Abstract
Objective:
The main aim of this study was to assess knowledge, attitude, and practice of university faculty members and high school teachers regarding irrational antibiotic use and self-medication.
Methods:
In this cross-sectional survey, 320 university teaching staff and 150 high school teachers received a questionnaire that assessed their knowledge, attitude, and practice regarding the use of antibiotics and self-medication. The reliability of the questionnaire was assessed with Cronbach's alpha internal consistency coefficient and the results were analyzed with the Mann-Whitney U test. Spearman's correlation coefficient was used to determine the correlation between knowledge, attitude, and practice.
Results:
The questionnaires were completed by 134 university faculty members and 308 high school teachers, among whom 35.8% and 47.1%, respectively, reported self-medication with antibiotics during the previous year, mostly to relieve sore throat. High school teachers were significantly better than university teaching staff in their knowledge about the effects of antibiotics and in their usage practices. In both the groups, a weak direct linear relationship was detected between attitude and practice (r=0.243, r=0.238, P<0.01) and a weak inverse linear relationship was seen between knowledge and practice (P=0.22) in the high school teacher group.
Conclusions:
Our results showed that self-medication and the irrational use of antibiotics were common among highly educated people in a community population sample in Shiraz, Iran. The rational use of antibiotics may be favored by improving knowledge about these drugs.
Keywords: Academic staff, antibiotic, attitude, knowledge, practice, self-medication
INTRODUCTION
Although antimicrobial agents are used worldwide and their effectiveness is unquestionable, antibiotic misuse causes avoidable expense, adverse drug reactions, interactions, and resistance.[1–4] The adverse effects of the irrational use of antibiotics include enteropathy (irritable bowel syndrome, antibiotic-associated diarrhea), long-term illness, and high mortality rate.[4–8]
Self-medication with antibiotics which we studied here involves the use of antibiotics without a prescription for self-diagnosed or recurrent illnesses.[9]
Self-medication with antibiotics occurs worldwide,[6,8,10–13] especially in developing countries.[12] The prevalence is widespread, ranging from 9.5% in Slavonia,[14] 22% in Lithuania,[15] and 77.2% in Vietnam.[16] Different studies have identified various determinants of antibiotic self-medication, such as educational level,[14,17] sex,[14] age group,[14] lack of health insurance,[11,17] over-the-counter sale of antibiotics,[11,18] unused previous prescriptions at home,[19] type of illness,[20] cost of medical consultation,[11] and knowledge and attitude towards the consequences of self-medication.[21]
Surveys have shown that attitudes toward antibiotics differ among countries due to variations in culture, habits, education, and health care organization.[2] According to our literature review, no survey to date has addressed the knowledge, attitude, and practice toward antibiotic self-medication in Iranian highly-educated teaching professionals; so we designed the present study to investigate the relationship between mentioned factors in a community sample of this stratum.
METHODS
Design and setting
This cross-sectional study was done in Shiraz, the fourth-largest city of Iran, in 2009. After the participants were given explanatory information, they were asked to provide their oral consent for participation. Then participants completed an anonymous, self-administered questionnaire. The participants were 150 university teaching staff members (excluding physicians, dentists, and pharmacologists) selected by stratified random sampling (proportionate to size) among 700 faculty members at three universities for sciences, fine arts, and medical sciences, and 320 secondary school teachers, from a total of 2000, selected by random cluster sampling. We used different sampling methods because faculty members worked at only three locations and interviewing them was straightforward, whereas high school teachers worked at centers disseminated widely across the city which made face-to-face contacts time-consuming in a widespread distribution.
