- 3.WHO Life tables for WHO Member States [webpage on the Internet] Health statistics and health information systems. Geneva: World Health Organization; 2012. [Accessed September 22, 2012]. Available from: http://www.who.int/healthinfo/statistics/mortality_life_tables/en/ [Google Scholar]
- 4.Sarti C, Rastenyte D, Cepaitis Z, Tuomilehto J. International trends in mortality from stroke, 1968 to 1994. Stroke. 2000;31(7):1588–1601. doi: 10.1161/01.str.31.7.1588. [DOI] [PubMed] [Google Scholar]
- 5.Strong K, Mathers C, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366(9496):1578–1582. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 6.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2(1):43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 7.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors. Global Burden of Disease Study. Lancet. 1997;349(9063):1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 8.Marini C, Baldassarre M, Russo T, et al. Burden of first-ever ischemic stroke in the oldest old. Evidence from a population-based study. Neurology. 2004;62(1):77–81. doi: 10.1212/01.wnl.0000101461.61501.65. [DOI] [PubMed] [Google Scholar]
- 9.Dennis MS, Burn JP, Sandercock PA, Bamford JM, Wade DT, Warlow CP. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke. 1993;24(6):796–800. doi: 10.1161/01.str.24.6.796. [DOI] [PubMed] [Google Scholar]
- 10.SPREAD Live [webpage on the Internet] San Giovanni: Pierrel Research Italy; [Accessed February 9, 2012]. Available from: http://www.spread.it. Italian. [Google Scholar]
- 11.Herlitz J, Karlson BW, Hjalmarson A. Mortality and morbidity during one year of follow-up in suspected acute myocardial infarction in relation to early diagnosis: experiences from the MIAMI trial. J Intern Med. 1990;228(2):125–131. doi: 10.1111/j.1365-2796.1990.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 12.Dickstein K, Snappin S. Prediction of morbidity and mortality following myocardial infarction. J Am Coll Cardiol. 2002;39(s1):194. [Google Scholar]
- 13.Elizari MV, Martinez JM, Belziti C, et al. Morbidity and mortality following early administration of amiodarone in acute myocardial infarction. Eur Heart J. 2000;21(3):198–205. doi: 10.1053/euhj.1999.1687. [DOI] [PubMed] [Google Scholar]
- 14.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Gender-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341(4):217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 15.Tu JV, Brien SE, Kennedy CC, Pilote L, Ghali WA for Canadian Cardiovascular Outcomes Research Team. Introduction to the Canadian Cardiovascular Outcomes Research Team’s (CCORT) Canadian Cardiovascular Atlas project. Can J Cardiol. 2003;19(3):225–229. [PubMed] [Google Scholar]
- 16.Thom T, Haase N, Rosamond W, et al. for American Heart Association Statistics Committee and Strokes Statistics Subcommittee. Heart disease and stroke statistics – 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113(6):e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 17.Piscitelli P, Iolascon G, Greco M, et al. The occurrence of acute myocardial infarction in Italy: a five-year analysis of hospital discharge records. Aging Clin Exp Res. 2011;23(1):49–54. doi: 10.1007/BF03337744. [DOI] [PubMed] [Google Scholar]
- 18.Warlow CP, Dennis MS, van Gijn J, et al. Stroke: A Practical Guide to Management. 2nd ed. Oxford, UK: Blackwell Science Ltd; 2001. [Google Scholar]
- 19.Di Carlo A, Baldereschi M, Gandolfo C, et al. for ILSA Working Group. Stroke in an elderly population: incidence and impact on survival and daily function. The Italian Longitudinal Study on Aging. Cerebrovasc Dis. 2003;16(2):141–150. doi: 10.1159/000070594. [DOI] [PubMed] [Google Scholar]
- 20.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ. 1993;307(6914):1248–1250. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer HE, Tverdal A, Falch JA, Pedersen JI. Factors associated with mortality after hip fracture. Osteoporos Int. 2000;11(3):228–232. doi: 10.1007/s001980050285. [DOI] [PubMed] [Google Scholar]
- 22.Hagsten B, Svensson O, Gardulf A. Health-related quality of life and self-reported ability concerning ADL and IADL after hip fracture: a randomized trial. Acta Orthop. 2006;77(1):114–119. doi: 10.1080/17453670610045786. [DOI] [PubMed] [Google Scholar]
