Abstract
Exposure of the gastrointestinal (GI) tract to high doses of radiation can lead to lethality from the GI syndrome. Although the molecular mechanism regulating the GI syndrome remains to be fully defined, we have recently demonstrated that p53 within the GI epithelial cells controls the radiation-induced GI syndrome. Mice lacking p53 in the GI epithelium were sensitized to the GI syndrome, while transgenic mice with one additional copy of p53 called “Super p53” mice were protected from the GI syndrome. Here, we cross “Super p53” mice to p21−/− mice that lack the cyclin-dependent kinase inhibitor p21. Super p53; p21−/− mice are sensitized to the GI syndrome compared to Super p53 mice that retain one p21 allele. In addition, mice lacking p21 are not protected from the GI syndrome with one extra copy of p53. These results suggest that p21 protects “Super p53” mice from the GI syndrome.
INTRODUCTION
Currently, no therapy exists to mitigate against the acute gastrointestinal (GI) syndrome, a lethal radiation-induced sickness that occurs within 5–10 days after exposure of the abdomen to high doses of radiation (1). Death can occur as a consequence of damage to the crypt epithelium of the small intestine with shortening of the villi, which leads to an altered fluid and electrolyte transport, bacteremia and endotoxemia (1, 2). The need to develop countermeasures for potential exposure to radiation through radiological attack or disaster has increased the urgency for understanding the mechanism of the GI syndrome. However, the molecular mechanism that regulates the GI syndrome remains to be fully elucidated.
The response of the small intestine to radiation exposure is regulated by the tumor suppressor p53. In some cell types, activation of p53 by ionizing radiation leads to cell cycle arrest, which may allow time for repair of DNA damage. p53 promotes cell cycle arrest in part by inducing the cyclin-dependent kinase (cdk) inhibitor p21 (3–8). In other cell types, activation of p53 causes cell death by apoptosis (9). Two waves of apoptosis have been observed in the small intestine after radiation. One wave peaks 3–6 hours after exposure to relatively low doses of radiation (< 1 Gy) and requires p53 to activate the intrinsic pathway of apoptosis (10, 11). A second wave of cell death occurs 24 hours after exposure to larger doses of radiation (8 Gy) and appears to be a consequence of attempted mitosis with damaged chromosomes (12). This delayed apoptosis due to mitotic death was increased in the crypts of p53−/− mice (13). Mice deficient in p53 (i.e. p53−/−) do not demonstrate radiation-induced apoptosis of the crypt epithelium at 4 hours (12–14). Although this might be expected to protect mice from the GI syndrome, p53−/− mice are sensitized to the GI syndrome when compared to mice containing two copies of the wild-type p53 gene (15, 16) Mice lacking p53 show evidence of continuous crypt epithelial cell proliferation after radiation, which correlates with the accelerated death of damaged cells and rapid destruction of the surrounding intestinal tissue (6, 15). Therefore, p53-mediated cell cycle arrest may regulate the GI syndrome.
Recently, we used the Cre-loxP system to study the consequences of cell-type specific deletion of p53 on the GI syndrome (17). We observed that deletion of p53 in GI epithelial cells sensitized mice to the GI syndrome. Although deletion of p53 in endothelial cells did not affect the acute GI syndrome, these mice were sensitized to late effects of radiation. The mechanism by which p53 regulated the GI syndrome was independent of the intrinsic pathway of apoptosis as the GI syndrome was not affected by deletion of the pro-apoptotic genes Bak and Bax. Interestingly, we and others have observed that mice deficient in p21 are sensitized to the GI syndrome when compared to their wild-type p21 littermates (15–17). Therefore, p53 may control the GI syndrome by regulating p21.
