Abstract
The authors examined the association between life events and antihypertensive medication adherence in older adults and the moderating role of coping. A cross-sectional analysis was conducted by using data (n = 1,817) from the Cohort Study of Medication Adherence among Older Adults (recruitment conducted from August 2006 through September 2007). Life events occurring in the 12 months preceding the study interview were assessed via the Holmes Rahe Social Readjustment Rating Scale (SRRS), and coping levels were assessed via an adapted version of the John Henry Active Coping Scale. Low adherence to antihypertensive medication was defined as scores less than 6 on the 8-item Morisky Medication Adherence Scale (known as “MMAS-8”). Of study participants, 13.2% had low adherence, and 27.2% and 5.0% had medium (150–299) and high (≥300) SRRS scores, respectively. After multivariable adjustment, the odds ratios for low adherence associated with medium and high, versus low, SRRS were 1.50 (95% confidence interval: 1.11, 2.02) and 2.11 (95% confidence interval: 1.24, 3.58), respectively. When multivariable models were stratified by coping level, the association between life events and adherence was evident only among participants with low coping levels.
Keywords: coping, hypertension, medication adherence, older adults, stress
Persistent adherence to prescribed medications is essential to reducing the risk of cardiovascular disease and stroke among patients with hypertension (1). Although effective medical therapy and evidence-based treatment guidelines for hypertension are readily available, low adherence to antihypertensive medications is prevalent, and blood pressure control is still not optimal, particularly among older populations (2–4).
Numerous barriers to antihypertensive medication adherence have been identified (5, 6). Of these, psychosocial factors including depression (7–10), low social support (11), and poor quality of life (12, 13) have been shown to maintain a strong association with medication adherence among older adults. Stress arising from recent life events may also negatively impact adherence behavior, yet few data are available assessing the relation between life events and adherence to antihypertensive medications. Further, because an individual's coping approach can impact how he or she cognitively appraises a situation or event and ultimately derives stress from it (14), coping skills could play an integral role in buffering the impact of life events on adherence behavior. Therefore, we examined the association between life events and antihypertensive medication adherence and assessed the moderating role of active coping skills by using data from a large cohort of older adults.
MATERIALS AND METHODS
Study population and timeline
Data for the current analysis come from the Cohort Study of Medication Adherence among Older Adults (CoSMO). The primary goal of CoSMO is to investigate factors that influence adherence to antihypertensive medication in older adults; the study design, response rates, and baseline characteristics have been published previously (15). In brief, adults aged 65 years or older with essential hypertension were randomly selected from the roster of a large managed care organization in southeastern Louisiana. Recruitment was conducted from August 21, 2006, to September 30, 2007, and 2,194 participants completed the baseline survey (15). The 1,817 CoSMO participants included in this analysis were eligible if they 1) completed the 1-year follow-up survey conducted between 2007 and 2008 including the life events questionnaire (7.4% of participants did not complete the life events portion of the survey) and 2) answered at least 75% of the questions on the 8-item Morisky Medication Adherence Scale (MMAS-8) (1.9% of participants were excluded for answering fewer than 75% of MMAS-8 questions). Compared with participants who were included in this analysis, participants who were excluded were more likely to be African American and to not have completed high school (P < 0.05 for both comparisons). CoSMO was approved by the Ochsner Clinic Foundation's Institutional Review Board and the privacy board of the managed care organization (15).
Study measures
Study measures were drawn from participant surveys and from the databases of the managed care organization. Surveys were administered via telephone by trained interviewers. Specific to this analysis, the survey included assessment of sociodemographic and clinical factors in addition to medication adherence, life events, and coping level. Information regarding comorbid conditions was obtained from the administrative databases of the managed care organization.
Sociodemographic and clinical characteristics obtained by participant self-report included marital status, age, gender, race, educational attainment, height and weight, depressive symptoms, and duration of hypertension. Body mass index was calculated as weight (kg)/height (m)2, and age was dichotomized into 2 groups (65–74 vs. 75 years of age or older) with approximately half of the study population in each group. Marital status was collapsed into 2 categories: married (currently married or cohabitating) and not married (currently divorced, separated, widowed, or never married). Depressive symptoms were assessed by using the 20-item Center for Epidemiologic Studies Depression Scale (16, 17). The Charlson comorbidity index score was constructed by using comorbid conditions identified via International Classification of Diseases, Ninth Revision, codes (18, 19).
Self-reported antihypertensive medication adherence was ascertained by using MMAS-8. Self-report tools such as the MMAS-8 are simple to administer, feasible, and economical for use in clinical practice (20, 21). Further, the MMAS-8 was designed to facilitate the identification of barriers to and behaviors associated with adherence to chronic medications. The tool has been determined to be reliable and significantly associated with blood pressure control (P < 0.05) in individuals with hypertension (22) as well as with antihypertensive medication pharmacy fill rates (22, 23). Scores on the MMAS-8 range from 0 to 8, with scores of less than 6 reflecting low adherence (22).