Data collection
Data were collected with a questionnaire designed by the first author (MA). Content validity was verified by two community medicine specialists. The reliability of the questionnaire was tested in a pilot study with 15 university faculty members and 35 high school teachers with a Cronbach's alpha=0.80. The questionnaire consisted of four parts: Social and demographic, knowledge, attitude, and practice. The demographic part solicited information about age, sex, field of study, and academic rank for university faculty members (instructors, assistant, associate and full professors) or highest degree obtained (BS, MSc or other) for high school teachers. In the second and third parts, we originally provided three-category responses for attitude and knowledge items (correct, incorrect, and I don’t know) and in the fourth part (practice-related items), we originally provided two-category responses (yes, no). On analysis, we dichotomized the responses for practice-related items into “yes” (score 1) and “no” (score 0) answers.
Because there were 16 questions in this part, minimum and maximum scores for the practice part were 0 and 16 (the higher the score, the higher the rate of self-medication with antibiotics). The scores for attitude-related items ranged from three (for an “incorrect” response) to one (for a “correct” response). Because there were 15 possible responses in two items, the scores ranged from 15 to 45. Higher scores indicated an increasingly favorable attitude toward using antibiotics without a prescription. In the knowledge part, we dichotomized correct responses as one and incorrect responses as zero. Accordingly, minimum and maximum scores were zero and nine, respectively. Higher scores in this part indicated increasing knowledge of the consequences of irrational antibiotic use. The first question in the practice part was used to determine whether self-medication with antibiotics had occurred within the previous year.
Statistical analysis
The data were analyzed with Statistical Package for the Social Sciences (SPSS) V. 13.5 software. We used the Mann-Whitney U test to identify differences in knowledge, attitude, and practice between sexes, and between university faculty members and high school teachers. Pair-wise correlation coefficients were calculated to determine the relationships between different items. Spearman's correlation coefficient was used to recognize the correlation between knowledge, attitude, and practice. Differences with a P value less than 0.05 were considered statistically significant.
RESULTS
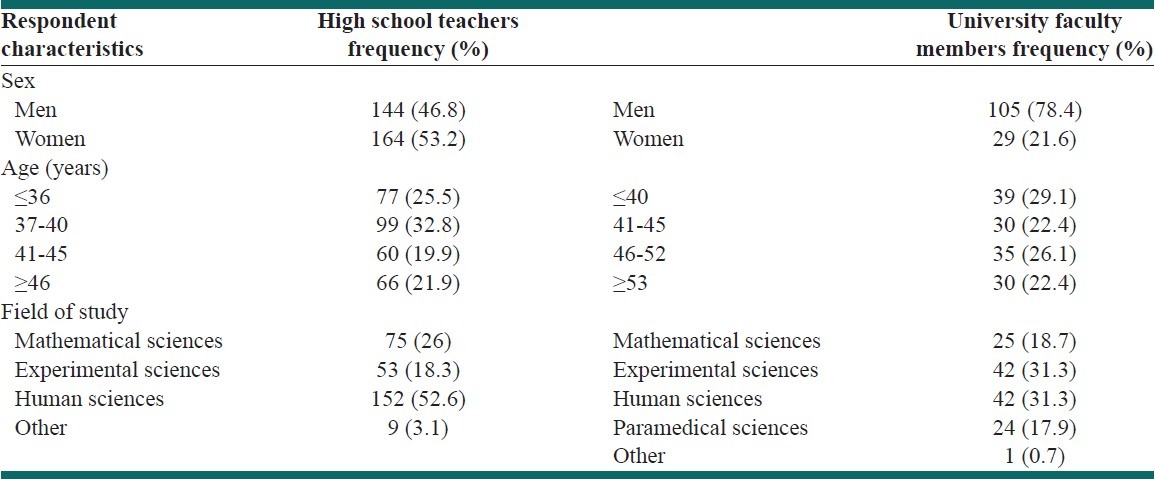
In the sample of high school teachers, 308 out of 320 (96.25%) participants returned questionnaires, and in the faculty group, 134 out of 150 (89.33%) returned questionnaires. Of the entire sample, 249 (56.3%) of the respondents were men. Most participants in the faculty group were men (104 individuals, 78.4%), but in the teacher group women predominated (164 individuals, 53.2%). Mean age (±SD) was 40.2 (±6.48) years among teachers and 45.93 (±9.08) years among the faculty members. Other demographic data are displayed in [Table 1].
