Abstract
Salt sensitivity of blood pressure (BP) is influenced by genetic and environmental factors. A dietary feeding study was conducted from October 2003 to July 2005 that included a 7-day low-sodium intervention (51.3 mmol sodium/day) followed by a 7-day high-sodium intervention (307.8 mmol sodium/day) among 1,906 individuals who were 16 years of age or older and living in rural northern China. Salt sensitivity of BP was defined as mean BP change from the low-sodium intervention to the high-sodium intervention. Usual physical activity during the past 12 months was assessed at baseline using a standard questionnaire. The multivariable-adjusted means of systolic BP responses to high-sodium intervention were 5.21 mm Hg (95% confidence interval (CI): 4.55, 5.88), 4.97 mm Hg (95% CI: 4.35, 5.59), 5.02 mm Hg (95% CI: 4.38, 5.67), and 3.96 mm Hg (95% CI: 3.29, 4.63) among participants from the lowest to the highest quartiles of physical activity, respectively (P = 0.003 for linear trend). The multivariable-adjusted odds ratio of high salt sensitivity of systolic BP was 0.66 (95% CI: 0.49, 0.88) for persons in the highest quartile of physical activity compared with those in the lowest quartile. Physical activity is significantly, independently, and inversely related to salt sensitivity of BP and may be particularly effective in lowering BP among salt-sensitive individuals.
Keywords: blood pressure, dietary sodium, physical activity, salt sensitivity
An increase in physical activity and a reduction in dietary sodium have been recommended as important lifestyle modifications for the prevention and treatment of hypertension (1, 2). Observational epidemiologic studies have reported an independent and inverse association between physical activity and the risk of hypertension (3). Randomized controlled trials have documented that physical activity lowers blood pressure (BP) in normotensive and hypertensive individuals (4). Observational epidemiologic studies and clinical trials also documented an independent and positive association between dietary sodium intake and BP (5–9). For example, the International Study of Salt and Blood Pressure (INTERSALT), a large cross-sectional study in 10,074 adults from 32 countries, reported that a 100-mmol higher level of urinary sodium excretion was associated with 6-mm Hg increase in systolic BP and a 3-mm Hg increase in diastolic BP (7). In a meta-analysis of clinical trials, Cutler and colleagues estimated that an average reduction in dietary sodium intake of 100 mmol/day resulted in 5.8-mm Hg and 2.5-mm Hg decrements in systolic and diastolic BP, respectively, in hypertensive individuals and 2.3-mm Hg and 1.4-mm Hg decrements in normotensive individuals (9).
Clinical trials have also documented that BP responses to dietary sodium intake vary among individuals, a phenomenon called “salt sensitivity” (10). Heterogeneity in salt sensitivity is influenced by age, race, sex, hypertension status, body weight, alcohol intake, and genetic factors (10–13). To our knowledge, the relation between physical activity level and salt sensitivity of BP has not been reported in the previous literature. Elucidating the interrelation between physical activity and BP responses to dietary sodium intervention could improve our knowledge of hypertension etiology and inform clinical guidelines and public health policy by identifying high-risk groups of people who will benefit most from intervention. We undertook a large dietary feeding study to examine the association of genetic and other risk factors with salt sensitivity of BP among a rural population residing in northern China. In the present article, we report the relation between physical activity and salt sensitivity of BP.
MATERIALS AND METHODS
Study participants
Details of the study population and methods for the Genetic Epidemiology Network of Salt Sensitivity (GenSalt) Study have been published elsewhere (14). In brief, the study was conducted in rural areas of northern China from October 2003 to July 2005. A community-based BP screening was conducted among people 18–60 years of age who resided in the study villages to identify potential probands and their families. Probands with a mean systolic BP of 130–160 mm Hg and/or a mean diastolic BP of 85–100 mm Hg and no use of antihypertensive medications were recruited for the dietary feeding study, along with their siblings, spouses, and offspring who were 16 years of age or older. Exclusion criteria included stage 2 hypertension (BP ≥160/100 mm Hg), secondary hypertension, clinical cardiovascular disease, diabetes mellitus (fasting plasma glucose ≥7.0 mmol/L), chronic kidney disease (positive urine albumin test by dipstick measurement), pregnancy, heavy alcohol consumption, a low-sodium diet, or use of antihypertensive or antidiabetic medications or insulin.
Institutional review boards or ethics committees at all participating institutions approved the study protocol. Written informed consent was obtained from each participant before baseline data collection and intervention.
Data collection
A standardized questionnaire was administered to participants by trained staff at the baseline examination to obtain information about demographic characteristics, personal and family medical history, and lifestyle risk factors (including cigarette smoking, alcohol consumption, and physical activity level). For the measurement of physical activity level, we adapted the Paffenbarger Physical Activity Questionnaire (15). Data were collected on the number of hours spent in vigorous and moderate activity on a usual day during the previous 12 months for weekdays and weekends separately to account for anticipated daily variability in energy expenditure. Examples provided for vigorous activity included shoveling, digging, heavy farming, jogging, brisk walking, heavy carpentry, and bicycling on hills, and examples of moderate activity included housework, regular walking, yard work, light carpentry, and bicycling on level ground.
