Abstract
Background
The familial Short QT Syndrome (SQTS) is associated with an increased risk of cardiac arrhythmia and sudden death. Gain-of-function mutations in the hERG K+ channel protein have been linked to variant 1 of the SQTS. A hERG channel pore (T618I) mutation has recently been identified in families with heritable SQTS. This study aimed to determine effects of the T618I-hERG mutation on (i) hERG current (IhERG) elicited by ventricular action potentials; (ii) the sensitivity of IhERG to inhibition by four clinically used antiarrhythmic drugs.
Methods
Electrophysiological recordings of IhERG were made at 37°C from HEK 293 cells expressing wild-type (WT) or T618I hERG. Whole-cell patch clamp recording was performed using both conventional voltage clamp and ventricular action potential (AP) clamp methods.
Results
Under conventional voltage-clamp, WT IhERG peaked at 0-+10 mV, whilst for T618I IhERG maximal current was right-ward shifted to ∼ +40 mV. Voltage-dependent activation and inactivation of T618I IhERG were positively shifted (respectively by +15 and ∼ +25 mV) compared to WT IhERG. The IhERG ‘window’ was increased for T618I compared to WT hERG. Under ventricular AP clamp, maximal repolarising WT IhERG occurred at ∼ -30 mV, whilst for T618I hERG peak IhERG occurred earlier during AP repolarisation, at ∼ +5 mV. Under conventional voltage clamp, half-maximal inhibitory concentrations (IC50) for inhibition of IhERG tails by quinidine, disopyramide, D-sotalol and flecainide for T618I hERG ranged between 1.4 and 3.2 fold that for WT hERG. Under action potential voltage clamp, T618I IC50s ranged from 1.2 to 2.0 fold the corresponding IC50 values for WT hERG.
Conclusions
The T618I mutation produces a more modest effect on repolarising IhERG than reported previously for the N588K-hERG variant 1 SQTS mutation. All drugs studied here appear substantially to retain their ability to inhibit IhERG in the setting of the SQTS-linked T618I mutation.
Introduction
The rapid delayed rectifier K+ channel current (IKr) is an important determinant of ventricular AP repolarisation and, consequently, of the duration of the QT interval on the electrocardiogram [1], [2]. Channels mediating IKr are formed by proteins encoded by hERG (human Ether-à-go-go Related Gene; alternative nomenclature KCNH2 [3], [4]). Native IKr and hERG channels exhibit sensitivity to pharmacological blockade by diverse drugs, including both Class Ia and Class III antiarrhythmic agents; excessive pharmacological inhibition of IKr/hERG leads to acquired long QT syndrome (LQTS [5]–[8]). Loss-of-function KCNH2 mutations are responsible for the LQT2 form of heritable long QT syndrome [9], [10], whilst gain-of-function mutations are responsible for the SQT1 form of heritable Short QT syndrome (SQTS [11], [12]).
The KCNH2 mutations first identified in SQTS patients led to a common asparagine to lysine (N→K) substitution within the external S5-Pore linker region of the hERG channel protein [13], [14]. hERG current (IhERG) carried by N588K-hERG mutant channels failed to rectify normally, due to a substantial (+60 to +90 mV) rightward shift in voltage-dependent inactivation [13], [15], [16]. The use in vitro of the action potential (AP) voltage clamp technique showed that the impaired inactivation of N588K hERG channels altered significantly the profile of IhERG during the plateau and repolarisation phases of ventricular APs, leading to increased IhERG occurring much earlier during the ventricular AP waveform [13], [15], [16]. Additionally, SQT1 patients with the N588K mutation were found to be refractory to treatment with Class III antiarrhythmic drugs (sotalol, ibutilide), but did respond to the Class Ia agents quinidine and disopyramide [13], [17]–[19]. This differential influence of the N588K mutation on clinical effectiveness of Class Ia and III drugs correlates with changes in IhERG blocking potency seen in vitro [13], [18], [20] and is explicable on the basis of the comparatively greater dependence of Class III than Class Ia drugs on IhERG inactivation in order to bind to the channel [21]. A second gain-of-function hERG mutation, identified in the S5 domain of zebrafish ERG (zERG; L499P; hERG homologue L532P) in reggae mutant zebrafish with accelerated cardiac repolarisation [22], has been found to produce marked kinetic alterations including to voltage and time-dependent inactivation [22], [23]. The L532P hERG homologue also exhibits altered sensitivity to Class III drug block [23].
