Abstract
The success of antiretroviral therapy (ART) programmes requires high adherence and retention in care. In light of healthcare shortages, group interventions may be optimal ways to deliver information and provide support to ART patients. This study assessed the acceptability of a group intervention for patients and their supporters, which aimed to decrease stigma, harness social support and improve adherence. 28 ART patients attended a four-hour group intervention and 11 brought someone they identified as a potential supporter. The intervention was led by HIV-infected facilitators and included interactive sessions on HIV, ART, caregiving, stigma and disclosure. Participants completed intake and exit interviews and participated in focus group discussions. Participants rated the intervention favourably and in FGDs patients said they gained knowledge about adherence, felt empowered to tackle stigma and disclose, and experienced reductions in loneliness. Supporters reported they learned how to provide better care, gained knowledge, and felt closer to the person they were taking care of. Both patients and supporters saw HIV-infected facilitators as role models. Opinions were mixed about benefits of combining patients and supporters in the same intervention due to confidentiality. The group intervention showed potential to reduce stigma, increase social support, and improve adherence to therapy.
Keywords: antiretroviral therapy, adherence, intervention, Tanzania, HIV/AIDS
Background
HIV is a major health concern in Tanzania, where an estimated 6.6% of women and 4.6% of men are HIV serpositive (Measure DHS 2008). In response to the increasing burden of HIV, the Tanzanian National AIDS Control Programme provides free antiretroviral therapy (ART) in government-coordinated care and treatment centres (CTC’s) across the country. At the most recent estimate, approximately 235,012 people were receiving ART and 454,681 were enrolled in HIV care, representing 21.5% of the estimated 2.1 million people living with HIV/AIDS in the country (Tanzanian National AIDS Control Programme 2009). As access to antiretroviral therapy (ART) expands to meet the need, and people are consequently living longer with HIV, more efforts need to be made to ensure adherence to therapy and improve the quality of life of those who are infected. Such efforts must take into account the already stretched health care system, which is limited in its ability to provide high-quality care for all ART patients that need it (Hanson et al. 2009).
Proper adherence to ART regimens is imperative to maximise therapeutic success and avoid drug resistance (Nieuwkerk et al. 2005, Bangsberg 2006, Bangsberg 2008). However, approximately 23% of patients in sub-Saharan Africa do not meet proper treatment adherence criteria (Mills et al. 2006b), and adherence to therapy and continuation in care often decreases over time (Howard et al. 2002, Aboubacrine et al. 2007, Rosen et al. 2007). It is generally agreed that patients need to maintain at least 95% adherence in order to minimize risk of virological failure (Paterson et al. 2000, Bangsberg 2006). For patients taking a twice-a-day drug regimen, 95% adherence translates into missing no more than one pill every 10 days. The challenges of maintaining high levels of adherence have been documented in both North America and sub-Saharan Africa (Mills et al. 2006a, Mills et al. 2006b), including Tanzania (Hardon et al. 2006, Hardon et al. 2007, Ramadhani et al. 2007, Watt et al. 2010) In addition, retention in care has proven to be a challenge in African settings (Rosen et al. 2007), including Tanzania (Roura et al. 2009, Wringe et al. 2009).
Stigma (Mahajan et al. 2008, Visser et al. 2009), disclosure (Ramadhani et al. 2007, Greeff et al. 2008, King et al. 2008, Mayfield Arnold et al. 2008) and lack of social support (DiMatteo 2004, Murphy et al. 2004) are important factors that impact HIV patients’ adherence to therapy and retention in care. HIV-related stigma is prevalent in Tanzania (Genberg et al. 2009) and is associated with low social support and limited HIV disclosure (Khumalo-Sakutukwa et al. 2008). HIV related stigma stems in part from fear of death, fear of the burden of caring for HIV infected patients, and fear of transmission of HIV (Maman et al. 2009). Reducing both perceived and experienced stigma can lead to HIV disclosure and the harnessing of social support, which in turn can facilitate adherence through reminders to take medication, provision of food and money, and emotional encouragement (Kumarasamy et al. 2005, Bikaako-Kajura et al. 2006, Watt et al. 2009). Additionally, social support is important for mitigating negative psychological sequelae from an HIV diagnosis and meeting financial obligations (Holmes et al. 2007).
Models for adherence interventions in higher resource countries such as the United States often rely on intensive individual counselling by trained professionals, telephone follow up, or mechanisms such as pagers or financial incentives (Haddad et al. 2000, Simoni et al. 2003, Cote et al. 2005, Simoni et al. 2008). In developing country settings, where limited financial and human resources do not permit such intensive interventions, a community-based approach that pairs ART patients with lay counsellors is often used to promote patients’ adherence (Behforouz et al. 2004, Coetzee et al. 2004, Koenig et al. 2004). However, such interventions continue to be individual and long-term in nature, and therefore face challenges in reaching all the patients who might benefit.
