Abstract
Background:
The availability of intraoperative fluoroscopy and improved access to varieties of spinal titanium implants has revived posterior spinal stabilization techniques with their distinct advantages. Our aim is to describe the profile of various spine pathologies requiring subaxial posterior spinal decompression, stabilization (using titanium implants), and arthrodesis, and to determine the rate of postoperative complications and factors affecting outcome.
Materials and Methods:
This is a prospective single institution study of consecutive adult patients seen during the study period. Data collected included the patients’ demographics, radiological findings, indication for surgery, surgical procedure, operation time, intraoperative blood loss, and postoperative complications.
Results:
There were 26 patients (15 males and 11 females). Their ages ranged between 24 and 78 years (median = 42 years). The most common indications for surgery were spinal trauma and degenerative spine disease (24 patients). The region that was most commonly stabilized was the lumbar- 12 cases (46.2%). No patients experienced neural or vascular injury as a result of screw position; likewise no patient had screw loosening. There was a case each of superficial surgical site infection and transient cerebrospinal fluid leak but no case of implant failure was encountered. The outcome was significantly associated with the etiology (0.030) of the indication for surgery and preoperative power grade (0.000).
Conclusion:
Spinal trauma and degenerative spine disease are the two most common indications for posterior spinal decompression, stabilization and fusion in our center. It is associated with acceptable postoperative complication rate when done under fluoroscopic guidance. Outcome is related more to the preoperative neurological deficit and etiology of the indication for surgical stabilization.
Keywords: Expansive laminoplasty, lateral mass screw, pedicle screws
INTRODUCTION
The three-column concept of the spine as developed by Denis is widely used as the conceptual framework for diagnosing acute overt spinal instability.1 Although originally devised based on a retrospective review of traumatic injuries to the thoracic and lumbar spine, it is now also applied to the subaxial (below C2) cervical spine and to nontraumatic instability. The clinical manifestation of spinal instability falls into three major categories: Neurological deficit (from spinal cord, cauda equina, or nerve root compression), pain and/or incapacitating deformity. Virtually any type of disease affecting the bones, discs, joints, or ligamentous support structures of the spine can produce spinal instability. These may be congenital or acquired (traumatic, degenerative, tumors, infections, inflammatory diseases, connective tissue disorders, postsurgical).
The last four decades have witnessed an increased understanding of spinal biomechanics, bone fusion techniques, development of different spinal instrumentation devices, advances in refinement of approaches to the spine, and evolvement of minimally invasive methods; all these have made it possible to stabilize virtually every segment of the spine successfully, regardless of the offending pathology. Hence, the use of spinal instrumentation has increased. The main question in modern spine surgery is ‘When to fuse’and not ‘How to fuse’.
Surgical approach to the spine might be simply classified into anterior, posterior or the combined approaches. Each has its role and the choice of the best approach depends on several factors, such as the level of the disease, extent of the lesion, need of spinal reconstruction or stabilization and competence of the surgeon. For the posterior approach, pedicle fixation is the gold standard. It traverses all three columns of the vertebrae with rigid fixation and control of all the three columns; however anterior column support is added if there is an inadequate anterior column support. The rigidity of pedicle fixation allows for the incorporation of fewer normal motion segments so as to achieve stabilization of an abnormal level and there are less requirements for postoperative bracing and improvements in fusion rates as compared with nonoperative management. The drawbacks are steep learning curve, caudal or medial penetration of the pedicle cortex which can result in dural or neural injury, extensive tissue dissection to expose the entry points of the screws, and to provide the required lateral to medial orientation for optimal screw trajectory, lengthy operative time with potential for significant blood loss, increased risk of infection, and costly procedures. However, minimally invasive techniques in spinal surgery (not yet possible in the country) are increasing in popularity due to numerous potential advantages, including reduced length of hospital stay, blood loss and requirements for postoperative analgesia as well as earlier return to work.2 Posterior cervical lateral mass screw fixation has been widely used for the management of cervical instabilities caused by trauma, neoplasm, degenerative disease or failed anterior fusion.3 Several studies of the safety and the biomechanical stability of the posterior cervical lateral mass screw have been published; and the application of the posterior lateral screw fixation method became easier as a result of the development of the polyaxial screw-rod system.4–7 Expansive laminoplasty is a quick and effective form of cervical decompression. Another major reason for advocating laminoplasty has been to prevent postoperative kyphotic deformity of the cervical spine and formation of the postlaminectomy membrane which is sometimes seen after laminectomy. This membrane might be prevented by preserving the posterior spinal elements. Several series with follow-up periods of up to 4 years have reported preservation of spinal alignment in patients who had straight, sigmoid, or kyphotic cervical spines before surgery.8,9
There has been steady and progressive advancement in spine stabilization techniques in Nigeria with the availability of magnetic resonance imaging (MRI), intraoperative fluoroscopy, and prompt access to spinal titanium implants. There is presently no study examining the use of these techniques in our environment. We decided to study the profile of various spine pathologies requiring subaxial posterior spinal decompression, stabilization (using titanium implants), and postero-lateral fusion, and determine the rate of postoperative complications and factors affecting outcome.