Recently, a novel SQT1 mutant has been identified in a Chinese family with a history of nocturnal sudden death [24]. Four of eleven family members evaluated exhibited shortened rate-corrected QT intervals (with a mean QTc interval of 316 ms) [24]. Genotyping of the proband identified a base transition (C1853T) that led to a threonine to isoleucine substitution at position 618 (located in the hERG channel pore helix) of hERG; this was absent in 200 ethnically matched controls [24]. In vitro biophysical analysis identified significant alterations to IhERG kinetics, including a ∼+50 mV shift in voltage dependent inactivation [24]. Pharmacological experiments with single high concentrations of quinidine or sotalol (producing 70% or greater inhibition of wild-type (WT) IhERG) were suggestive of retained IhERG block of T618I hERG during applied voltage commands [24]. At present, however, concentration-response data for pharmacological inhibition of T618I hERG appear to be lacking for any drug. Moreover, the effect of the T618I mutation on the profile of IhERG during dynamic physiological waveforms (ventricular APs) has not yet been reported. The present study was conducted to address both of these issues, through experiments on recombinant WT and T618I channel IhERG conducted at human physiological temperature.
Materials and Methods
Wild-type and T618I hERG
Human Embryonic Kidney (HEK-293) cells stably expressing WT hERG were donated by Prof Craig January [25]. HEK 293 cells used for transient transfection were obtained from ECCAC (catalog number 85120602). The T618I mutant was constructed using QuikChange® (Stratagene) mutagenesis. The following forward primer sequence was used: 5′CGG CGC TCT ACT TCA TCT TCA GCA GCC TCAC3′. DNA was sequenced for the full length of the hERG insert to ensure that only the correct mutation had been made (Eurofins MWG Operon).
Maintenance of Cells and Cell Transfection
Experiments employed HEK-293 cells stably or transiently expressing WT or T618I hERG constructs. Cells were passaged and maintained as described previously [23], [26]. For transient transfection experiments, 24 hours after plating cells out they were transiently transfected with 0.3 µg of T618I hERG construct using Lipofectamine™ LTX (Invitrogen) according to the manufacturer’s instructions. Expression plasmid encoding CD8 was also added as a transfection marker [26]. Cells were plated onto small sterilised collagen-coated glass coverslips 6 hours after transfection and recordings were made after at least 24 hours incubation at 37°C. Successfully transfected cells were identified using Dynabeads® (Invitrogen).
Electrophysiology
Once in the recording chamber, cells were superfused at 37°C with an external solution containing (in mM): 140 NaCl, 4 KCl, 2.5 CaCl2, 1 MgCl2, 10 Glucose and 5 HEPES (titrated to pH 7.45 with NaOH). Patch-pipettes (Corning 7052 glass, AM Systems) were pulled and heat-polished (Narishige MF83) to 2.5–4 MΩ; pipette dialysate contained (in mM): 130 KCl, 1 MgCl2, 5 EGTA, 5 MgATP, 10 HEPES (titrated to pH 7.2 using KOH) [26]; [27]. hERG current (IhERG) recordings were made using an Axopatch 200, 200A or 200B amplifier (Axon Instruments, now Molecular Devices) and a CV201, CV202A or CV203BU head-stage. Between 70–80% of pipette series resistance was compensated. Voltage-clamp commands were generated and data recorded using ‘WinWCP’ (John Dempster, Strathclyde University) or pClamp 9.0 and 10.0 (Molecular Devices). The ventricular action potential (AP) command used for AP clamp experiments was identical to that used in other recent studies from our laboratory [23], [27].