Table 1.
Distribution of demographic characteristics in the study population
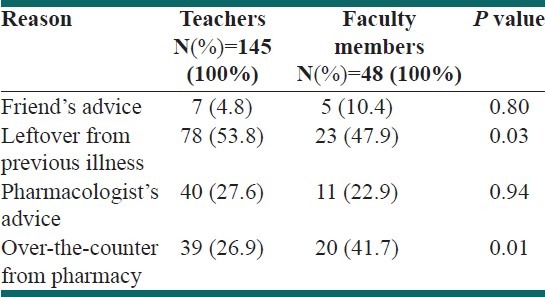
Among all the 442 respondents, 193 (43.7%) reported self-medication with antibiotics during the last year. In teacher and faculty groups, 145 (47.1%) and 48 (35.8%) participants reported self-medication, respectively. The difference between the groups was statistically significant (P=0.028). There was no correlation between respondents’ sex and self-medication with antibiotic (P=0.57). Also, no correlation was found between academic rank of university faculty member and self-medication with antibiotic (P=0.07) and neither does academic degree of high school teachers (P=0.188). The reasons participants reported for using nonprescription antibiotics were a friend's advice (12, 6.2%), leftover antibiotics from a previous illness (101, 52.3%), a pharmacologist's advice (51, 26.4%), and a pharmacist's compliance with a request for a specific antibiotic (59, 30.6%) [Table 2].
Table 2.
Reasons for self-medication with antibiotics
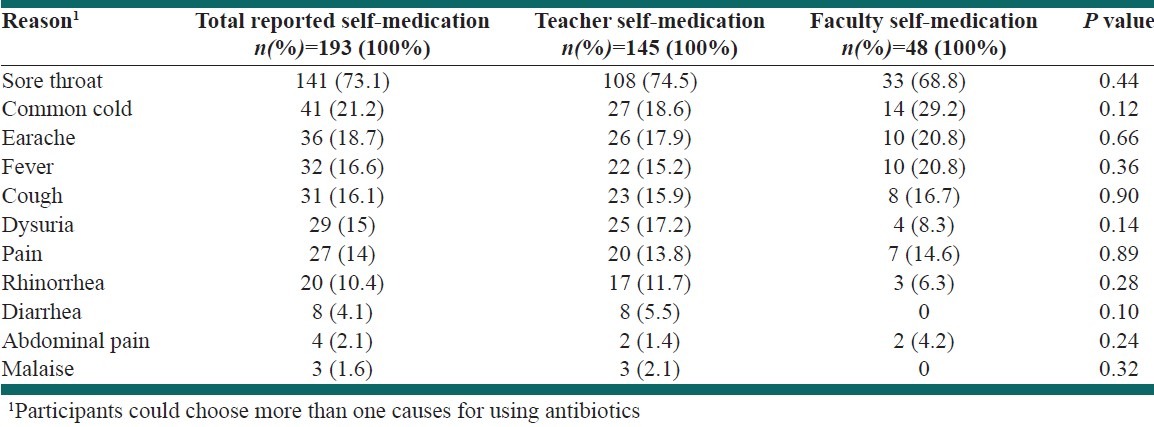
The most common causes of self-medication with antibiotics were sore throat (73.1%) and the least common cause was malaise (1.6%). No significant differences were seen between teachers and faculty members in the causes for using antibiotics without a prescription [Table 3].
Table 3.
Frequencies of common causes for using antibiotics
We also asked participants to indicate their knowledge, attitude, and practice in self-medication with antibiotics during the previous year. The responses revealed that teachers and faculty members differed significantly in knowledge (P=0.008), attitude (P=0.04), and practice (P<0.001). Teachers scored better in knowledge (median 7 in both group, mean 7.03 vs. 6.59) and attitude (median 24 vs. 23, mean 24.9 vs. 23.2) regarding the consequences of self-medication with antibiotics, although this difference may not have been clinically significant. In daily life, however (i.e., in actual practice), the irrational use of antibiotics was more common among teachers (median; 3 vs. 2) [Table 4].