Life events that occurred over the 12 months prior to the survey were assessed by using the Holmes Rahe Social Readjustment Rating Scale (SRRS) (24, 25). As part of the SRRS, participants were asked about 41 life events that are thought to evoke change in an individual's life. Life event data were then summarized in 2 ways. First, the total number of life events that each participant had experienced was calculated. Then, in accordance with SRRS scoring rules, each life event was assigned a predetermined life change units value ranging from 11 to 100, thought to correspond to “the amount and duration of change in one's accustomed pattern of life” (25, p. 123). Life change unit values were then summed for each participant to calculate a total SRRS score, with higher SRRS scores indicating greater stress. SRRS scores were categorized as low (<150), medium (150–299), or high (≥300) (24–26).
Problem-focused or active coping was assessed at the baseline CoSMO survey by using a 7-item coping scale (alpha reliability = 0.84) that has previously been shown to be associated with medication adherence in patients with hypertension (22). Items for the scale are drawn from the John Henry Active Coping Scale, a tool which assesses the concept that one can meet the demands of his/her environment through hard work and determination (27, 28). As part of the coping scale, participants were asked to rate 7 questions using a 4-point Likert scale (e.g., “I've always felt that I could make of my life pretty much what I wanted to make of it” with response options: strongly agree, agree, disagree, or strongly disagree), and scores for each item were summed for a total coping score that could range from 7 to 28. Higher scores connote psychological responses such as mental and physical vigor, tenacity, and personal efficacy when confronting psychosocial stressors, and lower coping levels connote lower levels of these traits. In accordance with previously used categorization schemes, low and high coping scores were classified as below and above the median value (median = 22), respectively, for CoSMO study participants (29–31).
Statistical analysis
Characteristics of CoSMO participants were calculated by category of SRRS score. Then, in order to better understand the impact of coping level on the association between life events and medication adherence, we stratified all analyses by coping level. The prevalence of low medication adherence was calculated for those who had and had not experienced each life event, with the statistical significance of the association between each life event and low adherence assessed with chi-square tests. Multivariable logistic regression models were used to assess cross-sectional relations between categories of SRRS scores and low medication adherence. Models were adjusted for age, race, education, gender, marital status, depressive symptoms, and the Charlson comorbidity index. Differences in the association between SRRS scores and medication adherence by level of coping were assessed in a multivariable adjusted model with all participants and interaction terms for coping by SRRS level.
RESULTS
The mean age of the 1,817 participants included in this analysis was 76.1 (standard deviation, 5.6) years, 28.4% were black, 59.6% were women, and 54.9% were married. Also, 62.9% had been diagnosed with hypertension for 10 or more years, and 56.4% had 2 or more comorbid conditions. Overall, 13.2% of participants had low antihypertensive medication adherence. The median number of life events reported was 4 (range, 0–22), and 27.2% and 5.0% had medium and high stressful life event scores, respectively.
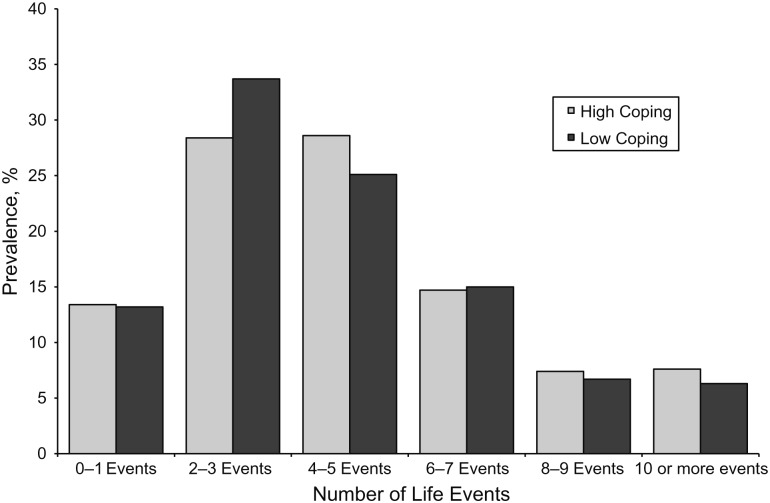
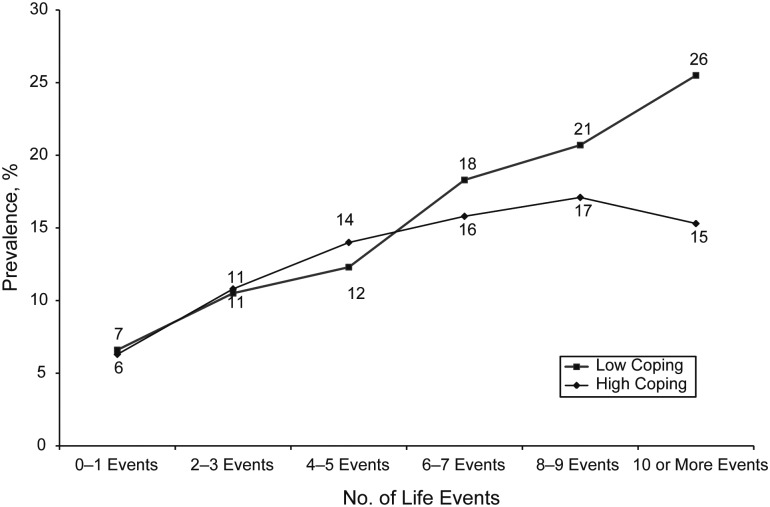
