Abstract
Background:
Immunization coverage rates in Nigeria have remained very poor, in spite of numerous programs and strategies, specifically designed to improve coverage. This study was to assess the possible effects of greater community participation on immunization coverage, by comparing the immunization coverage in a rural community with a functional community health committee, with an urban community, with no distinct community structure.
Materials and Methods:
The study was carried out in Ondewari, a rural, riverine community, in Bayelsa State; and Yenagoa, the capital of Bayelsa State, south-south Nigeria; using a cross-sectional, comparative study design. The data were collected using a structured interviewer-administered questionnaire, administered on female head of households in both communities, with under-five children; and used to collect information on the socio-demographic characteristics of the respondents, the immunization status of children in the household below the age of 2 years, and reasons for none and incomplete immunization.
Results:
A total of 288 respondents were studied in the rural community, while 270 respondents were studied in the urban center. The respondents in the urban center were significantly younger (P<0.01), better educated (P<0.001), and had fewer number of children (P<0.01). The immunization status of children in the rural community was significantly better than those in the urban community (P<0.000). Only 11.46% of the children in the rural community were not immunized, compared to 47.04% in the urban community. However, the dropout rate in the rural community was much higher; with a DPT dropout rate of 77.34%, compared to 12.39% in the urban community. Most of the reasons given in the urban community for the incomplete immunization were linked lack of motivation, and include relocation (11.34%) and the adverse rumor about childhood immunization (17.23%), while the reasons in the rural community were mostly health facility related, and included the absence of the vaccinator (20.46%) and nonavailability of vaccines (26.64%).
Conclusion:
The immunization coverage in the rural community was surprisingly better than that of the urban community, which can be attributed to better mobilization and participation in the delivery of immunization services.
Keywords: Childhood immunization coverage rate, community participation, rural, south-south Nigeria, urban
INTRODUCTION
Under-five mortality rate in Nigeria is one of the highest in the world, and vaccine preventable diseases are said to be responsible for at least 20% of these deaths.1 This informed the introduction of the Expanded Programme on Immunization by the World Health Organization in 1974, and the nationalization of the program in Nigeria in 1996, to expand coverage and increase the number of antigens.1 Although there was a significant increase in immunization coverage, it however proved very difficult to sustain, due to a number of factors including the nonavailability of vaccines, inaccessible immunization centers, long waiting times, and low demand, linked to poor knowledge and motivation.1,2
Goal 4 of the Millennium Development Goals that seeks to achieve a two-third drop in childhood mortality rate between 1990 and 2015 provided another impetus to improve immunization coverage in Nigeria.3 This led to the introduction of supplemental immunization programs and strategies like Reaching Every Ward, accelerated measles campaign and Immunization Plus Days (IPDs). These programs like all other MDG programs were hugely funded by government, and donor agencies, and ensured that immunization services were brought to homes, as vaccinators were provided with all the logistics needed to move from house to house, to immunize eligible children.1,3 This surprisingly has not resulted in any significant increase in immunization coverage rates in Nigeria, as the percentage of fully vaccinated children only increased from 13% in 2003, to 23% in 2008.4 We wish to postulate that the low immunization coverage achieved might be due to poor community mobilization and participation for the programs. Although community mobilization and participation often form parts of the programs,5 we suspect that they were not given the desired emphasis, especially as the true nature of community participation is often not well understood. Although community participation has assumed a lot of meanings since the Alma Ata declaration, the best subscribed definition remains that found in the Alma Ata declaration, that sees community participation as the process by which individuals and families assume responsibility for their own health and welfare, and for those of the community, and develop the capacity to contribute to their community's development.6 A more operational definition offered by Zakus and Lysack in 1998 defined community participation as a process whereby community members collectively assess their health needs and problems, and organize to develop strategies for implementing, maintaining, and monitoring solutions to those problems.7
Our suspicion is not entirely new, as suggested by the findings of other studies,8,9 and also during the controversy that trailed the polio eradication efforts in northern Nigeria.10,11 This was however blamed on religion and western conspiracy.9,10 This study is to test the hypothesis in south-south Nigeria where none of these fears existed. Our study compared immunization coverage in a rural community with a functional community health committee, with an urban community, with no distinct community structure. It is hoped that the findings of this study would help refocus the immunization effort in Nigeria, in its battle to eradicate polio, and achieve universal childhood immunization coverage.
MATERIALS AND METHODS
The study was carried out in Ondewari, a rural, riverine community, in the Southern Ijaw Local Government Area of Bayelsa State; and Yenagoa, the capital of Bayelsa State, south-south Nigeria.
