Abstract
Background
Integral components of behavioral weight-loss treatment include self-monitoring of diet and physical activity along with feedback to participants regarding their behaviors. While providing feedback has been associated with weight loss, no studies have examined the impact of feedback frequency on weight loss, or the mediating role of self-monitoring adherence in this relationship.
Purpose
This study examined the effect of participant feedback frequency on weight loss and determined if this effect was mediated by adherence to self-monitoring in a behavioral weight-loss trial conducted in the United States.
Method
Participants (N=210) were randomly assigned to one of three self-monitoring methods with either no daily feedback messages or daily feedback messages: 1) paper diary (PD)- no daily feedback, 2) personal digital assistant (PDA)- no daily feedback, and 3) PDA- daily, tailored feedback messages (PDA+FB). The Sobel test via bootstrapping examined the direct effect of feedback frequency on weight loss and the indirect effect through self-monitoring adherence.
Results
Receiving daily feedback messages significantly increased participants’ self-monitoring adherence. A significant effect of feedback frequency on weight loss was noted; however, after adjusting for self-monitoring adherence, the effect of feedback frequency on weight loss was no longer significant. Feedback frequency had a significant indirect effect on weight loss through self-monitoring adherence.
Conclusion
Self-monitoring adherence mediated the effect of feedback frequency on weight loss. Increasing the frequency with which participants receive feedback could enhance self-monitoring adherence, a critical component of behavioral weight-loss treatment.
Keywords: self-monitoring, mediation, adherence, feedback, weight loss, obesity
Introduction
Recent data indicate that 1.5 billion adults are overweight worldwide, and nearly two-thirds of the global population lives in a country where overweight and obesity affect mortality more than underweight [1]. While behavioral weight-loss interventions have demonstrated that a clinically significant reduction in weight is possible among overweight adults [2-3], modest effects in weight change are often seen [4] with varied outcomes even within the treatment group [5]. Additional evidence is needed to determine the most efficacious components of behavioral treatment in order to improve weight-loss outcomes.
A defining feature of behavioral treatment is setting measurable, behavioral goals for weight loss, and self-monitoring of dietary intake and physical activity, which is often accompanied by interventionist feedback to participants, is essential for facilitating goal achievement [6]. The aim of self-monitoring is to increase individuals’ awareness of their eating and activity behaviors and the associated situations that would benefit from behavior change [7]. Due to the importance feedback has in promoting behavior change [8], participants receive feedback regarding behaviors that promote or impede their achievement of dietary and physical activity goals. Providing participants with feedback has been associated with weight-loss success within the context of providing personalized weekly feedback in self-monitoring journals [9], emailing feedback on self-monitoring five times a week [10], and sending immediate text-messages in response to participant-texted information [11]. However, no studies have specifically examined the impact of feedback frequency, e.g., daily feedback, on weight loss.
Although self-monitoring dietary intake and physical activity has been documented as being critical for success in weight loss [12-14], few studies have examined the specific role that self-monitoring plays in behavioral weight-loss treatment [15]. Only one small, 16-week trial was found that examined self-monitoring as a possible mediator of the relationship between participant motivation and weight loss [16]. Information regarding the efficacy of the individual components of weight-loss interventions can be gleaned through mediation analysis, and data regarding the most potent intervention components would allow for a more efficient design of weight-loss programs. Therefore, the purpose of this study was to examine the effect of daily vs. no-daily participant feedback on weight loss and determine if this effect was mediated by self-monitoring adherence. We hypothesized that self-monitoring adherence would mediate the relationship between feedback and weight loss in a randomized clinical weight-loss trial.