Characteristics of CoSMO participants by SRRS scores are shown in Table 1. Participants with higher SRRS scores were less likely to be older (≥75 years of age) and more likely to be black and to have depressive symptoms. The prevalence of low adherence, by coping level, among the participants who experienced each life event in the SRRS is shown in Table 2. Among participants with lower coping levels, those who reported a change in financial state, a change in the health or behavior of a family member, and changes in recreational activities, church activities, social activities, sleeping activities, or eating habits had significantly lower adherence than those who had not experienced each of these events. Among participants with higher coping levels, those who had experienced a change in financial state or the death of a close friend had significantly lower adherence, and those who had taken a vacation had significantly higher adherence than their counterparts who had not experienced these events. The frequency distribution of the total number of life events experienced is shown in Figure 1, and the prevalence of low antihypertensive medication adherence corresponding to the number of life events experienced is shown in Figure 2. Regardless of coping level, the prevalence of low adherence increased with a higher number of life events experienced (Ptrend < 0.01 and < 0.001 for those with high and low coping, respectively). The association between more life events experienced and low adherence was similar for those with low and high coping for those experiencing fewer than 6 life events. For those experiencing 6 or more life events, more life events were associated with a higher prevalence of low adherence among individuals with low coping but not for their counterparts with high coping.
Table 1.
Characteristics of CoSMO Participants by the SRRS Score, 2007–2008a
| SRRS Scores |
||||||
|---|---|---|---|---|---|---|
| Low (n = 1,232) |
Medium (n = 495) |
High (n = 90) |
||||
| Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Life events, no.b | 2.9 (1.5) | 6.9 (1.8) | 12.1 (2.6) | |||
| Age ≥75 years | 56.7 | 51.9 | 41.1* | |||
| Women | 58.7 | 61.8 | 60.0 | |||
| Married | 56.4 | 51.5 | 53.3 | |||
| High school graduate | 80.4 | 80.8 | 77.8 | |||
| Black race | 25.2 | 33.3 | 45.6* | |||
| Hypertension duration ≥10 years | 61.8 | 65.5 | 64.4 | |||
| Comorbid index score ≥2 | 55.5 | 57.4 | 63.3 | |||
| Body mass index ≥25 kg/m2 c | 74.9 | 76.8 | 83.2 | |||
| Uncontrolled blood pressured | 29.8 | 30.3 | 39.8 | |||
| Depressive symptoms | 9.6 | 18.4 | 34.4* | |||
Abbreviations: CoSMO, Cohort Study of Medication Adherence among Older Adults; SD, standard deviation; SRRS, Holmes Rahe Social Readjustment Rating Scale.
* P < 0.001.
a All measures were collected at the time corresponding to the 1-year follow-up survey.
b Life events over the last year were measured by using the Holmes Rahe Social Readjustment Rating Scale, and scores are categorized as low (<150), medium (150–299), or high (≥300).
c Body mass index: weight (kg)/height (m)2.
d Uncontrolled blood pressure was defined as systolic/diastolic blood pressure ≥140/90 mm Hg.
Table 2.
Prevalence of Low Antihypertensive Medication Adherencea Associated With Life Events,b Stratified by Coping Level,c Among CoSMO Participants, 2007–2008
| Total Sample | No. With Life Event (n = 1,817) | Low Medication Adherence, % |
|
|---|---|---|---|
| High Coping (n = 947; 13.4%) | Low Coping (n = 869; 13.6%) | ||
| Vacation | 748 | 10.2* | 10.5 |
| Death of a close friend | 567 | 16.5* | 16.3 |
| Death in the family | 467 | 12.8 | 15.9 |
| Change in health/behavior of family member | 413 | 18.1 | 20.3*** |
| Gained a new family member | 362 | 12.4 | 17.3 |
| Change in amount/type of recreation | 320 | 17.2 | 19.9** |
| Change in the number of get-togethers | 315 | 16.3 | 15.5 |
| Change in financial state | 298 | 20.1* | 20.1*** |
| Large purchase | 291 | 12.4 | 14.9 |
| Change in eating habits | 280 | 13.4 | 26.7*** |
| Sexual difficulties | 266 | 15.8 | 17.5 |
| Change in sleeping habits | 252 | 13.1 | 20.0* |
| Change in living conditions | 226 | 17.2 | 15.5 |
| Outstanding personal achievement | 214 | 13.2 | 14.1 |
| Personal injury or illness | 214 | 15.0 | 15.0 |
| Change in church activities | 213 | 17.5 | 19.8* |
| Change in social activities | 195 | 14.7 | 22.6* |
| Change in residence | 132 | 15.5 | 11.5 |
| Retirement | 112 | 19.7 | 22.2 |
| Change in number of arguments with spouse | 105 | 12.5 | 14.3 |
Abbreviation: CoSMO, Cohort Study of Medication Adherence among Older Adults.