In light of the importance of sustaining adherence to ART, and the influence of stigma and social support on adherence outcomes, we developed and examined the acceptability of a group intervention addressing these issues for new ART patients in Arusha, Tanzania. In particular, we were interested in 1) whether new ART initiates would attend a group intervention outside of clinic hours, 2) whether they would choose to bring a treatment supporter with them, and 3) how the intervention would be perceived as addressing the needs of ART initiates and their treatment supporters in this setting. The findings help to identify important components for cost effective interventions to support the growing number of people starting ART in Tanzania and beyond.
Description of the intervention
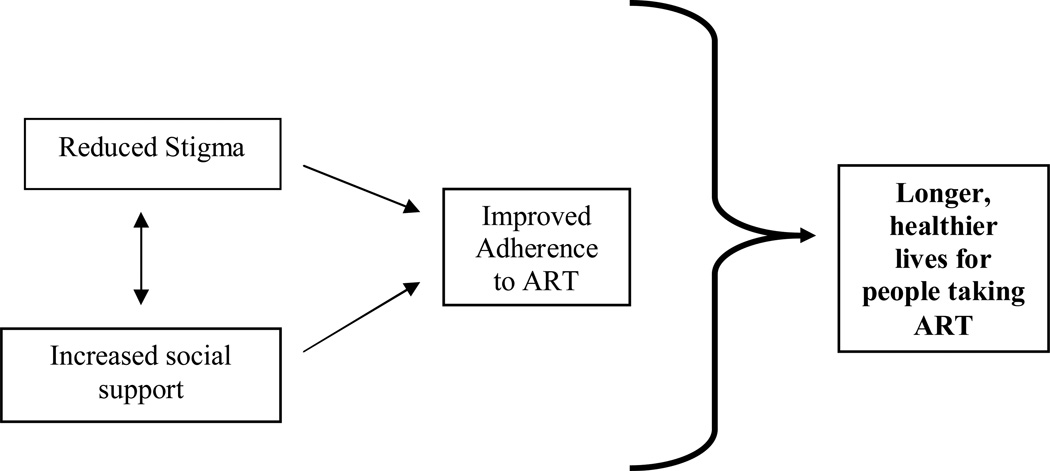
The aim of the intervention was to support longer, healthier lives for people living with HIV, specifically by decreasing HIV related stigma, increasing social support, and therefore improving adherence to ART (Figure 1). To inform the intervention, we conducted four focus group discussions (FGDs) with ART patients (selected based on participation in prior research), family members of ART patients (identified through the patient participants), health care providers (including all providers at the study clinic who provided direct care to ART patients), and HIV infected counsellors (all employed at the study clinic). The FGDs were facilitated by the last author (MJ), were transcribed in Kiswahili and translated into English. Themes were identified by closely reading the transcripts and highlighting topics to be covered in the intervention, issues of administration, and potential barriers for attendance. The FGDs suggested that new ART patients required information on the following: basic information about ART and how to use the medication, adherence, clinical care, healthy living, diet and nutrition, sexual activity, psychological issues, social support, disclosure and stigma. In addition, data suggested that treatment supporters of patients also required information about those topics, as well as specific information about meeting the physical and emotional needs of someone who is HIV infected and taking ART, and communicating effectively about HIV. The FGDs identified potential barriers to participation in an intervention, including transportation money, lack of time, and fear of stigma and involuntary disclosure. It was suggested that HIV-positive facilitators would best deliver the intervention, as a way to mitigate potential stigma and open up more honest discussions.
Figure 1.
Conceptual Framework of Pilot Intervention
Based on the themes that emerged from the FGDs, the authors worked together with the two identified facilitators (described below) to develop a four-hour group intervention for patients beginning ART, along with their self-selected treatment supporter (e.g., a family member or friend). The intervention focused on new ART initiates (taking ART for less than six months) because prior research we conducted (Watt et al. 2009) pointed to the importance of the initial treatment period for gaining skills and knowledge that would allow patients to succeed on ART.
The intervention, entitled “Zinduka”, Kiswahili for “stand up/wake up,” was developed in concordance with the social cognitive theory, which suggests that new behaviours and skills are best learned through observation and role playing (Baranowski et al. 2002). Two facilitators led the intervention, which included content on the basics about HIV and ART, caring for someone taking ART, stigma and disclosure. Role plays were used to create a safe environment for participants to learn communication and behavioural skills related to living with HIV and taking ART, and to facilitate open dialogue between patients and their supporters. The intervention was written up into a brief manual, which included all activities and a sample script for the facilitators, and it was translated into Kiswahili by the last author (MJ).
The two facilitators of the intervention were HIV infected individuals who were already active in the clinic and community as voluntary adherence counsellors (VACs). The VACs are trained by the clinic to provide support to ART patients in adhering to their medication. They receive a modest stipend from the clinic and are available to meet with patients during HIV clinic days and through home visits. The fact that the facilitators were living with HIV and taking ART from the study clinic meant that they could answer questions about what to expect over time and could provide insight into negotiating care at the clinic. Using HIV infected facilitators was also intended to provide a role model for living a positive and healthy life with HIV. The facilitators we chose had a secondary school education, were proficient in both Kiswahili and English, and had experience conducting workshops and making public presentations about HIV. They had substantial input into the development of the intervention, and received ongoing training on the content and delivery of the intervention, including several practice sessions.