MATERIALS AND METHODS
We carried out a prospective study of adult patients needing posterior spinal decompression and stabilization over a 16-month period (April 2010 to July 2011). The patients presented to the Neurosurgery unit of the Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria. Lagos State (a conurbation of cities) is the most populous state in Nigeria, a West African country which is the most populous country in Africa.
The preoperative evaluation included Magnetic resonance imaging (MRI) in all patients. A careful assessment of pulmonary and cardiac function was undertaken preoperatively. Concerns during anesthesia and positioning, like hemodynamics (drop in cardiac output), respiration and positioning injuries (iliac crest, genitals, upper chest, forehead/chin) were strictly looked for and prevented. Pressure on the abdomen was avoided and adequate support and padding of at risk areas including the eyes were ensured. Intraoperative localization of the bony level was done with spot fluoroscope. Planning and good communication between the anesthetist and surgeon was ensured prior to surgery and throughout the procedure. Neither autologous blood transfusion using a cell saver nor intraoperative somatosensory evoked potential monitoring was used for any of the surgeries because these facilities were not available. Closed suction drains were routinely placed intraoperatively just prior to wound closure. The patients were required to sit out of bed first day after surgery and to commence ambulation with the help of the physiotherapist 5 days after surgery with a thoracic, lumbar or thoracolumbar orthosis, or a rigid cervical collar in order to reduce spine motion. The orthosis was worn for up to 6 weeks after surgery, and a soft brace was recommended for additional 12 weeks. The minimum follow-up was 6 weeks.
Exclusion criteria were recent loco-regional infection, 1-3 vertebrae level decompressions that will not cause spinal instability (facets preserving surgery), fusions which are normally successful without fixation (no features of spinal instability), metal allergy, inadequately sized pedicles, pedicles compromised by fractures and lack of anterior column support.
Data concerning the patients’ demographics, pre- and post-operative power grade (most predominant power in the affected limbs), radiological findings, surgical indication, surgical procedure, fixation levels, intraoperative time, and postoperative complications were collected and analyzed. The intraoperative blood loss during surgery and blood transfusions were also noted. Surgical outcome measures consisted of postoperative complication rate and motor function gain. Outcome was classified as poor (power grade 0-1), fair (power grade 2-3), and good (power grade 4-5). The minimum follow-up period was 6 weeks. The data were stored electronically and subsequently analyzed. Two-tailed probability values, as calculated using the Fisher exact test, were used to assess the significance of outcome. The level of significance was set at P=0.05. All analysis was performed using statistical package for the social sciences (SPSS) advanced statistics software, version 17.0.
RESULTS
There were 26 patients (15 males and 11 females). Their ages ranged between 28 and 78 years (median=42 years). The most common indications for surgery were spinal trauma and degenerative spine disease (24 patients). The stabilization procedures done were pedicle screws with rods, expansive single-door miniplate laminoplasty (keeping the lamina open with titanium plates), and lateral mass screws with rods in 17, 5, and 4 patients respectively [Table 1]. The lumbar region was fixed in 12 cases (46.2%), cervical in 9 cases (34.6%), and the thoracolumbar region in 5 patients (19.2%).
Table 1.
Type of surgery and etiology of spinal pathology

Mean operative time was 217 minutes ranging between 90 minutes and 310 minutes. Longer operative times and higher blood loss were recorded for procedures that necessitated multilevel decompression and pedicle screw insertion [Table 2]. Only two patients had whole blood transfusion.
