Abstract
Background:
This study was performed to examine quality of life's dimensions and its relationship with some clinical and demographic characteristics on women with breast cancer under chemotherapy referred to the oncology hospital, Isfahan University of medical sciences, Iran.
Methods:
This Cross sectional study was conducted among 330 breast cancer patients with simple sampling methodology. Data collection instrument included a questionnaire contains 2 parts (clinical and demographic characteristics information and version 2.0 of the SF-36 questionnaire (the international version). The data were analyzed with 99% confidence by carried out using SPSS18 with using descriptive and analytic statistics.
Results:
The majority of subjects’ quality of life was moderate (53.93%). there was a statistically significant relationship between quality of life among breast cancer patients with chemotherapy sessions (P < 0.05, df =4, χ2 = 16.37). One way Analysis Of Variance (ANOVA) suggested the absence of any significant relationship between quality of life with marital status (f = 0.21; P = 0.92) and employment status (f = 0.26; P = 0.77). Also, Spearman test showed the absence of any significant relationship between quality of life with age (P = 0.60), and the elapsed duration from diagnosis (P = 0.68), however Spearman test showed significant relationship between quality of life and education status (P = 0.002, r = -0.84).
Conclusion:
With regard to results of this study, there was a direct correlation between the number of chemotherapy sessions and patients quality of life. The attitude of the population toward chemotherapy is usually inhibiting and negative, so patients, students and nurses should be trained about chemotherapy efficacy to improve their attitude about chemotherapy, which in turn would lead to improvement of the patients’ quality of life.
Keywords: Breast neoplasms, demography, drug therapy, quality of life
INTRODUCTION
Breast cancer is the most common cancer in women worldwide and its incidence is increasing, especially in developing countries. While this disease is a very important challenge in health system,[1] it includes one-third of all the cancers in women. Its prevalence in various countries is different and is 8-23 in every 100 women.[2] Increasing trend of cancer in recent decades and its adverse effects on all physical, emotional, spiritual, social and economic aspects caused not only people, but also many experts pay attention to this disease more than ever and also caused they introduced breast cancer as the major health problem of the century.[3]
Annually, approximately one million women with breast cancer are identified in the world.[4] Latest reports from Iranian Cancer Society show that 25 percent of all the cancers in Iranian women is breast cancer,[5] whereas the prevalence rate of breast cancer in Europe and the U.S. has been estimated 8 to 10 percent.[1] Furthermore, compared with other developed countries, Iranian women suffer from breast cancer a decade earlier.[6,7] Breast cancer the most common and most deadly diseases[1] and emotionally and mentally is the most influencing disease among women. Most of these patients would experience more severe mental problems that can reduce their quality of life (QoL) and their daily activities.[8]
Obviously, cancer and its treatment have a considerable impact on mental and social health and finally on QoL of patients with cancer.[9] Since 1997 s, more attention has been given to the concept of quality of life. One of its reasons in the new era is more emphasis on QoL versus quantity of life, increased health care costs and identifying the differences in health care resultants.[10]
Diagnosis of breast cancer is a very stressful event with deep effect on different aspects of women's daily life.[11] Accordingly, suffering from breast cancer gets a special importance due to impacts it has on different dimensions of QoL. Reviewing QoL in health studies is important because it is as an auxiliary measure in assessment of improvement rate in patients and also an assisting method in assessing various treatment results.[12]
More appropriate therapeutic methods can be used with reviewing the QoL in patients and identifying the effects of disease on different aspects of their life; besides, the therapeutic results can be evaluated in a shorter duration and improve it.[13] Moreover, obtained results from measuring patients QoL can be used in reviewing the inabilities of various groups and population improved from cancer, reviewing the quality of provided cares and comparing the advantages and disadvantages of treatments. They also can be used in screening those at the risk of psychological and social problems and following up those who are improved and cancer survivals. Nurses not only are trying to modify these problems by identifying different aspects of patients’ life, but they also can attract necessary collaboration to improve their QoL by presenting the problems to the relate social organizations and patients’ families.[14]
In recent years, given to high prevalence of breast cancer and the importance of its impact on all the aspects of patients’ life and also considering that cancerous patients under treatment confront many problems, as well as in our society the concept of QoL and its related factors have been paid less attention, identifying these factors to health staff would help society to organize its activities in order to promote the health level and improve QoL of these patients; therefore, the present study aimed to review aspect of QoL and its association with certain clinical and demographic characteristics of women with breast cancer under chemotherapy in Oncology hospital affiliated to Isfahan University of medical sciences, Iran. It is hoped that the results can be a guide for interventional studies in this regard and also support the patients with cancer.
