Summary
Aortic valve calcification (AVC) is a common disease of the elderly. It is a progressive disease ranging from mild valve thickening to severe calcification with aortic valve stenosis. Risk factors for AVC are similar to those for atherosclerosis: age, gender, hypercholesterolemia, diabetes, hypertension, smoking and renal failure. AVC shares many similarities to atherosclerosis, including inflammatory cells and calcium deposits, and correlates with coronary plaque burden. Presence of AVC is associated with increased risk of adverse cardiovascular events. The objective for this review is to discuss the clinical features, natural history and prognostic significance of aortic valve calcifications, including mechanical and hemodynamic factors of flow distribution.
Keywords: aortic valve calcification, multi-slice computed tomography, coronary calcium score, atherosclerosis
Aortic Stenosis
Aortic stenosis (AS) is the most frequent valvular disease in adults [1,2]. After hypertension and coronary artery disease, it is the third most common cause of myocardial damage. Prevalence of clinically relevant aortic stenosis in people over 65 years old is about 2% and increases with age [3]. After the age of 75 years the proportion raises to 3% and to 4% after the age of 80 [4]. Since rheumatic fever is now sporadic, atherosclerosis is considered the most common cause of aortic valve sclerosis (AVS). Fortunately, AVS progression to hemodynamically relevant stenosis is rare [4–6]. A population study on 2 000 patients showed that only 16% of AVS cases progress to AS and severe stenosis develops in only 2.5% of patients [6]. Despite the seemingly small percentage of cases of severe AS development, considering the prevalence of AVS, particularly in the elderly, and increasing lifespan, we must expect the problem to grow. Currently, about 50 thousand aortic valve replacement surgeries take place in Europe and the United States and a large proportion of patients require simultaneous coronary artery bypass grafting [7]. Transcatheter Aortic Valve Implantation (TAVI) is the alternative in people with high operative risk. Such patients often require prior revascularization through coronary intervention involving angioplasty and stent implantation.
Risk Factors for Progression of Aortic Valve Sclerosis to Hemodynamically Relevant Stenosis
It is estimated that valve area decreases yearly by about 0.1 cm2 in people with mild aortic stenosis progressing to AS [8,9]. Flow rate increases during that time by about 0.3 m/s, which corresponds to an increase in transvalvular gradient by about 3.4 mmHg up to 12 mmHg [8–11]. Eight years usually pass from the diagnosis of AVS to development of clinically significant stenosis. In many patients, despite features of aortic valve damage (AVS) the disease does not progress to hemodynamically relevant stenosis requiring cardiac surgry or TAVI.
Among the risk factors for AVS progression to hemodynamically relevant stenosis we include, among other things, high degree of valve calcification and presence of coronary calcifications [10,12]. Peter et al. [13] showed that we might expect quick progress of mild or moderate stenosis when the defect is accompanied by coronary artery disease. The process of valvular and coronary calcification progress simultaneously [14]. If the coronary artery calcification index in computed tomography (CCS) is >10 Agatston units, the number of valvular calcifications increases by 24.54±3.2% per year [14]. Risk factors for atherosclerosis such as: advanced age, obesity, smoking, dyslipidemia, diabetes, renal failure, including raised serum creatinine, calcium and phosphate concentrations, as well as presence of mitral ring calcifications, predispose to an increase in transvalvular gradient and a decrease in valve area [6,15], although the data from various observations regarding various risk factors are not entirely consistent [12].
Aortic Valve Sclerosis and Coronary Calcifications
Aortic valve sclerosis is more common in men than women. Leaflet thickening and risk of calcific AV damage doubles with every decade of life [4]. After the age of 65 years the percentage of people with AVS in general population reaches 29% and increases to 40% in people older than 75 years, only to reach 48% to 57% in a population above 80 years [4,12].