Table 2.
Age, operation time, and blood loss following stabilization

All cases of the lateral mass screws were performed with polyaxial screw-rod constructs. The screws were inserted using the modified Magerl trajectory. Most patients had 14-16 mm length and 3.5 mm diameter screws. No patients experienced neural or vascular injury as a result of screw position; likewise no patient had screw pullouts. There was one case each of superficial surgical site infection and transient cerebrospinal fluid leak, but no case of new postoperative neurological deficit or implant failure occurred. There was one case of peri-operative mortality. This patient had traumatic cervical myelopathy and died from undetected blocked endotracheal tube, third day after surgery (lateral mass screws with rods).
There was significant association between outcome and etiology of the disease (P=0.030) and preoperative power grade (0.000) [Table 3], but no significant association between outcome and gender (0.855), level of fixation (0.315), and type of surgical procedure (P=0.615) [Table 4]. Age was also not significantly associated with the type of surgery (P=0.299), preoperative power grade (0.530), postoperative power grade (0.973) or outcome of the patients (P=0.657) [Figure 1].
Table 3.
Pre- and post-operative motor level

Table 4.
Gender, etiology, surgery type, transfusion and pre-op power of the patients and relation to outcome

Figure 1.
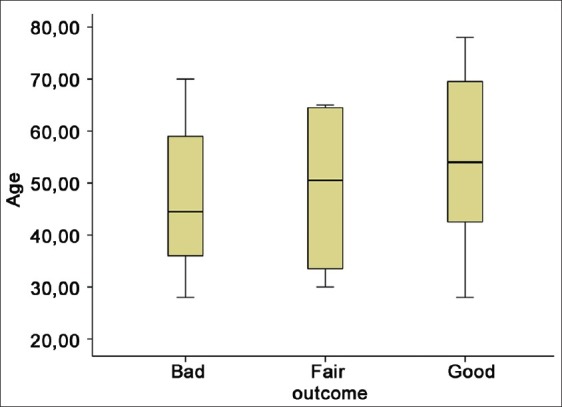
Relationship between age and surgical outcome
DISCUSSION
Spinal fusion and instrumentation were developed and applied as independent techniques for treatment of spinal instability in the first half of the 20th century. By the turn of the 20th century, spinal instrumentation, which mostly consisted of wiring of posterior elements, was employed sporadically for treatment of spine fractures. This method was first employed by Berthold Hadra in 1891.
Pedicle screw fixation is the most commonly used approach for internal stabilization of the lumbar spine [Figure 2]. Screws are inserted into the pedicles of the vertebrae to be fused and connected to each other with bilateral rods or plates. Pedicle screw fixation traverses all three columns of the vertebrae. It represents the strongest point of attachment of the spine and thus significant forces can be applied to the spine without failure of the bone-metal junction. The rigidity of pedicle fixation allows for the incorporation of fewer normal motion segments in order to achieve stabilization of an abnormal level and there are less requirements for postoperative bracing and improvements in fusion rates. The disadvantages include a steep learning curve, caudal or medial penetration of the pedicle cortex resulting in dural or neural injury, extensive tissue dissection to expose the entry points, lengthy operative time with potential for significant blood loss and increased risk of infection, and costly procedures. A combination of anterior and posterior fixation is suggested in severe destruction of vertebral bodies or gross fracture-dislocation.
Figure 2.