Method
Design and Participants
This study is a secondary analysis of the six-month data from the Self-Monitoring And Recording using Technology (SMART) trial, a 24-month randomized clinical trial of standard behavioral weight-loss treatment that compared the effect of three methods for self-monitoring dietary intake and physical activity on weight loss. The design of the SMART trial [17] and the primary outcomes at six months [18] are described in detail elsewhere. Three cohorts of individuals totaling 210 participants were recruited from the community between 2006 and 2008. Eligible participants were: between 18 and 59 years old; had a body mass index (BMI) of 27 to 43 kg/m2; agreed to be randomly assigned to one of the three groups; recorded their dietary intake for five days during the screening process; and had no major medical or psychiatric conditions [17]. Participants were randomly assigned to one of three self-monitoring groups: 1) a paper diary (PD, n=72); 2) a personal digital assistant with software for recording dietary intake and physical activity (PDA, n=68); or 3) a PDA with the same dietary and activity software plus daily feedback messages based upon the participant-recorded behaviors (PDA+FB, n=70).
Standard Behavioral Intervention
All participants received the same intervention emphasizing reduced energy intake (< 25% of calories from fat, 1200 or 1500 daily calories for women, 1500 or 1800 daily calories for men), increased energy expenditure (150 minutes of moderate-intensity exercise), and behavioral changes for eating and activity. Principal strategies of the standard behavioral intervention were presented in 45-90 minute group meetings of 10-15 participants and were led by a master’s-prepared dietician or exercise physiologist. Behavioral strategies included, for example, goal setting, stimulus control, problem solving, and relapse prevention. Participants met in three separate groups (PD, PDA, or PDA+FB) each week for four months and every other week for two months, totaling 20 group sessions in six months [17]. Self-monitoring was a key component of the intervention and required daily recording of all eating (calorie and fat gram) and activity behaviors. This study focuses on dietary self-monitoring, and self-monitoring adherence was objectively verified via the PD or PDA at each group session as “yes” if the participant recorded at least 50% of the weekly calorie goal or “no” if he/she did not. The measurement of dietary self-monitoring has varied greatly in the literature, and no standard definition of self-monitoring adherence exits [14], but we wished to quantify adherence (i.e., recorded at least 50% of weekly goal) rather than merely counting any submitted diary, regardless of completeness, as adherent to self-monitoring.
As part of the standardized treatment, participants in all three groups received interventionist feedback about their recorded eating and activity behaviors on a weekly basis for the first four months and a bi-weekly basis for the next two months. PDA+FB participants also received a tailored diet-related feedback message once daily. The daily messages were customized to the participants’ daily calorie/fat gram goals and the information they had recorded in the PDA along with their relative proximity to the dietary goals throughout the day. Using an established algorithm, the program randomly chose a time of day to send a feedback message. For example, if a participant’s intake had surpassed the calorie and fat gram goals by more than 60% at 1:00 pm he/she could receive a message like, “Try a little harder to watch high-calorie, high-fat foods.” If a participant was within 40-60% of the daily dietary goals at 3:00 pm, feedback such as, “Nice food choices; this will serve you well” might be received. Participants who were not recording would receive a message stressing the importance of self-monitoring. A detailed description of the tailored feedback messages and algorithm for delivery can be found elsewhere [17]. Participants in the PD and PDA groups received no daily feedback messages. The protocol was approved by the University of Pittsburgh Institutional Review Board, and written informed consent was provided by all participants.
Measures
Measures included self-monitoring adherence, feedback frequency, and the outcome measure, percent weight change at six months. Self-monitoring adherence was calculated as a proportion based on the number of sessions out of 20 that the participant had self-monitored. For example, a participant who had self-monitored 16 out of 20 sessions was 80% adherent to self-monitoring. Participants who missed a group session were permitted to submit their diary during the following session. Feedback frequency was dichotomized as the daily feedback group (PDA+FB) or the no-daily feedback group (PD and PDA). Percent weight change was calculated as the change in weight from baseline to six months standardized by the baseline value and expressed as a percentage. In a private room prior to each group session, body weight was measured by a staff member using a digital scale with the participant wearing lightweight clothing and no shoes.
