Abstract
OBJECTIVE:
The social vulnerability that is associated with food allergy (FA) might predispose children with FA to bullying and harassment. This study sought to quantify the extent, methods, and correlates of bullying in a cohort of food-allergic children.
METHODS:
Patient and parent (83.6% mothers) pairs were consecutively recruited during allergy clinic visits to independently answer questionnaires. Bullying due to FA or for any cause, quality of life (QoL), and distress in both the child and parent were evaluated via questionnaires.
RESULTS:
Of 251 families who completed the surveys, 45.4% of the children and 36.3% of their parents indicated that the child had been bullied or harassed for any reason, and 31.5% of the children and 24.7% of the parents reported bullying specifically due to FA, frequently including threats with foods, primarily by classmates. Bullying was significantly associated with decreased QoL and increased distress in parents and children, independent of the reported severity of the allergy. A greater frequency of bullying was related to poorer QoL. Parents knew about the child-reported bullying in only 52.1% of the cases. Parental knowledge of bullying was associated with better QoL and less distress in the bullied children.
CONCLUSIONS:
Bullying is common in food-allergic children. It is associated with lower QoL and distress in children and their parents. Half of the bullying cases remain unknown to parents. When parents are aware of the bullying, the child’s QoL is better. It is important to proactively identify and address cases in this population.
KEY WORDS: food allergy, anxiety, bullying, health-related quality of life, quality of life
What’s Known on This Subject:
Lifestyle and vulnerability associated with food allergy might predispose affected children to being bullied. Our previous parent survey identified high rates of bullying in this population, but child reports and emotional impact were not assessed.
What This Study Adds:
Bullying was common, often involving threats with food. Bullied food-allergic children, compared with nonbullied, report higher anxiety and lower quality of life. Parental awareness of bullying (∼50% of cases) was associated with better social and emotional functioning in the child.
Recent data suggest an 18% increase in childhood food allergies from 1997 to 20071 with up to 8% of children affected.2 Management of food allergy (FA) requires constant vigilance to avoid food allergens.3,4 The impact on patients and families is significant,5 with resulting decreases in health-related quality of life (QoL). Management of FA evokes potential social vulnerabilities that could predispose children to harassment and bullying.6 In turn, such bullying may be associated with reduced QoL, distress, and social isolation. In our previous study, 50% of parents of children with FA reported that their children in grades 6 through 10 had been bullied, teased, or harassed.6 Since children may not always tell their parents that bullying has occurred,7 it is important to ask the children directly about their experiences.8
The definition of bullying is controversial: although some authors require that bullying be a repeated offense,9–11 many recent legal definitions in the United States identify bullying as, essentially, any act that is intentionally done to harm another individual with a specific characteristic or vulnerability.12,13 Whether a one-time harassment should or should not be considered bullying for the purpose of prevention efforts is an empirical question that can be answered by comparing the impact of repeated versus infrequent offenses.9 The prevalence of bullying varies by country11 and depends on the measure used. In the United States,14 the prevalence of being a victim of moderate to frequent school-related bullying was reported to be ∼17%, whereas a recent UK-based study revealed a prevalence of 18.6% to 32.4%, depending on the respondent’s age.7 In addition to increased suicide risk in bullied children,7 for children with food allergies, having been bullied by the use of an allergen can also be associated with a life-threatening allergic reaction. Therefore, it is of particular interest to verify the extent to which bullying for any reasons is reported by children who suffer from FA, the extent to which it is related to FA in particular (and thus may pose an even greater risk), and its effects on QoL and distress.
As a part of the Enhancing, Managing, and Promoting Well-being and Resiliency program at the Jaffe Food Allergy Institute in the Department of Pediatrics at Mount Sinai Medical Center in New York City, we surveyed patients attending our allergy clinic and their parents about harassment and bullying, QoL, and distress (in both the child and the parent). We hypothesized that (1) bullying is common among food-allergic patients and would be reported by more than 30% of respondents; (2) parent and child reports of bullying of the child would not be consistent; and (3) repeated bullying would be associated with lower QoL and increased distress in both parents and children. This study focused on the bullied victim; we did not evaluate the effects of bullying on the perpetrator (the child who was the bully).
Methods
Patients and parents were consecutively recruited during visits to the Jaffe Food Allergy Institute at Mount Sinai in New York, New York, with a goal of obtaining data on 250 consenting patients/families. To ensure complete representation of the clinic’s population, investigators approached all parents/patients who met the liberal inclusion criteria (age 8–17, established diagnosis of FA, parent or guardian available to consent). Parents were surveyed separately from children but were allowed to be in the same room while answering the questionnaires. The study was approved by Mount Sinai’s Institutional Review Board and involved a full written consent (parent) and assent (minor patient).