Fluoroscopic picture of lumbar pedicle screws in situ
The advent of minimally invasive techniques in spinal surgery in developed and some developing countries is gaining popularity due to its numerous potential advantages, including reduced length of hospital stay, blood loss, and requirements for post-operative analgesia as well as earlier return to work.2 Additionally, intraoperative navigation in spinal neurosurgery has become standard practice as they increase the accuracy and safety of screw insertion. Multiple studies have proven the advantages and safety of computer-assisted spinal neurosurgery. Intraoperative computerized tomography (CT)-based image guidance for placement of spinal implants has an accuracy that exceeds reported rates with other image guidance systems, such as virtual fluoroscopy and 3D isocentric C-arm-based stereotactic systems.10 Furthermore, with the use of intraoperative CT scanning, a postinstrumentation CT scan allows the surgeon to evaluate the accuracy of instrumentation before wound closure and revise as appropriate. Electromagnetic field (EMF)-based navigation systems are also available to aid more accurate placement of percutaneous pedicle screws while reducing radiation exposure.11
Cervical open-door laminoplasty was first developed by Hirabayashi. He and some other authors have reported many methods concerning laminoplasty.12,13 In general, there are two major laminoplasty techniques, unilateral (open-door) and bilateral (midline opening). Submodifications of laminoplasty include the use of bone graft or instrumentation (miniplates). In the current study we used the technique described by O’Brien et al., using miniplates for fixation of the hinged lamina.14 It is widely regarded as a simple, safe, and cost-effective method for cervical spinal cord decompression. The procedure is also quick and associated with minimal blood loss [Table 2].
The usefulness of lateral mass internal fixation has been well documented in the clinical setting. The polyaxial screw-rod construct using the modified Magerl technique can be used for a variety of cervical spine pathologies with safety and efficiency. No patient in our series experienced spinal cord, neural or vertebral artery injury as a result of screw position. There was no case of surgical site infection amongst this group of patients; neither were there any screw pullouts or mechanical implant failures requiring removal of implants. Our study is similar to the findings of Al Barbarawi et al. and Katonis et al.15,16 These studies show that lateral mass fixation can be used safely with minimal complications and a low rate of morbidity for the treatment of cervical myelopathy.
In the 1950s, Paul Harrington pursued his historic work on correction of idiopathic and post-polio scoliosis by applying a combination of compression and distraction hooks and rods to the thoracolumbar spine.17 The success of the Harrington rod system with deformity correction led to its subsequent use for treatment of overt spinal instability (e.g., post-traumatic instability). However, it soon became apparent that the application of spinal instrumentation (without fusion) for treatment of spinal instability often ended in breakage or loosening of the hardware (hardware failure). Harrington later expressed the idea that there is a “race between instrumentation failure and acquisition of spinal fusion.” This principle and the realization that the problems of pseudarthrosis and hardware failure could be resolved if bone grafting and instrumentation were used simultaneously laid the basis of modern spine stabilization surgery. In current practice, bone grafting and instrumentation are often used concurrently based on the expectation that internal fixation of spine enhances the success of bone fusion while a successful bone fusion eliminates the possibility of hardware failure by reducing the chronic biomechanical stresses on the hardware construct. The mode of fusion in our series was postero-lateral fusion. This was added to the stabilization technique in all cases with autologous bone graft.
An adequate preoperative evaluation, accurate surgical planning, constant communication with the anesthetist and careful surgical technique are key to achieving good outcomes and to appreciably reduce the risk of complications. Cerebrospinal fluid (CSF) leaks can occur as a result of spine surgery or trauma. These leaks represent serious problems because of persistent headaches and the possibility of meningitis. Surgical management is often needed and requires meticulous direct closure of the dura or closure by means of a fascial graft.18 A successful repair usually follows the use of fascial graft, fibrin glue, gelatin sponge, lumbar CSF drainage, and bed rest. We had one patient with iatrogenic CSF leak which was not noticed intraoperatively. It was managed by nursing the patient in a prone position for 10 days with resolution of the leak.