A cross-sectional, comparative study design was used, with the data collected using a structured interviewer-administered questionnaire. The questionnaire was administered to female head of households in both communities, with under-five children; and used to collect information on the socio-demographic characteristics of the respondents, the immunization status of children in the household below the age of 2 years, and reasons for none and incomplete immunization.
The study was designed to detect a 5% difference in immunization coverage, with an alpha error of 5%, acceptable beta error of 20%, and a statistical power of 80%; while the national average of immunization coverage of 23% was also used.4 Using the usual formula for sample size determination for studying proportions in populations of less than 10,000,12 the minimum required sample size was thus determined to be 272, but made up to 288 to take care of nonresponses.
Data analysis was by SPSS 17.0 software, Microsoft word, and Excel. Summary measures were calculated for each outcome of interest; and the differences between the communities were tested using the appropriate statistical test. For all statistical tests, P value of 0.05 or less was considered statistically significant.
Ethical clearance
The approval to undertake the study was sought and obtained from the ethical review committee of the University of Port Harcourt Teaching Hospital, Port Harcourt, the Bayelsa State Ministry of Health, as well as from the Chiefs of the communities. Informed consent was also sought and received from all the study participants.
RESULTS
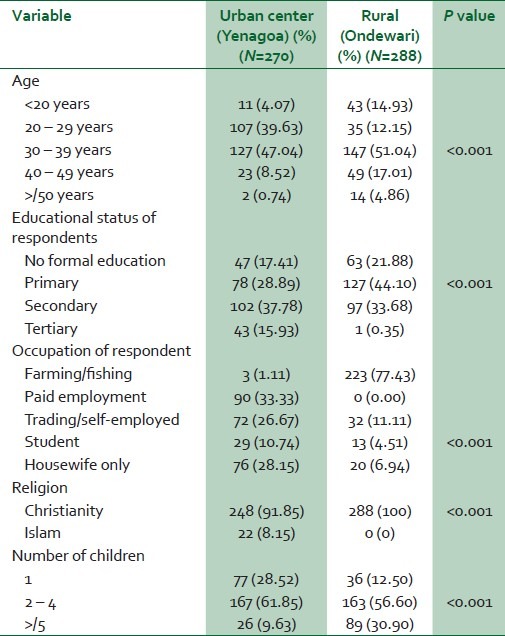
A total of 288 respondents were studied in the rural community, while 270 respondents were studied in the urban center. Most of the children (253, 87.85%) were delivered outside a health facility, by a Traditional Birth Attendant, compared to 89 (32.63%) in the urban community. The socio-demographic characteristics of the respondents are shown in Table 1. The respondents in the urban center were significantly younger (P<0.01), better educated (P<0.001), and had fewer number of children (P<0.01). The average age of the respondents in the urban community was 30.84 years, compared to 33.32 years in the rural community; more than half of the respondents in the urban community had more than secondary school education, compared to 34.03% in the rural community, while the average number of children for respondents in the urban community was 2.72, compared to 3.68 in the rural community. The respondents in the rural community were mostly farmers and fisherfolks.
Table 1.
The socio-demographic characteristics of the study participants
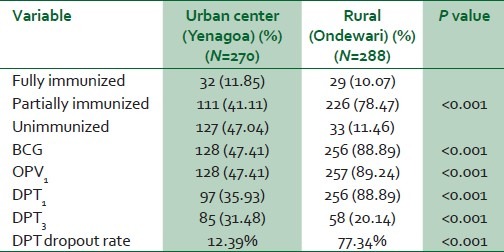
The immunization status of the children is shown in Table 2. The immunization status of children in the rural community was significantly better than those in the urban community (P<0.000). Only 11.46% of the children in the rural community were not immunized, compared to 47.04% in the urban community. However, the dropout rate in the rural community was much higher; the DPT dropout rate was 77.34%, and more than a three quarter of the children (78.47%) were unable to complete their immunization, compared to a DPT dropout rate of 12.39% in the urban community.
Table 2.
The immunization status of the children
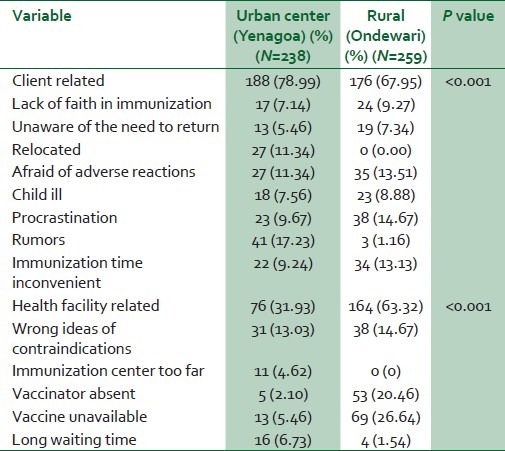
The reasons for the inability to immunize the child or to complete the immunization were assessed and grouped into client related and health facility related, and presented in Table 3. The respondents in the urban community gave more reasons that could be linked to their lack of motivation, while the reasons given by the respondents in the rural community were mostly health facility-related. The respondents in the urban community were more deterred by their relocation (11.34%) and the adverse rumor about childhood immunization (17.23%), while the absence of the vaccinator (20.46%) and nonavailability of vaccines (26.64%) more seriously affected the immunization in the rural community.