Demographic and Allergy Characteristics
Caregivers indicated their child’s age, gender, and race/ethnicity; their family income level; their own education level; their child’s specific food allergies; and whether they have ever used epinephrine.
Assessment of Bullying
Child Report
Our questionnaire used a few constructs utilized in the Revised Olweus Bully/Victim Questionnaire.11,15 Specific language about FA was used. We did not predefine bullying as a recurrent event, to be able to research whether nonrepeated harassment affects QoL and distress. Children were also asked about bullying for other reasons but in less detail (we queried children about the frequency of bullying only related to FA, to avoid confusion in repeatedly answering similar questions). Consistent with previous definitions,9 we a priori defined reports of being bullied more than twice a month as “frequently bullied” in subanalyses.
We report about 3 groups of bullied children that are not mutually exclusive: children or parents who reported that the child was bullied due to FA (but may have also reported having been bullied for other reasons), children or parents who reported that the child has been bullied due to other reasons (but may have also been bullied due to FA), and children or parents who have reported bullying for any reason.
Parent Report About Whether Their Food-Allergic Child Has Been Bullied
The questionnaire was previously used in this population.6 Parents were asked to report about bullying related to food-allergy as well as bullying for any other reason.
Child Outcomes
The Multidimensional Anxiety Scale for Children–10 Items (MASC-10) was used to assess anxiety.16 We used the summary score (range, 0–30, higher scores = more anxiety).
Pediatric Quality of Life Inventory 4.0
The Pediatric Quality of Life Inventory 4.0 (PedsQL 4.0)17,18 is a commonly used measure of health-related QoL. It can be scored as 1 scale (range, 0–100), with a higher score indicating a higher QoL, or as subscales (range, 0–100 for each subscale as well): physical functioning, emotional functioning, social functioning, and school functioning. There is a child (ages 8–12 years) and adolescent version (ages 13–18 years). We predefined 2 aspects of QoL: general QoL (summary score) and social functioning as the most relevant to bullying.
Parent Outcomes
Impact of Events Scale
The Impact of Events Scale (IES)19 is a 15-item self-report questionnaire (score range, 0–75, with 75 indicating the highest level of distress) that measures current subjective distress and posttraumatic stress, as related to a specific event. The IES was examined and validated in numerous clinical and normative settings,20,21 including with parents of children with medical illnesses.21,22 To ensure that we measure parental distress related to the child’s FA, we cited it as the stressor (eg, “I tried to remove my child’s food allergy from my memory”), as we have previously done for other illnesses.21
Food Allergy Quality of Life-Parental Burden
We used the 17-item Food Allergy Quality of Life-Parental Burden,23 a validated questionnaire23–25 to measure the effect of the child’s FA on the parent’s QoL. Higher scores (ranging from 0 to 102) indicate a stronger impact of the illness (lower QoL).
Statistical Analyses
All analyses were conducted by using IBM SPSS Statistics package, 19th edition (SPSS Inc, Chicago, IL). Descriptive statistics were used to characterize the sample. Independent-sample t tests were used to compare outcomes between groups (child and parents who do or do not report bullying). Analysis of variance (ANOVA) was used to examine differences on the outcome measures between more than 2 groups (based on frequency of bullying) by using Tukey’s posthoc tests to determine specific group differences. For those analyses, which were only done regarding bullying related to FA, child reports were divided into 3 categories: those who did not report any bullying, those who reported infrequent bullying (less than twice a month), and those who reported frequent bullying (twice a month or more). To evaluate whether the relationship between bullying, distress, and reduced QoL is confounded by the severity of allergy, in a subanalysis we conducted ANOVAs for each outcome measure with 2 fixed factors: bullying (child or parent report), and the severity of the allergy as measured by self-reported number of allergies (1–2 or > 2) or whether the parent did or did not report having used epinephrine in the past. A “Kappa” statistic was computed to assess the degree of agreement between child and parent reports of bullying. A P value (α level) of less than .05, 2-tailed, was chosen as the level of statistical significance.
Results
Families were enrolled from April 2011 to November 2011. During the 70 days in which research staff was present in the clinic for enrollment, all 312 patients presenting to the clinic who were potentially eligible for participation were approached. Secondary screening identified 29 patients as noneligible, mainly because of diagnostic uncertainty about FA, 26 patients did not consent to the survey, and 257 patients and their parents did consent, of which 251 completed the survey and are included in the present analysis. The parent completing the survey was most often the mother (83.6%). Baseline characteristics of participants by bullying history (1 patient did not answer the FA bullying question) are presented in Table 1. The participants were primarily white and of high income.