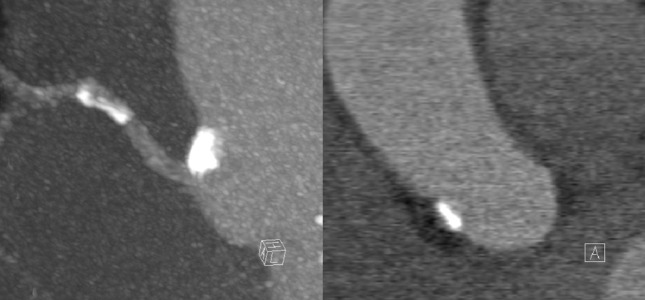
Calcific aortic sclerosis coexists with coronary artery disease in about 40% of patients. The risk of myocardial infarction is significantly larger in those patients than in case of coronary artery disease without coexisting AV damage [16]. In a population-based MESA (Multi-Ethnic Study of Atherosclerosis) study, which included people between 45 and 84 years old (mean 62 years), aortic valve calcifications (AVC) were found all together in 13% of subjects [17]. This percentage increased with the severity of coronary artery calcification. In CCS examination, for values ranging: 1–99 Agatston units, 100–399 Agatston units and 400 or more Agatston units the frequency of AVC was 14%, 25% and 38%, respectively [17]. It means, that the greater the degree of coronary artery calcification, the more likely it is to observe aortic valve calcification in computed tomography (Figure 1). In other words, identification of calcifications on the aortic valve predicts with large probability the presence of coronary lesions. Aortic valve calcification is rare in the absence of coronary artery calcifications (about 5%) and, in such cases, is a manifestation of pathologies other than atherosclerosis.
Figure 1.
Calcification of aortic valve leaflets shown in multi-slice computed tomography imaging. A fragment of coronary stent is visible in the right coronary artery (segment 2). Minute calcifications are also visible in the left anterior descending and circumflex branch. Disseminated coronary artery atherosclerosis often accompanies AVS.
Many observations suggest that aortic valve calcification is not a passive phenomenon. Endothelial cells and myofibroblasts, among other things, actively participate in it and the process itself is very similar to atherosclerotic arterial disease [18], as evidenced by endothelial dysfunction accompanying AVS and histological picture of degenerated leaflets usually containing signs of chronic inflammation and extracellular matrix calcification [19,20].
As long as 150 years ago Virchof and Rokitansky noted that vascular calcifications exhibit many similarities to osseous tissue. Newest studies corroborate that multipotential cells, such as fibroblasts and smooth muscle cells, participate in formation of calcifications due to the ability to differentiate into osteoblasts, which are involved in extracellular matrix calcification. Osteoblastic transformation of cells from the mesenchymal lineage is initiated by hemodynamic factors (oscillatory shear stress), leading to increased production of, i.a. BMP protein (Bone Morphogenic Protein), as well as by metabolic disorders accompanying renal failure and diabetes such as: hyperphosphatemia, hypercalcemia and oxidative stress [21].
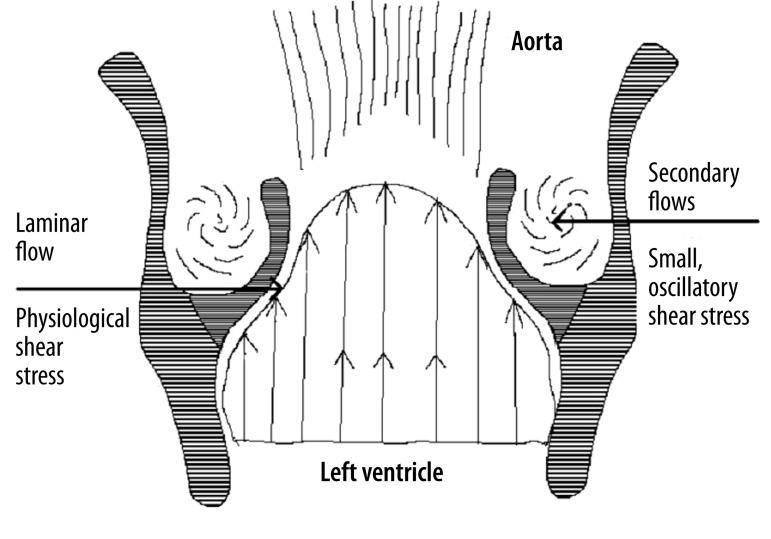
An indirect argument for common pathomechanism of AVS and atherosclerosis is such that sclerosis and subsequent calcification of aortic valve leaflets is promoted by the same classical risk factors that cause endothelial dysfunction, as well as hemodynamic factors involving formation of secondary flows, where the vessel wall is exposed to low/oscillatory shear stress [22,23]. Influence of flow-related (hemodynamic) factors on development of calcifications is evidenced by the fact, that they are formed on the aortic side of leaflets, which is exposed to turbulent flows and oscillatory shear stress, while the ventricular surface, subjected to laminar flow and physiological shear stress, is protected from atherosclerotic damage (Figures 2, 3) [24].