Three BP measurements were obtained every morning during the 3-day baseline observation period and on days 5, 6, and 7 of each intervention period by trained and certified individuals using a random-zero sphygmomanometer according to a standard protocol adapted from procedures recommended by the American Heart Association (16). BP was measured with the participant in the sitting position after they had rested for 5 minutes. Participants were advised to avoid consumption of alcohol, coffee, or tea, cigarette smoking, and exercise for at least 30 minutes before their BP measurements. BP observers were blinded to the participants' dietary interventions. Body weight, height, and waist circumference were measured twice with the participants in light indoor clothing without shoes during their baseline examination. Waist circumference was measured 1 cm above the participants' navel during light breathing.
Intervention
Study participants received a low-sodium diet (3 g sodium chloride or 51.3 mmol sodium per day) for 7 days followed by a high-sodium diet (18 g sodium chloride or 307.8 mmol sodium per day) for an additional 7 days. In previous studies in which salt sensitivity was assessed, 10–70 mmol sodium/day was used for low-sodium interventions and 180–345 mmol sodium/day was used for high-sodium interventions (17). Dietary total energy intake varied according to the baseline energy intake of each participant. All foods were cooked without salt, and prepackaged salt was added to the individual study participant's meal when it was served by the study staff. Study participants were not blinded to their dietary sodium intake because it was not possible to blind the taste. To ensure compliance with the intervention program, participants were required to eat breakfast, lunch, and dinner at the study kitchen under the supervision of study staff during the entire study. Study participants were instructed to avoid consumption of any foods or beverages that were not provided by the study. Three timed urinary specimens (one 24-hour specimen and two 8-hour overnight specimens) were obtained during the 3 days of baseline examination and the last 3 days of each intervention period to monitor compliance with the dietary sodium intervention. Overnight urinary sodium excretion was converted to 24-hour values based on formulas developed from data obtained in a subgroup of study participants. Three separate formulas were developed for baseline, low-sodium intervention, and high-sodium intervention using a simple linear regression of 24-hour values on 8-hour overnight values.
The results from the 24-hour urinary excretions of sodium and potassium showed excellent compliance with the study diet. The mean of 24-hour urinary excretions of sodium and potassium were 242.4 mmol and 36.9 mmol at baseline, 47.5 mmol and 31.4 mmol during the low-sodium intervention, and 244.3 mmol and 35.7 mmol during the high-sodium intervention, respectively.
Statistical analysis
BP levels at baseline and during the dietary sodium intervention were calculated as the mean of 9 measurements from 3 clinical visits during the 3-day baseline observation or on days 5, 6, and 7 of each intervention phase. Salt sensitivity of BP was defined as the mean BP during the high-sodium intervention minus the mean BP during the low-sodium intervention. High salt sensitivity was defined as an increase in BP of 5% or more during the high-sodium intervention relative to the BP level during the low-sodium intervention ((BP on high-sodium diet − BP on low-sodium diet)/BP on low-sodium diet). In this study population, a 5% change corresponded to a mean absolute change of 5.57 mm Hg in systolic BP and 3.55 mm Hg in diastolic BP.
The physical activity information obtained from the questionnaire was converted to metabolic equivalent (MET) hours per day. The MET is a ratio of the metabolic rate while performing a given task to the metabolic rate while seated and resting. One MET represents an expenditure of 1 kilocalorie per kilogram of body weight per hour and is equivalent to sitting quietly. MET-hours per day were calculated by weighting the number of hours spent in each activity intensity category by a MET value that corresponded to the occupation group represented in that activity intensity category. The MET weight for vigorous activity was 3.67 for farming and the MET weight for moderate activity was 2.56 for working within the household (18). The average MET-hours per day were calculated by weighting MET-hours for weekdays and weekends and were then divided into quartiles for analysis.
The associations between physical activity and salt sensitivity of BP were assessed using linear and logistic regression models. Generalized estimation equations were used to fit linear and logistic models with empirical estimates of standard errors. All analyses included a term for family cluster and accounted for nonindependence of family members with an exchangeable correlation structure. Age- and sex-adjusted mean BP responses to the high-sodium intervention and percentages of high salt sensitivity of BP were calculated by quartiles of MET-hours per day, and the statistical significance of differences in these characteristics across quartiles was tested using linear or logistic regression analyses. In addition, age, sex, educational level, cigarette smoking, alcohol consumption, body mass index (weight (kg)/height (m)2), baseline BP, and 24-hour urinary excretion of sodium and potassium were further adjusted in the multivariable linear and logistic regression analyses. The quartile with the lowest physical activity level was used as the reference group. To test for linear trend, the median MET-hours per day in each physical activity quartile were treated as a continuous variable in regression models. Unless otherwise stated, P < 0.05 was considered statistically significant and all tests were 2-sided. Statistical analyses were performed using SAS, version 9.2 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
A total of 1,906 study participants met all eligibility criteria and took part in the dietary sodium intervention. Of these, 1,860 (97.6%) subjects completed the low-sodium and high-sodium interventions. Participants who did not complete the study did not differ in terms of baseline characteristics from those who did complete the study. The majority of subjects engaged in work activity of moderate intensity (50.3%) or vigorous intensity (37.9%). During leisure time, most subjects engaged in activities of light intensity (51.1%) or were sedentary (28.7%). On a usual day, participants spent an average of 3.3 hours in vigorous activity and 4.6 hours in moderate activity.