* P < 0.05, **P < 0.01, ***P < 0.001 for comparison of low adherence in those participants experiencing each life event versus those who did not.
a Antihypertensive medication adherence was measured at the 1-year CoSMO follow-up survey by using the Morisky Medication Adherence Scale (MMAS-8): Low medication adherence was defined as an MMAS-8 score of <8.
b Life events reported by <5% of the sample are not listed. Life events over the last year were measured at the 1-year CoSMO follow-up survey by using the Holmes Rahe Social Readjustment Rating Scale (SRRS).
c Coping was measured at the baseline CoSMO survey by using a 7-item coping scale: Low and high coping are defined as scores above and below the median for the sample, respectively. Coping data were not available for 1 participant in the sample.
Figure 1.
Prevalence of total number of life events, stratified by coping level, among CoSMO participants, 2007–2008. Life events over the last year were measured at the 1-year CoSMO follow-up survey by using the Holmes Rahe Social Readjustment Rating Scale (SRRS). Coping was measured at the baseline Cohort Study of Medication Adherence among Older Adults (CoSMO) survey by using a 7-item coping scale: Low and high coping scores are defined as scores above and below the median for the sample, respectively.
Figure 2.
Prevalence of low medication adherence by number of life events, stratified by coping level, among CoSMO participants, 2007–2008. Antihypertensive medication adherence was measured at the 1-year CoSMO follow-up survey by using the 8-item Morisky Medication Adherence Scale (MMAS-8): Low medication adherence was defined as an MMAS-8 score of less than 8. Life events over the last year were measured at the 1-year CoSMO follow-up survey by using the Holmes Rahe Social Readjustment Rating Scale (SRRS). Coping was measured at the baseline Cohort Study of Medication Adherence among Older Adults (CoSMO) survey by using a 7-item coping scale: Low and high coping scores are defined as scores above and below the median for the sample, respectively.
The relation between SRRS scores and low adherence, overall and by level of coping, is shown in Table 3. The prevalence of low adherence was 11.0%, 16.6%, and 24.4% among participants with low, medium, and high SRRS scores, respectively (Ptrend < 0.001). After multivariable adjustment, participants with medium and high stressful life event scores had a higher odds of low medication adherence, compared with those with low stressful life event scores (odds ratio = 1.50, 95% confidence interval: 1.11, 2.02 and odds ratio = 2.11, 95% confidence interval: 1.24, 3.58, respectively). The interaction between coping and SRRS level did not reach statistical significance (P > 0.10); however, when multivariable models were stratified by coping level, the association between life events and adherence was statistically significant only among participants with low coping levels.
Table 3.
Adjusted Odds Ratios for Low Medication Adherencea Associated With SRRS,b Overall and Stratified by Coping Level,c Among CoSMO Participants, 2007–2008
| Low Medication Adherence, % | Odds Ratiod | 95% CI | |
|---|---|---|---|
| All participants (n = 1,817) | |||
| Low SRRS score | 11.0 | 1.00 | Referent |
| Medium SRRS score | 16.6 | 1.50* | 1.11, 2.02 |
| High SRRS score | 24.4 | 2.94* | 1.24, 3.58 |
| Low coping (n = 869) | |||
| Low SRRS score | 10.5 | 1.00 | Referent |
| Medium SRRS score | 18.2 | 1.50* | 1.15, 2.72 |
| High SRRS score | 30.0 | 2.11* | 1.39, 6.22 |
| High coping (n = 947) | |||
| Low SRRS score | 11.4 | 1.00 | Referent |
| Medium SRRS score | 15.2 | 1.25 | 0.81, 1.91 |
| High SRRS score | 20.0 | 1.48 | 0.69, 3.17 |
Abbreviations: CI, confidence interval; CoSMO, Cohort Study of Medication Adherence among Older Adults; SRRS, Holmes Rahe Social Readjustment Rating Scale.