Figure 2.
Distribution of shear stress on aortic valve leaflets. Laminar flow and physiological shear stress on the ventricular surface of AV leaflets constitute a hemodynamic factor facilitating endothelial integrity and promoting production of anti-inflammatory agents. On the other hand, turbulent flow and resulting low, oscillatory shear stress on the aortic surface of AV leaflets and in the coronary sinus area lead to increased endothelial permeability and pro-atherogenic phenotypic transformation, including augmented matrix calcification.
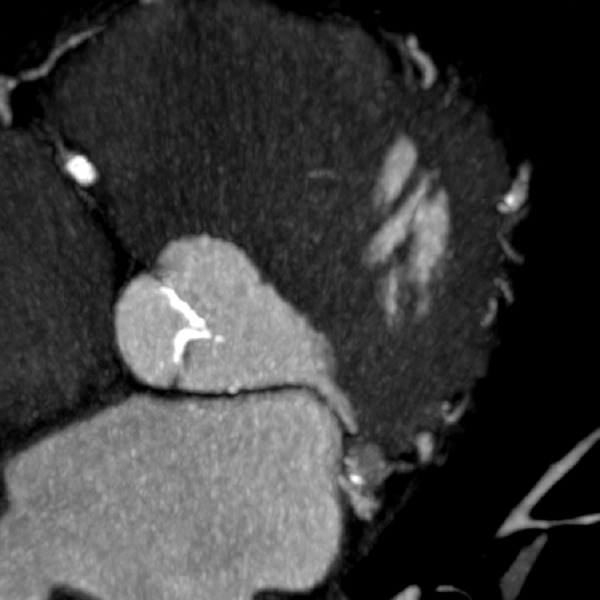
Figure 3.
Multi-slice computed tomography imaging. Atherosclerotic aortic wall calcification (right coronary sinus near the site of origin of right coronary artery). Partially calcified atherosclerotic plaque in the proximal right coronary artery.
Another example indicating the influence of hemodynamic factors on valvular damage and calcification is bicuspid valve, which is characterized by disrupted flow [25,26]. With time, almost all patients with this congenital anomaly develop more or less severe AS. However, valvular damage occurs two decades earlier in comparison to a normal, tricuspid valve. Altered flow hemodynamics contributes to aortic dilatation, which often accompanies bicuspid aortic valve.
Endothelium exhibits several mechanisms of counteracting the adverse effects of flow (low/oscillatory shear stress). However, these mechanisms become impaired in the presence of numerous risk factors that lead to endothelial dysfunction. In such case, vascular wall becomes susceptible to damage caused by disrupted flow.
Calcific aortic valve damage is an important predictor of coronary artery disease. Cumulative amount of aortic valve and mitral ring calcifications demonstrated in computed tomography or ultrasound examination correlates with CCS [27]. Pressman et al. [27] express the view that presence of AVS in echocardiography suggests high likelihood of advanced atherosclerotic lesions in epicardial arteries and should be an indication for coronary artery disease evaluation. Messika-Zeiotum et al. [12] demonstrated that the extent of coronary artery calcifications in EBCT is more pronounced in people with AVC regardless of sex and age. Respective CCS values in patients with AVC amounted to: 441±802 compared with 256±566 in people without AVC. Moreover, in the discussed study, coronary artery calcifications were more frequent in the presence of AVC.