TABLE 1.
Demographic Characteristics of Patients Reporting Bullying Due to FA Versus the Rest of the Sample
| Yes Bullying Due to FA, N (%) | No Bullying Due to FA, N (%) | P | |
|---|---|---|---|
| Gender | .90 | ||
| Boy | 49 (32.0) | 104 (68.0) | — |
| Girl | 30 (31.3) | 66 (68.8) | — |
| Not reported | 0 | 1 | — |
| Age, y | .15 | ||
| Children, 8–12 | 55 (29.1) | 134 (70.9) | — |
| Adolescents, 13–17 | 23 (39.0) | 36 (61.0) | — |
| Not reported | 1 | 1 | — |
| Ethnicity | <.01 | ||
| Hispanic | 9 (64.3) | 5 (35.7) | — |
| Non-Hispanic | 67 (29.5) | 160 (70.5) | — |
| Not reported | 6 | 3 | — |
| Racea | NA | ||
| White | 64 (29.6) | 151 (69.9) | — |
| Asian | 10 (32.3) | 21 (67.7) | — |
| African American | 4 (80.0) | 1 (20.0) | — |
| Indian | 1 (33.3) | 2 (66.7) | — |
| Not reported | 5 | 5 | — |
| Income | .10 | ||
| Below 100 000 | 12 (42.9) | 16 (57.1) | — |
| Above 100 000 | 45 (27.4) | 119 (72.6) | — |
| Not reported | 22 | 36 | — |
| Parent highest education level | .08 | ||
| High school | 0 | 4 (100) | — |
| Some college | 6 (66.7) | 3 (33.3) | — |
| College | 38 (36.9) | 65 (63.1) | — |
| Graduate degree | 34 (26.4) | 95 (73.6) | — |
| Other | 1 (25.0) | 3 (75.0) | — |
| Not reported | 0 | 1 | — |
| Allergies | .05 | ||
| 1–2 | 23 (24.2) | 72 (75.8) | — |
| >2 | 56 (36.4) | 98 (63.6) | — |
| Not reported | 0 | 1 | — |
| Severity of FA | .23 | ||
| Used epinephrine | 33 | 55 | — |
NA, not applicable.
Sums to over 251% and 100% because respondents could report more than 1 category. Therefore, statistical comparisons are not presented.
Child and Parent Reports About the Prevalence and Nature of Bullying
Table 2 displays the rates of bullying reported by participants. Overall, 45.4% of the children and 36.3% of their parents indicated that the child has been bullied/harassed for any reason. There was poor agreement in parent versus child reports of bullying due to reasons other than FA, κ = .269. Parents also reported less bullying/harassment of their children than the children regarding bullying due to FA (31.5% per children’s reports, 24.7% according to the parents). Here, the agreement was fair to moderate, κ = .50.
TABLE 2.
Frequency of Bullying Reported by Participants, N = 251
| Child Report | Parent Report | Agreement, %a | κ | |
|---|---|---|---|---|
| Bullied for reasons other than FA | 52.1 | .27 | ||
| Yes, % (n) | 29.5 (74) | 27.5 (69) | — | — |
| No, % (n) | 70.5 (177) | 61.8 (155) | — | — |
| Unsure, % | NA | 9.624 | — | — |
| Not reported, % | 0 | 1.23 | — | — |
| Bullied due to FA | 59.5 | .50 | ||
| Yes, % (n) | 31.5 (79) | 24.7 (62) | — | — |
| No, % (n) | 68.1 (171) | 69.3 (174) | — | — |
| Unsure, % | NA | 5.614 | — | — |
| Not reported, % | 0.41 | 0.41 | — | — |
| Bullied for any reason | ||||
| Yes, % (n) | 45.4 (114) | 36.3 (91) | — | — |
NA, not applicable.
Percent of parents who said that the child was bullied among all the instances in which children indicated that they were in fact being bullied.