METHODS
This cross-sectional study was conducted among 330 patients with breast cancer were enrolled in the study during six months (since August 27, 2011 to February 20, 2012) in Sayyed-Al-Shohada hospital affiliated to Isfahan University of Medical Sciences through convenient sampling method. The inclusion criteria were age over 18, definitive confirmation of the breast cancer diagnosis by specialist, passing at least a year from disease, have no history of treatment for other types of cancer, no known mental problems or being treated with psychotropic drugs and be able to speak standard Persian. Moreover, any unwanted factor caused lack of ability to response the questions of the questionnaire physically or mentally, and also suffering from secondary breast cancer were the exclusion criteria. In order to collect data, a two-part questionnaire was used; the first part was related to clinical and demographic characteristics (age, time passed from diagnosis, marital status, educational level, employment status and the number of chemotherapy sessions) and the second part was the Short Form 36 Health Survey (SF-36) related to the Quality of Life.
The SF-36 Questionnaire version 2.0 was translated and used in this study that its reliability and validity have been approved in previous studies in more than 50 countries including Iran.[15]
The version 2.0 of the SF-36-the international version, a comprehensive short-form generic measure of health-related quality of life, consists of 36 items; 35 of which are aggregated into eight multi-item scales that measure physical functioning (PF), role-emotional (RE), role-physical (RP), bodily pain (BP), social functioning (SF), mental health (MH), vitality (VT) and understanding general health (GH).[16–19] Each scale is scored from 0 to 100, with 100 being the most favorable score.[18,20,21] This questionnaire consists of 6 questions concerning general health, 10 questions for physical functioning, 4 questions for vitality, 5 questions for mental health, 2 questions for social functioning, 4 questions for role-physical, 3 questions for role-emotional and 2 questions for bodily pain.[22] In this questionnaire, some of questions are scored according to the 1 to 5 Likert scale, some according to 1 to 3 and some other questions according to 1 to 2 Likert scale and the total score was analyzed based on score 100.[22] The scores of the questionnaire were analyzed in three low (0-33), moderate (34-66) and high levels (66-100).[23] The responding method for the QoL questionnaire varied from dual mode (Yes/No) to 6-degree Likert Scale. In this tool, increased score indicates higher level of QoL.[24]
The International Quality of Life Assessment (IQOLA) Project translate, validate, and standardize the SF-36 Health Survey for the use in multinational clinical trials and other international studies.[19]
The reliability of the eight scales and two summary measures has been estimated using both internal consistency and test–retest methods. With rare exceptions, published reliability statistics have exceeded the minimum standard of 0.70 recommended for measures used in group comparisons in more than 25 studies; most have exceeded 0.80. Reliability estimates for physical and mental summary scores usually exceed 0.90.[19]
Results from clinical studies, comparing scores for patients before and after treatment, have largely supported hypotheses about the validity of SF-36 scales based on results of the psychometric studies.[19] The reliability and validity of the SF-36 as a measure of health-related quality of life is well established.[17] Reliability coefficients have been reported as 0.81-0.88 (36 items). Discriminate validity was established, and the alpha coefficients ranged from 0.734-0.813.[18]
SF-36 questionnaire is a standard criteria used internationally in clinical research for assessing health policy and also evaluating the health status of public population, and in Iran also it has been used to evaluate QoL of diabetic and cardiovascular patients by professors and students of Tarbiat Modares University.[24] Despite the proved reliability of questionnaire, at the present study reliability of this questionnaire in patients with breast cancer has been done in a pilot study and its Pearson correlation coefficient obtained 75% through test re-test method with a two-week interval.
