Abstract
This article reviews the concepts of curricular integration and integrative learning. These concepts have reemerged in contemporary higher education reforms and are crucial in pharmacy programs where students are expected to acquire the knowledge, skills, and abilities needed for competent practice in a complex environment. Enhancing integration requires negotiating obstacles, including institutional traditions of disciplinary structures and disciplinary differences in understandings of knowledge and approaches to teaching and learning; investing the time and effort to design and implement integrated curricula; and using learning-centered pedagogical strategies. Evidence supporting the value of such efforts is not compelling, as much because of insufficient research as lackluster findings. Future avenues of scholarly inquiry are suggested to evaluate curricular integration, distinguishing between the curriculum espoused by planners, the curriculum enacted by instructors, and the curriculum experienced by students.
Keywords: pharmacy education, curricular integration, program evaluation, curriculum
When we put together a jigsaw puzzle, we usually have a picture to guide us. None of the pieces means anything taken alone; only when the pieces are put together do they mean something….This jigsaw puzzle metaphor ought to say something to educators. It is, after all, not unlike how young people experience the curriculum in too many schools. They move from one classroom to another, from one time block to another, from one textbook to another, from one teacher to another, confronted by disconnected, fragmented pieces of information or skills. For these young people, the curriculum is a pile of jigsaw puzzle pieces without a picture.
– James A. Beane, Toward a Coherent Curriculum1
INTRODUCTION
Increased attention is being paid to curricular integration in pharmacy education reform.2,3 Integration is seen as a strategy for making educational experiences coherent, relevant, and engaging; connecting diverse disciplines; and facilitating higher-order learning. Problems and situations that arise in pharmacy practice rarely fall neatly into the disciplinary categories traditionally used to structure pharmacy curricula. If the main purposes of pharmacy education are to provide students with the competencies to function within a large, complex healthcare system and to manage patients’ drug therapies for myriad medical conditions, then curricula that integrate disciplines and theory with practice would be beneficial.4,5 Also, curricular integration is explicitly called for in the accreditation standards for pharmacy programs in both the United States (Accreditation Council for Pharmacy Education Standard 10) and Canada (Canadian Council for Accreditation of Pharmacy Programs Standard 9).6,7
Integrative learning has long been the goal of educational programs; however, the responsibility for accomplishing it is shifting from students being expected to make their own connections between coursework in different disciplines and between their classroom and real-life experiences, to instructors and institutions being responsible for designing curricula that will support integrative learning.8-11 Concerns with curricular integration are driven in part by recognition that integrative learning needs to be fostered to occur for most students, and is hampered by institutional factors such as the proliferation of courses and programs, the diversity of the student population, and the emergence of specialized disciplines.12-15 However, curricular integration is not a panacea for pharmacy students’ fragmented educational experiences or lack of preparedness for practice. There is a danger of integration for integration’s sake rather than for sound educational purposes.16,17 There are gains and losses, and barriers that must be overcome in designing and implementing integrated curricula.
The purpose of this paper is to examine the nature and purpose of curricular integration, strategies for and obstacles to curricular integration, and existing and proposed avenues of scholarly inquiry in curricular integration. This paper draws upon insights gleaned from curriculum design and research experiences in the entry-to-practice program of the Faculty of Pharmaceutical Sciences at the University of British Columbia in Vancouver, Canada.