Table 4.
Knowledge, attitude and practice in the irrational use of antibiotics
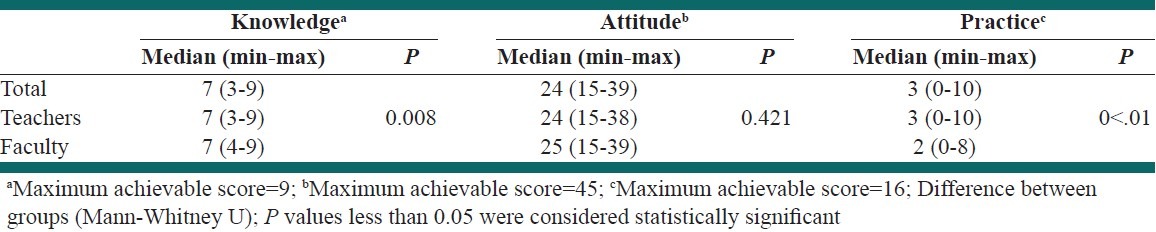
A total of 135 out of 308 (43.8%) teachers and 56 out of 134 faculty members (41.7%) achieved an acceptable score (i.e., 7) for knowledge about the consequences of administrating antimicrobial agents without a prescription. In the attitude part, 190 out of 308 teachers (61.6%) and 80 out of 134 (59%) faculty members who responded obtained an acceptable scores (i.e., 15) in attitude toward the irrational use of antibiotics. In the teacher group, we found a weak inverse correlation between knowledge and practice (r=–0.218). A weak direct correlation between attitude and practice was found in both teachers (r=0.343) and faculty members (r=0.238).
DISCUSSION
Selecting an appropriate antibiotic is the main concern in modern medicine and is strongly dependent on the correct diagnosis of the disease and adequate knowledge of antimicrobial issues.[1] Using antibiotics without considering these factors is the main cause of the emergence of resistant microorganisms, a phenomenon that contributes to excessive costs in health services.[1,6] Unfortunately, despite antimicrobial policies which restrict the availability of antimicrobial agents, self-medication with antibiotics is still highly prevalent.[2,5,22]
Prior to any intervention for promoting rational antibiotic administration, it is necessary to determine the prevalence of self-medication and the factors that contribute to this practice. Because these issues are specific for each country, estimating the magnitude of the problem with due regard for locally important factors seems necessary. In this study, we examined a sample of high school teachers and university faculty members mainly because we had no data for these groups and also because they are representative of the educated sectors of Iranian society. We hypothesized that their knowledge, attitude, and practice scores would be higher than in other types of population-based samples. Overall, the rate of self-medication with antibiotics during the preceding year in our sample was 43.7% (47.1% among teachers and 35.8% among faculty). These rates are better than the results reported by Buke et al.[7] in a survey of faculty members (64.5%) and in a sample of university students[23] (44.1%). Our rates are also relatively in concordance with rates reported by Sarahroodi and her colleagues in Iranian medical students (42.2%) and in Iranian non-medical students (48%).[24] However, our figures were relatively higher than the results obtained from surveys of the lay population in the United Arab Emirates (56.3%),[5] Sudan(48.1%),[25] Turkey (44.1%),[23] Europe (41%),[26] Israel (36.2%),[27] Vietnam (29.8%),[28] Spain (28%),[28] and Sweden (16.8%).[13]
Because teachers and faculty members are mentors for their students and a source of knowledge in society, the rates we found are disappointing. Surprisingly, self-medication with antibiotics is common among educated groups,[17] probably because of better access to the internet and pharmaceutical handbooks. In addition, other contributing factors noted by our participants and those of other studies were leftover antibiotics from a previous illness,[2,5,6,8,10,13,27,29–31] a friend's advice,[27] consulting with a pharmacist,[5,23,28,30] poor access to doctors,[6] and availability of over-the-counter antibiotics.[5,8,18,25,26] However, informal strategies which facilitate access to antibiotics, such as purchasing antibiotics via the internet, and over-the-counter purchases abroad,[5,6] can also play important roles.