Study site
The study was conducted in 2007 at a government supported faith based clinic in Arusha, Tanzania. The study clinic began offering ART in 2003 (at cost), and has offered free ART since 2004, funded by the United States Presidents Emergency Plan for AIDS Relief (PEPFAR). Patients are eligible for free ART from the study clinic if they have a CD4 count of less than 200 cells/mL or WHO clinical stage IV disease. The vast majority of ART patients at the time were prescribed Triomune (manufactured by Cipla in Mumbai, India), a twice-a-day single combination ART pill containing stavudine, lamivudine and nevirapine. Prior to beginning ART, patients meet with a qualified HIV counsellor for approximately 10 minutes to discuss ART treatment and potential side effects. Additionally, the clinic paired patients with one of 15 HIV infected lay counsellors (VAC’s), who were tasked with providing emotional and informational support to patients by making at least one visit to their homes and being available to meet with them during clinic hours. At the time of the study, the clinic was following over 1100 patients on ART and employed two doctors and two counsellors to provide ART-related services. Conversations with clinic management and providers prior to the study implementation revealed concerns about inconsistencies in the quality and quantity of information and support provided to ART initiates, and a perception that these challenges would increase as the ranks of ART patients continued to grow at the clinic.
Methods
During two distinct one-week periods, all patients (n=37) presenting at the study clinic who had been taking ART for fewer than six months were invited to participate in the study. Clinic counsellors identified eligible patients and referred them to a study recruiter. Potential participants were informed about the study, and, if they provided consent, were asked basic demographic questions including level of education, employment status, travel time to the clinic, modes of transportation used, and disclosure of HIV status. Pharmacy records were used to confirm age and start date of ART. Participants were given an invitation to an intervention the following Saturday, as well as an invitation to bring a treatment supporter of their choice. They were told that a treatment supporter was a family member or friend who knew about their HIV status and provided, or had the potential to provide, support to help them live positively with HIV.
On the day of the intervention, treatment supporters completed intake interviews to collect demographic information, and both ART patients and treatment supporters completed exit interviews, which included questions about what participants learned from the intervention and feedback to improve the intervention. Follow up phone calls were made to those who agreed to participate in the study but did not attend the intervention, in order to assess barriers for attendance. The second author (EA) and the last author (MJ) attended both intervention sessions to collect quality assurance data, including whether all 20 sub-sections of the intervention were covered in their entirety. All participants received compensation estimated to cover transportation costs to and from the group intervention (approximately $2).
Upon leaving the intervention, both groups of participants (ART patients and their treatment supporters) were invited to return later in the week to participate in a focus group discussion (FGD). Five FGDs were conducted, three for patients and two for those who attended the intervention as treatments supporters. The FGDs followed a semi-structured interview guide to elicit detailed feedback about the intervention, including how the intervention changed their perceptions of HIV and ART; how participants felt about the group setting and the engagement of treatment supporters in the program; and what recommendations they would have for revising the intervention. Each group lasted between 60 and 90 minutes, and participants received compensation for their time and transportation (approximately $2).
Six Tanzanian interviewers were trained to recruit patients and administer the research instruments. Half were female and four were living with HIV. The Tanzanian study coordinator (last author, MJ), who had specific training in qualitative methods, conducted all of the FGDs, together with a note taker. Demographic surveys, intake surveys and exit interviews were entered into Excel and basic frequencies were analyzed. The FGDs were audiorecorded, transcribed in Kiswahili, and translated into English. The first two authors (MW and EA) analyzed the focus group data through multiple readings of the transcripts and identification of common themes and patterns, until consensus was achieved. The data were further examined and summarized through descriptive text-based summaries and data display matrices (Miles et al. 1994). Representative, verbatim quotes were selected to illustrate key findings.
The study had IRB approval from the UNC School of Public Health and the Tanzanian Institute for Medical Research.