DEFINING CURRICULAR INTEGRATION
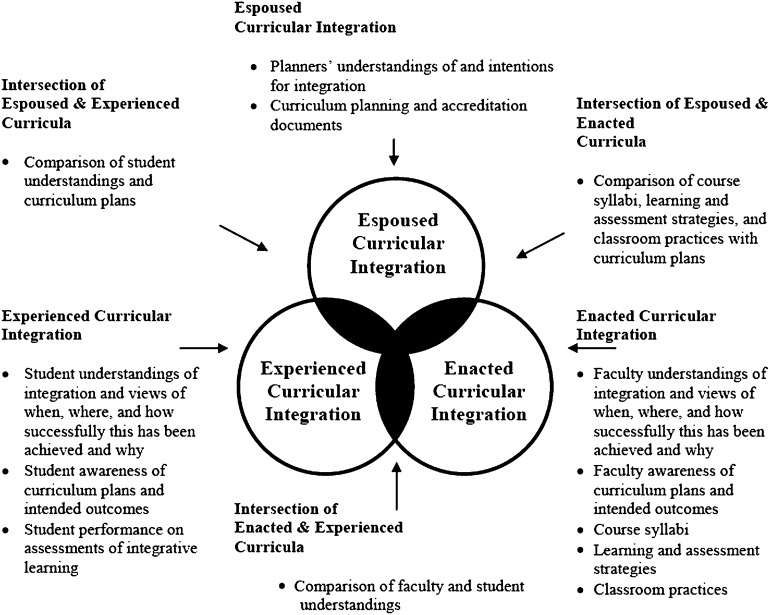
Many consider the terms integration and interdisciplinarity synonymous and do not distinguish among multidisciplinary, interdisciplinary, and transdisciplinary approaches to curriculum design.9 Different definitions for curricular integration have been suggested, but one that is well-suited to pharmacy curricula is the “intentional uniting or meshing of discrete elements or features [of a planned educational experience].”18 Another distinction that is not always made is that between integrated and integrative curricula, the former referring to educational experiences designed to demonstrate to students the patterns and applications of different knowledge domains, and the latter referring to curricula in which students create their own patterns.8 Further confusion arises from differing conceptions of the term curriculum. These include curriculum as the intentions of program planners (the espoused curriculum), curriculum as the learning and assessment activities implemented by instructors in the program (the enacted curriculum), and curriculum as the way in which educational activities are taken up by students (the experienced curriculum). These 3 concepts of curriculum converge and diverge in various ways. For example, the enacted curriculum may diverge from the espoused curriculum because of failure to implement certain elements as intended or to changes over time as the curriculum evolves. Also, students’ learning experiences may fall short of or go well beyond the intentions of the formal activities of the program.
Curricular integration is considered to have horizontal and vertical dimensions, terms which also suffer from inconsistent use. In pharmacy programs, horizontal integration usually refers to integration across basic science disciplines such as medicinal chemistry, pharmaceutics, and pharmacology, while vertical integration typically refers to integration of basic and clinical sciences.19-22 However, the combination of basic and clinical sciences within a unit or year of study has also been referred to as horizontal integration, while the term vertical integration has also been applied to spiral curricula, with topics revisited in increasingly complex ways as the program proceeds.23,24 A comprehensive approach to the design of an integrated curriculum for a pharmacy program must attend to horizontal and vertical dimensions and to structural and pedagogical strategies to facilitate integrative learning.
Horizontal Integration: Crossing Disciplinary Boundaries
Integration across disciplines can take various forms, from multidisciplinarity, with the disciplines separately focusing on a common theme, to interdisciplinarity, with the disciplines developing a shared understanding of a topic, to transdisciplinarity, where disciplinary distinctions are not evident. Each approach has its place, as may disciplinary isolation. Harden notes that no single integration strategy is ideal in a complex curriculum and proposes an “integration ladder,” which provides a gradated scale of cross-disciplinary approaches.25 These range from “awareness,” where the curriculum is discipline-based but instructors have knowledge of the content of coursework in other disciplines, to “transdisciplinarity,” where the curriculum revolves around real-world experiences, without regard for discipline-specific understandings. Intermediate approaches use strategies such as incorporation of material from other disciplines, joint teaching by instructors from different disciplines, and inclusion of interdisciplinary units in the curriculum to enhance integration.25
Vertical Integration: Connecting Across Time and Between Theory and Practice
Vertical integration has 2 aspects: (1) the progression of the curriculum over time, where content unfolds in a logical order and prior learning is accounted for and used to advantage; and (2) the connection to real-world contexts where learning is applied. This latter element is especially important in pharmacy programs, where learning from the classroom is expected to be put to safe and effective use in the clinical practice setting.
Pharmacy curricula are traditionally structured with the basic sciences components in the early years and clinical experiences in the later years. A more contemporary approach is an “inverted triangles” curriculum, with clinical experience provided from the beginning and gradually becoming more dominant and with basic sciences dominant in the beginning and persisting until the end of the program.4,21 The intention of this curricular structure is to enhance integration of theory and practice by (1) using early clinical experience to provide context for learning in the basic sciences, and (2) encouraging the grounding of clinical practice in the basic sciences.
Integrative Learning
Integrative learning has been defined as “an understanding and a disposition that a student builds across the curriculum and co-curriculum, from making simple connections among ideas and experiences to synthesizing and transferring learning to new, complex situations within and beyond campus.”26 This type of learning does not occur spontaneously for most students. Rather, it requires an active process of using theoretical knowledge from diverse subjects and real-life experiences to construct meaningful wholes, and is more likely to occur when deliberately facilitated by instructors.12,13 Further, for integrative learning to occur, students must have the ability to perceive relationships; have, or gain in the process, the knowledge to perceive these relationships; have the ability to generalize through identifying similarities and suppressing dissimilarities; and have the desire for this type of learning.27 Given differences between individuals in their abilities and proclivities as learners, the integrative learning achieved through integrated curricula will vary between students and contexts, and may well differ from curriculum planners’ and instructors’ intentions.