In summary, spinal trauma and degenerative spine disease are the two most common indications for posterior spinal decompression, stabilization and fusion in our center. These procedures are associated with minimal postoperative complications when performed under fluoroscopic guidance. Good outcome is mainly related to the preoperative neurological deficit and the etiology. The lack of cell savers or intraoperative neuromonitoring with somatosensory evoked potentials does not preclude a successful surgery. The above procedures should be part of the surgical armamentarium in our environment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1984;189:65–76. [PubMed] [Google Scholar]
- 2.Mobbs RJ, Sivabalan P, Li J. Techniques, challenges and indications for percitaneous pedicle screw fixation. J Clin Neurosci. 2011;18:741–9. doi: 10.1016/j.jocn.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 3.Jeanneret B, Magerl F, Ward EH, Ward JC. Posterior stabilization of the cervical spine with hook plates. Spine (Phila Pa 1976) 1991;16(3 Suppl):S56–63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 4.Coe JD, Warden KE, Sutterlin CE, 3rd, McAfee PC. Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine (Phila Pa 1976) 1989;14:1122–31. doi: 10.1097/00007632-198910000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Deen HG, Birch BD, Wharen RE, Reimer R. Lateral mass screw-rod fixation of the cervical spine: A prospective clinical series with 1-year follow-up. Spine J. 2003;3:489–95. [PubMed] [Google Scholar]
- 6.Joseffer SS, Post N, Cooper PR, Frempong-Boadu AK. Minimally invasive atlantoaxial fixation with a polyaxial screw-rod construct: Technical case report. Neurosurgery. 2006;58(4 Suppl 2):ONS-E375. doi: 10.1227/01.NEU.0000208955.12461.C7. discussion ONS-E375. [DOI] [PubMed] [Google Scholar]
- 7.Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J. 2007;16:479–84. doi: 10.1007/s00586-006-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hidai Y, Ebara S, Kamimura M, Tateiwa Y, Itoh H, Kinoshita T, et al. Treatment of cervical compressive myelopathy with a new dorsolateral decompressive procedure. J Neurosurg. 1999;90(2 Suppl):178–85. doi: 10.3171/spi.1999.90.2.0178. [DOI] [PubMed] [Google Scholar]
- 9.Chiba K, Toyama Y, Watanabe M, Maruiwa H, Matsumoto M, Hirabayashi K. Impact of longitudinal distance of the cervical spine on the results of expansive open-door laminoplasty. Spine (Phila Pa 1976) 2000;25:2893–8. doi: 10.1097/00007632-200011150-00010. [DOI] [PubMed] [Google Scholar]
- 10.Tormenti MJ, Kostov DB, Gardner PA, Kanter AS, Spiro RM, Okonkwo DO. Intraoperative computed tomography image-guided navigation for thoracolumbar spinal instrumentation in spinal deformity surgery. Neurosurgery Focus. 2010;28:E11. doi: 10.3171/2010.1.FOCUS09275. [DOI] [PubMed] [Google Scholar]
- 11.von Jako R, Finn MA, Yonemura KS, Araghi A, Khoo LT, Carrino JA, et al. inimally invasive percutaneous transpedicular screw fixation: Increased accuracy and reduced radiation exposure by means of a novel electromagnetic navigation system. Acta Neurochir (Wien) 2011;153:589–96. doi: 10.1007/s00701-010-0882-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8:693–9. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Miyazaki K, Kirita Y. Extensive simultaneous multisegment laminectomy for myelopathy due to the ossification of the posterior longitudinal ligament in the cervical region. Spine (Phila Pa 1976) 1986;11:531–42. doi: 10.1097/00007632-198607000-00005. [DOI] [PubMed] [Google Scholar]
- 14.O’Brien MF, Peterson DP, Casey ATH, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium mini-plate stabilization. A computerized morphometric analysis. Spine (Phila Pa 1976) 1996;21:474–84. doi: 10.1097/00007632-199602150-00012. discussion 484. [DOI] [PubMed] [Google Scholar]
- 15.Al Barbarawi MM, Audat ZA, Obeidat MM, Qudsieh TM, Dabbas WF, Obaidat MH, et al. Decompressive cervical laminectomy and lateral mass screw-rod arthrodesis. Surgical analysis and outcome. Scoliosis. 2011;6:10. doi: 10.1186/1748-7161-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katonis P, Papadakis SA, Galanakos S, Paskou D, Bano A, Sapkas G, et al. Lateral Mass Screw Complications: Analysis of 1662 Screws. J Spinal Disord Tech. 2010;24:415–20. doi: 10.1097/BSD.0b013e3182024c06. [DOI] [PubMed] [Google Scholar]
- 17.Harrington PR. The history and development of Harrington instrumentation. Clin Orthop Relat Res. 1973;93:110–2. doi: 10.1097/00003086-197306000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Chauhan C, Frances GA, Kemeny AA. The avoidance of surgery in the treatment of subarachnoid cutaneous fistula by the use of an epidural blood patch: Technical case report. Neurosurgery. 1995;36:612–3. doi: 10.1227/00006123-199503000-00025. discussion 613-4. [DOI] [PubMed] [Google Scholar]