Dyslipidemias and Aortic Valve Sclerosis
Identical risk factors facilitate calcific aortic valve damage and coronary artery disease. The reasons for both leaflet degeneration and atherosclerosis are multifactorial and not entirely known. In population studies AVS is more often accompanied by hypertension and diabetes [4,12]. Interestingly, predictive strength of particular risk factors for aortic valve damage is similar to that for coronary artery disease [28].
Several studies demonstrated a relationship between dyslipidemia, including increased concentration of serum total cholesterol and LDL fraction, reduced HDL level, and AVS [4,29,30]. However, not all studies corroborate these results. For example, the Helsinki Ageing Study[31] did not confirm dyslipidemia as a risk factor for the occurrence of aortic valve calcifications. Moderate significance of dyslipidemia for progression of aortic valve damage is evidenced by the randomized clinical studies [32,33], as well as a metaanalysis conducted on nearly 4 000 patients [34]. Studies failed to demonstrate that lipid-lowering therapy could slow down the progression of stenosis, although its use seems justified by an increased risk of acute coronary syndromes [35]. It is believed that lipid dyslipidemia may be of significance at early stages of aortic leaflet damage through deterioration of endothelial function. In case of changed transvalvular flow conditions, involving augmentation of atherogenic secondary flows, high level of holesterol no longer play an important role and disease progression is determined by abnormal hemodynamics. Mechanical damage is an important element of disease progression, analogously to atherosclerotic plaque formation. This phenomenon involves „reading” of atherogenic shear stress by the endothelium located on the aortic surfaces of valve leaflets and transforming it into biological signals (increased production of adhesion, pro-inflammatory and pro-calcification factors) [36].
Aortic Valve Sclerosis as a Prognostic Factor for Cardiovascular Events
Aortic valve sclerosis is associated with increased morbidity and mortality from cardiovascular causes. In a prospective observational study Cardiovascular Heart Study, which included 1 610 people over 65 years old, AVS was associated with a 40% increase in the risk of myocardial infarction and 50% increase in the risk of cardiovascular death [37]. Similarly to another prospective cohort study, which included 2 000 patients with AVS, the risk of cardiovascular events was almost twice as high [38]. Other studies also confirm that AVS constitutes an independent predictive factor for myocardial infarction and stroke [39].
The reason for AVS increasing the risk of cardiovascular events is not precisely known. One of the explanations may be provided by observations documenting common coexistence of AVC and coronary artery disease. Additionally, the severity of atherosclerosis is greater than when the valve remains undamaged [12,27,39,40]. Patients with AVS more frequently present with multivessel disease lub high plaque burden [41]. Also, as demonstrated by Wong et al. [42], mixed plaques, more susceptible to breaking, constitute a great proportion of lesions present in AVS patients.
Conclusions
Aortic valve calcifications are often seen in CCS examinations or coronary artery angiography performed using multi-slice computed tomography. Risk factors and causes of development of AVC and coronary calcifications are similar. Presence of classical risk factors common for atherosclerosis and AVS points to the influence of endothelial dysfunction manifesting as, i.a. decreased production of anti-atherosclerotic factors (e.g. nitric oxide). Flow conditions, including formation of secondary flows in the area where endothelium is most susceptible to disturbed flows and pro-atherogenic, low and oscillatory shear stress is another mechanism common for both disorders. Hemodynamic hemodynamic milieu, with concomitant endothelium susceptibility on “injury” caused by flow in response to an „injury” caused by flow (low and oscillatory shear stress) explains the not at random localization of lesions in the coronary arteries as well as why calcification involves aortal surfaces of AV leaflets and aortic wall calcifications occur most often in the area of coronary sinuses. Presence of AVC is an unfavorable prognostic factor for the occurrence of cardiovascular events, which should be attributed to the accompanying advanced coronary atherosclerosis, including presence of unstable plaque.
