Abstract
Meaningful use of electronic health records to coordinate care requires skillful synthesis and integration of subjective and objective data by practitioners to provide context for information. This is particularly relevant in the coordination of care for children with complex special health care needs. The purpose of this paper is to present a conceptual framework and example of meaningful use within an innovative telenursing intervention to coordinate care for children with complex special health care needs. The TeleFamilies intervention engages an advanced practice nurse in a full-time care coordinator role within an existing hospital-based medical home for children with complex special health care needs. Care coordination is facilitated by the synthesis and integration of internal and external data using an enhanced electronic health record and telehealth encounters via telephone and videoconferencing between the advanced practice nurse and the family at home. The advanced practice nurse’s ability to maintain an updated plan of care that is shared across providers and systems and build a relationship over time with the patient and family supports meaningful use of these data.
Keywords: meaningful use, telehealth, care coordination, DIKW framework
According to the American Nurses Association (ANA), wisdom is the appropriate use of knowledge to manage and solve human problems between types of information1. In clinical practice, the application of experience, intelligence, creativity, and knowledge enables the nurse to make timely clinical decisions based on wisdom, recognizing which information is most important to the plan of care2. This paper describes an innovative model of care that engages an advanced practice registered nurse (APRN) in high-intensity care coordination for children with complex special health care needs (SHCN). The value of this intervention is in matching the enhanced skills and role of the APRN with the level of complexity of data and information involved in coordination of care for this population. Through this intervention, the APRN applies wisdom to manage a complex plan of care.
The Affordable Care Act recognizes the value of coordinated care as essential for cost-effective delivery of health care in the United States3. There is also support for using electronic health records (EHRs) to facilitate coordination of care across systems and at transitions of care, and EHRs are widely expected to improve provider decisions and patient outcomes4. The HITECH portion of the American Recovery and Reinvestment Act mandated that incentives should be offered for meaningful use of EHRs5. Meaningful use of EHRs refers to the ability to transmit information, use decision support, and generate information that is important to patients, health care practice, and public health6. While policy development is essential in driving health care improvements, providers’ experiences do not match policy-makers’ expectations of the role of EHRs in care coordination7. A limitation of these expectations is an assumption that meaningful use of data is independent of the practitioner’s role, educational preparation, and ability to use knowledge to manage human problems.
Evidence suggests that while EHRs facilitate within-office communication, they are less useful in supporting coordination across settings and have limited ability to capture dynamic planning and the medical decision-making process7. Another limitation of expectations for EHRs in care coordination is the time required to monitor, update, and interpret data in the EHR for patients with complex, chronic health conditions. This is particularly true for children who have special health care needs. Approximately 14% of all children have a special health care need (SHCN), defined as having a chronic physical, developmental, behavioral, or emotional condition and requiring more services than typical children8. A subset of these children has unique needs due to the complexity of their chronic conditions. Because of the higher need for and use of health care services, the costs per capita of healthcare for children with complex SHCN are significantly higher than for children in the general population9.
Health records for individuals with SHCN differ from those for children with periodic health needs or single chronic conditions. Children with complex health issues have numerous providers across multiple systems, frequent changes in health status, and multiple medications and problem lists that fluctuate, resulting in data spread across multiple EHR systems. Coordination of care for children with complex SHCN requires the practitioner to have an advanced scope of knowledge and practice as well as dedicated time devoted to the care coordinator role. There is evidence that healthcare charges for typically high-cost patient groups are lower when advanced practice nurses (APRNs) have the autonomy to act upon their knowledge and clinical judgment, and that savings are proportional to nurse dose (time and contacts)10. These factors, along with our experience with a pilot project designed to coordinate care for a cohort of children with complex SHCN11, were the catalysts for the on-going TeleFamilies project.
The TeleFamilies Project
TeleFamilies is a model of care currently being tested in a four-year (2010–2014), randomized controlled trial (RCT) funded by the NIH/National Institutes of Nursing Research (PI: Finkelstein, R01NR010883). The aim of TeleFamilies is to evaluate the effect of increasing levels of telehealth technology on health care service utilization, child and family outcomes, and perceptions of telehealth technology among children with complex SHCN and their families. Subjects are randomized into one of three groups: (1) a control group receiving usual care that includes licensed practical nurse (LPN)-delivered care coordination (n=50); (2) an intervention group receiving APRN-delivered telephone care coordination (n=50); and (3) an intervention group receiving APRN-delivered telephone plus video care coordination (n=50). The duration of each family’s enrollment is 30 months, which includes 6 months of baseline data collection prior to randomization, and 2 years in the usual care or intervention groups.