Results
Demographics
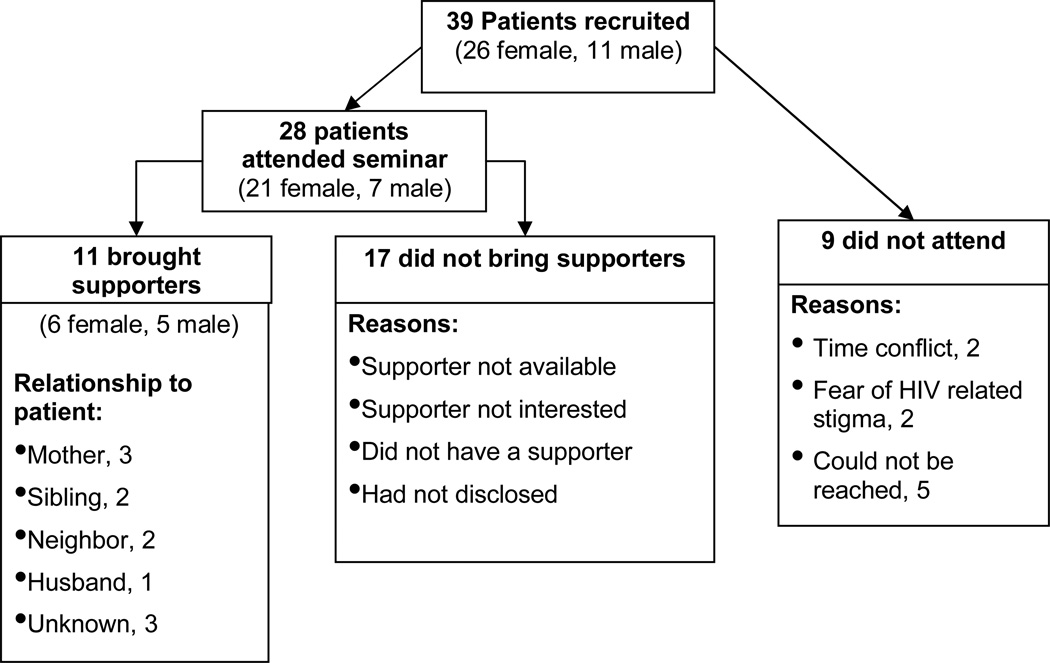
Of 37 recruited patients, 28 (76%) attended the intervention and 11 (39%) brought supporters (Figure 2). Of the nine patients who did not attend, only four could be reached by telephone. Reasons given for non-attendance included fear of HIV-related stigma (n=2) and time conflict (n=2). Participating patients included 21 women and seven men, with a mean age of 37.6 years. Participants had been taking ART between one and six months, with an average time on ART of 3.3 months. Seven (19%) had not disclosed to anyone at the time of recruitment. Only 13.8% of the participants had education beyond primary school, and 8% reported having paid employment. Quality assurance data revealed that the intervention was delivered as intended in the manual, with all 20 sections covered with participants in each session.
Figure 2.
Recruitment and attendance of participants
A total of 23 patients (82%) and 11 treatment supporters (100%) participated in focus group discussions following the interventions.
Exit interviews
During exit interviews, both patients and supporters rated the usefulness of the intervention in its entirety and divided into specific components. When asked to rate the intervention numerically on a scale of 1–5, ratings were overall favourable (Table 1). Both patients and treatment supporters gave the highest overall rating to “gaining information on ART.”
Table 1.
Participants’ ratings of the seminar on a scale of 1 (lowest) to 5 (highest) (n=39)
| Usefulness of seminar (by topic) | Patients | Treatment supporters | ||
|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | |
| Overall | 4.76 | 0.56 | 4.27 | 1.19 |
| Information on HIV | 4.68 | 0.71 | 4.55 | 0.69 |
| Information on ART | 4.90 | 0.50 | 4.45 | 0.82 |
| Information on use of ART | 4.76 | 0.47 | -- | -- |
| How to overcome stigma | 4.66 | 0.67 | -- | -- |
| How to talk to others on their HIV status | 4.24 | 1.20 | -- | -- |
| How to support someone who is HIV infected | -- | -- | 3.82 | 1.33 |
| How to support someone to adhere | -- | -- | 4.36 | 1.03 |
| How to support patients to live positively | -- | -- | 3.64 | 1.01 |
| How to support someone to disclose | -- | -- | 4.09 | 0.83 |
Focus group discussions
Qualitative findings revealed key benefits of the intervention, in particular that the intervention increased social support, reduced loneliness, helped participants to see HIV as a “normal disease”, and reduced both internalized and externalized stigma. In addition, participants reported that they appreciated the opportunity to learn necessary information about ART and correct rumours, which for the supporters alleviated their hesitation in caring for someone living with HIV.
Reductions in stigma and loneliness through normalizing HIV
Both patients and supporters talked about how the intervention helped them to see HIV as a normal disease that affected many people, and that it therefore reduced their own perceptions of HIV stigma. This came in large part through the group setting, which facilitated interacting with others who were HIV infected.
It helped me to see this problem as any other normal problem and I got new ideas of living positively. It helped me reduce worries after seeing that this is a problem that a lot of people are concerned with. (Female patient on ART)
Treatment supporters similarly reported that the intervention helped to normalize the disease, which in turn increased their confidence to provide effective support.
This seminar will enable us to help our patients effectively. And it has helped us to see the patient as a normal person. (Male supporter)
Participants felt that the intervention reduced both their perceived and internalized stigma, which can be detrimental to positive living with ART. This impact on alleviating stigma was in large part due to the presence of healthy, confident facilitators who were open about their HIV, as this participant pointed out:
First, we are so grateful that even the facilitators have the problem the same as ours, and are the people who are very much experienced about living positively and they have used ARTs for a long time. This encourages us that we can live longer like our facilitators. (Female patient on ART)
Treatment supporters also reported benefits from their exposure to the facilitators, conveying that it challenged their notions about the association between HIV and death.
Once, a lot of people were despaired that if you get this problem then that’s your end, but after attending the seminar you find that you can continue to live. (Female supporter)
Benefits of the intervention for adherence
Participants talked about how the intervention provided important information about ART and adherence, and in particular that it helped to correct prior misconceptions. In some cases, patients had not previously grasped the importance of taking the pill every day at the same time, and in other cases, they had heard that it was essential to take the pill at the same time, but this was taken to a detrimental extreme.