DESIGNING THE INTEGRATED CURRICULUM
As integrative learning does not “just happen” for most students, careful curriculum planning is required to foster this outcome. Ultimately, the intention is to “replace the mystifying mosaic of many separated courses and unrelated extracurriculum experiences by an educational program that has unity.”8 The integrated curriculum should provide students with opportunities to observe and evaluate others’ integrative efforts; to deal with problems that draw on and require new connections between prior experiences; and to relate classroom learning to the external world.8
Integrative Structures
Structural strategies for improving integration in pharmacy programs, at least in the horizontal dimension, include sequential scheduling of related courses (eg, a pathophysiology class, followed by a pharmacology class, followed by a therapeutics class) and the inclusion of occasional learning activities in one discipline that call on knowledge from other disciplines (eg, a pharmacy practice laboratory exercise that draws on biochemistry concepts, or the inclusion of physical assessment activities in a pathophysiology course).28,29 Numerous examples of such strategies have been reported previously in the Journal.30-35
Fuller integration is achieved by using body systems and/or disease states, rather than disciplines, to structure the curriculum.36,37 Thus, a pharmacy curriculum might include modules on the cardiovascular system, the respiratory system, and so on, rather than courses in pharmaceutics, medicinal chemistry, pharmacology, therapeutics, etc. Examples include the programs at Butler University (in the curriculum as intended) and Dalhousie University (in the curriculum as implemented).38,39 Both programs still contain some discipline-based courses, but the bulk of each curriculum is designed as a series of integrated modules.38,39 These 2 programs appear to be fairly similar, but there are notable differences in both the modules offered and the order in which they occur. It is not clear how these choices were made, nor are the strategies for vertical integration reported for these curricula, either with regard to the progression from one module to the next or with regard to connections between classroom-based and experiential elements.
Integrative Pedagogies
In addition to themed arrangements of content, specific pedagogic strategies have the potential to facilitate integrative learning. These include the use of general ability-based outcomes to define learning expectations, case-based and problem-based learning, capstone courses, experiential learning, and comprehensive authentic assessment. These strategies speak to the logical necessity of making clear to students what they are expected to know and be able to do, and aligning educational experiences and assessment tasks with those expectations. Fortunately, these are familiar learning-centered practices already in use to varying degrees in pharmacy programs.
The articulation of general ability-based outcomes is helpful in integrative learning because such outcomes transcend disciplinary boundaries and signal that the intention of the curriculum is not simply mastery of content knowledge, but also the ability to synthesize, apply, and communicate knowledge in complex, real-world situations. Well-designed case-based, problem-based, and capstone learning activities simulate those complex, real-world situations and provide opportunities for students to observe the importance of and to practice the skill of integrating knowledge across disciplines. Experiential learning, which can take the form of community service learning, co-op work, clinical placements, etc., all provide opportunities to apply theory to practice. They are also a source of complex, real-world situations that can be drawn upon to support the learning of theory.