Table 1 presents the age- and sex-adjusted baseline characteristics of study participants by physical activity quartile. Participants who were more physically active were older, were more likely to be male, attained a lower level of education, had lower baseline BP levels, and were less likely to have hypertension. There was not a statistically significant difference in sodium and potassium excretion by physical activity quartile.
Table 1.
Age- and Sex-Adjusteda Baseline Characteristics by Physical Activity Quartile for Entire Study Population, Genetic Epidemiology Network of Salt Sensitivity Study, China, 2003–2005
| Characteristic | Physical Activity Level, MET-hours per day |
P for Trend | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <15.1 (n = 440) |
15.1–22.9 (n = 506) |
23.0–34.4 (n = 471) |
>34.4 (n = 489) |
||||||
| Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | ||
| Age, years | 35.2 (0.66) | 38.6 (0.43) | 39.9 (0.43) | 40.5 (0.42) | <0.0001 | ||||
| Male sex | 40.4 | 48.4 | 52.4 | 71.0 | <0.0001 | ||||
| High school education or higher | 20.6 | 12.9 | 14.5 | 11.8 | <0.0001 | ||||
| Current smoker | 4.1 | 6.0 | 6.5 | 5.4 | 0.18 | ||||
| Current drinker | 15.9 | 15.8 | 18.2 | 16.9 | 0.54 | ||||
| Body mass indexb | 23.3 (0.16) | 23.6 (0.15) | 23.4 (0.15) | 23.1 (0.15) | 0.20 | ||||
| Waist circumference, cm | 80.6 (0.50) | 80.5 (0.42) | 80.8 (0.46) | 79.1 (0.48) | 0.04 | ||||
| 24-hour urinary sodium, mmol | 238.2 (3.21) | 244.6 (2.92) | 241.5 (2.99) | 243.1 (3.06) | 0.39 | ||||
| 24-hour urinary potassium, mmol | 36.8 (0.47) | 36.6 (0.40) | 36.5 (0.39) | 37.0 (0.40) | 0.87 | ||||
| Baseline systolic BP, mm Hg | 117.1 (0.67) | 118.6 (0.61) | 117.3 (0.71) | 115.9 (0.63) | 0.09 | ||||
| Baseline diastolic BP, mm Hg | 73.9 (0.49) | 74.8 (0.47) | 74.0 (0.48) | 72.5 (0.45) | 0.01 | ||||
| BP ≥140/90 mm Hg | 9.9 | 10.6 | 7.5 | 5.5 | 0.002 | ||||
Abbreviations: BP, blood pressure; MET, metabolic equivalent; SE, standard error.
a Age was adjusted for sex and sex was adjusted for age. All other variables were adjusted for age and sex.
b Weight (kg)/height (m)2.
Table 2 shows an inverse association between the adjusted mean absolute and percent change in BP from the low-sodium intervention to the high-sodium intervention and quartile of physical activity. The multivariable-adjusted average increase in systolic BP was 5.26 mm Hg among persons in the lowest quartile of physical activity compared with 3.92 mm Hg in persons in the highest quartile of physical activity. There was an average increase of 2.20 mm Hg in diastolic BP among those in the lowest physical activity level quartile compared with a 1.19-mm Hg increase in the highly physically active group. This statistically significant linear trend was preserved after additional adjustment for baseline BP (all P values for trend ≤0.01). The same inverse association was observed for the mean percent change in BP from the low-sodium intervention to the high-sodium intervention and the level of physical activity (all P values for trend ≤0.03).
Table 2.