We also studied the GI syndrome in Super p53 mice that contain one extra copy of the wild-type p53 allele, for a total of 3 copies of the p53 gene (18). The Super p53 mice express increased levels of p53 and exhibit an enhanced DNA damage response when compared to wild-type mice (18). Remarkably, the Super p53 mice were protected from the GI syndrome when compared to wild-type p53 littermates. Here we use mouse genetics to investigate the molecular mechanism for the protection of Super p53 mice from the GI syndrome. We find that deletion of p21 sensitizes Super p53 mice to the GI syndrome and that mice lacking p21 are not protected from the GI syndrome with an extra copy of p53.
MATERIALS AND METHODS
Mice
Animal procedures used in these experiments were approved by the IACUC committee at Duke University. Mice were housed in a temperature and humidity controlled room on a 12 hour light/dark cycle, and given free access to food and water. The Super p53 mouse strain p53 tg used in this experiment was kindly provided on a C57BL6 background by Manuel Serrano and described previously (18). The p21−/− mice were kindly provided by Tyler Jacks on a 129 Sv/Jae background. Experiments were carried out on compound transgenic mice of mixed C57BL6/129 SvJae backgrounds that were 6–8 weeks of age. To minimize the effect of differences in genetic background all experiments utilized age-matched, littermate controls.
Radiation Treatments
For all experiments, mice were irradiated with ionizing radiation using an X-RAD 320 Biological Irradiator (Precision X-ray Inc.). Unanesthetized mice were held in jigs and placed under lead shielding to protect the head and front limbs from radiation exposure to deliver subtotal body irradiation (SBI) as described previously (17). Mice were treated 50 cm from the source of radiation (SSD) with a dose rate of 2 Gy/min with 320 kVp X-rays, using 12.5 mA and a filter consisting of 2.5 mm Al and 0.1 mm Cu. The dose rate was measured with an ion chamber by members of the Radiation Safety Division at Duke University.
RESULTS
Super p53; p21−/− mice are sensitized to the GI syndrome
Cell cycle arrest after radiation occurs in a p53-dependent manner, which is regulated in part by induction of the cyclin-dependent kinase inhibitor p21(4). Because Super p53 mice can show increased p21 induction after radiation (18) and because deleting p21 sensitizes mice to the GI syndrome (15–17), we tested the role of p21 in mediating the GI syndrome in Super p53 mice after sub-total body irradiation (SBI). We studied the GI syndrome in Super p53 mice with an intact p21 pathway (Super p53; p21 +/−) or in littermate mice in which p21 was deleted (Super p53; p21−/−). Just as deletion of p21 sensitizes wild-type mice with two copies of p53 to the GI syndrome, (15–17) deletion of p21 also sensitized Super p53 mice to the GI syndrome after SBI (Fig 1). Similar results were obtained in two independent experiments. These results indicate that p21 mediates the GI Syndrome in Super p53 mice.
FIGURE 1.
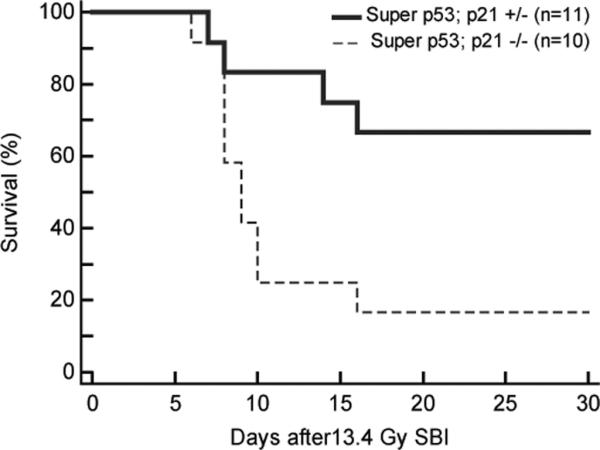
Deletion of p21 sensitizes Super p53 mice to the GI syndrome. Kaplan-Meier analysis of Super p53; p21+/− mice and Super p53; p21−/− littermates after 13.4 Gy SBI. By log-rank comparison, p<0.02.