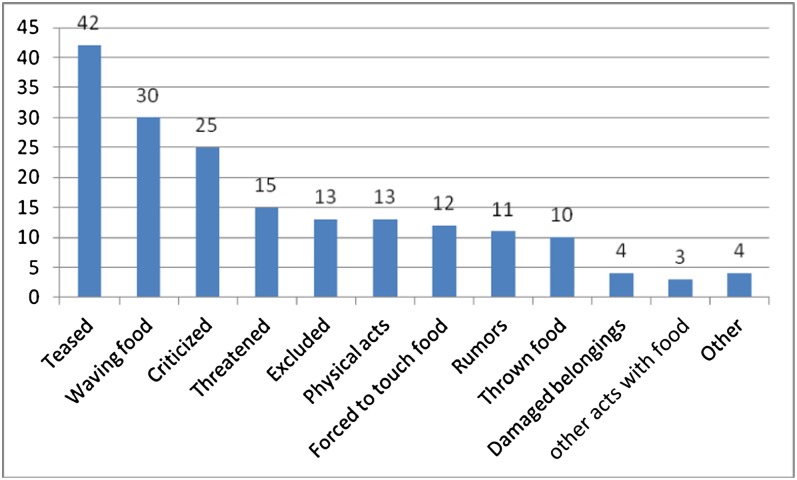
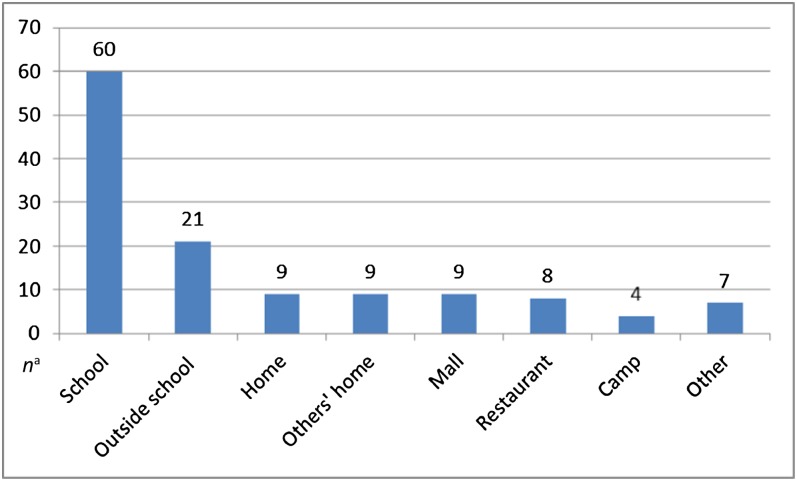
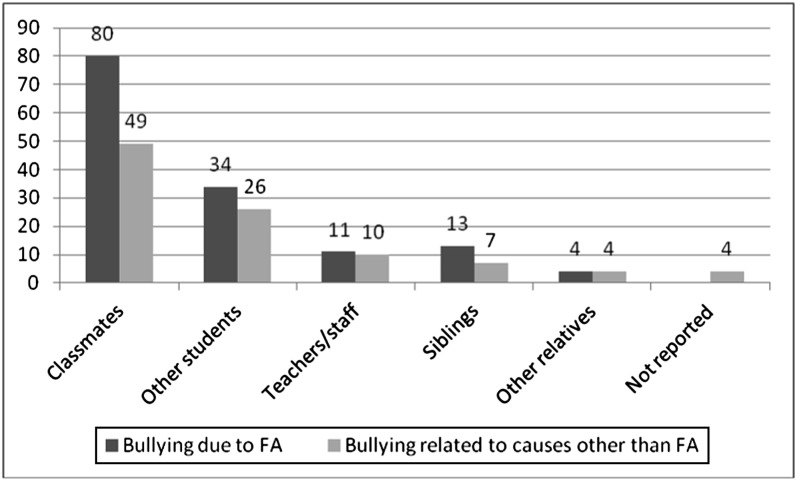
The reported methods of bullying/harassment in FA-related cases are presented in Fig 1. The settings in which bullying due to FA happened are presented in Fig 2, and Fig 3 shows the reported offenders: 80% of the children who were bullied due to FA reported that a classmate was an offender.
FIGURE 1.
Reported methods of bullying (y axis, percent reporting).
FIGURE 2.
Setting in which bullying occurred (child report). an, number of respondents who endorsed the specific setting. Some subjects reported more than 1 setting and therefore categories are not mutually exclusive.
FIGURE 3.
Child-reported offenders (y axis, percent reported).
Notification About Bullying
Most (87%) of the children who were bullied about their FA reported that they told someone about what happened: 71% told their parents, 35% told a teacher, 32% told a friend, 20% told a sibling, and 13% told a principal. Of those who did not tell their parents, 22% told a friend, whereas only 9% told a teacher, suggesting that when parents are not notified, friends are the most important source of information. Only 42.5% of children reported that they told their parents about bullying for any reason.