Assessment of integrative learning is a particular challenge.10,40 As with instructional strategies, however, many familiar forms of assessment may be useful if designed to give students opportunities to demonstrate integrative learning. Elements of integrative learning to look for in students’ work include (1) connections between content across disciplines, (2) transference of skills, abilities, theories, or methods gained in one context to new contexts, (3) connections between academic knowledge and life experiences, (4) communication in ways that enhance meaning, and (5) reflections on learning and self-assessing.26 Comprehensive assessments that simultaneously evaluate basic and clinical sciences in pharmacy programs may be particularly valuable, as they transcend the structural elements of the curriculum. For example, students scoring higher on the basic sciences component of a comprehensive examination in their fourth year than in their first year (when the material was taught) has been attributed to their integration of this content with their clinical knowledge during their fourth-year practice experiences.39 However, assessing integrative learning is still challenging, and highlights the importance of faculty leadership and professional development initiatives in the successful use of this and all integrative pedagogies.10
Integrative Efforts at the University of British Columbia
The pharmacy program at the University of British Columbia is mainly structured along disciplinary lines, with sequences of courses in pharmacy practice, medicinal chemistry, pharmaceutics, pathophysiology, clinical pharmacy, and nonprescription therapy supplemented by streams of pharmacy skills laboratory/tutorial courses, case-based tutorials, experiential clerkships, and elective courses. Horizontal integration is achieved through 2 main mechanisms. The first is the inclusion of a case-based tutorial course in each year of the program, explicitly for the purpose of integrating concepts from other courses. The second is the linking of disciplinary courses through co-requisites and scheduling. For example, the pathophysiology, pharmacology, clinical pharmacy, and nonprescription therapy courses list each other as co-requisites and, to the extent possible, are scheduled in consecutive hours in the same classroom. Course coordinators aim for logical sequencing of content and may trade timeslots to facilitate this — an example of “temporal coordination” on Harden’s ladder.25
Additional horizontal integration efforts are emerging as a result of changes in faculty governance. For many years, the faculty had 5 discipline-based divisions. Division members shared research interests and were responsible for the courses in their discipline. In September 2009, these divisions were dissolved. Research and graduate studies functions are now managed by interdisciplinary groups, and entry-to-practice program functions are led by a director and 4 coordinators (1 coordinator for each of the 4 years in the program). The director and coordinators have successfully facilitated connections between courses that were previously isolated (eg, linking a medicinal chemistry course to a pharmacy skills laboratory course through the inclusion of chemical structures on a “Top 200” drugs list now used in both courses — an example of “harmonization” on Harden’s ladder); improving temporal coordination of content in several areas, including diabetes, hypertension, and female reproduction; and piloting a multidisciplinary module in pulmonary disease.25,41
Two forms of vertical integration also occur in the curriculum. Integration over time is achieved by instructors in disciplinary courses collaborating to ensure that the sequencing of topics from term to term and year to year is appropriate, that gaps and repetition are avoided, and that overlaps are used strategically to reinforce concepts. Integration between theory and practice is achieved through brief exposures to practice in the first year of the program and practice experience courses from the second year to the fourth year. Coordinators of the practice experience courses confer with other instructors, particularly in the pharmacy skills and case-based courses, to ensure that students have the opportunity to learn the necessary knowledge and skills to meet performance expectations. Deficiencies in students’ knowledge or skills noted by preceptors are communicated so courses can be modified as needed. For example, the aforementioned drug list was originally created in response to preceptor feedback on students’ poor product knowledge. This is a modest intervention, however, and no real effort is made to infuse the practice elements of the curriculum with the classroom elements, or vice versa.
Integrative pedagogies are also used in the program. For example, a set of ability-based outcomes underpins the curriculum and reference is made to these in all course syllabi; case-based learning occurs in numerous courses, not just in the case-based tutorial stream; and integrative assessment strategies, including case-based and objective structured clinical examinations (OSCEs), are used in selected courses across the curriculum. Regardless, there is consensus within the faculty that greater integration of the curriculum would be desirable. Questions persist, though, about the form(s) this should take, the pace and degree of change needed in the program, and the sustainability of integrative efforts.
OBSTACLES TO CURRICULAR INTEGRATION
There are numerous barriers to creating better integrated pharmacy curricula. As with any substantive curricular change, considerable time and effort are required to plan a coherent program of study to facilitate students’ acquisition of higher-order knowledge, skills, and abilities. Additional challenges to curricular integration include the nature of academia, which is rooted in disciplines, and the limitations of the evidence supporting integrative efforts.
The Nature of Academic Disciplines
Given that much of the focus on curricular integration is on the crossing of disciplinary boundaries, one of the major obstacles to curricular integration is the need to overcome centuries of institutional history. The earliest European universities offered education in separate subjects, and disciplinary communities coalesced as knowledge expanded and research became an important mission of universities.42 As the disciplines evolved, they developed distinct views of knowledge and norms of research, publication, and education, resulting in the formation of “academic tribes,” where faculty members locate their professional aspirations and academic identity.43
With disciplinary differences in the nature of knowledge come differences in approach to teaching and learning. Entwistle, in fact, suggests that “[t]here is an inner logic of the subject and its pedagogy. There is a logic that holds together the various strands of a discipline or topic area, and there is a logical connection between the intellectual demands of the subject and how best to teach it.”13 This “logical connection” between disciplinary learning and teaching can give rise to unique pedagogical strategies, so-called “signature pedagogies,” within disciplines.44 To give a pharmacy-specific example, pharmacologists use drug classes as the organizing framework for their unique knowledge, whereas clinicians use disease states.