The SF-36 has been administered successfully in general population surveys in the United States and other countries, as well as to young and older adult patients with specific diseases. It can be administered in 5-10 min with a high degree of acceptability and data quality.[19]
Considering the ethical considerations and obtaining consent of the patients, the researchers began to complete the questionnaires. The data were analyzed after collection and coding through Software SPSS version 18 and descriptive (frequency distribution, mean, standard deviation) and analytical statistics (ANOVA test, Chi-square test, Pearson and Spearman correlation coefficient) with 99% confidence Interval.
RESULTS
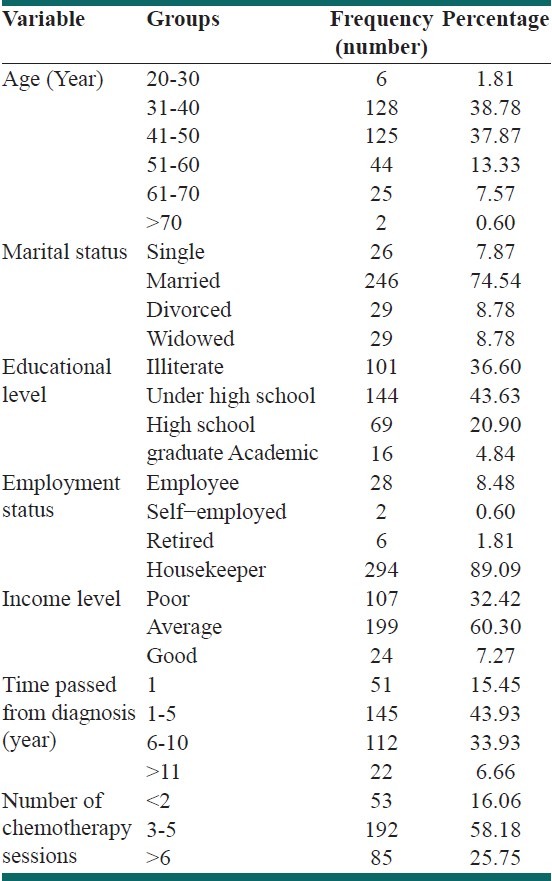
According to the results of the present study, mean age of the study subjects was 43.2±5.8 years. Most of the subjects (74.54%) were married and 43.63 percent were under high school graduates. While, only 4.84 percent had university academic degree. Moreover, in terms of employment, most of the subjects were housekeepers (89.09%). According to the obtained data, 30.68 percent of the patients had a family history of breast cancer. The duration of the disease for most of the patients (43.93%) was between 1-5 years. Other demographic information is illustrated in Table 1.
Table 1.
Demographic characteristics of the study subjects with breast cancer
According to the results of the present study, QoL of most of the study subjects (53.93%) was in a moderate level (34-66) and then 33.63 percent in a good level (>66) and finally 12.42 percent in a poor level (0-33).
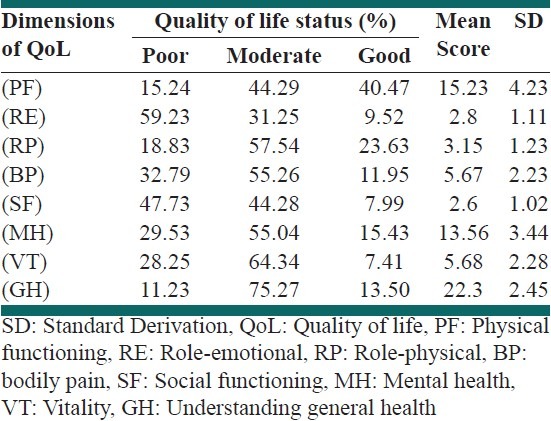
Table 2 shows mean and SD of the scores related to dimensions of QoL in patients with breast cancer. As also indicated in Table 2, the highest mean score is related to GH understanding (22.3) which indicates better situation of this aspect compared with other aspects of QoL. Moreover, SF and RE were the lowest with 2.6 and 2.8, respectively.
Table 2.