Mean Absolute and Percentage Blood Pressure Responses to the High-Sodium Intervention by Physical Activity Levels, Genetic Epidemiology Network of Salt Sensitivity Study, China, 2003–2005
| Physical Activity Level, MET-hours per day | Age- and Sex-Adjusted |
Multivariable-Adjusteda |
Multivariable-Adjustedb |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Systolic |
Diastolic |
Systolic |
Diastolic |
Systolic |
Diastolic |
|||||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Absolute Blood Pressure Responses, mm Hg | ||||||||||||
| <15.1 | 5.30 | 4.73, 5.87 | 2.34 | 1.85, 2.82 | 5.26 | 4.60, 5.93 | 2.20 | 1.63, 2.76 | 5.21 | 4.55, 5.88 | 2.15 | 1.59, 2.71 |
| 15.1–22.9 | 5.21 | 4.71, 5.70 | 2.23 | 1.74, 2.72 | 5.13 | 4.50, 5.77 | 2.07 | 1.49, 2.66 | 4.97 | 4.35, 5.59 | 2.00 | 1.41, 2.58 |
| 23.0–34.4 | 5.12 | 4.56, 5.67 | 2.11 | 1.63, 2.58 | 5.09 | 4.43, 5.74 | 1.97 | 1.38, 2.57 | 5.02 | 4.38, 5.67 | 1.92 | 1.33, 2.51 |
| >34.4 | 3.94 | 3.40, 4.48 | 1.35 | 0.81, 1.88 | 3.92 | 3.24, 4.61 | 1.19 | 0.56, 1.82 | 3.96 | 3.29, 4.63 | 1.21 | 0.59, 1.84 |
| P for trend | 0.0009 | 0.006 | 0.001 | 0.007 | 0.003 | 0.01 | ||||||
| Percentage Blood Pressure Responses | ||||||||||||
| <15.1 | 4.81 | 4.28, 5.34 | 3.48 | 2.76, 4.20 | 4.79 | 4.17, 5.41 | 3.28 | 2.47, 4.09 | 4.76 | 4.14, 5.39 | 3.24 | 2.43, 4.05 |
| 15.1–22.9 | 4.67 | 4.22, 5.11 | 3.37 | 2.65, 4.10 | 4.62 | 4.05, 5.19 | 3.16 | 2.31, 4.01 | 4.53 | 3.97, 5.10 | 3.10 | 2.25, 3.96 |
| 23.0–34.4 | 4.65 | 4.14, 5.15 | 3.19 | 2.49, 3.89 | 4.62 | 4.03, 5.22 | 2.98 | 2.09, 3.86 | 4.59 | 4.00, 5.18 | 2.94 | 2.06, 3.83 |
| >34.4 | 3.65 | 3.15, 4.13 | 2.27 | 1.48, 3.07 | 3.61 | 2.99, 4.23 | 2.01 | 1.08, 2.94 | 3.63 | 3.02, 4.25 | 2.02 | 1.09, 2.95 |
| P for trend | 0.002 | 0.02 | 0.002 | 0.02 | 0.004 | 0.03 | ||||||
Abbreviations: CI, confidence interval; MET, metabolic equivalent.
a Multivariable model A included age, sex, body mass index, educational level, cigarette smoking, alcohol consumption, and baseline urinary excretion of sodium and potassium.
b Multivariable model A plus baseline systolic or diastolic blood pressure.
Table 3 shows an inverse association between physical activity level as a continuous variable and the adjusted absolute and percentage changes in systolic and diastolic BP from the low-sodium intervention to the high-sodium intervention. For example, in the multivariable-adjusted model including baseline BP, a 1-standard deviation increase in physical activity level (11.5 MET-hours) was associated with a 0.46-mm Hg (95% confidence interval: −0.74, −0.19; P = 0.001) lower increase in systolic BP. The inverse relation was consistent for all models, systolic and diastolic BP, and absolute and percentage change in BP (all P values ≤0.006).
Table 3.
Association Between a 1-Standard-Deviation Increase in Physical Activity Level (11.5 Metabolic Equivalent-Hours) and Blood Pressure Responses, Genetic Epidemiology Network of Salt Sensitivity Study, China, 2003–2005
| Model | Systolic Blood Pressure |
Diastolic Blood Pressure |
||||
|---|---|---|---|---|---|---|
| Regression Coefficient | 95% CI | P Value | Regression Coefficient | 95% CI | P Value | |
| Absolute Blood Pressure Responses, mm Hg | ||||||
| Age- and sex-adjusted | −0.53 | −0.81, −0.26 | 0.0001 | −0.41 | −0.65, −0.16 | 0.001 |
| Multivariable-adjusteda | −0.52 | −0.80, −0.24 | 0.0003 | −0.41 | −0.66, −0.16 | 0.001 |
| Multivariable-adjustedb | −0.46 | −0.74, −0.19 | 0.001 | −0.38 | −0.63, −0.13 | 0.003 |
| Percentage Blood Pressure Responses | ||||||
| Age- and sex-adjusted | −0.46 | −0.71, −0.21 | 0.0003 | −0.52 | −0.88, −0.16 | 0.005 |
| Multivariable-adjusteda | −0.45 | −0.70, −0.20 | 0.0005 | −0.54 | −0.91, −0.17 | 0.004 |
| Multivariable-adjustedb | −0.42 | −0.67, −0.17 | 0.001 | −0.52 | −0.89, −0.15 | 0.006 |
Abbreviation: CI, confidence interval.
a Multivariable model A included age, sex, body mass index, educational level, cigarette smoking, alcohol consumption, and baseline urinary excretion of sodium and potassium.
b Multivariable model A plus baseline systolic or diastolic blood pressure.