By design, the APRN’s caseload is limited to 100 families at any given time as she provides services to patients in the intervention arms of the study. The RCT tests the hypothesis that as the level of care coordination role preparation and telehealth use in coordination increases, unplanned health care service use will decrease and quality of life for the children and their families will improve. This paper describes a conceptual framework for the APRN intervention in the TeleFamilies project.
Setting and Sample
The setting for this project is a large urban general pediatrics clinic affiliated with a children’s hospital. The clinic and hospital share an integrated, CCHIT*-certified EHR. Eight pediatricians and four APRNs provide primary care to approximately 10,000 children during 25,000 outpatient visits a year. A subset of this population is enrolled in a clinic-developed Special Needs Program (SNP), which serves approximately 600 children with complex SHCN. The SNP is state-certified as a pediatric health care home (medical home), which is an approach to care in which providers and families work in partnership to improve health outcomes and quality of life for individuals with chronic health conditions12. All subjects recruited for the study are enrolled in the SNP and are between the ages of 2 and 15 years at enrollment. Additional inclusion criteria are: the parent respondent speaks English, and the child meets four of five criteria for having a SHCN as defined by the CSHCN screener13.
TeleNursing Intervention: Telephone and Video Care Coordination
The APRN care coordinator is employed full-time in a care coordinator role with dedicated office space designed for telephone and videoconferencing. Whereas families of children receiving usual care in the SNP contact the clinic’s main number for all matters related to care coordination, families randomized into the APRN intervention groups contact the APRN directly using a dedicated telephone line. Families randomized to the video intervention also have the option of interacting with the APRN via videoconferencing. Families in this group receive a telehealth package free-of-charge that includes a netbook computer, web camera, HIPAA compliant videoconferencing software and broadband internet connection. Technical support is provided by the TeleFamilies project staff, who set up the netbook and internet connection and provide a standardized testing protocol in the home at randomization to ensure functionality.
Enhanced Functionality of the EHR for Care Coordination
Core objectives of the federal HITECH Act focus on EHR support to improve health care, including basic patient data entry, clinical decision support, electronic order entry, and providing patients with their health information4. All of these objectives are encompassed in the APRN-administered intervention through the use of the clinic’s EHR. Within the TeleFamilies intervention, data such as demographics and laboratory results are recorded as structured data, and diagnoses, medications and allergies are updated regularly by the APRN. Additionally, a current plan of care is provided to families and available to providers. Key information is electronically exchanged among EHR users. Privacy and security of data are ensured through data encryption and system-level security. Quality measures including functional status, health care service use, and the presence of an updated care plan are tracked and reported. As a certified health care home, the clinic maintains a list of patients with specific conditions for quality improvement and research.
The hospital and clinic use an integrated EHR that makes inpatient, outpatient and family record viewing possible. The TeleFamilies project’s APRN, who has extensive experience with the health information technology suite, shaped the enhancements to the existing EHR for care coordination. In addition, adaptations were facilitated by TeleFamilies project personnel with telehealth and nursing informatics expertise. The enhancements were facilitated through collaboration with the hospital’s information technology staff and administrators.
All children enrolled in the SNP have a Patient Home Summary which is a custom built EHR-based plan of care. Data including demographics, problem lists, allergies, medications and devices are auto-populated into this plan from structured EHR data. Patient Home Summary data that are not auto-populated but critical to coordinate a child’s care (e.g. home treatments, external providers and relevant treatment information, community services, school) are synthesized and integrated from external documents and entered by the care coordinator. For children in the intervention groups, the EHR has an additional free-text form to document the process and outcomes of telehealth care coordination. Based on evidence16,17 related to care coordination, a unique EHR documentation template (Table 1) was developed to reflect the critical elements of care coordination with prompts to facilitate updating chronic care plans. Like the care coordination template, the plan of care has customized pages and data fields to prompt documentation of critical elements of care. These decision support tools allow multiple providers involved in the child’s care (such as subspecialists, rooming staff, and primary care providers) to view critical information in a single summary, decreasing the need for the family to repeat their story and the child’s history.
Table 1.