Statistical Analysis
Analyses were performed using the intention-to-treat principle regardless of participants’ adherence and retention. Missing weight measurements due to attrition were handled by adding 0.3 kg/month to the last recorded session weight. This conservative method has been used previously to account for possible weight regain after study drop out [13] and is based on the commonly noted weight regain of 3.0 kg in one-year behavioral weight-loss trials [19-20]. Means and standard deviations were computed for continuous variables; frequency counts and percentages were calculated for categorical variables. Wilcoxon rank-sum tests or two sample t-tests and chi-square tests of independence were used to compare baseline characteristics, self-monitoring adherence, and percent weight change between the daily feedback group and the no-daily feedback group.
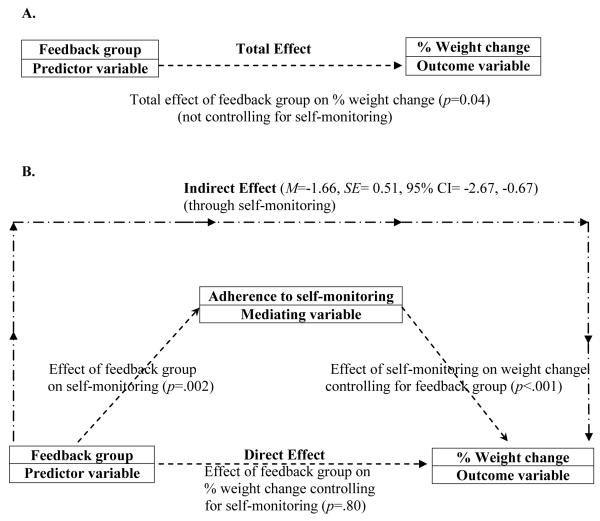
To examine the mediating effect of self-monitoring adherence on the relationship between feedback frequency and weight loss, feedback frequency was treated as a binary variable (1=daily feedback and 0=no daily feedback). The weight-loss trial was not powered a priori to detect mediational effects, but for this study, mediation analyses were performed using the Preacher and Hayes simple mediation macro through SAS (version 9.1.3, SAS Institute, Inc., Cary, NC) with the Sobel test via bootstrapping [21]. We simultaneously tested the direct effect of feedback on weight change, controlling for self-monitoring adherence, and the indirect effect of feedback on weight change through self-monitoring adherence (Figure).
Figure.
Graphical depiction of the direct and indirect effects of feedback group on percent weight change
Note. Feedback groups = 1) daily feedback messages or 2) no daily feedback messages
Model assessment via residual analysis revealed that the residuals from each model were approximately normally distributed based on examination of histograms and normal probability plots. Sensitivity analyses were performed to assess data points that were outliers and/or influential, which were detected via graphical analysis of the raw data and the residuals. A female participant with an unrealistic weight gain at six months (13.3 kg) was excluded from the analyses, and results without this outlier are reported. The significance level for two-sided hypothesis testing was set at 0.05.
Results
The participants were mostly female (85%), White (79%), and married (69%). There were no differences between the feedback groups in baseline demographic variables, weight, or BMI (Table). One hundred ninety-two (91%) participants completed the six-month assessment including 93% of the daily feedback group and 91% of the no-daily feedback group. No differences in age, gender, race, or BMI were noted between those who completed the assessment and those who did not.
Table.
Baseline characteristics of participants by feedback group
| Characteristic | No-daily Feedback (n=140) |
Daily Feedback (n=70) |
|---|---|---|
|
n (%)
|
||
| Female | 119 (85.0) | 59 (84.3) |
| White | 110 (78.6) | 55 (78.6) |
| Married | 97 (69.3) | 47 (67.1) |
| Employed full time | 120 (85.7) | 54 (77.1) |
|
|
||
|
Mean (SD)
|
||
| Age (years) | 47.0 (8.8) | 46.4 (9.5) |
| Education (years) | 15.7 (3.0) | 15.5 (3.0) |
| Weight (kg) | 93.8 (14.8) | 93.7 (15.9) |
| BMI (kg/m2) | ||
| Women | 33.7 (4.2) | 34.2 (4.8) |
| Men | 34.5 (5.1) | 35.5 (4.4) |
Note. No significant differences were noted between the groups. BMI=body mass index; SD=standard deviation.