Frequency distribution, mean and SD of the 8 quality of life dimensions in study subjects with breast cancer
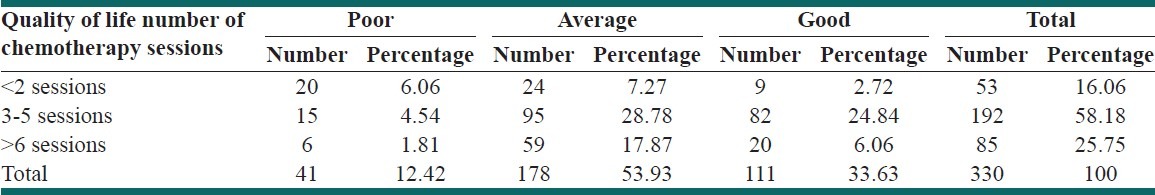
In terms of correlation of demographic variables with QoL of patients with breast cancer, the results showed that there was a significant correlation between QoL of patients with cancer with the number of chemotherapy sessions (df = 4; X2 = 16.37; P < 0.05). Table 3 shows the frequency distribution of the patients under chemotherapy in terms of QoL according to the number of chemotherapy sessions.
Table 3.
Frequency distribution of patients with breast cancer under chemotherapy in terms of quality of life according to the number of chemotherapy sessions
In addition, according to the findings of the present study, statistically there was no significant correlation between demographic variables such as age, time passed from diagnosis, marital status and employment status with QoL. In fact, One Way ANOVA showed there was no significant correlation between QoL with marital status (f = 0.21; P = 0.92) and employment status (f = 0.26; P = 0.77). Also, Spearman test showed there was no significant correlation between QoL with age (r = -0.23; P = 0.60) and elapsed duration of diagnosis (r = 0.12; P = 0.68). However, Spearman test showed that there was a significant correlation between QoL with educational level (r = -0.84; P = 0.002)
DISCUSSION
In the present study, QoL of most of the study subjects (53.93%) was moderate, then was good (33.63%) and finally was poor (12.42%). In supporting the findings of the present study, the study of Nematollahi titled as quality of life in breast cancer patients referred to selected clinics of Tehran University of Medical Sciences showed that QoL of most of them (66%) has been moderate.[25] Furthermore, our study results were also in accordance with other studies.[26,27] However, in the study of Mohan et al., the results indicated that QoL of most of the study subjects was lower than average.[28] The difference might be due to difference in the study population (in Mohan, there were patients with lung cancer and in the present study there were women with breast cancer) and also a large difference in the number of subjects.[28]
According to the findings of the present study, statistically there was no significant correlation between demographic variables such age, time passed from diagnosis, income level, marital status and employment status with QoL. This finding was in accordance with other studies.[25,29,30] Moreover, the results of another study showed that there was no significant correlation between the time passed from cancer diagnosis and QoL.[31]
However, the study results of Holzner et al., showed that duration of disease can reduce the QoL of cancerous patients.[32] Furthermore, the study results of Paskett et al., indicated that there was a significant correlation between patients’ age with QoL.[33] One of the probable reasons for these controversies is difference in the number of subjects; so that the number of subjects in the study of Paskett et al., was 245 and in Holzner was 87 people, and it was 330 in the present study. Besides, the other reasons of difference between the results of the above mentioned studies could be due to difference in type of questionnaire and sampling method.
One of the other findings of the present study was significant correlation between educational level and QoL of patients with breast cancer. Thus, increased rate of educational level in the study subjects also increased with mean score of QoL. In supporting the results of the present study, the study of Ozon et al., titled as quality of life in breast cancer patients in Turkey showed that statistically there was no significant correlation between age, marital status, monthly income level with QoL; however, there was a direct correlation between education and QoL. In a study by Shim et al., there was also a significant correlation between education and QoL; while there was no correlation between age and marital status with QoL.[34] The reasons of these differences can be due to probable differences in some inclusion criteria and/or other above mentioned causes.
On the other hand, it should be noted that a considerable number of patients in the present study were illiterate or low-educated; therefore, data collection in all the patients was done as the researcher loudly read the questions and completed the questionnaire. Therefore, it is likely that some questions are not precisely answered and it was one of the limitations of the study.