Bullying and Child Outcomes
Table 3 displays differences in child outcomes in cases who did and did not report bullying for any reason, and Table 4 displays the same outcomes for bullying related to FA. Bullying for any reason was associated with higher anxiety (MASC-10 scores), as well as poorer QoL overall and poorer social QoL.
TABLE 3.
Child Outcomes Depending on Whether They Experience Bullying Due to Any Reason
| Yes Bullying Average Score (SD), N = 74 | No Bullying Average Score (SD), N = 177 | t | P | |
|---|---|---|---|---|
| MASC-10 (anxiety) | 10.29 (5.28) | 7.90 (4.47) | 3.47 | <.01 |
| PedsQL 4.0-Total | 81.20 (11.64) | 88.00 (9.28) | 4.87 | <.01 |
| PedsQL 4.0-Social | 82.26 (16.69) | 92.71 (9.50) | 6.23 | <.01 |
A higher MASC-10 score denotes more anxiety. A higher PedsQL 4.0 score denotes better quality of life.
TABLE 4.
Child Outcomes Depending on the Frequency of Experiencing Bullying Related to FA
| None, N = 158, Average (SD) | Infrequent, N = 57, Average (SD) | Frequent, N = 30, Average (SD) | P | Posthoc Tests | |
|---|---|---|---|---|---|
| MASC-10 anxiety | 7.79 (4.40) | 9.92 (4.87) | 10.27 (5.89) | <.01 | Infrequent, frequent > none |
| PedsQL 4.0-Total | 88.68 (9.14) | 83.46 (9.19) | 77.50 (13.50) | <.01 | All comparisons significant |
| PedsQL 4.0-Social | 93.40 (9.96) | 86.32 (9.47) | 76.75 (20.79) | <.01 | All comparisons significant |
A higher MASC-10 score denotes more anxiety. A higher PedsQL 4.0 score denotes better quality of life.
Table 4 shows the results of ANOVAs with bullying frequency as the fixed factor. Six patients did not report the frequency of bullying. The significance of between-groups differences is presented as posthoc tests. Children who were bullied experienced significantly greater anxiety and decreased general as well as social QoL as compared with children without a history of bullying. Children who reported being bullied more than twice per month (frequent bullying) reported significantly worse QoL as compared with children who were bullied less frequently, but their anxiety levels were not significantly higher.
Bullying and Parent Outcomes
Twenty-seven parents were unsure whether their children were bullied for reasons other than FA, and 15 were unsure about bullying due to FA. For those who thought they knew whether their child was bullied or not, differences in parents’ outcomes are shown in Table 5. Parental distress (IES score) and QoL were worse when parents thought that their child was bullied for any reason (FA or other).
TABLE 5.
Parent Outcomes Depending on Parents’ Perceptions of Whether Their Child Was Bullied
| Child Bullied for Reasons Other Than FA, Average (SD) | Child Bullied Due to FA, Average (SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Yes, N = 69 | No, N = 155 | t | P | Yes, N = 62 | No, N = 174 | t | P | |
| IES | 10.65 (9.88) | 7.55 (9.90) | 2.16 | .03 | 11.98 (10.72) | 7.28 (9.64) | 3.19 | <.01 |
| QoL | 40.13 (20.78) | 29.43 (18.33) | 6.07 | <.01 | 45.20 (20.33) | 28.52 (17.91) | 6.07 | <.01 |
A higher IES score denotes more distress. A higher QoL score denotes lesser QoL.
Bullying, Severity of FA, and QoL/Distress
In all analyses, bullying was significantly associated with the outcome variables independent of the severity of allergy.
The Effect of Parents’ Knowledge About the Child Being Bullied on the Parents’ and the Child’s QoL
When parents knew that their children are being bullied for any reason, the parents’ QoL was significantly lower, and the child’s QoL was significantly better (Table 6). Differences in PedsQL 4.0 total scores between those whose parent did versus did not know about FA-related bullying were nonsignificant, perhaps because bullying related to FA was more likely to be disclosed to parents in the first place, but differences on the PedsQL 4.0 social subscale persisted: when parents knew about FA-related bullying, the child’s social functioning was significantly better.
TABLE 6.
Parent and Child Outcomes in Cases in Which the Child Said That He or She Was Bullied, Depending on Whether the Parent Knew or Did Not Know That the Child Was Being Bullied
| Parent Knew That the Child Is Bullied | Parent Did Not Know That the Child Is Bullied | P | |
|---|---|---|---|
| Ba: Parent QoL (higher score = worse QoL) | 43.02 | 31.31 | .02 |
| Ba: Child QoL (higher score = better QoL) | 84.14 | 78.18 | .03 |
| FAb: Parent QoL (higher score = worse QoL) | 45.08 | 35.97 | .05 |
| FAb: Child QoL (higher score = better QoL) | 81.2 | 82.3 | .70 |
| FAb: Child QoL social functioning subscale (higher score = better QoL) | 88.43 | 79.42 | .01 |
Bullying for any reason, including but not limited to FA (69 parents knew, 155 did not know).