Table 3.
Reasons for incomplete immunization (multiple reasons)
DISCUSSION
The number of children in both communities that were fully immunized was low. It is lower than the national and south-south Nigeria averages,4 and shows the effort required to achieve the target of universal childhood immunization in both communities. This is unfortunate considering that the Reaching Every Ward approach, the accelerated measles campaign, and the Immunization Plus Days (IPDs) strategy were able to nearly double immunization coverage in the country from 13% in 2003 to 23% in 2008.4 It is however likely that the communities in Bayelsa State did not fully benefit from these programs, since most of them were engulfed in armed youth restiveness during the period.
It was very surprising to find that more children were not immunized in the urban community, compared to the rural community. This is even as the respondents in the urban community were better educated, and therefore should have better health seeking behavior. The 2008 demography and health survey in Nigeria had indicated that mother's level of education is strongly related to immunization coverage, with mothers with secondary education more than eight times more likely to fully immunize their children than mothers without education.4 The survey also indicated that children in urban areas are more than twice as likely as rural children to be fully vaccinated. This finding of our study is also contrary to several other studies in Nigeria, and elsewhere in the world.13,14 The possible reasons for this could be from the reasons given by the respondents for their inability to immunize their children, and the fact that the respondents in the rural community were better encouraged to patronize the immunization services, by the effort of their community health committee.15 The Ondewari community in the years prior to the study had suffered a series of measles epidemics that compelled the community Chiefs and health committee to ensure that all children in the community were immunized.
Several respondents in our urban community were deterred by the negative rumor about childhood immunization. This was not a big problem in our rural community, but was prominent in the other parts of Nigeria, especially northern Nigeria.1,10,11 These negative rumors originated from outside the south-south region of Nigeria, and were spread through the mass media. This probably explains its little effect in our rural community, where the exposure to the mass media is more limited. It however identifies the need for health workers to be more proactive in responding to rumors that are potentially damaging to the utilization of important health services.
The relocation of some of the respondents in our urban community prevented them from immunizing their children. This was not a problem in our rural community, especially because most of the residents were indigenes, and therefore permanent residents of the community. On the other hand, most of the respondents in the urban community (Yenagoa) were actually recent migrants, attracted by the growing economic opportunities in the town. Rural-urban migration has been shown to adversely affect the utilization of health services, including immunization.8,16 Antia reviewed immunization records in Nigeria and found that children of rural nonmigrant mothers were more than two times more likely to be fully immunized than children of rural-urban migrant mothers.17 It is also known that poor urban migrants often feel excluded and worried by the crowd in the immunization clinic, because they lack fine cloths, or have thin babies who might provoke moral disapproval. They are also discouraged by the fact that they do not have prior social connection with the clinic staff, and therefore likely to be the last to be attended to.8
It was not surprising that health facility-related reasons played more part in deterring immunization in the rural community, compared to the urban community.2,8 This could be the reason for the high DPT drop-out rate in the rural community, in spite of the best effort of the community's health committee; it however confirms the well-known fact that access to and quality of health services are better in the urban communities. The community health committee found it difficult to fully stop the truancy among the health workers, as 20.5% of the respondents in our rural community were unable to immunize their children due to the absence of the vaccinator. This is a common and widespread problem in Nigeria, especially in the rural and riverine communities of the Niger delta.1,17 Rural and riverine communities like Ondewari are difficult to live and work in, because of the near absence of social amenities, but that also explains why the health workers were recruited from the communities, and therefore should not have problem living in their indigenous communities. Truancy amongst health workers can however be solved with the greater involvement of the community in the management of the health centers, including the discipline of erring workers.18 A study in Kogi State, north-central Nigeria showed that the involvement of the community in the evaluation of health workers is significantly associated with greater productivity per staff, in providing inpatient deliveries, immunizations, and outpatient consultation.18
The nonavailability of vaccine was as expected more of a problem in our rural community, and shows the greater logistic problem faced in getting vital medical supplies to had to reach communities.2,18 It is however not peculiar to the rural communities, as 5.5% of the respondents in our urban community could not immunize their children for the same reason. It was also an identified problem in other communities in Nigeria, and blamed on several factors including the huge cost of childhood immunization in Nigeria.1 Nigeria's immunization program was said to be the most expensive among developing countries, costing up to $226 per fully immunized child.1
CONCLUSION
The immunization coverage in our rural community was surprisingly better than that of the urban community. This can be attributed to the better mobilization and participation of the rural community in the delivery of immunization services. Greater emphasis should therefore be placed on community mobilization and participation in the effort to eradicate polio, and achieve universal childhood immunization coverage.