* P < 0.01.
a Antihypertensive medication adherence was measured at the 1-year CoSMO follow-up survey by using the Morisky Medication Adherence Scale (MMAS-8): Low medication adherence was defined as an MMAS-8 score of <8.
bLife events over the last year were measured at the 1-year CoSMO follow-up survey by using the SRRS, and SRRS scores are categorized as low (<150), medium (150–299), or high (≥300). Higher scores represent greater stress.
cCoping was measured at the baseline Cohort Study of Medication Adherence among Older Adults (CoSMO) survey by using a 7-item coping scale: Low and high coping scores are defined as scores above and below the median for the sample, respectively. Coping data were not available for 1 participant in the sample.
d Odds ratios were adjusted for age, race, education, gender, marital status, depressive symptoms, and comorbid conditions.
DISCUSSION
Previous research has shown that psychosocial factors play an important role in patients' medication-taking behavior (7, 9–12, 32, 33). The current study expands upon this body of literature, adding evidence that the occurrence of life events may impact medication adherence in older patients with hypertension. Older adults with higher SRRS scores had increased odds of low adherence to antihypertensive medications. This association was present only among those who had coping scores in the lower half of the sample. There are few prior studies assessing the impact of life events on adherence to medication regimens. Our findings are similar to results from a population with human immunodeficiency virus (HIV), where both stressful life events and patient-reported perceived stress were identified as barriers to sustained adherence to antiretroviral therapies (34). Previous research from the mental health literature also suggests that patients who experience stressful life events may have reduced motivation or ability to consistently adhere to psychiatric medications as prescribed (35).
Results from our study add evidence that life events can negatively impact adherence to medication regimens—particularly if a patient has lower coping skills and the total number of life events that he or she experiences is high. These results build upon our prior work that showed that lower scores on a hurricane-coping self-efficacy scale (indicating worse coping abilities) were associated with lower adherence to antihypertensive medications (36). The current study is one of very few to examine the moderating role of coping in the relation between life events and medication adherence (37). Despite the lack of previously published data, the concept that inherent personality factors or personal resources play an important role in how stress impacts health or health behaviors is not new (14, 38, 39). For example, in a study published in 1979, Kobasa (40) showed that differences in illness seen among executives experiencing the same levels of stress could be attributed to degree of “hardiness” (i.e., a strong commitment to self, attitude of vigor, sense of meaningfulness, and internal locus of control). More recent results in the HIV literature have shown that “distress tolerance” significantly moderates the association between life events and the number of reasons reported for medication nonadherence (37). In another study, life events had a stronger effect among HIV patients who are psychologically vulnerable (i.e., those experiencing depression) compared with those who are psychologically well (41). Our findings from patients with cardiovascular disease are in accordance with those from the HIV literature and highlight the importance of considering recent life events, coping ability, and/or emotional or psychological vulnerability in identifying patients who may be at risk for low adherence.
Life stress has been identified as a potent risk factor for the onset of a depressive episode (42, 43), particularly when it occurs later in life. In our study, participants who had higher SRRS scores had a significantly higher prevalence of depressive symptoms. Our analysis also shows that, among patients with lower coping skills, medication adherence was significantly lower for participants who reported those life events that are also consistent with depressive symptoms (i.e., changes in eating, sleeping, recreational, or social activities). However, results of multivariate models showed that the SRRS scores remain independently associated with medication adherence, even after adjusting for the presence of depressive symptoms. Although stress from the occurrence of life events, coping ability, and depression are likely closely intertwined, there may be only partial overlap in the mechanism through which they impact adherence. For example, the overwhelming sadness stemming from some types of life events (i.e., the death of a close friend or spouse) could affect adherence by triggering an episode of depression. However, other types of life events (i.e., recent retirement or a change in financial state) could impact adherence differently, by creating disruptions in previously established routines. Interventions focused on addressing psychosocial barriers to adherence should consider not only strategies focused on treatment of depressive symptoms but also behavioral strategies aimed to address stress and improve the coping skills needed for handling the disruptions caused by life events.
The occurrence of stressful life events has been associated with the onset or exacerbation of numerous types of chronic disease (44–50). Of relevance to this analysis, data from previous research have shown that stress from life events may contribute to the pathogenesis of coronary heart disease (48) and acute myocardial infarction (49, 50). Results from the current study support the concept that increased stress from life events may increase cardiovascular disease risk vis à vis disruptions in adherence to antihypertensive medications. Additional studies designed to elucidate the prospective relation among life stressors, health maintenance behaviors (i.e., adherence), blood pressure control, and cardiovascular outcomes would contribute important data to the literature.