In concordance with the results of other surveys,[7,8,10,11,23,24,26,30,31] our participants reported sore throats (73.1%) and common colds (21.2%) as major reasons for self-medication with antibiotics. Interestingly, Iran people believe that acute rheumatic fever usually results from an untreated sore throat, so they use antibiotics even if doctors reassure them that they are ineffective. The use of antibiotics for minor ailments like common colds shows that even members of the educated stratum of our society are unaware of the consequences of irrational antibiotic use and bears witness to the suboptimal effectiveness of regulations for antibiotic accessibility. These findings are not limited to our community.[5,11] Other studies reported different diseases and symptoms as major reasons for self-treatment with antibiotics, such as influenza,[5,32] upper respiratory infection,[22,29] bronchitis,[11,30,31] fever,[23] cough,[28,31] and teeth or gum symptom.[30]
Most of the participants in our survey attained good scores for knowledge, attitude, and practice in relation to antibiotic administration and claimed that they were careful about antibiotic use. However, self-medication with antibiotics was reported by about 43.7%. We estimated self-medication with antibiotics on the basis of the participants’ response to the question, “Have you ever used antibiotics for your children or yourself during the last year?” The divergence instated and actual practice may reflect the use of antibiotics without consulting a doctor on only one or two occasions during the previous year, even though the participants had adequate knowledge of and an appropriate attitude toward the consequences. Among our participants, better knowledge did not result in better attitude and practice, in contrast to the findings of earlier studies.[23,33]
Our survey had some limitations typical of population-based questionnaire surveys. One such limitation was the reliance on self-reported rather than observed antibiotic use. We used a cross-sectional method in view of the absence of data on knowledge, attitude, and practice regarding self-medication with antibiotics in Iran. Further research based on a prospective observational design should help to overcome this limitation. Moreover, our sample was confined to high school teachers and faculty members who are not representative of the entire Iranian population. To improve the generalizability, a random cluster sampling strategy to represent the entire population of Iran would be a useful solution.
CONCLUSION
Self-medication with antibiotics is a complex issue affected by various factors. Restricting the accessibility and availability to antibiotics seems essential to solve this problem. This goal might be feasible if regulatory laws[2,5,10,18] are legislated by the government and are accompanied by measures to educate people via the mass media.[2] To reduce self-medication with leftover antibiotics, doctors should prescribe antibiotics for a specific treatment period and should prescribe the exact number of tablets or capsules the patient will need.[10,11,18]
ACKNOWLEDGMENT
This article is the result of a research project approved by the Vice Chancellor for Research of Shiraz University of Medical Sciences. We thank Dr. A.R. Moasser and Dr. M. Banifatemi for their assistance in data collection and K. Shashok for improving the use of English in the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tunger O, Karakaya Y, Cetin CB, Dinc G, Borand H. Rational antibiotic use. J Infect Dev Ctries. 2009;3:88–93. doi: 10.3855/jidc.54. [DOI] [PubMed] [Google Scholar]