Examples of prompts in the electronic documentation template for recording the advanced care coordination process
| Content | Examples of Prompts | Data Type* | |||
|---|---|---|---|---|---|
| A | B | C | D | ||
| Clinical/Health Management Focus |
Acute illness management Nutrition/feeding/growth |
x | |||
| Past History |
Current medications Complicating family or social issues |
x | x | ||
| History of Present Illness, Review of Systems |
Home treatment Response to treatment |
x | x | x | x |
| Assessment/Diagnosis |
Change in symptoms Eating pattern issues/change |
x | x | ||
| Patient/Family |
Goals Strengths and needs |
x | x | ||
| Care Coordination Participants, Activity |
Caregiver (inpatient or discharge planning)
Educational/School (forms, consultation) Home Care |
x | x | ||
| Activities to Fulfill Patient/Family Needs |
Collaboration with care team Develop/modify care plan |
x | |||
| Plan/Follow-up |
Clinical (Primary care appointment, referral)
Home Management |
x | |||
Note. Data types: A) subjective historic; B) subjective current; C) objective current; D) objective historic. This information is not in the template, but is provided here to highlight the focus of each activity.
The APRN uses the EHR to review clinic schedules and admissions and to identify opportunities to connect face-to-face and clarify progress toward family goals and needs for coordination. For example, when a child is scheduled for a well-child or acute care general pediatrics clinic visit with a SNP primary care provider, the APRN may touch base with the family before or after the visit to identify care coordination needs. When a child in the APRN’s caseload is hospitalized, the APRN may visit the family during the stay to ensure seamless transitions from care settings and minimal disruption of the child’s home care regimen.
Meaningful Use of Data in the TeleFamilies Care Coordination Model
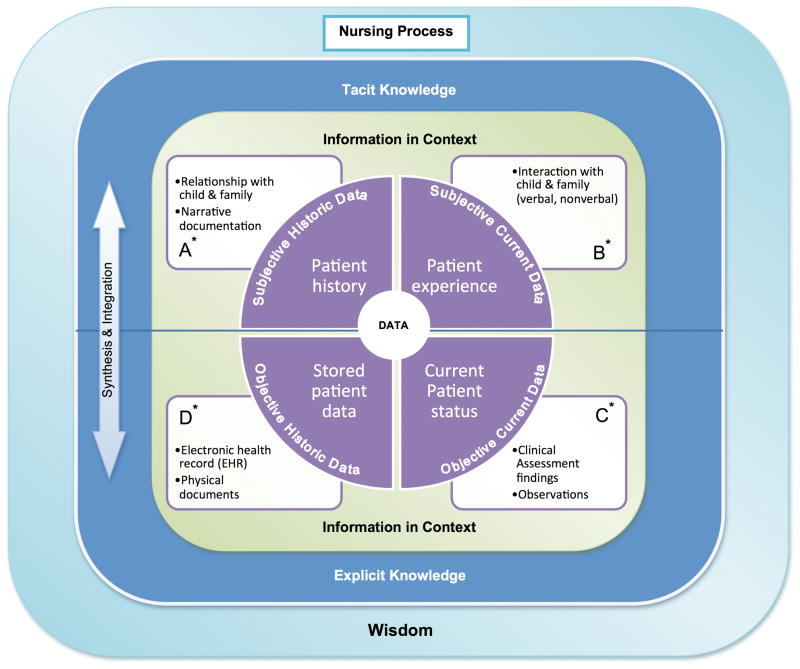
The TeleFamilies model of care coordination incorporates technology and engages the APRN in managing information in a way that supports a dynamic, meaningful, coordinated plan of care developed with the child and family. Figure 1 illustrates the conceptual model that depicts the nursing process of synthesizing and integrating data for care coordination. The ultimate aim of this coordination of care is improved health and quality of life for the child and family. At the systems level, the outcome is care that is effective, family-centered, efficient, safe, timely, and equitable; these are core aspects of quality of care as defined by the Institute of Medicine14. In this conceptual model, data are categorized as historic or current (represented by the left and right halves of the data circle), and as subjective or objective (represented by the top and bottom halves of the data circle). Subjective historic data are the patient’s perception of one’s history including health status, identity, experiences, relationships, and roles. Subjective current data are the patient’s current health-related experiences. Objective data also exist as historic or current; examples of current objective data include values, such as temperature, blood pressure, skin color, and qualities of a heart murmur. Once documented in a patient’s health record, these data become objective historic data. In the coordination of care for children with complex SHCNs, it is important to acknowledge the distinctions between historic and current data because health status is rarely static. Similarly, by appreciating the value of subjective data in the care of children in families, the nurse is able to include the child and family caregivers’ perceptions and experiences into the process of care. Furthermore, the APRN is able to synthesize and integrate data to develop and maintain a dynamic plan of care through her care coordination role that provides a platform for seamless, quality care by primary and specialty providers across settings.