I was taking my pills at 8:00 and even 20 minutes after the time I was not taking it… I was skipping until the next dose. But after the seminar I learned that you can still take your pill if you forgot. (Female patient on ART)
The seminar therefore helped patients to understand the important principle of adherence, but to hone their own judgement about having some flexibility, and importantly to feel empowered to seek advice from a health care provider or counsellor if they had questions related to adherence. The intervention also helped to correct misunderstandings that one would eventually be able to stop taking ART; that ART will stop working after a few years; and that taking ART will lead to an earlier death.
Through the role plays and discussions in the intervention, participants said they learned strategies to facilitate consistent use of ART. These strategies included finding a private place to take their pills if a neighbour or friend was visiting who didn’t know about their infection, and using a calendar to track pill taking and reduce the chance of taking more pills than prescribed. Treatment supporters also reported learning the importance of reminding patients to take their pills on time.
Additionally, participants said the intervention made them generally more comfortable with the idea of taking ART, because of both a realization that the medication will improve their health and prolong their lives, and a perception that they are not alone in taking ART. As people felt more comfortable with the idea of taking ART, they also felt more motivated to take the pills correctly and consistently.
When I came to this seminar I learned about these pills, that if I will use it, it will help me. Because [before] I was not trusting these pills. (Female patient on ART)
When I took these pills on the first day I cried a lot. But when I came to this seminar I see it’s normal, there are a lot of people who use the pills. (Female patient on ART)
Balancing need for social support and fear of disclosure
The majority of participants (76% of patients and 91% of supporters) were in support of an intervention format that combined both patients and their supporters. Those who expressed that they did not feel comfortable with a combined seminar were concerned with confidentiality and involuntary disclosure of their HIV status in the larger community.
In support of a group seminar that combined patients and supporters, participants suggested that the group setting reduced a sense of loneliness, as illustrated by this woman:
I was really comforted after seeing live the people who have lived many years with HIV. (Female patient on ART)
By coming together that helped us to see this problem is the problem of all. (Female supporter)
Participants also recognized that combining patients and supporters had a benefit of bringing patients and their supporters closer together, and sharing information that could later be reinforced in the home environment.
It would be very hard to come into agreement if everybody [patients and supporters] attended different seminars. But when you are together, you remind each other of what you learned… By attending the seminar together, it brings you closer, and even if he gets any problem it becomes easy for you to help him, because you know what you’re supposed to do. (Male supporter)
On the other hand, some participants suggested that a group setting introduced the fear of breaches in confidentiality and involuntary disclosure of patients’ HIV status in the broader community, as expressed by both a patient and a supporter.
They have to have their own day [intervention], because I think they won’t keep the secret to people in the streets. This is different for us as patients because we have the same problem then we can keep each other’s secret. (Female patient on ART)
But because of the need of secrets, it seems more important to attend different groups, because not all the treatment supporters can keep the secret of other patients. (Male supporter)
The intervention not only provided skills to disclose, but also provided positive models for disclosure by seeing patients together with their supporters. In one FGD, a patient who had not brought a treatment supporter to the intervention revealed that the intervention had encouraged her to disclose her HIV status to a relative for the first time in the days following the intervention.
Supporters remarked on benefiting from the group setting, which provided an opportunity to show support for their friend of family member taking ART. In the FGDs during the intervention development, supporters expressed feeling helpless on how to be of most comfort and help to their loved ones, so the intervention provided concrete ways for them to express and offer support, and opened up dialogue between patients and supporters, as expressed by these participants.
Actually, we were very happy, because we took the occasion to comfort them. (Female supporter)
It was an important occasion of showing great love. (Female supporter)
Discussion
Adherence to therapy (Mills et al. 2006b) and retention in care (Rosen et al. 2007) pose significant challenges to the scale-up of ART programs in sub-Saharan Africa. Providing adequate and consistent information and support to new ART initiates is essential to meet this challenge, but may be hampered due to shortages of health care providers and growing ranks of ART patients. A brief group intervention for ART initiates and their treatment supporters offers a likely cost-effective means to prepare patients for lifetime ART use, to increase social support, and to address psychosocial issues such as disclosure and stigma. In this study, we developed such an intervention and demonstrated its acceptability in a Tanzanian setting.
Prior to study implementation, clinic staff and counsellors were rightfully concerned about whether patients would attend a group intervention and whether they would invite and bring a treatment supporter. They noted patients’ fears of making their HIV status public and the logistical challenges that may interfere with their coming to the clinic on a weekend. However, high attendance rates (76% of those recruited) and the fact that a large proportion of patient attendees (39%) brought a treatment supporter confirmed that a group intervention such as this, offered outside of clinic hours, is acceptable in this setting.
Participants reported that they gained important and useful knowledge from the intervention, which indicates that the information was clearly presented and relevant to participants’ lives. In a low resource setting where trained health care providers are in short supply (Naicker et al. 2009), delivering this information in a consistent way in a group environment can ensure that all new patients and their supporters receive information necessary for them to effectively understand and manage their HIV infection and initiation onto therapy.