One of the other considerable findings was the presence of a significant correlation between QoL of patients with breast cancer with the number of chemotherapy sessions. Thus, increased number of chemotherapy sessions increased the mean score of QoL in patients and they had better quality of life. In confirmation of this finding, Shabanlooie in a study titled as reviewing the QoL of patients under chemotherapy referred to selected hospitals of Tabriz showed that there was a direct correlation between the QoL and number of chemotherapy sessions.[35] Moreover, the study results of Hurny et al., also were in accordance with the results of the present study.[36] While, Aghabarari et al., showed that there was an indirect (negative) correlation between QoL of patients and the number of chemotherapy sessions.[30] or the study of Kornblith that showed QoL of cancer patients had no significant difference before, during and after chemotherapy.[37]
One of the probable reasons in this conflict is difference in the assessment tool of QoL and a considerable difference in the sample size between the study of Aghabarari (n = 56) and in the present study (n = 330). In addition, a probable difference between the diet (type and amount of drug) and receiving new medications in each session of chemotherapy are the cases can influence on QoL and somehow justify these conflicts. However, given to the findings of the present study that there was a direct (positive) correlation between the chemotherapy sessions with QoL, it can be concluded that chemotherapy and increasing its sessions can promote quality of life of cancerous patients. Therefore, unlike the public belief, development of therapeutic plan and receiving further chemotherapy sessions can have the possibility of patient's adaptation with chemotherapy drugs and its side effects.
CONCLUSION
Given to the results of the present study that there was a direct correlation between the chemotherapy sessions with QoL and considering that negative and inhibiting attitude of the society toward chemotherapy, the effects of chemotherapy should be explained for students, nurses and patients through educational sessions and workshops in order to used these educations and modify their attitudes toward how properly deal with the issue of chemotherapy and finally promote and improve the quantitative and qualitative level of cancerous patients’ life.
Women are an important part of family and community; therefore, improving the QoL of women with cancer not only can improve their survival, but also can it increase the QoL and more cohesive family structure. Hence, it is necessary for the treatment team to assess and improve the QoL of patients meanwhile the role of nurses is highlighted.[38] Because nurses-as a member of medical team- have an important role in diagnosis, treatment and care from patients with cancer and since nurse spent more time with patients than other members of medical team, probably he/she is the first person can recognize the needs of patient and even his/her family and can be effective in improving their QoL.[39]
According to the findings of the present study, considering that there was a significant correlation between the number of chemotherapy sessions and QoL, it is recommended to conduct a study to compare the QoL of patients in chemotherapy sessions.
ACKNOWLEDGMENTS
Hereby, many appreciations go to all those who assisted us in conducting the present project and also other esteemed staff of Sayyed-Al-Shohada Hospital affiliated to Isfahan University of Medical Sciences, Isfahan, Iran.
Footnotes
Source of Support: NIL
Conflict of Interest: None to Declare
REFERENCES
- 1.Seedhom AE, Kamal NN. Factors Affecting Survival of Women Diagnosed with Breast Cancer in El-Minia Governorate, Egypt. Int J Prev Med. 2011;2:131–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Pollan M, Gustavsson P. High-risk occupations for breast cancer in the Swedish female working population. Am J Public Health. 1999;89:875–81. doi: 10.2105/ajph.89.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poorkiani M, Hazrati M, Abbaszadeh A, Jafari P, Sadeghi M, Dejbakhsh T, et al. Does a rehabilitation program improve quality of life in breast cancer patients? Payesh. 2010;9:61–8. [Google Scholar]