Figure 1.
Synthesis, integration, and communication of data, information, and knowledge in APRN care coordination for children with complex SHCN
The TeleFamilies model of care incorporates the core concepts of data, information, knowledge, and wisdom (DIKW) as described by the ANA2 in the DIKW framework. According to the DIKW framework, data are discrete facts that represent objects, events, and their properties as well as abstract concepts such as pain and spirituality15. Information is data that have been processed into a form that is meaningful. Knowledge is information in context, and wisdom is the appropriate use of knowledge to manage and solve human problems. Two features of professional nursing, according to the ANA1, are (1) integration of objective data with the patient’s subjective experience and (2) application of knowledge to the processes of diagnosis and treatment through the use of judgment and critical thinking. The TeleFamilies intervention utilizes the APRN’s expanded knowledge as well as role autonomy and specialization to integrate data for meaningful use in care coordination. She does this by contextualizing knowledge of historic and current, objective and subjective data.
The TeleFamilies intervention facilitates the contextualization of information in four important ways. First, the APRN practices full-time in her role as care coordinator (Figure 1, A). Her role allows her to develop relationships with families in the intervention groups over time and to gain an increasing awareness of the child and family’s perceptions of their history over time. The TeleFamilies intervention also contextualizes data by technology-enhanced interactions with families (Figure 1, B). Telehealth technology (telephone and videoconferencing) facilitates the APRN’s timely and integrated clinical decision making to coordinate care with families in an ongoing manner based on family needs and priorities. Through videoconferencing the APRN can more readily assess the child and family situation. The APRN’s enhanced scope of knowledge and practice is the third way that TeleFamilies facilitates contextualization of information for care coordination (Figure 1, C). For example, the APRN can perform a comprehensive assessment that incorporates her knowledge of pathophysiology, pharmacology, and sociocontextual factors; she can use that assessment to diagnose and manage acute and chronic conditions as an autonomous practitioner while maintaining communication with the child’s regular providers. The fourth way that TeleFamilies aids in contextualizing information is through enhanced functionalities of the EHR (Figure 1, D), described above.
A standard template for documentation of the APRN’s encounter provides a way to consistently and comprehensively record the processes involved in the care coordination encounter (Table 1). This serves several purposes, including communication of the care coordination encounter to other providers, ensuring that the range and scope of care coordination activities is consistently documented for future tracking purposes, and guiding the APRN in a systematic process of care that is based on evidence for what works in care coordination for children with complex SHCNs16,17. Because the TeleFamilies APRN has adequate time to review and update the EHR throughout an episode of care, information critical to care coordination and included in the Patient Home Summary is more complete and accurate over time.
Process Implementation
TeleFamilies recently completed year two of the four year RCT. Based on preliminary interviews with providers, it is evident that providers in the SNP have experienced positive changes in their ability to provide quality care to children in the intervention groups. These improvements include increased meaningful information in the EHR due to APRN synthesis and integration of internal and external data and efficiency in terms of communicating and triaging issues with patients and families. Additionally, the APRN’s scope of practice enables her to prescribe and refill medications in a timely manner. While quality outcomes related to safety have not been evaluated yet, providers posit that the APRN care coordinator increases safety by reducing risks related to inaccurate medication and problem lists and by improving completeness and timeliness in the transmission of information during transitions of care. To facilitate ongoing evaluation of the TeleFamilies intervention process and to document the roles and activities of care coordination, the APRN logs each encounter with a family in a study database. Over the first year of the intervention, the APRN had encounters with about one-quarter to one-third of her total caseload each month, with an average of 2 to 3 encounters per family per month. The families in the intervention groups value the availability and access to the APRN care coordinator.