Abbreviations
- AS
Aortal Stenosis
- AV
Aortic Valve
- AVC
Aortic Valve Calcification
- AVS
Aortic Valve Sclerosis
- CCS
Coronary Calcium Score
- EBCT
Electron Beam Computed Tomography
- SPECT
Single Photon Emission Computer Tomography
- TAVI
Transcatheter Aortic-Valve Implantation.
References:
- 1.Braunwald E. Heart Disease A Textbook of Cardiovascular Medicine pod redakcją E. Braunwald, D. Zipes. 7th ed. Philadelphia: Elsevier Sanders; 2005. [Google Scholar]
- 2.Selzer A. Changing aspects of the natural history of valvular aortic stenosis. N Engl J Med. 1987;317:91–98. doi: 10.1056/NEJM198707093170206. [DOI] [PubMed] [Google Scholar]
- 3.Otto CM, Lind BK, Kitzman DW, et al. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med. 1999;341:142–47. doi: 10.1056/NEJM199907153410302. [DOI] [PubMed] [Google Scholar]
- 4.Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol. 1997;29:630–34. doi: 10.1016/s0735-1097(96)00563-3. [DOI] [PubMed] [Google Scholar]
- 5.Faggiano P, Antonini-Canterin F, Erlicher A, et al. Progression of aortic valve sclerosis to aortic stenosis. Am J Cardiol. 2003;91:99–101. doi: 10.1016/s0002-9149(02)03011-4. [DOI] [PubMed] [Google Scholar]
- 6.Cosmi JE, Kort S, Tunick PA, et al. The risk of the development of aortic stenosis in patients with “benign” aortic valve thickening. Arch Intern Med. 2002;162:2345–47. doi: 10.1001/archinte.162.20.2345. [DOI] [PubMed] [Google Scholar]
- 7.Rajamannan NM. Calcific aortic stenosis: medical and surgical management in the elderly. Curr Treat Options Cardiovasc Med. 2005;7:437–42. doi: 10.1007/s11936-005-0028-9. [DOI] [PubMed] [Google Scholar]
- 8.Rosenhek R, Binder T, Porenta G, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000;343:611–17. doi: 10.1056/NEJM200008313430903. [DOI] [PubMed] [Google Scholar]
- 9.Bellamy MF, Pellikka PA, Klarich KW, et al. Association of cholesterol levels, hydroxymethylglutaryl coenzyme-A reductase inhibitor treatment, and progression of aortic stenosis in the community. J Am Coll Cardiol. 2002;40:1723–30. doi: 10.1016/s0735-1097(02)02496-8. [DOI] [PubMed] [Google Scholar]
- 10.Davies SW, Gerschlick AH, Balcon R. Progression of valvar aortic stenosis: a long-term retrospective study. Eur Heart J. 1991;12:10–14. doi: 10.1093/oxfordjournals.eurheartj.a059815. [DOI] [PubMed] [Google Scholar]
- 11.Nitta M, Nakamura T, Hultgren HN, et al. Progression of aortic stenosis in adult men: detection by noninvasive methods. Chest. 1987;92:40–43. doi: 10.1378/chest.92.1.40. [DOI] [PubMed] [Google Scholar]
- 12.Messika-Zeitoun D, Bielak LF, Peyser PA, et al. Aortic valve calcification: determinants and progression in the population. Arterioscler Thromb Vasc Biol. 2007;27:642–48. doi: 10.1161/01.ATV.0000255952.47980.c2. [DOI] [PubMed] [Google Scholar]
- 13.Peter M, Hoffmann A, Parker C, et al. Progression of aortic stenosis. Role of age and concomitant coronary artery disease. Chest. 1993;103:1715–19. doi: 10.1378/chest.103.6.1715. [DOI] [PubMed] [Google Scholar]
- 14.Takasu J, Shavelle DM, O’Brien KD, et al. Association between progression of aortic valve calcification and coronary calcification: assessment by electron beam tomography. Acad Radiol. 2005;12:298–304. doi: 10.1016/j.acra.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 15.Perkovic V, Hunt D, Griffin SV, et al. Accelerated progression of calcific aortic stenosis in dialysis patients. Nephron Clin Pract. 2003;94:c40–45. doi: 10.1159/000071280. [DOI] [PubMed] [Google Scholar]