Drugs
Disopyramide-phosphate powder (Sigma-Aldrich) was dissolved in Milli-Q water to produce an initial stock solution of 400 mM which was diluted further to produce stock solutions ranging down to 1 mM. Quinidine gluconate salt (Sigma-Aldrich) was dissolved in MilliQ water to produce an initial stock solution of 100 mM, which was diluted further to produce stock solutions ranging down to 30 µM. Flecainide acetate salt (Sigma-Aldrich) was dissolved in MilliQ water to produce an initial stock solution of 10 mM, which was diluted further to produce stock solutions ranging down to 1 mM. D-sotalol (Sequoia) was dissolved in DMSO to produce an initial stock solution of 100 mM, with further dilution of stocks to solutions ranging down to 10 µM. Disopyramide and quinidine containing stock solutions were diluted at least 1∶1000-fold with Tyrode’s solution to achieve the final concentrations stated in the Results text. For D-sotalol, dilutions of 1∶1000 fold were achievable for all final concentrations except 500 µM, for which a dilution of only 5∶1000 fold was possible. During recordings all external solutions were applied using a home-built, warmed and rapid solution exchange device [28].
Data Analysis
Concentration-response data were fitted by a standard Hill equation in order to obtain half-maximal inhibitory concentration (IC50) and Hill-coefficient (nH) values (±95% confidence intervals (C.I.)). Mean data are otherwise presented as mean ± SEM. The voltage dependence of IhERG activation was determined by fitting the values of IhERG tail currents (normalised to peak IhERG tail value and plotted against voltage) with a Boltzmann equation of the form:
| (1) |
where I is the IhERG tail amplitude following test potential Vm, IMax is the maximal IhERG tail observed during the protocol, V0.5 is the potential at which IhERG was half-maximally activated, and k is the slope factor for the relationship.
The voltage dependence of IhERG inactivation (assessed by studying availability) was determined by fitting normalised peak IhERG currents elicited by the third step of a three-step protocol (Figure 3A) by the equation:
| (2) |
where I = transient current elicited by the third step of the protocol, following a brief (2 ms) conditioning step (Vm) to relieve inactivation induced by the first step; IMax is the maximal transient current observed during the protocol and V0.5 and k denote, respectively, half-maximal inactivation voltage and slope factor for the fit to the plotted relation.
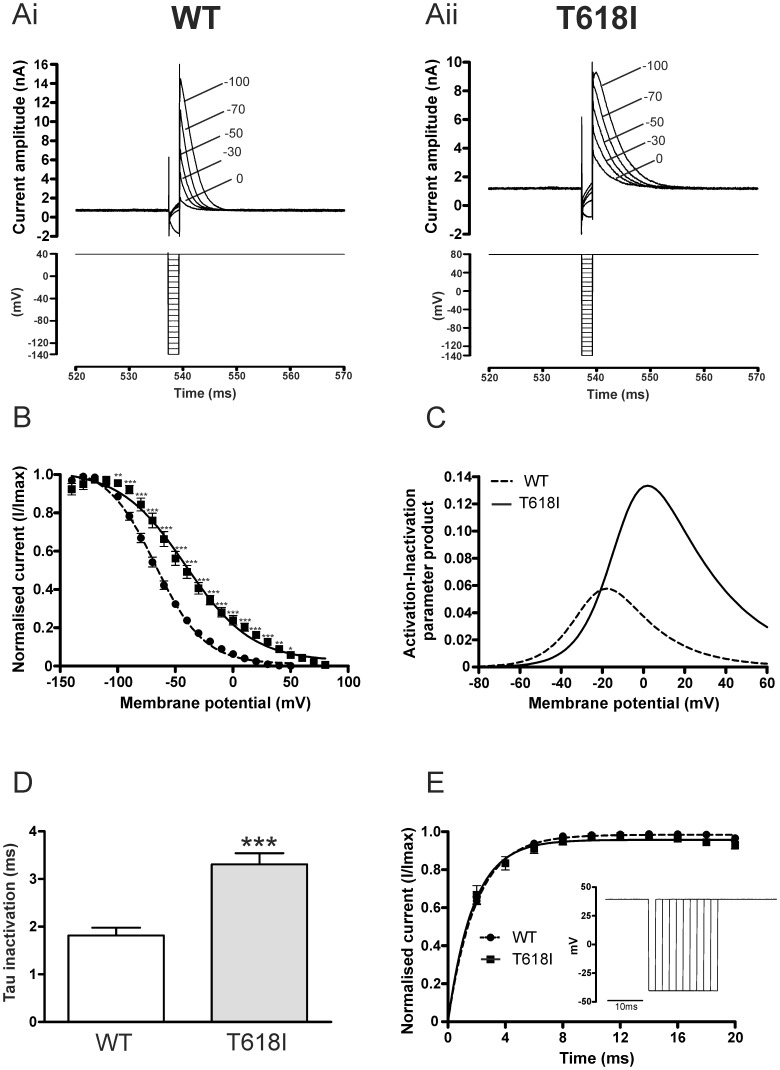
Figure 3. Voltage dependence of WT and T618I IhERG inactivation.