Strengths and limitations
The results of the study should be interpreted in light of some limitations. The medication adherence measure used in the current study relied on self-report, which could have led to the overestimation of adherence due to social desirability and recall biases. However, our prior work has revealed an association between the MMAS-8 and antihypertensive pharmacy fill data (23). While widely used life stress checklists such as the SRRS can be an efficient way to measure recent stressors, there are also some weaknesses inherent to use of such tools. Specifically, a number of studies have pointed out that life measure checklists contain inherent measurement error (51–53). However, we believe that such error was minimized in our study because questions regarding stress were embedded within a larger survey about hypertension, reducing the potential for participants to overreport stressors to satisfy the perceived needs of the research. In addition, because our results showed that life stress remained independently associated with low adherence after adjustment for depression, we do not believe study results can be explained by differential reporting of life stress among depressed and nondepressed individuals. Although the use of life change unit values to weigh life events in the SRRS recognizes that some life events can act as greater stressors than others, the process is limited by the assumption that an event will evoke the same amount of stress for each participant. For this reason, we have presented data as both the total number of events and as the overall SRRS score. Importantly, our results indicate that both scoring methods are consistently associated with antihypertensive medication adherence. Results from sensitivity analyses showed that the adjusted association with low medication adherence was comparable when the unweighted total number of events was used in place of the SRRS score. Another limitation inherent to the SRRS is its failure to discriminate between positive and negative life events. The assumption is made that change affects adherence vis à vis increased stress, which could occur regardless of whether the change was positive or negative. Additionally, the few life events that could be answered or perceived positively by patients (e.g., retirement) could impact adherence through disruption of previously established medication-taking routines. Finally, although the cross-sectional nature of the analysis does not allow us to empirically confirm the direction of the association, we hypothesize that such highly prevalent life events, such as death or change in the health/behavior of a family member, may lead to low adherence, rather than low adherence leading to these events.
This study has many strengths, including its large sample size, broad range of data collected (survey, administrative, and clinical data), and diversity of the sample with respect to sociodemographics and the presence of risk factors. Because CoSMO is limited to community-dwelling older adults in a managed care organization, confounding by access to care and health insurance is reduced. We believe that the study results are still highly generalizable: Over 80% of US adults with hypertension have health insurance, including almost all US citizens aged 65 years or older with health insurance and pharmacy benefits through Medicare (54, 55).
Conclusion
In the current analysis, older adults with low coping skills and more life events had lower adherence to prescribed antihypertensive medications. This study adds important data to the body of literature describing psychosocial factors associated with medication adherence among older adults, and it provides evidence that life events may be an important factor in adherence to prescribed medications. Health-care providers should consider assessment of recent life events and coping skills in identifying hypertension patients at risk for low adherence to prescribed medications.
ACKNOWLEDGMENTS
Author affiliations: Center for Health Research, Ochsner Clinic Foundation, New Orleans, Louisiana (Elizabeth W. Holt, Marie Krousel-Wood); Department of Epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana (Elizabeth W. Holt, Marie Krousel-Wood); Department of Epidemiology, University of Alabama at Birmingham, Birmingham, Alabama (Paul Muntner); Department of Biostatistics, Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana (Larry S. Webber, C. Joyce); and Department of Community Health Sciences, UCLA Fielding School of Public Health, Los Angeles, California (Donald E. Morisky).
This work was supported by the National Institute on Aging (grant R01 AG022536, M. Krousel-Wood, Principal Investigator).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Donald E. Morisky is the developer/owner of the copyrighted MMAS-8 that is available free through a license agreement for publicly funded researchers and students. Permission for use of MMAS-8 is required. Licensure agreement is available from Dr. Morisky at the UCLA Fielding School of Public Health.
Paul Muntner is a consultant for Amgen, Inc., and also receives research grant funding from Amgen, Inc.
REFERENCES
- 1.Hamilton GA. Measuring adherence in a hypertension clinical trial. Eur J Cardiovasc Nurs. 2003;2(3):219–228. doi: 10.1016/S1474-5151(03)00058-6. [DOI] [PubMed] [Google Scholar]