Differences in concepts of knowledge, expectations for thinking, and pedagogical practices complicate the process of crossing disciplinary boundaries in integrated curricula. However, a good grasp of disciplinary knowledge and skills is necessary for integrative learning, and takes time to develop, so disciplinary elements are still needed in integrated curricula.45 Significant time is also needed, though, for integrative learning. Within the confines of typical degree programs, this time comes at the expense of disciplinary learning, so it is no surprise that integrated curricula are criticized for loss of depth of disciplinary knowledge.18,46
Effort in Planning and Implementation
Considerable effort is required to design horizontally and vertically integrated curricula. Agreement on issues such as content and timing is required on a level far beyond that in traditional discipline-based programs. Obstacles to integration in pharmacy curricula include lack of faculty time, limited incentive, competition for time within the curriculum for content, non-standardized base knowledge of students, limited opportunity for interaction between basic scientists and clinicians, differences in level of interest in integration on the part of basic scientists and clinicians, and student resistance to unfamiliar pedagogies.19,47
Delivering and sustaining integrated curricula also requires time and resources. Even simple horizontal integration efforts such as coordinating topics between courses often depend on instructors being available at specific times, which may require ongoing planning and repeated negotiation. More elaborate integration efforts that require multiple instructors to be present at the same time are particularly challenging to schedule and may be deemed inefficient or too costly. One solution to this problem has been the creation of designated integrated learning areas, where groups of students are able to meet and access materials that teams of instructors have prepared, but instructors do not all have to be present at the same time.36 However, even creating dedicated space and preparing instructional materials requires the commitment of scarce resources, so this strategy may not be feasible or sustainable.
Lack of Evidence of Effectiveness
For all the apparent value of curricular integration, there is little evidence of substantive improvement in learning outcomes or other important parameters in integrated vs. traditional curricula. This is particularly troublesome in pharmacy programs, where the expectation for evidence-based practice in the clinical realm might reasonably be expected to apply in the educational realm. Reports that “students enjoyed [an interdisciplinary] professional skills development course” and that the course instructors “commented that students…demonstrated a greater understanding of the importance of basic sciences” or that “students as well as teachers appreciated both [horizontal and vertical] forms of integration highly” are encouraging but hardly compelling justification for curriculum change.48,49
More rigorous studies of learning outcomes of integrated curricula have demonstrated improvements that are modest at best. For example, a study comparing the diagnostic ability of medical students in a traditional curriculum, a problem-based learning curriculum, and a systems-based integrated curriculum showed similar performance by those in the problem-based and the integrated curriculum, both of which were better than performance in the traditional curriculum.22 However, the difference was small, so the practical significance of the difference in curricular format is questionable. Similarly, students in an extended practice experience at a single practice site that integrated clinical experience with coursework had nonsignificant improvements on examination scores compared to students completing the more typical practice experiences through various practice sites without integration with their coursework.50 That said, students in the integrated practice experiences gave significantly higher ratings for the effectiveness of their experience in preparing them to deal with patients in a truly caring manner, to deal with ethical dilemmas, to see the effect of social context on patients and their problems, to involve patients in decision making, to relate to diverse patient populations, and to be a self-reflective practitioner. 50 Such outcomes are desirable, of course, but a higher self-rating is not a demonstration of actual improvement in caring attitude, dealing with ethical dilemmas, etc. Mixed findings have also been reported, such as a shift to deeper learning approaches and a shift to more surface learning approaches by similar numbers of students in an integrated curriculum.51
Lack of evidence for effectiveness is not the same thing as lack of effectiveness, however. Much of the available literature is descriptive rather than evaluative. One review of the literature from 1992 to 2009 on interdisciplinary teaching and learning in higher education located only 10 reports of empirical studies.45 This may be because the task of conducting large-scale studies that would convincingly demonstrate the value of integrated curricula and the achievement of integrative learning is filled with challenges. There may be large gaps between the curriculum as planned, the curriculum as delivered by instructors, and the curriculum as experienced by students. Also, research on students has many ethical pitfalls and requires careful attention to procedures to ensure voluntary participation, protection of identity, and avoidance of negative consequences associated with participating, withdrawing, or refusing to participate. A further difficulty is that assessment of student learning is often poorly conducted. Even with well-designed research, the degree to which findings can be generalized may be questioned because institutional contexts, curricular structures, and student populations are complex and vary considerably.
Nevertheless, traditional curricula have been developed and implemented in the absence of supportive evidence. Lack of evidence for the value or effectiveness of integrated curricula should thus be seen as a call to enhanced efforts in the scholarship of teaching and learning, not as justification for avoiding curricular change.