To investigate whether p21 is necessary for an extra copy of p53 to protect mice GI syndrome, we also studied the GI syndrome in p53 WT; p21−/− mice and Super p53; p21−/− littermates after SBI. As seen in Figure 2, no protection from the GI syndrome was observed in the Super p53 mice that lacked p21 (Super p53; p21−/−). Taken together with our previously published experiments, (17) these data suggest that p21 is required for an extra copy of p53 to protect mice from the GI syndrome after SBI.
FIGURE 2.
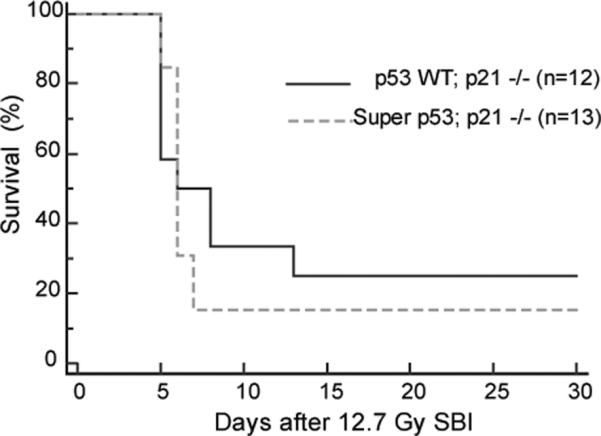
Super p53; p21−/− mice are not protected from the GI syndrome. Kaplan-Meier analysis of p53 WT; p21−/− mice and Super p53; p21−/− littermates after 12.7 Gy SBI. By log-rank comparison, p = 0.65.
DISCUSSION
We recently reported that mice with an extra copy of p53, Super p53 mice, are protected from the GI syndrome after SBI (17). In this study, we used mouse genetics to investigate the role of the cyclin-dependent kinase inhibitor p21 in mediating the GI syndrome in Super p53 mice. Similar to wild-type mice, which are sensitized to the GI syndrome by deleting p21 (15–17), we find that deleting p21 also sensitizes Super p53 mice to the GI syndrome following SBI (Fig 1). In mice that lacked p21, we did not observe that an additional copy of p53 protected mice from the GI syndrome (Fig 2).
Komorova and colleagues first reported that mice lacking p21 were sensitized to the GI syndrome (15). They also reported that mice lacking p53, which are resistant to radiation-induced apoptosis at early time points, were sensitized to the GI syndrome. Although crypt proliferation was blocked in wild-type mice after 15 Gy, in mice lacking p53, the GI epithelial cells continued to proliferate following irradiation (15). Between 72 and 96 hours these cells began to disappear, so Komorova et al. suggested these cells died via mitotic catastrophe.
More recently, Leibowitz and coworkers reported the response of the small intestine to radiation in mice lacking p53, p21, or the p53 target PUMA (16). PUMA is a BH3-only, proapoptotic member of the Bcl-2 family that is required for p53-mediated apoptosis of the GI tract (11). Remarkably, PUMA knock out mice have elevated levels of p21 and are resistant to the GI syndrome following whole body irradiation (WBI) (11). However, it was unclear whether the improved survival of PUMA null mice was due to abrogation of radiation-induced apoptosis of the GI epithelium (or perhaps other tissues such as the hematopoietic cells) or if elevated p21 also contributed to the improved survival of PUMA null mice. Liebowitz et al. compared animal survival, GI epithelial cell proliferation, and regeneration of small intestinal crypts in wild type, p53−/−, p21−/−,, PUMA−/−,, and p21−/−,; PUMA−/−, double knock out (DKO) mice. They observed decreased survival to 15 Gy WBI for p53 and p21 null mice. Although PUMA knock out mice showed increased survival following WBI, not only was this protection lost in the DKO mice lacking p21, but the DKO mice were more sensitive to the GI syndrome compared to wild-type mice (16). Therefore, elevated p21 expression may contribute to the protection of PUMA null mice from the GI syndrome. A key finding in this study was that even though p53 null, p21 null and DKO null mice had decreased survival following 15 Gy WBI, they nevertheless showed substantially increased crypt regeneration at 72 hours following WBI (16). Increased crypt regeneration in p21−/− mice after irradiation was also reported by George and colleagues (19). Taken together, these data demonstrate that crypt regeneration at 72 hours following WBI may not always be an appropriate surrogate for survival from the GI syndrome. Next, Liebowtiz and colleagues performed a series of elegant experiments to show that the GI epithelium of p21 null mice (and of p53 null mice) exposed to 15 Gy WBI undergoes aberrant cell-cycle progression with persistent DNA damage that leads to cell death via mitotic catastrophe (16). Deletion of PUMA in the DKO mice was not able to rescue this mitotic catastrophe that resulted from p21 deletion (16). We similarly found that deletion of the intrinsic pathway of apoptosis (Bak and Bax) was also not able to rescue the sensitivity to the GI syndrome caused by p53 deletion in the GI epithelium (17).