- 2.Kravitz RL, Hays RD, Sherbourne CD, et al. Recall of recommendations and adherence to advice among patients with chronic medical conditions. Arch Intern Med. 1993;153(16):1869–1878. [PubMed] [Google Scholar]
- 3.Dusing R. Overcoming barriers to effective blood pressure control in patients with hypertension. Curr Med Res Opin. 2006;22(8):1545–1553. doi: 10.1185/030079906X120995. [DOI] [PubMed] [Google Scholar]
- 4.Fields LE, Burt VL, Cutler JA, et al. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44(4):398–404. doi: 10.1161/01.HYP.0000142248.54761.56. [DOI] [PubMed] [Google Scholar]
- 5.Krousel-Wood M, Thomas S, Muntner P, et al. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 6.Hyre AD, Krousel-Wood MA, Muntner P, et al. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich) 2007;9(3):179–186. doi: 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krousel-Wood M, Islam T, Muntner P, et al. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010;40(3):248–257. doi: 10.1007/s12160-010-9217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krousel-Wood MA, Frohlich ED. Hypertension and depression: coexisting barriers to medication adherence. J Clin Hypertens (Greenwich) 2010;12(7):481–486. doi: 10.1111/j.1751-7176.2010.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang PS, Bohn RL, Knight E, et al. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17(7):504–511. doi: 10.1046/j.1525-1497.2002.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 11.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 12.Holt EW, Muntner P, Joyce CJ, et al. Health-related quality of life and antihypertensive medication adherence among older adults. Age Ageing. 2010;39(4):481–487. doi: 10.1093/ageing/afq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martinez YV, Prado-Aguilar CA, Rascon-Pacheco RA, et al. Quality of life associated with treatment adherence in patients with type 2 diabetes: a cross-sectional study. BMC Health Serv Res. 2008;8:164. doi: 10.1186/1472-6963-8-164. doi:10.1186/1472-6963-8-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Folkman S, Lazarus RS, Gruen RJ, et al. Appraisal, coping, health status, and psychological symptoms. J Pers Soc Psychol. 1986;50(3):571–579. doi: 10.1037//0022-3514.50.3.571. [DOI] [PubMed] [Google Scholar]
- 15.Krousel-Wood MA, Muntner P, Islam T, et al. Barriers to and determinants of medication adherence in hypertension management: perspective of the Cohort Study of Medication Adherence among Older Adults. Med Clin North Am. 2009;93(3):753–769. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knight RG, Williams S, McGee R, et al. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behav Res Ther. 1997;35(4):373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- 17.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1(3):385–401. [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.Hawkshead J, Krousel-Wood M. Techniques of measuring medication adherence in hypertensive patients in outpatient settings: advantages and limitations. Dis Manag Health Outcomes. 2007;15(2):109–118. [Google Scholar]
- 21.Grymonpre RE, Didur CD, Montgomery PR, et al. Pill count, self-report, and pharmacy claims data to measure medication adherence in the elderly. Ann Pharmacother. 1998;32(7/8):749–754. doi: 10.1345/aph.17423. [DOI] [PubMed] [Google Scholar]
- 22.Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Krousel-Wood M, Islam T, Webber LS, et al. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15(1):59–66. [PMC free article] [PubMed] [Google Scholar]
- 24.Masuda M, Holmes TH. Magnitude estimations of social readjustments. J Psychosom Res. 1967;11(2):219–225. doi: 10.1016/0022-3999(67)90011-6. [DOI] [PubMed] [Google Scholar]
- 25.Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 26.De-la-Revilla-Ahumada L, De-los-Rios-Alvarez AM, Luna-del-Castillo JD. Use of the Goldberg General Health Questionnaire (GHQ-28) to detect psychosocial problems in the family physician's office. Aten Primaria. 2004;33(8):417–422. doi: 10.1016/S0212-6567(04)79426-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernander AF, Duran RE, Saab PG, et al. Assessing the reliability and validity of the John Henry Active Coping Scale in an urban sample of African Americans and white Americans. Ethn Health. 2003;8(2):147–161. doi: 10.1080/13557850303563. [DOI] [PubMed] [Google Scholar]
- 28.James SA, Hartnett SA, Kalsbeek WD. John Henryism and blood pressure differences among black men. J Behav Med. 1983;6(3):259–278. doi: 10.1007/BF01315113. [DOI] [PubMed] [Google Scholar]
- 29.James SA. John Henryism and the health of African-Americans. In: LaVeist TA, editor. Race, Ethnicity, and Health: A Public Health Reader. San Francisco, CA: Jossey-Bass; 2002. pp. 350–368. [Google Scholar]
- 30.Merritt MM, Bennett GG, Jr, Williams RB, et al. Low educational attainment, John Henryism, and cardiovascular reactivity to and recovery from personally relevant stress. Psychosom Med. 2004;66(1):49–55. doi: 10.1097/01.psy.0000107909.74904.3d. [DOI] [PubMed] [Google Scholar]