PROPOSAL FOR EVALUATING CURRICULAR INTEGRATION
Effective undergraduate degree program reform requires a scholarly approach to curriculum evaluation, which includes investigation of curricular contexts, processes, and outcomes.52 There are many fruitful avenues for inquiry in the area of curricular integration. Possible research questions include: What understandings of and intentions for integration informed the planning of the curriculum? How did those understandings and intentions influence the design of the curriculum? How have instructors approached the task of implementing curricular integration? What are the drivers, barriers, and pedagogical supports that affect curricular integration, from student and faculty perspectives? What supports have been provided or would be required for improved integrative learning? To what extent is integrative learning demonstrated in students’ work? Figure 1, which distinguishes among the espoused, enacted, and experienced curricula and locates the intersections among them, provides examples of data sources useful for evaluating curricular integration.
Figure 1.
Examples of data sources for evaluating integration in the intersecting curricula.
CONCLUSIONS
Integration is an essential element of contemporary approaches to curriculum renewal in higher education generally, and in pharmacy programs in particular. Curricular integration is a complex, multifaceted process that requires a scholarly approach to development, implementation, and evaluation. While there are differing definitions of important concepts such as curriculum, curricular integration, interdisciplinarity, and integrative learning, the view taken here is that the crucial elements of integrated curricula are the horizontal connections between disciplines and the vertical connections between theory and practice. Further, it is essential to distinguish between the espoused, enacted, and experienced curricula, because a curriculum may neither be implemented as planned, nor have the outcomes expected.
The intention of curricular integration is to foster integrative learning, which in pharmacy programs manifests itself in expectations for graduates to apply knowledge and skills from multiple disciplines to the management of patients’ drug therapy in complex medical conditions. Integrative learning does not occur spontaneously for most students, and thus must be deliberately fostered through integrated curricula. However, the process of creating an integrated curriculum is not easy as it requires negotiation of barriers such as discipline-based institutional structures, concepts of knowledge, and traditions of teaching and learning; limited time and resources; and the need to develop integrative pedagogical and assessment strategies. The evidence to support such an effort is limited. Thus, there is a need for additional scholarly inquiry to more thoroughly evaluate approaches to and outcomes of curricular integration.
ACKNOWLEDGMENTS
The quote by James A. Beane, presented at the opening of this paper, is from the book Toward a Coherent Curriculum1 and is reprinted here with permission from the publisher, the Association for Supervision and Curriculum Development (ASCD), Alexandria, Virginia. Learn more about ASCD at www.ascd.org.
REFERENCES
- 1.Beane JA. Toward a Coherent Curriculum. Alexandria, VA: Association for Supervision and Curriculum Development; 1995. [Google Scholar]
- 2.Hubball H, Burt H. An integrated approach to developing and implementing learning-centred curricula. Int J Acad Dev. 2004;9(1):51–65. [Google Scholar]
- 3.Hutchings P, Huber MT, Ciccone A. The Scholarship of Teaching and Learning Reconsidered: Institutional Integration and Impact. San Francisco, CA: Jossey-Bass; 2011. [Google Scholar]
- 4.Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 5.Ratka A. Integration as a paramount educational strategy in academic pharmacy. Am J Pharm Educ. 2012;76(2):Article 19. doi: 10.5688/ajpe76219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed September 14, 2012. [Google Scholar]
- 7.Canadian Council for Accreditation of Pharmacy Programs. Accreditation standards and guidelines for the baccalaureate degree program in pharmacy. http://www.ccapp-accredit.ca/site/pdfs/university/CCAPP_accred_standards_degree_2006.pdf. Revised 2006. Accessed September 14, 2012. [Google Scholar]
- 8.Dressel P. The meaning and significance of integration. In: Henry NB, editor. The Integration of Educational Experiences: 57th Yearbook of the National Society for the Study of Education. Chicago, IL: National Society for the Study of Education; 1958. pp. 3–35. [Google Scholar]