(Ai, Aii) Upper traces show representative current records for WT IhERG (Ai) and T618I IhERG (Aii) elicited by voltage protocols shown in lower panels (see also ‘Results’ text). A more positive voltage (+80 mV) was used for the first and third steps for T618I hERG than for WT hERG (+40 mV) to ensure that complete inactivation occurred on membrane potential depolarisation. Note that for clarity of display only selected traces elicited by the protocol are shown. Numbers in Ai and Aii indicate command voltage at which currents recorded. (B) Plots against voltage (during the second step of the protocol) of IhERG availability. Peak current values and availability plots were constructed as described previously [16], employing deactivation correction as per [31]. A Boltzmann equation fit to the data gave a V0.5 for inactivation of −67.2 mV (k = 21.0 mV) for WT and a V0.5 of −44.3 mV (k = 29.8) for T618I (n = 11 and 6 cells respectively). (C) ‘Window current’ for WT and T618I hERG. Derived activation and inactivation V0.5 and k values from Figures 1D and 3B were used with equations 1 and 2 to calculate activation and inactivation variables at 2 mV intervals between −80 and +60 mV. Window IhERG was calculated as the activation-inactivation variable product at each voltage. (D) Bar charts comparing time constant of WT (n = 11) and T618I (n = 6) IhERG inactivation, following brief hyperpolarisation to −140 mV. Inactivating currents were fitted with a standard mono-exponential function (E) Recovery from inactivation time-course for WT and T618I hERG (protocol shown as inset). The dashed gray line denotes mono-exponential fit to WT data (n = 7). The solid line denotes mono-exponential fit to T618I data, with the dotted line connecting these data at successive time points (n = 9). Asterisks in B and C denote statistical significance: *p<0.05; **p<0.01; ***p<0.001.
Statistical analysis (SigmaPlot 12) utilised, as appropriate, an unpaired t-test, a Welch’s t-test not assuming equal variances, or a two way repeated measures ANOVA test. P values of less than 0.05 were taken as statistically significant.
Results
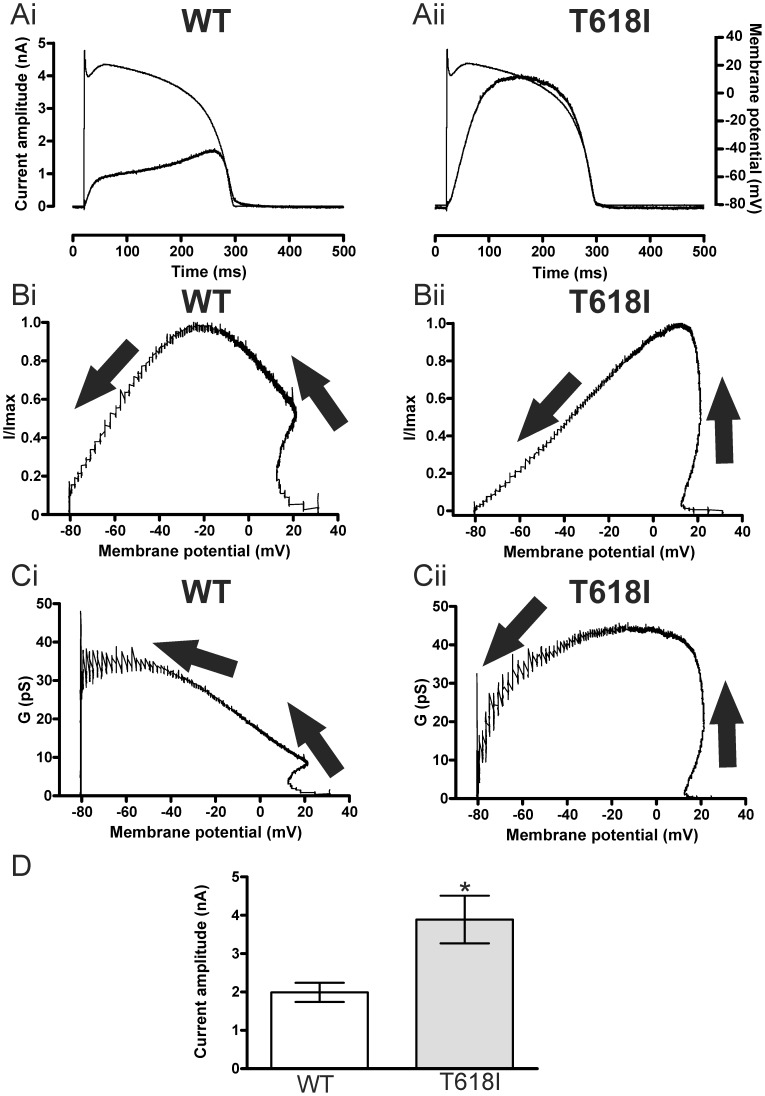
Effects of the T618I hERG Mutation on the Voltage-dependence of IhERG and its Activation
Figures 1Ai and Aii show representative current traces for WT and T618I IhERG elicited by the voltage protocol shown in the lower panels (Figures 1Bi and Bii). WT IhERG increased progressively with the magnitude of the applied voltage commands up to ∼0/+10 mV, positive to which the current during the applied command declined in amplitude. Prominent IhERG tails were observed on repolarisation to −40 mV after each voltage command, with tail current amplitude exceeding that of the preceding current during the depolarising step, particularly for