FA-related bullying (62 parents knew, 174 did not know).
Discussion
We found that 31.5% of children who suffer from FA in a specialty clinic in New York report that they were bullied or harassed related to the FA, which frequently involves threats with food, and 45.4% report bullying or harassment due to any reason. It is difficult to compare our results to those that were reported in other studies of bullying, both because of the variable methods that are used to measure bullying as well as because of the unique characteristics of our sample. The rate reported in a study that used a similar measure to ours in school-age children in Norway was 31.8%.9 Population studies using different methodologies revealed bullying rates of ∼17% to 35%,7,9–11,14 which should be compared with our reported rate of 45.4% of bullying for any reason. Although we acknowledge the limitation inherent in comparing between different methodologies or demographics, our findings suggest that food-allergic children who were seen in our clinic were bullied or harassed more frequently, as compared with the general population.
This finding, although alarming, is not surprising, given that children with FA have a vulnerability that can be easily exploited (ie, by a threat to throw the offending food item at the child), in addition to any additional vulnerability that they may have. The prevalence of bullying in children with special health care needs in the United States was reported to be 42.9%,26 which is consistent with our finding. We further found a clear association between reports of bullying, increased distress, and lower QoL, both for children and for their parents, and this association was independent of the severity of the allergy. Bullying related to FA was associated with as much decline in QoL and distress as any other type of bullying in our sample (it is a significant threat).
We found that repeated bullying is associated with lesser QoL and more distress in the victim as compared with less persistent bullying, but less frequent incidents were still associated with reduced QoL and distress as compared with no bullying at all. Since even infrequent bullying was associated with lower QoL, we believe that one should not wait for incidents to repeat to address them, a point that is increasingly recognized by the US legislature.12,13
In our sample, when children were bullied, their parents reported more distress and lower QoL. Interestingly, when the child was bullied but the parents did not know about it, the parents’ distress level was lower and their QoL was better as compared with parents who did know. This suggests that knowledge that their child is harassed, not the harassment itself, is the important determinant of parental QoL. Conversely, we found that children’s QoL is better, and their anxiety less pronounced, when their parents knew about the bullying. This result lends empirical support to the recommendation that to reduce the impact of bullying one should “Help the child identify bullying as well as how and to whom to report it.”27
The κ statistic indicated a weak agreement between parents’ and children’s reports about bullying for reasons other than FA, and a better (moderate) agreement regarding FA-related bullying. But even a moderate agreement is not reassuring: in victims of FA-related bullying, parents were still unaware of child-reported bullying ∼50% of the time in our sample.
Several limitations of our survey must be acknowledged. First, although self-reported information about bullying is commonly used,10 self-reports may introduce bias. Our study elicited self-reported bullying by parents and their children, but we were not able to ask for independent verification from teachers or other students. Second, although we tried to separately look at bullying for any reason and bullying related to FA, there is a risk that some respondents, especially young children, may not have been able to distinguish between the 2. Our “incomplete” rates (reported in the tables), although low, may be related to this complexity. Third, although this is a representative sample of our FA referral clinic, the respondents’ demographic mix is not representative of the general US population, and they may overall represent a more severe phenotype of FA. For example, the finding that Hispanic patients were more likely to report bullying in our survey suggests a relationship between ethnicity and bullying, but a broader ethnic representation is required to verify whether such an association in fact exists. Fourth, we do not have a control group of children who are not food-allergic but demographically similar to ours; therefore, comparisons that we present between our results to those observed with children without FA may be incomplete in that those other studies might have enrolled children whose baseline demographic characteristics are different from our cohort.
Notwithstanding those limitations, we found that bullying related to FA was common in our sample and is associated with decreased QoL and increased distress in both parents and the targeted children. We also found that much of this bullying remains unknown to parents, but that when parents do know, children report a better QoL and less anxiety. We found that bullying is a significant problem in children with FA who were seen in our clinic. Our clinic population is skewed toward more affluent white families, who would be expected to be less vulnerable to bullying.28,29 It is, therefore, likely that our findings, alarming as they may already be, may still underestimate the true rate of bullying experienced by food allergic children. There is a need to increase the likelihood that children disclose bullying; clinicians might consider asking a screening question about bullying during encounters with children with FA.