- 9.Jacobs HH. The growing need for interdisciplinary curriculum content. In: Jacobs HH, editor. Interdisciplinary Curriculum: Design and Implementation. Alexandria, VA: Association for Supervision and Curriculum Development; 1989. pp. 1–11. [Google Scholar]
- 10.Huber MT, Hutchings P, Gale R, Miller R, Breen M. Leading initiatives for integrative learning. Liberal Educ. 2007;93(2):46–51. [Google Scholar]
- 11.Miller R. Integrative learning assessment. Peer Rev. 2005;7(4):11–14. [Google Scholar]
- 12.Ambrose SA, Bridges MW, DiPietro M, Lovett MC, Norman MK. How Learning Works: Seven Research-Based Principles for Smart Teaching. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 13.Entwistle NJ. Teaching for Understanding at University: Deep Approaches and Distinctive Ways of Thinking. New York, NY: Palgrave Macmillan; 2009. [Google Scholar]
- 14.Arcario P, Eynon B, Clark JE. Making connections: integrated learning, integrated lives. Peer Rev. 2005;7(4):15–17. [Google Scholar]
- 15.Klein JT. Integrative learning and interdisciplinary studies. Peer Rev. 2005;7(4):8–10. [Google Scholar]
- 16.Bloom BS. Ideas, problems, and methods of inquiry. In: Henry NB, editor. The Integration of Educational Experiences: 57th Yearbook of the National Society for the Study of Education. Chicago, IL: National Society for the Study of Education; 1958. pp. 84–104. [Google Scholar]
- 17.Brophy J, Alleman J. A caveat: curriculum integration isn’t always a good idea. Educ Leadersh. 1991;49(2):66. [Google Scholar]
- 18.Case R. The anatomy of curricular integration. Can J Educ. 1991;16(2):215–224. [Google Scholar]
- 19.Brueckner JK, Gould DJ. Health science faculty members’ perceptions of curricular integration: insights and obstacles. J Int Assoc Med Sci Educ. 2006;16(1):31–34. [Google Scholar]
- 20.Dahle L, Brynhildsen J, Fallsberg MB, Rundquist I, Hammar M. Pros and cons of vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum: examples and experiences from Linköping. Sweden. Med Teach. 2002;24(3):280–285. doi: 10.1080/01421590220134097. [DOI] [PubMed] [Google Scholar]
- 21.Leinster S. The undergraduate curriculum. In: Dent JA, Harden RM, editors. A Practical Guide for Medical Teachers. 3rd ed. Edinburgh, UK: Elsevier; 2009. pp. 17–22. [Google Scholar]
- 22.Schmidt HG, Machiels-Bongaerts M, Hermans H, ten Cate TJ. The development of diagnostic competence: comparison of a problem-based, an integrated, and a conventional medical curriculum. Acad Med. 1996;71(6):658–664. doi: 10.1097/00001888-199606000-00021. [DOI] [PubMed] [Google Scholar]
- 23.Oliver R, Kersten H, Vinkka-Puhakka H, et al. Curriculum structure: principles and strategy. Eur J Dent Educ. 2008;12(Suppl. 1):74–84. doi: 10.1111/j.1600-0579.2007.00482.x. [DOI] [PubMed] [Google Scholar]
- 24.Prideaux D. In: Integrated learning. A Practical Guide for Medical Teachers. 3rd ed. Dent JA, Harden RM, editors. Edinburgh, UK: Elsevier; 2009. pp. 181–186. [Google Scholar]
- 25.Harden RM. The integration ladder: a tool for curriculum planning and evaluation. Med Educ. 2000;34(7):551–557. doi: 10.1046/j.1365-2923.2000.00697.x. [DOI] [PubMed] [Google Scholar]
- 26.Association of American Colleges and Universities. Integrative and applied learning VALUE rubric. Rhodes TL, editor. Valid Assessment of Learning in Undergraduate Education. Washington, D.C. http://www.aacu.org/value/rubrics/integrativelearning.cfmAmerican Association of Colleges and Universities. September 14, 2012;2010 . Accessed . [Google Scholar]
- 27.Krathwohl DR. The psychological bases for integration. In: Henry NB, editor. The Integration of Educational Experiences: 57th Yearbook of the National Society for the Study of Education. Chicago, IL: National Society for the Study of Education; 1958. pp. 43–65. [Google Scholar]
- 28.Harrold MW, McFalls MA. A pharmacy practice laboratory exercise to apply biochemistry concepts. Am J Pharm Educ. 2010;74(8):Article 144. doi: 10.5688/aj7408144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Albano CB, Brown W. Integration of physical assessment within a pathophysiology course for pharmacy. Am J Pharm Educ. 2012;76(1):Article 14. doi: 10.5688/ajpe76114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Witt-Enderby PA, McFalls-Stringert MA. The integration of basic cell biology concepts into the practice of pharmacy. Am J Pharm Educ. 2004;68(2):Article 40. [Google Scholar]