- 2.Radosević N, Vlahović-Palcevski V, Benko R, Peklar J, Miskulin I, Matuz M, et al. Attitudes towards antimicrobial drugs among general population in Croatia, Fyrom, Greece, Hungary, Serbia and Slovenia. Pharmacoepidemiol Drug Saf. 2009;18:691–6. doi: 10.1002/pds.1768. [DOI] [PubMed] [Google Scholar]
- 3.Arch G, Mainous AG, Everett CJ, Post RE, Diaz VA, Hueston WJ. Availability of antibiotics for purchase without a prescription on the internet. Ann Fam Med. 2009;7:431–5. doi: 10.1370/afm.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks GF, Butel JS, Morse SA. 22nd ed. New York: McGraw-Hill; 2001. Medical Microbiology. [Google Scholar]
- 5.Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;3:491–7. doi: 10.3855/jidc.466. [DOI] [PubMed] [Google Scholar]
- 6.Mainous AG, Diaz VA, Carnemolla M. Factors affecting Latino adults’ use of antibiotics for self-medication. J Am Board Fam Med. 2008;21:128–34. doi: 10.3122/jabfm.2008.02.070149. [DOI] [PubMed] [Google Scholar]
- 7.Buke AC, Ermertcan S, Hosgor-Limoncu M, Ciceklioglm M, Eren S. Rational antibiotic use and academic staff. Int J Antimicrob Agents. 2003;21:63–6. doi: 10.1016/s0924-8579(02)00272-8. [DOI] [PubMed] [Google Scholar]
- 8.Grigoryan L, Burgerhof JG, Haaijer-Ruskamp FM, Degener JE, Deschepper R, Monnet DL, et al. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. 2007;59:152–6. doi: 10.1093/jac/dkl457. [DOI] [PubMed] [Google Scholar]
- 9.Guidelines for the regulatory assessment of medicinal products for use in self.medication. World Health organization. 2000. [last cited on 2011 Oct 04]. WHO/EDM/QSM/00.1. downloaded 14.3.2011. Available from: http://apps.who.int/medicinedocs/pdf/s2218e/s2218e.pdf .
- 10.Lil J, Wang PS. Self-medication with antibiotics: A possible cause of bacterial resistance. Med Hypotheses. 2005;65:1000–1. doi: 10.1016/j.mehy.2005.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Grigoryan L, Burgerhof JG, Degener JE, Deschepper R, Lundborg CS, Monnet DL, et al. Determinants of self-medication with antibiotics in Europe: The impact of beliefs, country wealth and the healthcare system. J Antimicrob Chemother. 2008;61:1172–9. doi: 10.1093/jac/dkn054. [DOI] [PubMed] [Google Scholar]
- 12.Otoom SA, Sequeira RP. Health care providers’ perceptions of the problems and causes of irrational use of drugs in two Middle East countries. Int J Clin Pract. 2006;60:565–70. doi: 10.1111/j.1742-1241.2005.00808.x. [DOI] [PubMed] [Google Scholar]
- 13.Svensson E, Haaijer-Ruskamp FM, Lundborg CS. Self-medication with antibiotics in a Swedish general population. Scand J Infect Dis. 2004;36:450–2. doi: 10.1080/00365540410020721. [DOI] [PubMed] [Google Scholar]
- 14.Cizman M, HaaijerRuskamp F, Grigoryan L. Self-medication with antibiotics in the general Slovenian population. Int Antimicrob. 2005;26:69. [Google Scholar]
- 15.Berzanskyte A, Valinteliene R, Haaijer-Ruskamp FM, Gurevicius R, Grigoryan L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19:246–53. doi: 10.2478/v10001-006-0030-9. [DOI] [PubMed] [Google Scholar]
- 16.Phuong HL, Vries PJ, Nagelkerke N, Giao PT, Hung LQ, Binh TQ, et al. Acute undifferentiated fever in BinhThuan province, Vietnam: Imprecise clinical diagnosis and irrational pharmaco-therapy. Trop Med Int Health. 2006;11:869–79. doi: 10.1111/j.1365-3156.2006.01636.x. [DOI] [PubMed] [Google Scholar]
- 17.Saradamma RO, Higginbotham N, Nichter M. Social factors influencing the acquisition of antibiotics without prescription in Kerala state, South India. Soc Sci Med. 2000;50:891–903. doi: 10.1016/s0277-9536(99)00380-9. [DOI] [PubMed] [Google Scholar]