positive command voltages. These features are typical of WT IhERG [3], [4], [25], [29]. The traces shown in Figure 1Aii indicate that at potentials negative to 0 mV, T618I IhERG resembled WT IhERG. However, at test potentials between ∼ 0 and +40 mV (over which WT IhERG elicited by depolarising commands became reduced in amplitude), T618I IhERG continued to increase in magnitude. T618I IhERG began to decline in amplitude at test potentials positive to +40 mV. Notably, with positive test commands, T618I IhERG did not exhibit tail currents (Itails) that exceeded pulse current in amplitude (cf [24]). Figure 1C shows mean end-pulse current voltage (I–V) relations for WT and T618I IhERG, demonstrating maximal current for WT IhERG at ∼+10 mV and an area of negative slope in the I–V relation at more positive potentials. For T618I hERG, rectification of the I–V relation was positively voltage-shifted, with the area of negative slope in the I–V relation occurring positive to +40 mV. Figure 1D shows mean normalised I–V relations for WT and T618I hERG Itails, fitted with equation 1 (Methods). For WT IhERG the mean activation V0.5 was −23.1±1.5 mV (n = 6), whilst for T618I IhERG this was −8.0±3.4 mV (n = 7; p<0.01 versus WT). The corresponding k values were 7.8±1.5 and 8.5±0.9 mV respectively (p>0.05).
Figure 1. Basic characteristics of T618I IhERG.
(A,B) Upper traces (A) show representative current records for WT IhERG (Ai) and T618I IhERG (Aii) elicited by voltage protocols shown in B (Bi – WT and Bii - T618I; note that for WT IhERG measurements, successive voltage steps increased by 10 mV increments up to +60 mV, whilst for T618I IhERG successive steps increased by 20 mV up to +100 mV). Note that for clarity of display only selected traces elicited by the protocol are shown. Numbers in Ai and Aii indicate command voltage at which currents recorded. Note different current scales in Ai and Aii. (C) Current voltage (I–V) relations for WT (n = 6) and T618I (n = 5) IhERG elicited by the voltage protocol shown in panel B. Data are shown for end pulse I–V relations, in which currents for each cell studied were normalized to the current value at 0 mV. (D) I–V relations for WT (n = 6) and T618I (n = 7) tail current recorded at −40 mV following repolarisation from the test potentials plotted on the membrane potential axis (for these measurements IhERG tails were measured following depolarising steps to potentials between −40 and +60 mV (in 10 mV increments)). Tail currents were measured relative to the instantaneous current elicited by the brief (50 ms) step from −80 to −40 mV prior to the applied voltage commands. Data were fitted by equation 1, to give the V0.5 and k values in the Results text. Asterisks in C and D denote statistical significance: *p<0.05; **p<0.01 ***p<0.001.