- 16.Cowell SJ, Newby DE, et al. Scottish Aortic Stenosis and Lipid Lowering Trial, Impact on Regression (SALTIRE) Investigators. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med. 2005;352:2389–97. doi: 10.1056/NEJMoa043876. [DOI] [PubMed] [Google Scholar]
- 17.Nasir K, Katz R, Al-Mallah M, et al. Relationship of aortic valve calcification with coronary artery calcium severity: the Multi-Ethnic Study of Atherosclerosis (MESA) J Cardiovasc Comput Tomogr. 2010;4:41–46. doi: 10.1016/j.jcct.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Mazzone A, Venneri L, Berti S. Aortic valve stenosis and coronary artery disease: pathophysiological and clinical links. J Cardiovasc Med (Hagerstown) 2007;8:983–89. doi: 10.2459/JCM.0b013e32802e6c3d. [DOI] [PubMed] [Google Scholar]
- 19.Mohler ER, Gannon F, Reynolds C, et al. Bone formation and inflammation in cardiac valves. Circulation. 2001;103:1522–28. doi: 10.1161/01.cir.103.11.1522. [DOI] [PubMed] [Google Scholar]
- 20.Rajamannan NM, Subramaniam M, Rickard D, et al. Human aortic valve calcification is associated with an osteoblast phenotype. Circulation. 2003;107:2181–84. doi: 10.1161/01.CIR.0000070591.21548.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohler ER. Mechanisms of aortic valve calcification. Am J Cardiol. 2004;94:1396–402. doi: 10.1016/j.amjcard.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 22.Agmon Y, Khandheria BK, Meissner, et al. Aortic valve sclerosis and aortic atherosclerosis: different manifestations of the same disease? Insights from a population-based study. J Am Coll Cardiol. 2001;38:827–34. doi: 10.1016/s0735-1097(01)01422-x. [DOI] [PubMed] [Google Scholar]
- 23.Wasilewski J, Kiljański T. Biomechaniczna przyczyna miażdżycy. Wydawnictwo Politechniki Łódzkiej; ŁódŸ: 2011. [in Polish] [Google Scholar]
- 24.Ge L, Sotiropoulos F. Direction and magnitude of blood flow shear stresses on the leaflets of aortic valves: is there a link with valve calcification? J Biomech Eng. 2010;132:014505. doi: 10.1115/1.4000162. [DOI] [PubMed] [Google Scholar]
- 25.Rajamannan NM. Bicuspid aortic valve disease: the role of oxidative stress in Lrp5 bone formation. Cardiovasc Pathol. 2011;20:168–76. doi: 10.1016/j.carpath.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vergara C, Viscardi F, Antiga L, et al. Influence of Bicuspid Valve Geometry on Ascending Aortic Fluid Dynamics: A Parametric Study. Artif Organs. 2012;36(4):368–78. doi: 10.1111/j.1525-1594.2011.01356.x. [DOI] [PubMed] [Google Scholar]
- 27.Pressman GS, Crudu V, Parameswaran-Chandrika A, et al. Can total cardiac calcium predict the coronary calcium score? Int J Cardiol. 2011;146:202–6. doi: 10.1016/j.ijcard.2009.06.057. [DOI] [PubMed] [Google Scholar]
- 28.Freeman RV, Otto CM. Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation. 2005;111:3316–26. doi: 10.1161/CIRCULATIONAHA.104.486738. [DOI] [PubMed] [Google Scholar]