Perhaps even more importantly than delivering information, the intervention structure helped to normalize HIV infection, and in turn had an impact on both self stigma and perceived stigma. The benefits of group interventions on psychosocial factors among HIV infected people have been documented elsewhere (Hyde et al. 2005). In this setting, there was evidence that engaging HIV infected role models helped to reduce internalized shame and stigma and facilitate HIV disclosure. The inclusion of treatment supporters and patients in the same intervention resulted in mixed feedback. While both groups pointed to the advantages of harnessing and strengthening patients’ social support, there was also an expressed concern that the group setting may compromise the confidentiality of participants’ HIV status. Although the majority found that the benefits of a group setting outweighed any potential risks, future studies may explore potential advantages of segregated interventions or an option to choose either combined or separate groups.
The targeting of the intervention to patients who are initiating ART has significant advantages. The first few months of initiating ART requires additional information and support to navigate care, manage side effects and develop a routine for medication adherence. By conducting an intervention during the early stages of ART treatment, there is the potential to expedite the process of disclosure, which can lead to acquiring the social support and tools needed to adhere to medication and remain in care (Watt et al. 2009).
We found that using HIV infected facilitators was a particular advantage of this intervention. HIV infected counsellors as mentors and role models have been used by community-based organizations since the beginning of the epidemic, but few interventions have evaluated their impact (Simoni et al. 2007). In this setting, the fact that the facilitators were already engaged in providing care at the study site made their participation even more effective. The two facilitators we used had secondary school education and previous experience leading groups for HIV infected people. Although we did not follow participants over time, it is possible that some participants may have had follow up with the facilitators in the months after the intervention, since the facilitators were always present during HIV clinic days at the study site. Although not measured or reported, engaging HIV infected individuals as facilitators and research assistants may have had added benefit for those individuals themselves in building their skill set and helping them to become stronger advocates for HIV in their communities.
This study was limited by several factors, including a short time period, small sample size, single study site, participant self-selection, and lack of behaviour change data. The number of participants who were eligible to participate in the study but chose not to be referred to the study coordinator was not documented, although referring counsellors anecdotally said that a small handful of people chose not to be referred because they lacked time on their appointment day. Not having data about referral refusals over-estimates our uptake of the intervention, and provides an indication that the intervention may not be appealing or feasible for certain groups (e.g., those with employment or other regular responsibilities). Additionally, there were 5 patient participants (out of 28) who did not attend a FGD to give feedback on the intervention. It is possible that those who did not attend a FGD were people who were less satisfied with, or less invested in, the intervention, which may therefore bias our conclusions about its acceptability. The intervention was piloted in a relatively small, faith-based clinic, which offered important support systems for patients, including individual counselling and pairing with an HIV-infected peer counsellor. It is possible that the observed feasibility and acceptability was in part a factor of the setting, and that the results would not be replicated in other settings, in particular large public clinics with a less personal nature.
Conclusions
Despite its limitations, the study points to the potential acceptability and feasibility of a group intervention for new ART initiates and their treatment supporters in a low resource setting, facilitated by HIV positive individuals. The high rate of attendance and positive assessments from both patients and their supporters are encouraging and suggest the need for a more rigorous evaluation of such an intervention. Further research may consider the added value of a multi-session intervention, although it should keep in mind the cost and feasibility of the intervention format for scale up. Future studies should also explore the most appropriate stage of treatment for patients to attend such an intervention, and whether patients and supporters should be included in the same or different groups.
As the number of people taking ART in low-resource settings continues to increase, and additional pressures are put on already stretched health care systems, it is imperative that we identify low-cost and feasible interventions to ensure that ART initiates have adequate information and support to retain them in care and bolster their adherence to therapy. A brief group intervention that involves ART patients and their treatment supporters and is facilitated by HIV infected lay counsellors may meet this need and should be evaluated further.
Acknowledgements
This study was conducted while the first author was a student at the University of North Carolina Gillings School of Global Public Health. Funding was provided by the GSK UNC-Duke Global Health Program, funded by the GSK Foundation. The authors appreciate the support of the Duke Center for AIDS Research in the preparation of the manuscript.