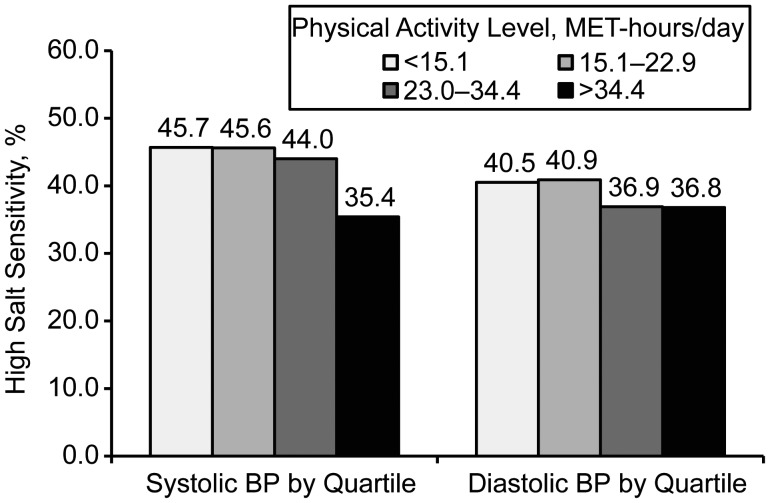
Age- and sex-adjusted proportions of high salt sensitivity of systolic and diastolic BP by physical activity quartile are presented in Figure 1. The proportion of subjects with high salt sensitivity decreased with increasing physical activity levels. For systolic BP, 45.7% of the least physically active participants were highly salt sensitive, whereas 35.4% of the most active were highly salt sensitive (P value for trend = 0.003). For diastolic BP, 40.5% of the least active participants were highly salt sensitive compared with 36.8% of the most active (P value for trend = 0.15).
Figure 1.
Age- and sex-adjusted proportions of high salt sensitivity (≥5% blood pressure (BP) increase from low-sodium to high-sodium intervention) by quartile of physical activity levels, Genetic Epidemiology Network of Salt Sensitivity Study, China, 2003–2005. P for systolic blood pressure trend = 0.003; P for diastolic blood pressure trend = 0.15. MET, metabolic equivalent.
There was a statistically significant and independent dose-response association between physical activity and high salt sensitivity (Table 4). The odds ratio of high salt sensitivity of systolic BP decreased significantly with higher physical activity levels as compared with the lowest physical activity level. The relation was consistent for all 3 models predicting high sensitivity of systolic BP (all P values for trend ≤0.005). For example, in the multivariable-adjusted model, the odds ratio for high salt sensitivity was 0.65 (95% confidence interval: 0.49, 0.86) for systolic BP when comparing subjects in the highest activity level with those in the lowest activity level. In contrast, the mean percent change in diastolic BP across physical activity quartiles was only marginally statistically significant (P values for trend = 0.09) in the multivariable-adjusted models.
Table 4.
Odds Ratios for the Association Between High Salt Sensitivity and Physical Activity Levels, Genetic Epidemiology Network of Salt Sensitivity Study, China, 2003–2005
| Physical Activity, MET-hours per day | Model |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age- and Sex-Adjusted |
Multivariable-Adjusteda |
Multivariable-Adjustedb |
|||||||
| OR | 95% CI | P Value | OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Systolic Blood Pressure Increase ≥5% | |||||||||
| <15.1 | 1 | Referent | 1 | Referent | 1 | Referent | |||
| 15.1–22.9 | 0.99 | 0.77, 1.29 | 0.99 | 0.98 | 0.75, 1.27 | 0.85 | 0.96 | 0.73, 1.25 | 0.74 |
| 23.0–34.4 | 0.93 | 0.70, 1.25 | 0.64 | 0.93 | 0.70, 1.24 | 0.63 | 0.93 | 0.69, 1.25 | 0.62 |
| >34.4 | 0.65 | 0.49, 0.86 | 0.003 | 0.65 | 0.49, 0.86 | 0.003 | 0.66 | 0.49, 0.88 | 0.004 |
| P value for trend | 0.003 | 0.003 | 0.005 | ||||||
| Diastolic Blood Pressure Increase ≥5% | |||||||||
| <15.1 | 1 | Referent | 1 | Referent | 1 | Referent | |||
| 15.1–22.9 | 1.02 | 0.79, 1.31 | 0.88 | 0.99 | 0.77, 1.28 | 0.95 | 0.99 | 0.77, 1.28 | 0.95 |
| 23.0–34.4 | 0.86 | 0.67, 1.12 | 0.26 | 0.84 | 0.65, 1.09 | 0.19 | 0.84 | 0.65, 1.09 | 0.19 |
| >34.4 | 0.86 | 0.66, 1.12 | 0.26 | 0.82 | 0.62, 1.08 | 0.15 | 0.82 | 0.63, 1.08 | 0.15 |
| P value for trend | 0.15 | 0.09 | 0.09 | ||||||
Abbreviations: CI, confidence interval; MET, metabolic equivalent; OR, odds ratio.
a Multivariable model A included age, sex, body mass index, educational level, cigarette smoking, alcohol consumption, and baseline urinary excretion of sodium and potassium.
b Multivariable model A plus baseline systolic or diastolic blood pressure.