Our results in the present study of the role of p21 in the radiation-induced GI syndrome in p53 gain-of-function transgenic mice (super p53 mice) complement prior studies with wild-type p53 (15–17). Taken together, they demonstrate that p21 plays a critical role in allowing p53 to protect mice from the GI syndrome. Therefore, modulating the p53–p21 pathway may be a useful strategy to protect or mitigate the GI syndrome.
ACKNOWLEDGEMENTS
We thank Manuel Serrano for providing the Super p53 mice and Tyler Jacks for providing the p21−/− mice. We thank Greg Tudor and Cath Booth for helpful suggestions. This work was supported by RC1AI078521 to DK from the National Institute of Allergy and Infectious Diseases.
REFERENCES
- 1.Mettler FA, Voelz GL. Major Radiation Exposure - What to Expect and How to Respond. N Engl J Med. 2002;346(20):1554–61. doi: 10.1056/NEJMra000365. [DOI] [PubMed] [Google Scholar]
- 2.Zhang L, Sun W, Wang J, Zhang M, Yang S, Tian Y, et al. Mitigation Effect of an FGF-2 Peptide on Acute Gastrointestinal Syndrome After High-Dose Ionizing Radiation. Int J Radiat Oncol Biol Phys. 2010;77(1):261–8. doi: 10.1016/j.ijrobp.2009.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brugarolas J, Chandrasekaran C, Gordon JI, Beach D, Jacks T, Hannon GJ. Radiation-induced cell cycle arrest compromised by p21 deficiency. Nature. 1995;377:552–7. doi: 10.1038/377552a0. [DOI] [PubMed] [Google Scholar]
- 4.Bunz F, Dutriaux A, Lengauer C, Waldman T, Zhou S, Brown JP, et al. Requirement for p53 and p21 to sustain G2 arrest after DNA damage. Science. 1998;282(5393):1497–501. doi: 10.1126/science.282.5393.1497. [DOI] [PubMed] [Google Scholar]
- 5.Castedo M, Perfettini JL, Roumier T, Kroemer G. Cyclin-dependent kinase-1: linking apoptosis to cell cycle and mitotic catastrophe. Cell Death Differ. 2002;9:1287–93. doi: 10.1038/sj.cdd.4401130. [DOI] [PubMed] [Google Scholar]
- 6.Komarova EA, Christov K, Faerman AI, Gudkov AV. Different impact of p53 and p21 on the radiation response of mouse tissues. Oncogene. 2000;19:3791–8. doi: 10.1038/sj.onc.1203717. [DOI] [PubMed] [Google Scholar]
- 7.El-Deiry WS, Tokino T, Velculescu VE, Levy DB, Parsons R, Trent JM, et al. WAF1, a potential mediator of p53 tumor suppression. Cell. 1993;75(4):817–25. doi: 10.1016/0092-8674(93)90500-p. [DOI] [PubMed] [Google Scholar]
- 8.Efeyan A, Collado M, Velasco-Miguel S, Serrano M. Genetic dissection of the role of p21Cip1/Waf1 in p53-mediated tumour suppression. Oncogene. 2007;26(11):1645. doi: 10.1038/sj.onc.1209972. [DOI] [PubMed] [Google Scholar]
- 9.Potten CS, Wilson JW, Booth C. Regulation and Significance of Apoptosis in the Stem Cells of the Gastrointestinal Epithelium. Stem Cells. 1997;15(2):82–93. doi: 10.1002/stem.150082. [DOI] [PubMed] [Google Scholar]