The mean adherence to self-monitoring for those who did not receive daily feedback was lower (64%, SD=31%) than those who received daily feedback (78%, SD=27%), χ2(1)=11.1, p<0.001. Participants who did not receive daily feedback lost less weight in kilograms (M=5.0 kg, SD=5.6) and percent weight loss (M=5.5%, SD=6.2%) compared to those who received daily feedback (M=7.0 kg, SD=6.5 and M=7.3%, SD=6.6%), χ2(1)=3.87, p<0.05 and t(207)=1.97, p<0.05, respectively.
When examining self-monitoring adherence as a mediating variable, weight change was regressed on feedback groups, and a significant effect of feedback group on weight loss was noted (β=−1.86, SE=0.94, p=0.04, i.e., total effect depicted in Figure- panel A). After adjusting for self-monitoring adherence, the effect of feedback group on weight loss was no longer significant (β=−0.20, SE=0.81, p=0.80, i.e., direct effect depicted in Figure- panel B). Receiving daily feedback messages significantly increased self-monitoring adherence (β=0.14, SE=0.04, p=0.002), and self-monitoring adherence was significantly associated with weight loss (β=−11.78, SE=1.24, p<0.001), such that the effect of feedback group on weight loss was mediated by self-monitoring adherence (M=−1.66, 95% CI=−2.67, −0.67, i.e., indirect effect depicted in Figure- panel B).
Discussion
These analyses revealed that self-monitoring adherence mediated the effect of participant feedback on weight loss in a behavioral weight-loss trial. Studies regarding the effect of mediator variables on weight loss in behavioral trials have been sparse, despite a call for examinations of effective treatment components in randomized clinical trials [22]. Most work has focused on examining behavioral (e.g., physical activity, alcohol intake, emotional eating) [15, 23] or psychosocial (e.g., autonomous regulation, flexible cognitive restraint, exercise self-efficacy) [24-25] variables as mediators of the intervention’s effect on weight loss. Few have considered treatment adherence in a mediating role. Perri et al. examined a composite adherence variable of nine behaviors (e.g., self-monitoring, performing recommended minutes of exercise) and found that the effect of treatment group on weight was partially mediated by adherence; but, the effect of self-monitoring adherence was not isolated [26]. Despite the previously-documented importance of self-monitoring for weight-loss success [12-14], only one study was found that specifically examined self-monitoring adherence as a mediator of weight loss. In a 16-week trial conducted via the Internet, adherence to completing self-monitoring diaries mediated the effect of autonomous motivation on weight loss among 62 women [16]. Likewise, our findings support a mediating role for self-monitoring adherence and fill an important gap in the literature regarding efficacious intervention components in behavioral weight-loss trials.
We also found that the daily feedback group had higher adherence to self-monitoring and greater weight loss than those not receiving daily feedback. While studies have found that feedback to participants is beneficial for weight loss [9, 11], none have compared the impact of different feedback frequencies on weight loss. Krukowski et al. found that weekly facilitator feedback in self-monitoring journals was one of the best predictors of weight loss in a web-based program [9]. Immediate text-message feedback in response to the participant texting his/her weight to the study database resulted in text-messaging participants losing more weight than the control group, and receiving immediate feedback was rated as one of the most helpful aspects of the program. Although this study demonstrated the usefulness of immediate feedback in the intervention group, the control group received no feedback at all [11]. Our study compared no daily feedback to daily feedback administered via a mobile device (PDA) and documented the importance of a higher frequency of feedback for promoting self-monitoring adherence. More frequent participant feedback could be facilitated by increased use of mobile devices like smart phones with email messaging [27] or text messaging [11, 28-29]. Even automated messages have been effective for decreasing body fat [30] and weight [31]; this automaticity enhances the potential to incorporate instant feedback.