DISCUSSION
The present large population-based dietary feeding study identified a strong, consistent dose-response relation between level of physical activity and salt sensitivity of BP. Salt sensitivity of BP decreased progressively with higher levels of physical activity. This association was statistically significant and independent of important covariables.
These findings have important clinical and public health implications. Hypertension is a prevalent disorder and leading cause of premature deaths in the United States and worldwide (19, 20). In addition, high salt sensitivity of BP has been shown to increase the risk of cardiovascular disease and premature mortality (21, 22). An increase in physical activity level and a reduction in dietary sodium have been identified as 2 major approaches for the prevention and treatment of hypertension (1, 2). Our findings suggest that high levels of physical activity protect against salt sensitivity of BP, as evidenced by participants in the highest quartile of physical activity having much lower BP responses than the participants in the lower 3 quartiles of physical activity. However, sodium consumption impacts BP across all levels of physical activity. Because of this, a low-dietary-sodium intervention could be beneficial to all people. Moreover, these findings also provide further support for the recommendations to increase physical activity for the prevention and treatment of hypertension, especially among those with a high dietary sodium intake. Because dietary sodium intake in the US population is well above recommended levels (23), increased physical activity should play an important role in programs aimed at BP reduction in the US general population.
The protective effect of increased levels of physical activity on BP responses to high sodium intake might occur through several potential mechanisms, such as reduction of insulin resistance, improvement of endothelial function, and inhibition of sympathetic nervous system activity. Physical activity has been shown to be associated with reduced insulin resistance (24), and insulin resistance decreases renal sodium excretion, leading to extracellular fluid volume expansion and salt-sensitive hypertension (25, 26). The shear stress associated with physical activity has been shown to improve vascular endothelial function through increased nitric oxide production, reduce pathologic constriction, and improve blood flow (27, 28). The association between inhibition of nitric oxide synthesis and salt sensitivity of BP was shown in an animal study (29). The physiologic response to exercise is a reduction of sympathetic nervous system activity potentially through altered gene expression in the brain (30). Excessive salt consumption can lead to impaired central sympathetic system inhibition, followed by increased peripheral sympathetic activity, which affects renal hemodynamics and ultimately results in the observed salt sensitivity of BP (31). Studies have suggested the role of the sympathetic nervous system in salt sensitivity of BP as indicated by increased response to the cold pressor test (32), higher plasma norepinephrine levels (33), higher dopamine levels (34), and decreased number of β2-adrenergic receptors (35).
The present study has several strengths. To our knowledge, this investigation is the largest population-based feeding study in which salt sensitivity was examined. The compliance of subjects to the dietary intervention was excellent, as evidenced by multiple 24-hour urinary excretion assessments. Strict data quality control was enforced to ensure the validity of the results. Careful measurement of study variables, and the outcome variable in particular, allowed for precise and accurate estimation of the association. To minimize measurement bias during the assessment of BP, a minimum of 9 readings were obtained from multiple clinical visits by the same trained observers using the same random-zero sphygmomanometer during each phase of the study. This study not only assessed leisure-time activity but also incorporated work-related activity.
One potential limitation of our study is the short duration of the intervention period. Exposure to a 1-week low-sodium intervention and 1-week high-sodium intervention is the standard procedure for studying salt sensitivity. The relation of such a relatively short intervention to future health effects is not known definitively. However, in the Olivetti Heart Study, BP response to a short-term (3-day) dietary sodium intervention was associated with incidence of hypertension in long-term follow-up (36). Furthermore, previous clinical studies have shown that the methodology used to estimate salt sensitivity in this study is reproducible (37, 38). Another potential limitation is the generalizability of study findings. This study was conducted in a farming population in China who had a relatively high overall level of physical activity. Whereas the majority of this study population engaged in work-related activity of moderate (50.3%) or vigorous intensity (37.9%), the prevalence of moderate-intensity work in the United States is estimated to be 20% (39). On average, Genetic Epidemiology Network of Salt Sensitivity Study participants spent 3.3 hours in vigorous activity and 4.6 hours in moderate activity per day, and US adults spent less than 2 hours in vigorous activity and 1.5–2.2 hours in moderate activity per week (40). Because of this, we might not be able to see the extent of the protective effect of physical activity on sodium sensitivity. However, we should expect an even larger effect of dietary sodium intake on BP in a much less physically active population. Lastly, we were unable to assess potential confounding of the relation between physical activity and salt sensitivity of BP by diet characteristics because of a lack of detailed information collected on usual diet from standard measurement tools, such as food frequency questionnaires or 24-hour dietary recalls.