- 31.Marshall LL, Nykamp D. Active-learning assignments to integrate basic science and clinical course material. Am J Pharm Educ. 2010;74(7):Article 119. doi: 10.5688/aj7407119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karimi R, Arendt CS, Cawley P, Buhler AV, Elbarbry F, Roberts SC. Learning bridge: curricular integration of didactic and experiential education. Am J Pharm Educ. 2010;74(3):Article 48. doi: 10.5688/aj740348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stewart AL, Buckner IS, Wildfong PLD. A shared assignment to integrate pharmaceutics and pharmacy practice course concepts. Am J Pharm Educ. 2011;75(3):Article 44. doi: 10.5688/ajpe75344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kolluru S, Roesch DM, de la Fuente AA. A multi-instructor, team-based, active-learning exercise to integrate basic and clinical sciences content. Am J Pharm Educ. 2012;76(2):Article 33. doi: 10.5688/ajpe76233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.112th Annual Meeting of the American Association of Colleges of Pharmacy, San Antonio, TX, July 9-13, 2011. Am J Pharm Educ. 201175(5):Article 105. [Google Scholar]
- 36.Davis MH, Harden RM. Planning and implementing an undergraduate medical curriculum: the lessons learned. Med Teach. 2003;25(6):596–608. doi: 10.1080/0142159032000144383. [DOI] [PubMed] [Google Scholar]
- 37.Ryan G, Hanrahan J, Krass I, Sainsbury E, Smith L. Best practices assessment to guide curricular change in a bachelor of pharmacy program. Am J Pharm Educ. 2009;73(1):Article 12. doi: 10.5688/aj730112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hrubey TW. An integrated case-based curricular model for the entry-level doctor of pharmacy degree. Am J Pharm Educ. 1996;60(3):265–274. [Google Scholar]
- 39.Whelan AM, Mansour S, Farmer P. Outcomes-based integrated hybrid PBL curriculum. Am J Pharm Educ. 2002;66(3):302–311. [Google Scholar]
- 40.Boix-Mansilla V. Assessing student work at disciplinary crossroads. Change. 2005;37(1):14–21. [Google Scholar]
- 41.Pearson ML, Fielding DW, Albon SP, Brady CM, Wasan KM, Verma AM.Climbing Harden's ladder: harmonization, temporal coordination, and correlation. Abstract in 112th annual meeting of the American Association of Colleges of Pharmacy San Antonio, TX: July 9-13, 2011Am J Pharm Educ. 2011755Article 105 [Google Scholar]
- 42.Kreber C. The University and its Disciplines: Teaching and Learning Within and Beyond Disciplinary Boundaries. New York, NY: Routledge; 2009. [Google Scholar]
- 43. Becher T, Trowler P. Academic Tribes and Territories: Intellectual Enquiry and the Culture of Disciplines. 2nd ed. Philadelphia, PA: Open University Press; 2001.
- 44.Shulman LS. Signature pedagogies in the professions. Daedalus. 2005;134(3):52–59. [Google Scholar]
- 45.Spelt EJH, Biemans HJA, Tobi H, Luning PA, Mulder M. Teaching and learning in interdisciplinary higher education: a systematic review. Educ Psychol Rev. 2009;21(4):365–378. [Google Scholar]
- 46.Smith SR. Toward an integrated medical curriculum. Med Health RI. 2005;88(8):258–261. [PubMed] [Google Scholar]
- 47.Stull R, Carter RA. Integrating the pharmacy curriculum: more to consider than improving learning. Am J Pharm Educ. 2002;66(4):407–410. [Google Scholar]
- 48.Hammer DP, Paulsen SM. Strategies and processes to design an integrated, longitudinal professional skills development course sequence. Am J Pharm Educ. 2001;65(1):77–85. [Google Scholar]
- 49.Brynhildsen J, Dahle L, Fallsberg MB, Rundquist I, Hammar M. Attitudes among students and teachers on vertical integration between clinical medicine and basic science within a problem-based undergraduate medical curriculum. Med Teach. 2002;24(3):286–288. doi: 10.1080/01421590220134105. [DOI] [PubMed] [Google Scholar]
- 50.Ogur B, Hirsh D, Krupat E, Bor D. The Harvard Medical School-Cambridge integrated clerkship: an innovative model of clinical education. Acad Med. 2007;82(4):397–404. doi: 10.1097/ACM.0b013e31803338f0. [DOI] [PubMed] [Google Scholar]
- 51.Balasooriya CD, Hughes C, Toohey S. Impact of a new integrated medicine program on students' approaches to learning. High Educ Res Dev. 2009;28(3):289–302. [Google Scholar]
- 52.Hubball H, Pearson ML. Scholarly approaches to curriculum evaluation: critical contributions for undergraduate degree programme reform in a Canadian context. In: Saunders M, Trowler P, Bamber V, editors. Reconceptualising Evaluation in Higher Education: The Practice Turn. Maidenhead, UK: SRHE & Open University Press; 2011. pp. 186–192. [Google Scholar]