- 31.Merritt MM, McCallum TJ, Fritsch T. How much striving is too much? John Henryism active coping predicts worse daily cortisol responses for African American but not white female dementia family caregivers. Am J Geriatr Psychiatry. 2011;19(5):451–460. doi: 10.1097/JGP.0b013e3181eaffa4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams GC, Patrick H, Niemiec CP, et al. Reducing the health risks of diabetes: how self-determination theory may help improve medication adherence and quality of life. Diabetes Educ. 2009;35(3):484–492. doi: 10.1177/0145721709333856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rose M, Fliege H, Hildebrandt M, et al. The network of psychological variables in patients with diabetes and their importance for quality of life and metabolic control. Diabetes Care. 2002;25(1):35–42. doi: 10.2337/diacare.25.1.35. [DOI] [PubMed] [Google Scholar]
- 34.Leserman J, Ironson G, O'Cleirigh C, et al. Life events and adherence in HIV. AIDS Patient Care STDS. 2008;22(5):403–411. doi: 10.1089/apc.2007.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magura S, Laudet AB, Mahmood D, et al. Adherence to medication regimens and participation in dual-focus self-help groups. Psychiatr Serv. 2002;53(3):310–316. doi: 10.1176/appi.ps.53.3.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Islam T, Muntner P, Webber LS, et al. Cohort Study of Medication Adherence in Older Adults (CoSMO): extended effects of Hurricane Katrina on medication adherence among older adults. Am J Med Sci. 2008;336(2):105–110. doi: 10.1097/MAJ.0b013e318180f175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O'Cleirigh C, Ironson G, Smits JA. Does distress tolerance moderate the impact of life events on psychosocial variables and behaviors important in the management of HIV? Behav Ther. 2007;38(3):314–323. doi: 10.1016/j.beth.2006.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hinkle LE, Jr, Christenson WN, Kane FD, et al. An investigation of the relation between life experience, personality characteristics, and general susceptibility to illness. Psychosom Med. 1958;20(4):278–295. doi: 10.1097/00006842-195807000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Cohen F. Stress and bodily illness. Psychiatr Clin North Am. 1981;4(2):269–286. [PubMed] [Google Scholar]
- 40.Kobasa SC. Stressful life events, personality, and health: an inquiry into hardiness. J Pers Soc Psychol. 1979;37(1):1–11. doi: 10.1037//0022-3514.37.1.1. [DOI] [PubMed] [Google Scholar]
- 41.Bottonari KA, Safren SA, McQuaid JR, et al. A longitudinal investigation of the impact of life stress on HIV treatment adherence. J Behav Med. 2010;33(6):486–495. doi: 10.1007/s10865-010-9273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brilman EI, Ormel J. Life events, difficulties and onset of depressive episodes in later life. Psychol Med. 2001;31(5):859–869. doi: 10.1017/s0033291701004019. [DOI] [PubMed] [Google Scholar]
- 43.Lueboonthavatchai P. Role of stress areas, stress severity, and life events on the onset of depressive disorder: a case-control study. J Med Assoc Thai. 2009;92(9):1240–1249. [PubMed] [Google Scholar]
- 44.Naldi L, Peli L, Parazzini F, et al. Family history of psoriasis, stressful life events, and recent infectious disease are risk factors for a first episode of acute guttate psoriasis: results of a case-control study. J Am Acad Dermatol. 2001;44(3):433–438. doi: 10.1067/mjd.2001.110876. [DOI] [PubMed] [Google Scholar]
- 45.Gupta MA, Gupta AK. Stressful life events are associated with a higher frequency of cutaneous sensory symptoms: an empirical study of non-clinical subjects. J Eur Acad Dermatol Venereol. 2004;18(5):560–565. doi: 10.1111/j.1468-3083.2004.00931.x. [DOI] [PubMed] [Google Scholar]
- 46.Tosevski DL, Milovancevic MP. Life events and physical health. Curr Opin Psychiatry. 2006;19(2):184–189. doi: 10.1097/01.yco.0000214346.44625.57. [DOI] [PubMed] [Google Scholar]
- 47.Potagas C, Mitsonis C, Watier L, et al. Influence of anxiety and reported life events on relapses in multiple sclerosis: a prospective study. Mult Scler. 2008;14(9):1262–1268. doi: 10.1177/1352458508095331. [DOI] [PubMed] [Google Scholar]
- 48.Rafanelli C, Roncuzzi R, Milaneschi Y, et al. Stressful life events, depression and demoralization as risk factors for acute coronary heart disease. Psychother Psychosom. 2005;74(3):179–184. doi: 10.1159/000084003. [DOI] [PubMed] [Google Scholar]
- 49.Magni G, Corfini A, Berto F, et al. Life events and myocardial infarction. Aust N Z J Med. 1983;13(3):257–260. doi: 10.1111/j.1445-5994.1983.tb04653.x. [DOI] [PubMed] [Google Scholar]
- 50.Lundberg U, Theorell T, Lind E. Life changes and myocardial infarction: individual differences in SRRS scaling. J Psychosom Res. 1975;19(1):27–32. doi: 10.1016/0022-3999(75)90047-1. [DOI] [PubMed] [Google Scholar]
- 51.Monroe SM, Roberts JE. Conceptualizing and measuring life stress: problems, principles, procedures, progress. Stress Med. 1990;6(3):209–216. [Google Scholar]
- 52.Raphael KG, Cloitre M, Dohrenwend BP. Problems of recall and misclassification with checklist methods of measuring stressful life events. Health Psychol. 1991;10(1):62–74. doi: 10.1037//0278-6133.10.1.62. [DOI] [PubMed] [Google Scholar]
- 53.Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Annu Rev Clin Psychol. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. doi:10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- 54.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 55.Schober SE, Makuc DM, Zhang C, et al. Health insurance affects diagnosis and control of hypercholesterolemia and hypertension among adults aged 20-64: United States, 2005–2008. NCHS Data Brief. 2011;(57):1–8. [PubMed] [Google Scholar]