- 4.Guarneri V, Conte PF. The curability of breast cancer and the treatment of advanced disease. Eur J Nucl Med Mol Imaging. 2004;31:S149–61. doi: 10.1007/s00259-004-1538-5. [DOI] [PubMed] [Google Scholar]
- 5.Taleghani F, Yekta ZP, Nasrabadi AN. Coping with breast cancer in newly diagnosed Iranian women. J Adv Nurs. 2006;54:265–72. doi: 10.1111/j.1365-2648.2006.03808_1.x. [DOI] [PubMed] [Google Scholar]
- 6.Harirchi I, Karbakhsh M, Kashefi A, Momtahen AJ. Breast cancer in Iran: Results of a multi-center study. Asian Pac J Cancer Prev. 2004;5:24–7. [PubMed] [Google Scholar]
- 7.Sirous M, Ebrahimi A. The Epidemiology of Breast Masses among Women in Esfahan. J Surg. 2008;16:51–6. [Google Scholar]
- 8.Pedram M, Mohammadi M, Naziri GH, Aeinparast N. Effectiveness of cognitive-behavioral group therapy on the treatment of anxiety and depression disorders and on raising hope in women with breast cancer. J Woman Soc. 2011;1:61–75. [Google Scholar]
- 9.Kearney N, Richardson A. 1st ed. Philadelphia, PA: Churchill Livingstone; 2006. Nursing Patients with Cancer: Principles and Practice. [Google Scholar]
- 10.McNeil C. Oxford, UK: Oxford University Press; 2008. Quality of Life Researchers Have New Tool and New Focus on Measurement. [DOI] [PubMed] [Google Scholar]
- 11.Lu W, Cui Y, Zheng Y, Gu K, Cai H, Li Q, et al. Impact of newly diagnosed breast cancer on quality of life among Chinese women. Breast Cancer Res Treat. 2007;102:201–10. doi: 10.1007/s10549-006-9318-5. [DOI] [PubMed] [Google Scholar]
- 12.Kheil Tash A, Montazeri A, Nabaei B. Article Title: Factors predicting quality of life in patients with leukemia and lymphoma. Payesh. 2006;5:77–82. [Google Scholar]
- 13.Baghery H, Bakuei S. Survey of quality of life in patients with chronic obstructive pulmonary disease admitted to Imam Hussein hospital of Shahrood. J QOL. 2005;2:1–11. [Google Scholar]
- 14.Hassan Pour Dehkordi A, Shaban M. Relationship between cancer characteristics and quality of life in the cancer patients under chemotherapy referred to selected clinic of Tehran University of Medical Sciences. JSKUMS. 2005;6:63–70. [Google Scholar]
- 15.Montazeri A, Goshtasebi A, Vahdaian M, Gandek B. The Short-form Health Survey (SF-36): Translation and validation study of the Iranian version. Qual Life Res. 2005;14:875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 16.Hazavehei SM, Sabzmakan L, Hassanzadeh A, Rabiei K. The effect of precede Model-based educational program on depression level in patients with coronary artery bypass grafting. JQUMS. 2008;12:32–40. [Google Scholar]
- 17.Broeckel JA, Jacobsen PB, Balducci L, Horton J, Lyman GH. Quality of life after adjuvant chemotherapy for breast cancer. Breast Cancer Res Treat. 2000;62:141–50. doi: 10.1023/a:1006401914682. [DOI] [PubMed] [Google Scholar]
- 18.Byar KL, Berger AM, Bakken SL, Cetak MA. Impact of Adjuvant Breast Cancer Chemotherapy on Fatigue, Other Symptoms, and Quality of Life. Oncol Nurs Forum. 2006;33:E18–26. doi: 10.1188/06.ONF.E18-E26. [DOI] [PubMed] [Google Scholar]
- 19.Ware JE., Jr SF-36 Health Survey Update. Spine (Phila Pa 1976) 2000;25:3130–9. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 20.Ganz PA, Kwan L, Stanton AL, Krupnick JL, Rowland JH, Meyerowitz BE, et al. Quality of Life at the End of Primary Treatment of Breast Cancer: First results from the moving beyond Cancer randomized trial. J Natl Cancer Inst. 2004;96:376–87. doi: 10.1093/jnci/djh060. [DOI] [PubMed] [Google Scholar]
- 21.Behrouzifar S, Zenouzi Sh, Nezafati M, Esmaili H. Factors Affecting the Patients’ Quality of Life after Coronary Artery Bypass Graft. IJN. 2009;22:31–41. [Google Scholar]
- 22.Taraghi Z, Ilali E, Abedini M, Zarvani A, Khoshnama I, Mohammadpour R, et al. Quality of Life among Multiple Sclerosis Patients. IJN. 2007;20:51–9. [Google Scholar]