- 29.Boon A, Cheriex E, Lodder J, et al. Cardiac valve calcification: characteristics of patients with calcification of the mitral annulus or aortic valve. Heart. 1997;78:472–74. doi: 10.1136/hrt.78.5.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aronow WS, Schwartz KS, Koenigsberg M. Correlation of serum lipids, calcium, and phosphorus, diabetes mellitus and history of systemic hypertension with presence or absence of calcified or thickened aortic cusps or root in elderly patients. Am J Cardiol. 1987;59:998–99. doi: 10.1016/0002-9149(87)91144-1. [DOI] [PubMed] [Google Scholar]
- 31.Lindroos M, Kupari M, Valvanne J, et al. Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J. 1994;15:865–70. doi: 10.1093/oxfordjournals.eurheartj.a060602. [DOI] [PubMed] [Google Scholar]
- 32.Rossebø AB, Pedersen TR, Boman K, et al. SEAS Investigators Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med. 2008;359:1343–56. doi: 10.1056/NEJMoa0804602. [DOI] [PubMed] [Google Scholar]
- 33.Chan KL, Teo K, Dumesnil JG, et al. ASTRONOMER Investigators Effect of Lipid lowering with rosuvastatin on progression of aortic stenosis: results of the aortic stenosis progression observation: measuring effects of rosuvastatin (ASTRONOMER) trial. Circulation. 2010;121:306–14. doi: 10.1161/CIRCULATIONAHA.109.900027. [DOI] [PubMed] [Google Scholar]
- 34.Parolari A, Tremoli E, Cavallotti L, et al. Do statins improve outcomes and delay the progression of non-rheumatic calcific aortic stenosis? Heart. 2011;97:523–29. doi: 10.1136/hrt.2010.215046. [DOI] [PubMed] [Google Scholar]
- 35.Shah SJ, Ristow B, Ali S, et al. Acute myocardial infarction in patients with versus without aortic valve sclerosis and effect of statin therapy (from the Heart and Soul Study) Am J Cardiol. 2007;99:1128–33. doi: 10.1016/j.amjcard.2006.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wasilewski J, Kiljański T. Miszalski-Jamka: Mechanotransdukcja – istotny mechanizm w procesie miażdżycowym. Kardiol Pol. 2011;69:717–20. [in Polish] [PubMed] [Google Scholar]
- 37.Otto CM, Lind BK, Kitzman DW, et al. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med. 1999;341:142–47. doi: 10.1056/NEJM199907153410302. [DOI] [PubMed] [Google Scholar]
- 38.Aronow WS, Ahn C, Shirani J, et al. Comparison of frequency of new coronary events in older subjects with and without valvular aortic sclerosis. Am J Cardiol. 1999;83:599–600. A8. doi: 10.1016/s0002-9149(98)00922-9. [DOI] [PubMed] [Google Scholar]
- 39.Völzke H, Haring R, Lorbeer R, et al. Heart valve sclerosis predicts all-cause and cardiovascular mortality. Atherosclerosis. 2010;209:606–10. doi: 10.1016/j.atherosclerosis.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 40.Yamamoto H, Shavelle D, Takasu J, et al. Valvular and thoracic aortic calcium as a marker of the extent and severity of angiographic coronary artery disease. Am Heart J. 2003;146:153–59. doi: 10.1016/S0002-8703(03)00105-4. [DOI] [PubMed] [Google Scholar]
- 41.Soydinc S, Davutoglu V, Dundar A, et al. Relationship between aortic valve sclerosis and the extent of coronary artery disease in patients undergoing diagnostic coronary angiography. Cardiology. 2006;106:277–82. doi: 10.1159/000093491. [DOI] [PubMed] [Google Scholar]
- 42.Wong ND, Sciammarella M, Arad Y, et al. Relation of thoracic aortic and aortic valve calcium to coronary artery calcium and risk assessment. Am J Cardiol. 2003;92:951–55. doi: 10.1016/s0002-9149(03)00976-7. [DOI] [PubMed] [Google Scholar]