References
- Aboubacrine SA, Niamba P, Boileau C, Zunzunegui MV, Machouf N, Nguyen VK, Rashed S. Inadequate adherence to antiretroviral treatment and prevention in hospital and community sites in Burkina Faso and Mali: a study by the ATARAO group. International Journal of STD and AIDS. 2007;18(11):741–747. doi: 10.1258/095646207782212243. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clinical Infectious Diseases. 2006;43(7):939–941. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR. Preventing HIV antiretroviral resistance through better monitoring of treatment adherence. Journal of Infectious Diseases. 2008;197(Suppl 3):S272–S278. doi: 10.1086/533415. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Perry C, Parcel G. How individuals, environments, and health behavior interact: Social Cognitive Theory. In: Glanz K, Rimer B, Lewis FM, editors. Health Behavior and Health Education: Theory, research and practice. San Francisco: Jossey-Bass; 2002. pp. 165–184. [Google Scholar]
- Behforouz HL, Farmer PE, Mukherjee JS. From directly observed therapy to Accompagnateurs: Enhancing AIDS treatment outcomes in Haiti and in Boston. Clinical Infectious Diseases. 2004;38:S429–S436. doi: 10.1086/421408. [DOI] [PubMed] [Google Scholar]
- Bikaako-Kajura W, Luyirika E, Purcell DW, Downing J, Kaharuza F, Mermin J, Malamba S, Bunnell R. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS and Behavior. 2006;10(4 Suppl):S85–S93. doi: 10.1007/s10461-006-9141-3. [DOI] [PubMed] [Google Scholar]
- Coetzee D, Boulle A, Hildebrand K, Asselman V, Van Cutsem G, Goemaere E. Promoting adherence to antiretroviral therapy: the experience from a primary care setting in Khayelitsha, South Africa. AIDS. 2004;18(Suppl 3):S27–S31. doi: 10.1097/00002030-200406003-00006. [DOI] [PubMed] [Google Scholar]
- Cote JK, Godin G. Efficacy of interventions in improving adherence to antiretroviral therapy. International Journal of STD and AIDS. 2005;16(5):335–343. doi: 10.1258/0956462053888934. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Genberg BL, Hlavka Z, Konda KA, Maman S, Chariyalertsak S, Chingono A, Mbwambo J, Modiba P, Van Rooyen H, Celentano DD. A comparison of HIV/AIDS-related stigma in four countries: negative attitudes and perceived acts of discrimination towards people living with HIV/AIDS. Social Science and Medicine. 2009;68(12):2279–2287. doi: 10.1016/j.socscimed.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeff M, Phetlhu R, Makoae LN, Dlamini PS, Holzemer WL, Naidoo JR, Kohi TW, Uys LR, Chirwa ML. Disclosure of HIV status: experiences and perceptions of persons living with HIV/AIDS and nurses involved in their care in Africa. Qualitative Health Research. 2008;18(3):311–324. doi: 10.1177/1049732307311118. [DOI] [PubMed] [Google Scholar]
- Haddad M, Inch C, Glazier RH, Wilkins AL, Urbshott G, Bayoumi A, Rourke S. Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane Database of Systematic Reviews. 2000;(3):CD001442. doi: 10.1002/14651858.CD001442. [DOI] [PubMed] [Google Scholar]
- Hanson S, Thorson A, Rosling H, Ortendahl C, Hanson C, Killewo J, Ekstrom AM. Estimating the capacity for ART provision in Tanzania with the use of data on staff productivity and patient losses. PLoS ONE. 2009;4(4):e5294. doi: 10.1371/journal.pone.0005294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, Kglatwane J, Kinsman J, Kwasa R, Maridadi J, Moroka TM, Moyo S, Nakiyemba A, Nsimba S, Ogenyi R, Oyabba T, Temu F, Laing R. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19(5):658–665. doi: 10.1080/09540120701244943. [DOI] [PubMed] [Google Scholar]
- Hardon AP, Davey S, Gerrits T, Hodgkin C, Irunde HF, Kgatlwane J, Kinsman J, Nakiyemba A, Laing R. From access to adherence: The challenges of antiretroviral treatment: Studies from Botswana, Tanzania and Uganda. Geneva: World Health Organization; 2006. [Google Scholar]
- Holmes WC, Bilker WB, Wang H, Chapman J, Gross R. HIV/AIDS-specific quality of life and adherence to antiretroviral therapy over time. Journal of Acquired Immune Deficiency Syndrome. 2007;46(3):323–327. doi: 10.1097/QAI.0b013e31815724fe. [DOI] [PubMed] [Google Scholar]
- Howard AA, Arnsten JH, Li YT, Vlahov D, Rich JD, Schuman P, Stone VE, Smith DK, Schoenbaum EE. A prospective study of adherence and viral load in a large multi-center cohort of HIV-infected women. AIDS. 2002;16(16):2175–2182. doi: 10.1097/00002030-200211080-00010. [DOI] [PubMed] [Google Scholar]
- Hyde J, Appleby PR, Weiss G, Bailey J, Morgan X. Group-level interventions for persons living with HIV: a catalyst for individual change. AIDS Education and Prevention. 2005;17(1 Suppl A):53–65. doi: 10.1521/aeap.17.2.53.58699. [DOI] [PubMed] [Google Scholar]
- Khumalo-Sakutukwa G, Morin SF, Fritz K, Charlebois ED, van Rooyen H, Chingono A, Modiba P, Mrumbi K, Visrutaratna S, Singh B, Sweat M, Celentano DD, Coates TJ. Project Accept (HPTN 043): a community-based intervention to reduce HIV incidence in populations at risk for HIV in sub-Saharan Africa and Thailand. Journal of Acquired Immune Deficiency Syndrome. 2008;49(4):422–431. doi: 10.1097/QAI.0b013e31818a6cb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King R, Katuntu D, Lifshay J, Packel L, Batamwita R, Nakayiwa S, Abang B, Babirye F, Lindkvist P, Johansson E, Mermin J, Bunnell R. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS and Behavior. 2008;12(2):232–243. doi: 10.1007/s10461-007-9307-7. [DOI] [PubMed] [Google Scholar]