In summary, our study indicates that physical activity is significantly, independently, and inversely related to salt sensitivity of BP, with a graded dose-response association between lower level of physical activity and higher salt sensitivity. Among the study participants who were physically inactive, BP response to high salt consumption was greater than that among persons who were physically active. However, BP response to salt consumption was observed at every level of physical activity. Our findings suggest that physical activity may be particularly effective in lowering BP among salt-sensitive individuals.
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, School of Public Health and Tropical Medicine, Tulane University, New Orleans, Louisiana (Casey M. Rebholz, Lydia A. Bazzano, Jiang He); Cardiovascular Institute and Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, and National Center for Cardiovascular Disease, Beijing, China (Dongfeng Gu, Jian-Feng Huang, Jie Cao, Ji-Chun Chen, Jianxin Li); Department of Medicine, School of Medicine, Tulane University, New Orleans, Louisiana (Jing Chen, Lydia A. Bazzano, Jiang He); Institute of Basic Medicine, Shandong Academy of Medical Sciences, Shandong, China (Fanghong Lu); Department of Medicine, Xi'an Jiaotong University School of Medicine, Shanxi, China (Jianjun Mu); Shandong Center for Diseases Control and Prevention, Shandong, China (Jixiang Ma); School of Public Health, Zhengzhou University, Henan, China (Dongsheng Hu); Xinle Traditional Chinese Medicine Hospital, Hebei, China (Xu Ji); and National Laboratory of Medical Molecular Biology, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China (Depei Liu).
This work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (grants U01HL072507, R01HL087263, and R01HL090682).
Conflict of interest: none declared.
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288(15):1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 3.Carnethon MR, Evans NS, Church TS, et al. Joint associations of physical activity and aerobic fitness on the development of incident hypertension: coronary artery risk development in young adults. Hypertension. 2010;56(1):49–55. doi: 10.1161/HYPERTENSIONAHA.109.147603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 5.Jones DW. Dietary sodium and blood pressure. Hypertension. 2004;43(5):932–935. doi: 10.1161/01.HYP.0000126610.89002.c6. [DOI] [PubMed] [Google Scholar]
- 6.Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007;356(19):1966–1978. doi: 10.1056/NEJMra064486. [DOI] [PubMed] [Google Scholar]
- 7.Elliott P, Stamler J, Nichols R, et al. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. BMJ. 1996;312(7041):1249–1253. doi: 10.1136/bmj.312.7041.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 9.Cutler JA, Follmann D, Allender PS. Randomized trials of sodium reduction: an overview. Am J Clin Nutr. 1997;65(suppl):643–651. doi: 10.1093/ajcn/65.2.643S. [DOI] [PubMed] [Google Scholar]
- 10.Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27(3):481–490. doi: 10.1161/01.hyp.27.3.481. [DOI] [PubMed] [Google Scholar]
- 11.Vollmer WM, Sacks FM, Ard J, et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135(12):1019–1028. doi: 10.7326/0003-4819-135-12-200112180-00005. [DOI] [PubMed] [Google Scholar]
- 12.He J, Gu D, Chen J, et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens. 2009;27(1):48–54. doi: 10.1097/hjh.0b013e328316bb87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris RC, Sebastian A, Forman A, et al. Normotensive salt sensitivity: effects of race and dietary potassium. Hypertension. 1999;33(1):18–23. doi: 10.1161/01.hyp.33.1.18. [DOI] [PubMed] [Google Scholar]
- 14.GenSalt Collaborative Research Group. GenSalt: rationale, design, methods and baseline characteristics of study participants. J Hum Hypertens. 2007;21(8):639–646. doi: 10.1038/sj.jhh.1002207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paffenbarger RS, Blair SN, Lee I, et al. Measurement of physical activity to assess health effects in free-living populations. Med Sci Sports Exerc. 1993;25(1):60–70. doi: 10.1249/00005768-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88(5):2460–2470. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan JM. Salt sensitivity. Definition, conception, methodology, and long-term issues. Hypertension. 1991;17(suppl I):I-61–I-68. doi: 10.1161/01.hyp.17.1_suppl.i61. [DOI] [PubMed] [Google Scholar]
- 18.Tudor-Locke C, Ainsworth BE, Washington TL, et al. Assigning metabolic equivalent values to the 2002 census occupational classification system. J Phys Act Health. 2011;8(4):581–586. doi: 10.1123/jpah.8.4.581. [DOI] [PubMed] [Google Scholar]