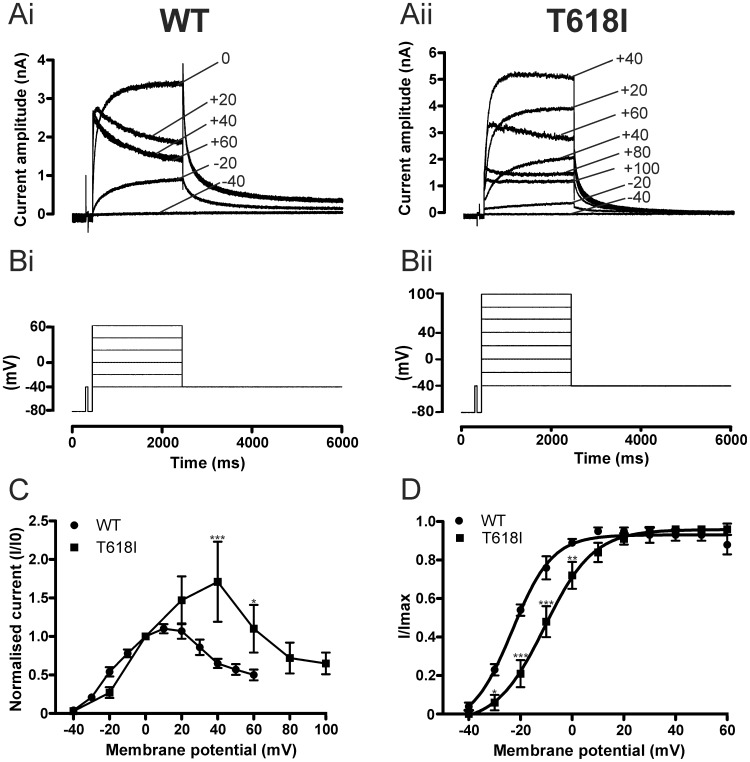
Effects of the T618I Mutation on IhERG Activation and Deactivation Time-course
In order to investigate effects of the T618I mutation on the time-course of IhERG activation, we used an “envelope of tails protocol” in which Itails were measured at −40 mV following activating commands of different durations from −80 to 0 mV (see inset to Fig. 2A). Itails elicited by commands of different duration were normalised to the maximum current during the protocol and plotted as a function of command pulse duration, as shown in Figure 2A (cf [23], [30]). Mono-exponential fits to the data yielded a τactivation of 104.1±8.3 ms for WT IhERG and of 112.0±13.0 ms for T618I IhERG (n = 5 and 6 cells respectively; p>0.5), indicating that activation time-course was similar for WT and T618I IhERG during this protocol. In order to compare IhERG deactivation time-course between WT and T618I hERG, Itails elicited at −40 mV following voltage commands to +20 mV were fitted with a standard bi-exponential function. Figures 2Bi and Bii show respectively the mean fast and slow time-constants of deactivation (τf ‘fast tau’ and τs ‘slow tau’, respectively) for WT and T618I IhERG. Both fast and slow phases of deactivation were faster for T618I than WT IhERG (evidenced by smaller tau values plotted in Figure 2B; p<0.05 and p<0.01 respectively for τf and τs versus WT). However, the relative proportion of fast and slow deactivation did not differ between WT and T618I IhERG (quantified in Figure 2C as proportion of total deactivating current described by τf).
Figure 2. WT and T618I IhERG time-course of activation and deactivation.
(A) Plots of time-course of IhERG activation obtained using an “envelope-of-tails” protocol– see inset and ‘Results’ text. For each cell, the peak current amplitudes at each time-point were normalized to the maximal current observed during the protocol. (Bi, Bii) Bar charts comparing τf (Bi) and τs (Bii) values for deactivation of WT (n = 11) and T618I (n = 11) hERG tail currents on repolarisation to -40 mV following a 2 s depolarisation from −80 mV to +20 mV. Currents were fitted with a standard bi-exponential equation (C) Bar-chart showing the proportion of fast deactivation on repolarisation to −40 mV for WT and T618I IhERG (n = 11 cells for each condition). Asterisks in Bi and Bii denote statistical significance: *p<0.05; **p<0.01.