ACKNOWLEDGMENT
We wish to thank the Chiefs, members of the Community Development Committee and the entire people of study communities for their assistance and cooperation during the study. We also wish to thank Professor BC Didia for his comments. We however wish to state that the opinions expressed in this article are entirely ours.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.The State of Routine Immunization Services in Nigeria and Reasons for Current Problems. Abuja, Nigeria: DFID; 2005. FBA Health Systems Analysts. [Google Scholar]
- 2.Adeiga A, Omilabu SA, Audu RA, Sanni FA, Lakehinde GF, Balogun O, et al. Infant immunization coverage in difficult-to-reach area of Lagos metropolis. Afr J Clin Exp Microbiol. 2005;6:227–31. [Google Scholar]
- 3.State of the world's vaccines and immunization. 3rd ed. Geneva: World Health Organization; 2009. WHO, UNICEF, World Bank. [Google Scholar]
- 4.Nigeria Demographic and Health Survey 2008. Calverton, Maryland: USAID; 2009. National Population Commission (Nigeria) and ORC Macro; pp. 20–2. [Google Scholar]
- 5.Shimp L. Published by the Basic Support for Institutionalizing Child Survival Project (BASICS II) for the United States Agency for International Development. Arlington, Virginia: BASICS II; 2004. Strengthening Immunization Programs: The Communication Component. [Google Scholar]
- 6.Declaration of Alma-Ata. International conference on primary health care. USSR: Alma-Ata; 1978. Sep 6-12, WHO. [PubMed] [Google Scholar]
- 7.Zakus JD, Lysack CL. Revisiting community participation. Health Policy Plan. 1998;13:1–12. doi: 10.1093/heapol/13.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Cassell JA, Leach M, Fairhead JR, Small M, Mercer CH. The social shaping of childhood vaccination practice in rural and urban Gambia. Health Policy Plan. 2006;21:373–91. doi: 10.1093/heapol/czl020. [DOI] [PubMed] [Google Scholar]
- 9.Atkinson J, Vallely A, Fitzgerald L, Whittaker M, Tanner M. The architecture and effect of participation: A systematic review of community participation for communicable disease control and elimination.Implications for malaria elimination. Malar J. 2011;10:225. doi: 10.1186/1475-2875-10-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akande AA, Akande TM. Polio eradication in Nigeria: controversies and way forward. Afr J Clin Exp Microbiol. 2006;7:173–9. [Google Scholar]
- 11.Babalola S, Adewuyi A. Factors Influencing Immunization Uptake in Nigeria: A Theory-based Research in Six States. Abuja: PATHS; 2005. [Google Scholar]
- 12.Araoye MO. Research methodology with statistics for health and social sciences. Ilorin: Nathandex Publishers; 2003. [Google Scholar]
- 13.Odiit A, Amuge B. Comparison of vaccination status of children born in the health units and those born at home. East Afr Med J. 2003;80:3–6. doi: 10.4314/eamj.v80i1.8658. [DOI] [PubMed] [Google Scholar]
- 14.Nair TN, Varughese E. Immunization coverage of infants: Rural-urban difference in Kerala. Indian Pediatrics. 1994;31:139–43. [PubMed] [Google Scholar]
- 15.Owais A, Hanif B, Siddiqui AR, Agha A, Zaidi AK. Does improving maternal knowledge of vaccines impact infant immunization rates? A community based randomized-controlled trial in Karachi, Pakistan. BMC Public Health. 2011;11:239. doi: 10.1186/1471-2458-11-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Antai D. Migration and child immunization in Nigeria: individual- and community-level contexts. BMC Public Health. 2010;10:116. doi: 10.1186/1471-2458-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United Nations Development Programme (UNDP): Niger Delta Human Development Report: A History of Derivation Formula. UNDP. 2006 [Google Scholar]
- 18.Das-Gupta M, Gauri V, Khemani S. Decentralised delivery of primary health services in Nigeria: Survey evidence from the States of Lagos and Kogi. Geneva: Development Research Group, The World Bank; 2004. [Google Scholar]