Telehealth technology has enhanced the APRN’s ability to collect, interpret, and communicate information across settings and providers. During a videoconferencing encounter, the APRN care coordinator facilitated decision-making by capturing an image of a symptomatic child using a screen shot during a video encounter, and emailed this to a provider on another campus. With this information, the team was able to manage the child’s symptoms without a visit to the clinic. For some families, child health crises that may have previously required hospitalization have been effectively managed at home through a series of interactions with the APRN over an episode of care. In another example, the APRN monitored and managed a child’s transition from intravenous to enteral feedings via telephone, and email, and fax exchanges with the parent and the care team over time. The child was able to remain at home while the APRN remained in the clinic.
Conclusions
Meaningful use of data requires the ability to generate, manage, and communicate information in ways that are important to patients, health care practice, public health, and policymakers4. The conceptual model presented in this paper provides a framework for understanding historic, current, objective, and subjective data in coordination of care for individuals with chronic health conditions and the role of the APRN in transforming this data into meaningful information that is shared with both providers and families. TeleFamilies’ model of care matches the enhanced scope of knowledge and practice of the APRN with the level of complexity inherent in coordinating care for children with complex health needs. The on-going RCT aims to test the hypothesis that this model of care will result in improved outcomes in terms of quality of care and health for children and families. If this hypothesis is supported, project outcomes may inform payment models that include care coordination by an APRN as a covered service. Results will be disseminated following completion of the RCT.
Footnotes
Certification Commission for Health Information Technology
References
- 1.American Nurses Association. Nursing’s social policy statement: The Essence of the Profession. Silver Spring, MD: nursesbooks.org; 2010. [Google Scholar]
- 2.American Nurses Association. Nursing Informatics: Scope and Standards of Practice. Silver Spring, MD: nursesbooks.org; 2008. [Google Scholar]
- 3.Office of the Legislative Council, US House of Representatives. Compilation of Patient Protection and Affordable Care Act. 111th Congress 2d Session; May 2010; Print 111–1. [Google Scholar]
- 4.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 5.American Recovery and Reinvestment Act of 2009. Public Law 111-5. 2009 Jan 9; http://www.gpo.gov/fdsys/pkg/PLAW-111publ5/pdf/PLAW-111publ5.pdf.
- 6.DesRoches CM, Campbell EG, Vogeli C, et al. Electronic health records’ limited successes suggest more targeted uses. Health Aff (Millwood) 2010;29(4):639–646. doi: 10.1377/hlthaff.2009.1086. [DOI] [PubMed] [Google Scholar]
- 7.O’Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2010;25(3):177–185. doi: 10.1007/s11606-009-1195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services. The National Survey of Children with Special Health Care Needs Chartbook 2005–2006. 2008 http://mchb.hrsa.gov/cshcn05/
- 9.Wise PH, Huffman LC, Brat G. A critical analysis of care coordination strategies for children with special health care needs. 2007. Technical Review No. 14. AHRQ Publication No. 07-0054. [PubMed] [Google Scholar]
- 10.Brooten D, Youngblut JM. Nurse dose as a concept. J Nurs Scholarsh. 2006;38(1):94–99. doi: 10.1111/j.1547-5069.2006.00083.x. [DOI] [PubMed] [Google Scholar]
- 11.Cady R, Finkelstein S, Kelly A. A telehealth nursing intervention reduces hospitalizations in children with complex health conditions. J Telemed Telecare. 2009;15(6):317–320. doi: 10.1258/jtt.2009.090105. [DOI] [PubMed] [Google Scholar]
- 12.Minnesota Department of Health. Minnesota’s vision: A better state of health/Health care homes. 2011 www.health.state.mn.mn.us/healthreform/homes/certification.
- 13.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: Development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2:38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.IOM. Envisioning the national health care quality report. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 15.Matney S, Brewster PJ, Sward KA, Cloyes KG, Staggers N. Philosophical approaches to the nursing informatics data-information-knowledge-wisdom framework. ANS Adv Nurs Sci. 2011;34(1):6–18. doi: 10.1097/ANS.0b013e3182071813. [DOI] [PubMed] [Google Scholar]
- 16.McAllister JW, Presler E, Cooley WC. Practice-Based Care Coordination: A Medical Home Model. Pediatrics. 2007;120:e723–e733. doi: 10.1542/peds.2006-1684. [DOI] [PubMed] [Google Scholar]
- 17.Antonelli RC, McAllister JW, Popp J. Making Care Coordination a Critical Component of the Pediatric Health System: A Multidisciplinary Framework. Commonwealth fund. 2009 pub. no. 1277; www.commonwealthfund.org.