Some limitations and strengths to this study should be noted. The use of existing data in a secondary analysis and the relative homogeneity of the participants are limitations. Most participants were female, White, and employed full-time with 15 years of education, limiting the generalizability of these findings. The strengths of this study include the use of a prospective, randomized design examining self-monitoring adherence over six months, the objective measure of adherence via the paper diary or PDA data, and the high participant retention (91%).
In conclusion, this study adds to the body of knowledge on the efficacious components of behavioral weight-loss interventions and contributes to the limited literature examining the role of participant feedback frequency and the mediating effect of self-monitoring adherence. These findings show that self-monitoring adherence mediated the effect of feedback frequency on weight loss, and suggest that increasing the frequency with which participants receive feedback, potentially through the use of mobile technologies, may enhance self-monitoring adherence, a critical part of successful behavioral weight-loss treatment.
Acknowledgements
Thank you to the participants of the SMART trial for their time; the Data Manager, Edvin Music, MSIS; and the Project Director, Mindi Styn, PhD. Funding/Support: National Institutes of Health grants #RO1-DK71817 and K24 Award, NR010742; Data Management Core of the Center for Research in Chronic Disorders, NIH-NINR #P30-NR03924; the General Clinical Research Center, NIH-NCRR-GCRC #5MO1-RR00056; and the Clinical Translational Research Center, NIH/NCRR/CTSA Grant UL1 RR024153 at the University of Pittsburgh.
Footnotes
Trial Registration: clinicaltrials.gov Identifier: NCT00277771
Contributor Information
Melanie Warziski Turk, Duquesne University School of Nursing, 524 Fisher Hall, 600 Forbes Avenue, Pittsburgh, PA, 15282, USA.
Okan U. Elci, Center of Biostatistics, University of Mississippi Medical Center, Arthur C. Guyton Research Complex, 2500 North State St., Jackson, MS, 39216, USA.
Jing Wang, University of Texas Health Science Center at Houston, 6901 Bertner Avenue, Room 614 School of Nursing, Houston, TX, 77030, USA.
Susan M. Sereika, University of Pittsburgh Graduate School of Public Health and School of Nursing, 360 Victoria Bldg., Pittsburgh, PA, 15261, USA.
Linda J. Ewing, University of Pittsburgh School of Medicine, 3811 O’Hara St., Pittsburgh, PA, 15213, USA.
Sushama D. Acharya, U.S. Centers for Disease Control and Prevention, Center for Global Health, Division of Parasitic Diseases and Malaria, 4770 Buford Highway, Atlanta, GA, 30341, USA.
Karen Glanz, 423 Guardian Drive, Schools of Nursing and Medicine, University of Pennsylvania, Philadelphia, PA, 19104, USA.
Lora E. Burke, University of Pittsburgh Graduate School of Public Health and School of Nursing, 415 Victoria Bldg., Pittsburgh, PA, 15261, USA.