- 23.Sadeghiye Ahri S, Arshi S, Iranparvar M, Emami F, Siahpoosh H. The Effect of Complications of Type II Diabetes on Patients’ Quality of Life. J Ardabil Univ Med Sci. 2009;8:394–402. [Google Scholar]
- 24.Baraz-Pardenjani SH, Mohammadi E, Boroumand B. The Effect of Self – Care Teaching by Video Tape on Physical Problems and Quality of Life in Dialysis Patients. IJN. 2008;21:121–32. [Google Scholar]
- 25.Nematollahi A. Tehran: Tehran University of Medical Sciences; 2004. Quality of life in the breast cancer patients referred to selected clinic of Tehran University of Medical Sciences. [MS Thesis] [Google Scholar]
- 26.Sammarco A. Perceived social support, uncertainty, and quality of life of younger breast cancer survivors. Cancer Nurs. 2001;24:212–9. [PubMed] [Google Scholar]
- 27.Bakhshi R, Davachi A, Kamali P. Tehran: Iran University of Medical Sciences; 2000. Effect of nurse counseling on quality of life among women with breast cancer treated with radiotherapy at the Cancer Institute of Tehran in 2000. [MS Thesis] [Google Scholar]
- 28.Mohan A, Mohan C, Bhutani M, Pathak AK, Pal H, Das C, et al. Quality of life in newly diagnosed patients with lung cancer in a developing country: Is it important? Eur J Cancer Care (Engl) 2006;15:293–8. doi: 10.1111/j.1365-2354.2006.00654.x. [DOI] [PubMed] [Google Scholar]
- 29.Rustoen T. Hope and quality of life, two central issues for cancer patients: A theoretical analysis. Cancer Nurs. 1995;18:355–61. [PubMed] [Google Scholar]
- 30.Agha Barari M, Ahmadi F, Mohammadi E, Hagizadeh E, Varvarani A. Physical, emotional and social dimension of quality of life among breast cancer women under chemotherapy. IJNR. 2007;1:55–65. [Google Scholar]
- 31.Thatcher N, Hopwood P, Anderson H. Improving quality of life in patients with non-small cell lung cancer: Research experience with gemcitabine. Eur J Cancer. 1997;33:S8–13. doi: 10.1016/s0959-8049(96)00336-x. [DOI] [PubMed] [Google Scholar]
- 32.Holzner B, Kemmler G, Kopp M, Moschen R, Schweigkofler H, Dunser M, et al. Quality of life in breast cancer patients-not enough attention for long-term survivors? Psychosomatics. 2001;42:117–23. doi: 10.1176/appi.psy.42.2.117. [DOI] [PubMed] [Google Scholar]
- 33.Paskett E, Herndon J, Donohue K, Naughton M, Grubbs S, Pavy M, et al. Health Related Quality of Life in Long Term Breast Cancer Survivors. Cancer. 2009:1109–20. doi: 10.1002/cncr.24140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shim EJ, Mehnert A, Koyama A, Cho SJ, Inui H, Paik NS, et al. Health-related quality of life in breast cancer: A cross-cultural survey of German, Japanese, and South Korean patients. Breast Cancer Res Treat. 2006;99:341–50. doi: 10.1007/s10549-006-9216-x. [DOI] [PubMed] [Google Scholar]
- 35.Shabanlooie R, Motaarefi H. Proceedings of the 1st Congress of Quality of life in Tarbiat Modares University. Tehran, Iran: Tarbiat Modares University Publication; 2005. Quality of life among chemotherapy patients admitted to selected hospitals in Tabriz. [Google Scholar]
- 36.Hurny C, Bernhard J, Coates AS, Castiglione-Gertsch M, Peterson HF, Gelber RD, et al. Impact of adjuvant therapy on quality of life in women with node-positive operable breast cancer.International Breast Cancer Study Group. Lancet. 1996;347:1279–84. doi: 10.1016/s0140-6736(96)90936-8. [DOI] [PubMed] [Google Scholar]
- 37.Kornblith AB, Lan L, Archer L, Partridge A, Kimmick G, Hudis C, et al. Quality of Life of Older Patients with Early Stage Breast Cancer Receiving Adjuvant Chemotherapy: A Companion Study to Cancer and Leukemia, Group B49907. J Clin Oncol. 2011;29:1022–8. doi: 10.1200/JCO.2010.29.9859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watson T, Mock V. Exercise as an Intervention for Cancer-Related Fatigue. Phys Ther. 2004;84:736–43. [PubMed] [Google Scholar]
- 39.Phipps WJ, Monahan FD, Sands JK, Marek JF, Neighbors M. Louis, Missouri: Mosby; 2003. Medical-Surgical Nursing: Health and Illness Perspectives. [Google Scholar]