Glossary
- ANOVA
analysis of variance
- FA
food allergy
- IES
Impact of Events Scale
- MASC-10
Multidimensional Anxiety Scale for Children–10 Items
- PedsQL 4.0
Pediatric Quality of Life Inventory 4.0
- QoL
quality of life
Footnotes
Dr Shemesh conceptualized and designed the study, drafted the initial article, and approved the final article as submitted; Dr Annunziato carried out the initial analyses, reviewed and revised the article, and approved the final article as submitted; Mr Ambrose designed the data collection instruments, coordinated and supervised data collection, critically reviewed the article, and approved the final article as submitted; Dr Ravid designed the data collection instruments, and coordinated and supervised data collection, critically reviewed the article, and approved the final article as submitted; Ms Mullarkey designed the data collection instruments, and coordinated and supervised data collection, critically reviewed the article, and approved the final article as submitted; Ms Rubes designed the data collection instruments, and coordinated and supervised data collection, critically reviewed the article, and approved the final article as submitted; Ms Chuang designed the data collection instruments, and coordinated and supervised data collection, critically reviewed the article, and approved the final article as submitted; Ms Sicherer designed the data collection instruments, critically reviewed the article, and approved the final article as submitted; and Dr Sicherer conceptualized and designed the study, drafted the initial article, and approved the final article as submitted.
Dr Ravid's current affiliation is Lucile Packard Children's Hospital at Stanford, Palo Alto, California.
FINANCIAL DISCLOSURE: Dr Sicherer is a consultant for the Food Allergy Initiative and is an advisor for the Food Allergy and Anaphylaxis Network; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The Enhancing, Managing, and Promoting Well-being and Resiliency (EMPOWER) program and this research are supported by a generous donation from the Jaffe Family Foundation. Dr Sicherer receives research support from the National Institutes of Health (NIH) National Institute of Allergy and Infectious Diseases and the Food Allergy Initiative. Dr Shemesh receives research funding from the NIH National Institute of Diabetes and Digestive and Kidney Diseases and the Jaffe Family Foundation as a part of their support of the EMPOWER program.
COMPANION PAPERS: Companions to this article can be found on pages e1 and e288, online at www.pediatrics.org/cgi/doi/10.1542/peds.2012-1106 and www.pediatrics.org/cgi/doi/10.1542/peds.2012-3253.
References
- 1.Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009;124(6):1549–1555 [DOI] [PubMed] [Google Scholar]
- 2.Gupta RS, Springston EE, Warrier MR, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1). Available at: www.pediatrics.org/cgi/content/full/128/1/e9 [DOI] [PubMed] [Google Scholar]
- 3.Burks AW, Jones SM, Boyce JA, et al. NIAID-sponsored 2010 guidelines for managing food allergy: applications in the pediatric population. Pediatrics. 2011;128(5):955–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sicherer SH, Mahr T, American Academy of Pediatrics Section on Allergy and Immunology . Management of food allergy in the school setting. Pediatrics. 2010;126(6):1232–1239 [DOI] [PubMed] [Google Scholar]
- 5.Lieberman JA, Sicherer SH. Quality of life in food allergy. Curr Opin Allergy Clin Immunol. 2011;11(3):236–242 [DOI] [PubMed] [Google Scholar]
- 6.Lieberman JA, Weiss C, Furlong TJ, Sicherer M, Sicherer SH. Bullying among pediatric patients with food allergy. Ann Allergy Asthma Immunol. 2010;105(4):282–286 [DOI] [PubMed] [Google Scholar]
- 7.Winsper C, Lereya T, Zanarini M, Wolke D. Involvement in bullying and suicide-related behavior at 11 years: a prospective birth cohort study. J Am Acad Child Adolesc Psychiatry. 2012;51(3):271–282, e3 [DOI] [PubMed] [Google Scholar]
- 8.Oppenheimer J, Bender B. The impact of food allergy and bullying. Ann Allergy Asthma Immunol. 2010;105(6):410–411 [DOI] [PubMed] [Google Scholar]
- 9.Solberg ME, Olweus D. Prevalence estimation of school bullying with the Olweus Bully/Victim Questionnaire. Aggress Behav. 2003;29(3):239–268 [Google Scholar]