- 18.Volpato DE, de Souze BV, Dalla Rosa LG, Melo LH, Daudt CA, Deboni L. Use of antibiotics without medical prescription. Braz J Infect Dis. 2005;9:288–91. doi: 10.1590/s1413-86702005000400004. [DOI] [PubMed] [Google Scholar]
- 19.Richman PB, Garra G, Eskin B, Nashed AH, Cody R. Oral antibiotic use without consulting a physician: A survey of ED patients. Am J Emerg Med. 2001;19:57–60. doi: 10.1053/ajem.2001.20035. [DOI] [PubMed] [Google Scholar]
- 20.Moghadamnia AA, Ghadimi R. Self-medication of patients with common cold among 15-45 year old individuals (BABOL; 1998) Sci J Babol Univ Med Sci. 2000;2:26–32. [Google Scholar]
- 21.Tan YS, Hong CY, Chong PN, Tan ES, Lew YJ, Lin RT. Knowledge that upper respiratory tract infection resolves on its own is associated with more appropriate health-seeking behavior and antibiotic cognition. Singapore Med J. 2006;47:518–24. [PubMed] [Google Scholar]
- 22.Pereira FS, Bucaretchi F, Stephan C, Cordeiro R. Self-medication in children and adolescents. J Pediatr (Rio J) 2007;83:453–8. doi: 10.2223/JPED.1703. [DOI] [PubMed] [Google Scholar]
- 23.Buke C, Hosgor-Limoncu M, Ermertcan S, Ciceklioglu M, Tuncel M, Köse T, et al. Irrational use of antibiotics among university Students. J Infect. 2005;51:135–9. doi: 10.1016/j.jinf.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 24.Sarahroodi S, Arzi A, Sawalha AF, Ashtarinezhad A. Antibiotics self-medication among Shuthern Iranian university students. Int J Pharmacol. 2010;6:48–52. [Google Scholar]
- 25.Awad A, Eltayeb I, Motowe L, Thalib L. Self-medication with antibiotics and antimicrobials in the community of Khartum State, Sudan. J Pharm Sci. 2005;8:326–31. [PubMed] [Google Scholar]
- 26.Väänänen MH, Pietilä K, Airaksinen M. Self-medication with antibiotics-does it really happen in Europe? Health Policy. 2006;77:166–71. doi: 10.1016/j.healthpol.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Raz R, Edelstein H, Grigoryan L, Haaijer-Ruskamp FM. Self-Medication with Antibiotics by a Population in Northern Israel. Isr Med Assoc J. 2005;7:722–5. [PubMed] [Google Scholar]
- 28.Okumura J, Wakai S, Umenai T. Drug utilization and self-medication in rural communities in Vietnam. Soc Sci Med. 2002;54:1875–86. doi: 10.1016/s0277-9536(01)00155-1. [DOI] [PubMed] [Google Scholar]
- 29.Chan GC, Tang SF. Parental knowledge, attitudes and antibiotic use for acute upper respiratory tract infection in children attending a primary healthcare clinic in Malaysia. Singapore Med J. 2006;47:266–70. [PubMed] [Google Scholar]
- 30.Grigoryan L, Haaijer-Ruskamp FM, Burgerhof JG, Mechtler R, Deschepper R, Tambic-Andrasevic A, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12:452–9. doi: 10.3201/eid1203.050992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fischer T, Fischer S, Kochen MM, Hummers-Pradier E. Influence of patient symptoms and physical findings on general practitioners’ treatment of respiratory tract infections: A direct observation study. BMC Fam Pract. 2005;6:6. doi: 10.1186/1471-2296-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen C, Chen YM, Hwang KL, Lin SJ, Yang CC, Tsay RW, et al. Behavior, attitude and knowledge about antibiotic usage among residents of Changhua, Taiwan. J Microbiol Immunol Infect. 2005;38:53–9. [PubMed] [Google Scholar]
- 33.Parimi N, Pinto Pereira L, Prabhakar P. Caregivers’ practices, knowledge and beliefs of antibiotics in paediatric upper respiratory tract infections in Trinidad and Tobago: A cross-sectional study. BMC Fam Pract. 2004;5:28. doi: 10.1186/1471-2296-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]