- 19.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 20.Cutler JA, Sorlie PD, Wolz M, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 21.Morimoto A, Uzu T, Fujii T, et al. Sodium sensitivity and cardiovascular events in patients with essential hypertension. Lancet. 1997;350(9093):1734–1737. doi: 10.1016/S0140-6736(97)05189-1. [DOI] [PubMed] [Google Scholar]
- 22.Weinberger MH, Fineberg NS, Fineberg SE, et al. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001;37(Pt 2):429–432. doi: 10.1161/01.hyp.37.2.429. [DOI] [PubMed] [Google Scholar]
- 23.Bernstein AM, Willett WC. Trends in 24-h urinary sodium excretion in the United States, 1957–2003: a systematic review. Am J Clin Nutr. 2010;92(5):1172–1180. doi: 10.3945/ajcn.2010.29367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gill JM. Physical activity, cardiorespiratory fitness and insulin resistance: a short update. Curr Opin Lipidol. 2007;18(1):47–52. doi: 10.1097/MOL.0b013e328012b8bd. [DOI] [PubMed] [Google Scholar]
- 25.Chen J, Gu D, Huang J, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009;373(9666):829–835. doi: 10.1016/S0140-6736(09)60144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galletti F, Strazzullo P, Ferrara I, et al. NaCl sensitivity of essential hypertensive patients is related to insulin resistance. J Hypertens. 1997;15(12):1485–1491. doi: 10.1097/00004872-199715120-00017. [DOI] [PubMed] [Google Scholar]
- 27.Paterick TE, Fletcher GF. Endothelial function and cardiovascular prevention: role of blood lipids, exercise, and other risk factors. Cardiol Rev. 2001;9(5):282–286. doi: 10.1097/00045415-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Hambrecht R, Wolf A, Gielen S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med. 2000;342(7):454–460. doi: 10.1056/NEJM200002173420702. [DOI] [PubMed] [Google Scholar]
- 29.Tolins JP, Shultz PJ. Endogenous nitric oxide synthesis determines sensitivity to the pressor effect of salt. Kidney Int. 1994;46(1):230–236. doi: 10.1038/ki.1994.264. [DOI] [PubMed] [Google Scholar]
- 30.Mueller PJ. Exercise training and sympathetic nervous system activity: evidence for physical activity dependent neural plasticity. Clin Exp Pharmacol Physiol. 2007;34(4):377–384. doi: 10.1111/j.1440-1681.2007.04590.x. [DOI] [PubMed] [Google Scholar]
- 31.Strazzullo P, Barbato A, Vuotto P, et al. Relationships between salt sensitivity of blood pressure and sympathetic nervous system activity: a short review of evidence. Clin Exp Hypertens. 2001;23(1–2):25–33. doi: 10.1081/ceh-100001194. [DOI] [PubMed] [Google Scholar]
- 32.Chen J, Gu D, Jaquish CE, et al. Association between blood pressure responses to the cold pressor test and dietary sodium intervention in a Chinese population. Arch Intern Med. 2008;168(16):1740–1746. doi: 10.1001/archinte.168.16.1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campese VM, Romoff MS, Levitan D, et al. Abnormal relationship between sodium intake and sympathetic nervous system activity in salt-sensitive patients with essential hypertension. Kidney Int. 1982;21(4):371–378. doi: 10.1038/ki.1982.32. [DOI] [PubMed] [Google Scholar]
- 34.Gill JR, Grossman E, Goldstein DS. High urinary dopa and low urinary dopamine-to-dopa ratio in salt-sensitive hypertension. Hypertension. 1991;18(5):614–621. doi: 10.1161/01.hyp.18.5.614. [DOI] [PubMed] [Google Scholar]
- 35.Kotanko P, Höglinger O, Skrabal F. Beta 2-adrenoceptor density in fibroblast culture correlates with human NaCl sensitivity. Am J Physiol. 1992;263(3):623–627. doi: 10.1152/ajpcell.1992.263.3.C623. [DOI] [PubMed] [Google Scholar]
- 36.Barba G, Galletti F, Cappuccio FP, et al. Incidence of hypertension in individuals with different blood pressure salt-sensitivity: results of a 15-year follow-up study. J Hypertens. 2007;25(7):1465–1471. doi: 10.1097/HJH.0b013e3281139ebd. [DOI] [PubMed] [Google Scholar]
- 37.Sharma AM, Schattenfroh S, Kribben A, et al. Reliability of salt-sensitivity testing in normotensive subjects. Klin Wochenschr. 1989;67(12):632–634. doi: 10.1007/BF01718145. [DOI] [PubMed] [Google Scholar]
- 38.Draaijer P, de Leeuw P, Maessen J, et al. Salt-sensitivity testing in patients with borderline hypertension: reproducibility and potential mechanisms. J Hum Hypertens. 1995;9(4):263–269. [PubMed] [Google Scholar]
- 39.Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6(5):e19657. doi: 10.1371/journal.pone.0019657. (doi:10.1371/journal.pone.0019657) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spees CK, Scott JM, Taylor CA. Differences in amounts and types of physical activity status in US adults. Am J Health Behav. 2012;36(1):56–65. doi: 10.5993/ajhb.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]