- 10.Olweus D. Bullying at School: What We Know and What We Can Do. Oxford, UK: Blackwell; 1993 [Google Scholar]
- 11.Kyriakides L, Kaloyirou C, Lindsay G. An analysis of the Revised Olweus Bully/Victim Questionnaire using the Rasch measurement model. Br J Educ Psychol. 2006;76(pt 4):781–801 [DOI] [PubMed] [Google Scholar]
- 12.Stuart-Cassel V, Bell A, Springer JF. Analysis of state bullying laws and policies: a report submitted to the US Department of Education, December 2011. Available at: http://www2.ed.gov/rschstat/eval/bullying/state-bullying-laws/state-bullying-laws.pdf. Accessed April 10, 2012
- 13.Greene MB. State bullying laws with definitions: a Web document, updated April 23, 2011. Available at: http://njbullying.org/documents/statelawswithdefinitions.doc. Accessed April 10, 2012
- 14.Nansel TR, Overpeck M, Pilla RS, Ruan WJ, Simons-Morton B, Scheidt P. Bullying behaviors among US youth: prevalence and association with psychosocial adjustment. JAMA. 2001;285(16):2094–2100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olweus D. The Revised Olweus Bully/Victim Questionnaire. Mimeo. Bergen, Norway: Research Center for Health Promotion (HEMIL Center), University of Bergen; 1996 [Google Scholar]
- 16.March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(4):554–565 [DOI] [PubMed] [Google Scholar]
- 17.Limbers CA, Newman DA, Varni JW. Factorial invariance of child self-report across healthy and chronic health condition groups: a confirmatory factor analysis utilizing the PedsQLTM 4.0 Generic Core Scales. J Pediatr Psychol. 2008;33(6):630–639 [DOI] [PubMed] [Google Scholar]
- 18.Varni JW, Limbers CA, Newman DA, Seid M. Longitudinal factorial invariance of the PedsQL 4.0 Generic Core Scales child self-report Version: one year prospective evidence from the California State Children’s Health Insurance Program (SCHIP). Qual Life Res. 2008;17(9):1153–1162 [DOI] [PubMed] [Google Scholar]
- 19.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218 [DOI] [PubMed] [Google Scholar]
- 20.Sundin EC, Horowitz MJ. Impact of Event Scale: psychometric properties. Br J Psychiatry. 2002;180:205–209 [DOI] [PubMed] [Google Scholar]
- 21.Shemesh E, Newcorn JH, Rockmore L, et al. Comparison of parent and child reports of emotional trauma symptoms in pediatric outpatient settings. Pediatrics. 2005;115(5). Available at: www.pediatrics.org/cgi/content/full/115/5/e582 [DOI] [PubMed] [Google Scholar]
- 22.Kean EM, Kelsay K, Wamboldt F, Wamboldt MZ. Posttraumatic stress in adolescents with asthma and their parents. J Am Acad Child Adolesc Psychiatry. 2006;45(1):78–86 [DOI] [PubMed] [Google Scholar]
- 23.Cohen BL, Noone S, Muñoz-Furlong A, Sicherer SH. Development of a questionnaire to measure quality of life in families with a child with food allergy. J Allergy Clin Immunol. 2004;114(5):1159–1163 [DOI] [PubMed] [Google Scholar]
- 24.Springston EE, Smith B, Shulruff J, Pongracic J, Holl J, Gupta RS. Variations in quality of life among caregivers of food allergic children. Ann Allergy Asthma Immunol. 2010;105(4):287–294 [DOI] [PubMed] [Google Scholar]
- 25.Leung TF, Yung E, Wong YS, Li CY, Wong GW. Quality-of-life assessment in Chinese families with food-allergic children. Clin Exp Allergy. 2009;39(6):890–896 [DOI] [PubMed] [Google Scholar]
- 26.Van Cleave J, Davis MM. Bullying and peer victimization among children with special health care needs. Pediatrics. 2006;118(4). Available at: www.pediatrics.org/cgi/content/full/118/4/e1212 [DOI] [PubMed] [Google Scholar]
- 27.AbilityPath. Org contributors. Walk a mile in their shoes: bullying and the child with special needs. Available at: www.abilitypath.org/areas-of-development/learning–schools/bullying/articles/walk-a-mile-in-their-shoes.pdf; page 28. Accessed April 10, 2012
- 28.Due P, Merlo J, Harel-Fisch Y, et al. Socioeconomic inequality in exposure to bullying during adolescence: a comparative, cross-sectional, multilevel study in 35 countries. Am J Public Health. 2009;99(5):907–914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carlyle KE, Steinman KJ. Demographic differences in the prevalence, co-occurrence, and correlates of adolescent bullying at school. J Sch Health. 2007;77(9):623–629 [DOI] [PubMed] [Google Scholar]