- 23.Di Monaco M, Vallero F, Di Monaco R, Tappero R, Cavanna A. Muscle mass and functional recovery in women with hip fracture. Am J Phys Med Rehabil. 2006;85(3):209–215. doi: 10.1097/01.phm.0000200387.01559.c0. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerman S, Hawkes WG, Hebel JR, Fox KM, Lydick E, Magaziner J. The Lower Extremity Gain Scale: a performance-based measure to assess recovery after hip fracture. Arch Phys Med Rehabil. 2006;87(3):430–436. doi: 10.1016/j.apmr.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 25.Latham NK, Jette DU, Warren RL, Wirtalla C. Pattern of functional change during rehabilitation of patients with hip fracture. Arch Phys Med Rehabil. 2006;87(1):111–116. doi: 10.1016/j.apmr.2005.08.121. [DOI] [PubMed] [Google Scholar]
- 26.Piscitelli P, Iolascon G, Gimigliano F, et al. for SIOMMMS study group, CERSUM research group. Incidence and costs of hip fractures compared to acute myocardial infarction in the Italian population: a 4-year survey. Osteoporos Int. 2007;18(2):211–219. doi: 10.1007/s00198-006-0224-9. [DOI] [PubMed] [Google Scholar]
- 27.Piscitelli P, Santoriello A, Buonaguro FM, et al. for CROM, Human Health Foundation Study Group. Incidence of breast cancer in Italy: mastectomies and quadrantectomies performed between 2000 and 2005. J Exp Clin Cancer Res. 2009;28:86. doi: 10.1186/1756-9966-28-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tarantino U, Capone A, Planta M, et al. The incidence of hip, forearm, humeral, ankle, and vertebral fragility fractures in Italy: results from a 3-year multicenter study. Arthritis Res Ther. 2010;12(6):R226. doi: 10.1186/ar3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Piscitelli P, Camboa P, Fitto F, Iolascon G, Guida G. Femoral fractures and orthopaedic surgery: a 4-year survey in Italy. J Orthopaed Traumatol. 2005;6:203–206. [Google Scholar]
- 30.Piscitelli P, Gimigliano F, Gatto S, et al. Hip fractures in Italy: 2000–2005 extension study. Osteoporos Int. 2010;21(8):1323–1330. doi: 10.1007/s00198-009-1084-x. [DOI] [PubMed] [Google Scholar]
- 31.Gorelick PB. The burden and management of TIA and stroke in government-funded healthcare programs. Am J Manag Care. 2009;15(Suppl 6):S177–S184. [PubMed] [Google Scholar]
- 32.Gerzeli S, Tarricone R, Zolo P, Colangelo I, Busca MR, Gandolfo C. The economic burden of stroke in Italy. The EcLIPSE Study: Economic Longitudinal Incidence-based Project for Stroke Evaluation. Neurol Sci. 2005;26(2):72–80. doi: 10.1007/s10072-005-0439-0. [DOI] [PubMed] [Google Scholar]
- 33.Payne KA, Huybrechts KF, Caro JJ, Craig Green TJ, Klittich WS. Long term cost-of-illness in stroke: an international review. Pharmacoeconomics. 2002;20(12):813–825. doi: 10.2165/00019053-200220120-00002. [DOI] [PubMed] [Google Scholar]
- 34.Spieler JF, Lanoë JL, Amarenco P. Costs of stroke care according to handicap levels and stroke subtypes. Cerebrovasc Dis. 2004;17(2–3):134–142. doi: 10.1159/000075782. [DOI] [PubMed] [Google Scholar]
- 35.Caro JJ, Huybrechts KF, Duchesne I. Management patterns and costs of acute ischemic stroke: an international study. For the Stroke Economic Analysis Group. Stroke. 2000;31(3):582–590. doi: 10.1161/01.str.31.3.582. [DOI] [PubMed] [Google Scholar]
- 36.Jönsson B, Buxton M, Kahan T, Poulter NR, Svarvar P for Anglo- Scandinavian Cardiac Outcomes Trial, Health Economic Working Group. The effects of cardiac events on quality of life and indirect costs. J Hum Hypertens. 2001;15(Suppl 1):S91–S93. doi: 10.1038/sj.jhh.1001214. [DOI] [PubMed] [Google Scholar]
- 37.Etemad LR, McCollam PL. Total first-year costs of acute coronary syndrome in a managed care setting. J Manag Care Pharm. 2005;11(4):300–306. doi: 10.18553/jmcp.2005.11.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zethraeus N, Molin T, Henriksson P, Jönsson B. Costs of coronary heart disease and stroke: the case of Sweden. J Intern Med. 1999;246(2):151–159. doi: 10.1046/j.1365-2796.1999.00546.x. [DOI] [PubMed] [Google Scholar]
- 39.Eisenstein EL, Shaw LK, Anstrom KJ, et al. Assessing the clinical and economic burden of coronary artery disease: 1986–1998. Med Care. 2001;39(8):824–835. doi: 10.1097/00005650-200108000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Turpie AG. Burden of disease: medical and economic impact of acute coronary syndromes. Am J Manag Care. 2006;12(Suppl 16):S430–S434. [PubMed] [Google Scholar]