- 10.Potten CS. Extreme sensitivity of some intestinal crypt cells to X and [gamma] irradiation. Nature. 1977;269(5628):518–21. doi: 10.1038/269518a0. [DOI] [PubMed] [Google Scholar]
- 11.Qiu W, Carson-Walter EB, Liu H, Epperly M, Greenberger JS, Zambetti GP, et al. PUMA Regulates Intestinal Progenitor Cell Radiosensitivity and Gastrointestinal Syndrome. Cell Stem Cell. 2008;2(6):576–83. doi: 10.1016/j.stem.2008.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merritt AJ, Potten CS, Kemp CJ, Hickman JA, Balmain A, Lane DP, et al. The role of p53 in spontaneous and radiation-induced apoptosis in the gastrointestinal tract of normal and p53-deficient mice. Cancer Res. 1994;54(3):614–7. [PubMed] [Google Scholar]
- 13.Merritt AJ, Allen TD, Potten CS, Hickman JA. Apoptosis in small intestinal epithelia from p53-null mice: evidence for a delayed, p53-independent G2/M-associated cell death after gamma-irradiation. Oncogene. 1997;14(23):2759–66. doi: 10.1038/sj.onc.1201126. [DOI] [PubMed] [Google Scholar]
- 14.Clarke A, Gledhill S, Hooper M, Bird C, Wylie A. p53 dependence of early apoptotic and proliferative responses within the mouse intestinal epithelium following gamma-irradiation. Oncogene. 1994;9(6):1767–3. [PubMed] [Google Scholar]
- 15.Komarova EA, Kondratov RV, Wang K, Christov K, Golovkina TV, Goldblum JR, et al. Dual effect of p53 on radiation sensitivity in vivo: p53 promotes hematopoietic injury, but protects from gastro-intestinal syndrome in mice. Oncogene. 2004;23(19):3265–71. doi: 10.1038/sj.onc.1207494. [DOI] [PubMed] [Google Scholar]
- 16.Leibowitz BJ, Qiu W, Liu H, Cheng T, Zhang L, Yu J. Uncoupling p53 Functions in Radiation-Induced Intestinal Damage via PUMA and p21. Molecular Cancer Research. 2011;9(5):616–25. doi: 10.1158/1541-7786.MCR-11-0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirsch DG, Santiago PM, di Tomaso E, Sullivan JM, Hou W-S, Dayton T, et al. p53 Controls Radiation-Induced Gastrointestinal Syndrome in Mice Independent of Apoptosis. Science. 2010;327(5965):593–6. doi: 10.1126/science.1166202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia-Cao I, Garcia-Cao M, Martin-Caballero J, Criado LM, Klatt P, Flores JM, et al. `Super p53' mice exhibit enhanced DNA damage response, are tumor resistant and age normally. EMBO J. 2002;21(22):6225–35. doi: 10.1093/emboj/cdf595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George RJ, Sturmoski MA, May R, Sureban SM, Dieckgraefe BK, Anant S, et al. Loss of p21Waf1/Cip1/Sdi1 enhances intestinal stem cell survival following radiation injury. American Journal of Physiology - Gastrointestinal and Liver Physiology. 2009;296(2):G245–G54. doi: 10.1152/ajpgi.00021.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]