- Koenig SP, Leandre F, Farmer PE. Scaling-up HIV treatment programmes in resource-limited settings: the rural Haiti experience. AIDS. 2004;18(Suppl 3):S21–S25. doi: 10.1097/00002030-200406003-00005. [DOI] [PubMed] [Google Scholar]
- Kumarasamy N, Safren SA, Raminani SR, Pickard R, James R, Krishnan AK, Solomon S, Mayer KH. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care and STDs. 2005;19(8):526–537. doi: 10.1089/apc.2005.19.526. [DOI] [PubMed] [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, Szekeres G, Coates TJ. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Abler L, Parker L, Lane T, Chirowodza A, Ntogwisangu J, Srirak N, Modiba P, Murima O, Fritz K. A comparison of HIV stigma and discrimination in five international sites: the influence of care and treatment resources in high prevalence settings. Social Science and Medicine. 2009;68(12):2271–2278. doi: 10.1016/j.socscimed.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayfield Arnold E, Rice E, Flannery D, Rotheram-Borus MJ. HIV disclosure among adults living with HIV. AIDS Care. 2008;20(1):80–92. doi: 10.1080/09540120701449138. [DOI] [PubMed] [Google Scholar]
- Measure DHS. Tanzania HIV/AIDS Indicator Survey 2007–08. Calverton, Maryland: ORC Macro; 2008. [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis : an expanded sourcebook. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, Wilson K, Buchan I, Gill CJ, Cooper C. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006a;3(11):e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, Rachlis B, Wu P, Cooper C, Thabane L, Wilson K, Guyatt GH, Bangsberg DR. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006b;296(6):679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Hoffman D, Steers WN. Predictors of antiretroviral adherence. AIDS Care. 2004;16(4):471–484. doi: 10.1080/09540120410001683402. [DOI] [PubMed] [Google Scholar]
- Naicker S, Plange-Rhule J, Tutt RC, Eastwood JB. Shortage of healthcare workers in developing countries--Africa. Ethnicity and Disease. 2009;19(1 Suppl 1):S1-60–S1-64. [PubMed] [Google Scholar]
- Nieuwkerk PT, Oort FJ. Self-reported adherence to antiretroviral therapy for HIV-1 infection and virologic treatment response: a meta-analysis. Journal of Acquired Immune Deficiency Syndromes. 2005;38(4):445–448. doi: 10.1097/01.qai.0000147522.34369.12. [DOI] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Ramadhani HO, Thielman NM, Landman KZ, Ndosi EM, Gao F, Kirchherr JL, Shah R, Shao HJ, Morpeth SC, McNeill JD, Shao JF, Bartlett JA, Crump JA. Predictors of incomplete adherence, virologic failure, and antiviral drug resistance among HIV-infected adults receiving antiretroviral therapy in Tanzania. Clinical Infectious Diseases. 2007;45(11):1492–1498. doi: 10.1086/522991. [DOI] [PubMed] [Google Scholar]
- Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-saharan Africa: a systematic review. PLoS Medicine. 2007;4(10):e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roura M, Busza J, Wringe A, Mbata D, Urassa M, Zaba B. Barriers to sustaining antiretroviral treatment in Kisesa, Tanzania: a follow-up study to understand attrition from the antiretroviral program. AIDS Patient Care and STDs. 2009;23(3):203–210. doi: 10.1089/apc.2008.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Amico KR, Pearson CR, Malow R. Strategies for promoting adherence to antiretroviral therapy: a review of the literature. Current Infectious Disease Reports. 2008;10(6):515–521. doi: 10.1007/s11908-008-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Pantalone DW, Turner BJ. Antiretroviral adherence interventions: a review of current literature and ongoing studies. Topics in HIV Medicine. 2003;11(6):185–198. [PubMed] [Google Scholar]
- Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychology. 2007;26(4):488–495. doi: 10.1037/0278-6133.26.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanzanian National AIDS Control Programme. Dar es Salaam, Government of Tanzania: 2009. Review of the national patient monitoring system for HIV care and treatment in Tanzania. [Google Scholar]
- Visser MJ, Makin JD, Vandormael A, Sikkema KJ, Forsyth BW. HIV/AIDS stigma in a South African community. AIDS Care. 2009;21(2):197–206. doi: 10.1080/09540120801932157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Maman S, Earp JA, Eng E, Setel PW, Golin CE, Jacobson M. "It's all the time in my mind": facilitators of adherence to antiretroviral therapy in a Tanzanian setting. Social Science and Medicine. 2009;68(10):1793–1800. doi: 10.1016/j.socscimed.2009.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Maman S, Golin C, Earp J, Bangdiwala SI, Jacobson M. Factors associated with self reported adherence to antiretroviral therapy in a Tanzanian setting. AIDS Care. 2010;22(3):381–389. doi: 10.1080/09540120903193708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wringe A, Roura M, Urassa M, Busza J, Athanas V, Zaba B. Doubts, denial and divine intervention: understanding delayed attendance and poor retention rates at a HIV treatment programme in rural Tanzania. AIDS Care. 2009;21(5):632–637. doi: 10.1080/09540120802385629. [DOI] [PubMed] [Google Scholar]