References
- 1.World Health Organization [Accessed June 15, 2011];Obesity and overweight fact sheet. WHO website. http://www.who.int/mediacentre/factsheets/fs311/en/
- 2.Burke LE, Warziski M, Styn MA, Music E, Hudson AG, Sereika SM. A randomized clinical trial of a standard versus vegetarian diet for weight loss: the impact of treatment preference. Int J Obes. 2008;32:166–176. doi: 10.1038/sj.ijo.0803706. [DOI] [PubMed] [Google Scholar]
- 3.Carels RA, Young KM, Wott CB, et al. Weight bias and weight loss treatment outcomes in treatment-seeking adults. Ann Behav Med. 2009;37(3):350–355. doi: 10.1007/s12160-009-9109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Franz MJ, Vanwormer JJ, Crain AL, et al. Weight-loss outcomes: A systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107(10):1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Stolley MR, Fitzgibbon ML, Schiffer L, et al. Obesity Reduction Black Intervention Trial (ORBIT): Six-month results. Obesity. 2008;17:100–106. doi: 10.1038/oby.2008.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foster GD, Makris AP, Bailer BA. Behavioral treatment of obesity. Am J Clin Nutr. 2005;82(Supp(1)):230S–235S. doi: 10.1093/ajcn/82.1.230S. [DOI] [PubMed] [Google Scholar]
- 7.Wadden TA, Crerand CE, Brock J. Behavioral treatment of obesity. Psychiatr Clin North Am. 2005;28(1):151–170. doi: 10.1016/j.psc.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Patterson R. The new focus: Integrating behavioral science into disease management. In: Patterson R, editor. Changing Patient Behavior: Improving Outcomes in Health and Disease Management. Jossey-Bass; San Francisco: 2001. pp. 1–21. [Google Scholar]
- 9.Krukowski RA, Harvey-Berino J, Ashikaga T, Thomas CS, Micco N. Internet-based weight control: the relationship between web features and weight loss. Telemed J E Health. 2008;14(8):775–782. doi: 10.1089/tmj.2007.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA. 2003;289(14):1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 11.Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr. 2009;12(12):2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- 12.Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172–7. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 13.Wadden TA, Berkowitz RI, Womble LG, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. New Engl J Med. 2005;353(20):2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- 14.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: A systematic review of the literature. J Am Diet Assoc. 2011;111:92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lubans D, Morgan P, Collins C, Warren J, Callister R. Exploring the mechanisms of weight loss in the SHED-IT intervention for overweight men: A mediation analysis. Int J Behav Nutr Phys Act. 2009;6(1):76. doi: 10.1186/1479-5868-6-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self-monitoring and weight loss in a 16-week Internet behavioral weight loss intervention. J Nutr Educ Behav. 2010;42(3):161–167. doi: 10.1016/j.jneb.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Burke LE, Styn MA, Glanz K, et al. SMART trial: A randomized clinical trial of self-monitoring in behavioral weight management-design and baseline findings. Contemp Clin Trials. 2009;30(6):540–551. doi: 10.1016/j.cct.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke LE, Conroy MB, Sereika SM, et al. The effect of electronic self-monitoring on weight loss and dietary intake: A randomized behavioral weight loss trial. Obesity. 2011;19(2):338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C. Benefits of lifestyle modification in the pharmacologic treatment of obesity: a randomized trial. Arch Intern Med. 2001;161(2):218–227. doi: 10.1001/archinte.161.2.218. [DOI] [PubMed] [Google Scholar]
- 20.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bourchard C, James WPT, editors. Handbook of Obesity. Marcel Dekker; New York: 1998. pp. 855–877. [Google Scholar]
- 21.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 22.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 23.Andrade AM, Coutinho SR, Silva MN, et al. The effect of physical activity on weight loss is mediated by eating self-regulation. Patient Educ Couns. 2010;79(3):320–326. doi: 10.1016/j.pec.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Teixeira PJ, Silva MN, Coutinho SR, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity. 2010;18(4):725–735. doi: 10.1038/oby.2009.281. [DOI] [PubMed] [Google Scholar]
- 25.Silva MN, Markland D, Carraca EV, et al. Exercise autonomous motivation predicts 3-yr weight loss in women. Med Sci Sports Exerc. 2011;43(4):728–737. doi: 10.1249/MSS.0b013e3181f3818f. [DOI] [PubMed] [Google Scholar]
- 26.Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. J Consult Clin Psychol. 2001;69(4):722–726. [PubMed] [Google Scholar]
- 27.Coons MJ, Roehrig M, Spring B. The potential of virtual reality technologies to improve adherence to weight loss behaviors. J Diabetes Sci Technol. 2011;5(2):340–344. doi: 10.1177/193229681100500221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: A feasibility study. Health Informatics J. 2009;15(1):17–25. doi: 10.1177/1460458208099865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36(2):165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 30.Hurling R, Catt M, Boni MD, et al. Using internet and mobile phone technology to deliver an automated physical activity program: Randomized controlled trial. J Med Internet Res. 2007;9(2):e7. doi: 10.2196/jmir.9.2.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]