Effects of the T618I hERG Mutation on IhERG Inactivation
In order to characterize the effect of the T618I mutation on the voltage-dependence of IhERG inactivation, voltage dependent availability of IhERG was determined for WT- and T618I-hERG by applying voltage protocols used in prior investigations from our laboratory to study effects on inactivation of gain-of-function hERG mutations [16], [23]. These were comprised of an initial (500 ms) depolarizing step to activate and then fully inactivate IhERG, followed by brief (2 ms) repolarizing steps to a range of potentials to relieve inactivation to varying extents, followed by a third depolarization step that elicited a rapidly inactivating IhERG. The magnitude of peak current elicited by the third step reflected the extent of availability induced by the (second) repolarizing step. Similar to prior studies of gain-of-function hERG mutations performed in our laboratory [16], [23], in order to ensure complete inactivation of IhERG during the initial step of the voltage protocol, for T618I IhERG a depolarizing step to +80 mV was used, compared to +40 mV for WT IhERG. The lower panels of Figures 3Ai and Aii show the portion of the protocol that incorporated the repolarizing step and subsequent depolarization phases, with the upper panels showing corresponding IhERG records. Peak current amplitudes were obtained by fitting the declining phase of the transient IhERG records with a mono-exponential function and extrapolation to the beginning of the third pulse [16], [23]. The resulting values were normalized to the maximal current seen during the protocol and were plotted against repolarization step voltage. The availability/inactivation V0.5 value for WT IhERG derived from a fit to the data with equation 2 was −65.5±2.2 mV with a k value of 19.8±0.6 (n = 11 cells). For T618I IhERG, the corresponding values were: V0.5 of −40.7±5.1 mV and k of 26.9±1.9 mV (n = 6 cells; and, respectively, p<0.01 and 0.001 versus control). For the sake of completeness, the data were further analysed by correction for deactivation using the method of Smith et al. [31] then plotted against voltage and fitted with equation 2 (Figure 3B), which gave V0.5 values of –67.2±2.0 and −44.3±5.1 mV respectively for WT and T618I IhERG (p<0.01) and respective k values of 21.0±0.6 and 29.8±1.7 mV (P<0.001). Thus, IhERG inactivation V0.5 was positively shifted by ∼+23 to +25 mV for T618I IhERG compared to WT IhERG, with an accompanying 7 to 9 mV increase in k value. In order to establish the overall effects of altered steady-state voltage-dependent kinetics of the T618I mutation, we calculated ‘window current’ for WT and T618I hERG, as the activation-inactivation variable product across a range of voltages between −80 and +60 mV. Figure 3C shows that the IhERG window was both positively shifted and significantly larger for T618I than WT IhERG.
The time-course of development of inactivation for WT and T618I IhERG was compared by mono-exponential fitting of the decline of transient currents elicited following the repolarizing step to −140 mV. This yielded τ-values for WT and T618I IhERG inactivation of 1.86±0.17 ms and 3.32±0.28 ms respectively (Figure 3D; n = 11 and 6 respectively; p<0.01). To compare the rate of recovery from inactivation between the two channels, we used a protocol used in prior IhERG studies ([23], [30] see also inset of Figure 3E): a 500-ms depolarisation to +40 mV was applied from a holding potential of −80 mV to activate and inactivate IhERG. Membrane potential was then repolarised to −40 mV for an increasing periods of time (between 2 and 20 ms) to induce recovery from inactivation. Transient currents were then subsequently elicited by a 100-ms depolarisation to +40 mV. Figure 3E shows plots of WT and T618I peak outward transient current magnitude against the duration of the repolarization step (with currents normalized to maximal current seen during the protocol). Fits to the data with a mono-exponential function gave τ values of 1.99±0.12 ms for WT (n = 7) and of 1.93±0.30 ms for T618I (n = 9) (p>0.05).
Collectively, the results from these experiments indicate that the T618I mutation induced a positive shift in the voltage-dependence of IhERG inactivation, augmented the IhERG ‘window’, slowed the time-course of development of IhERG inactivation, but did not alter significantly the rate of recovery of IhERG from inactivation.
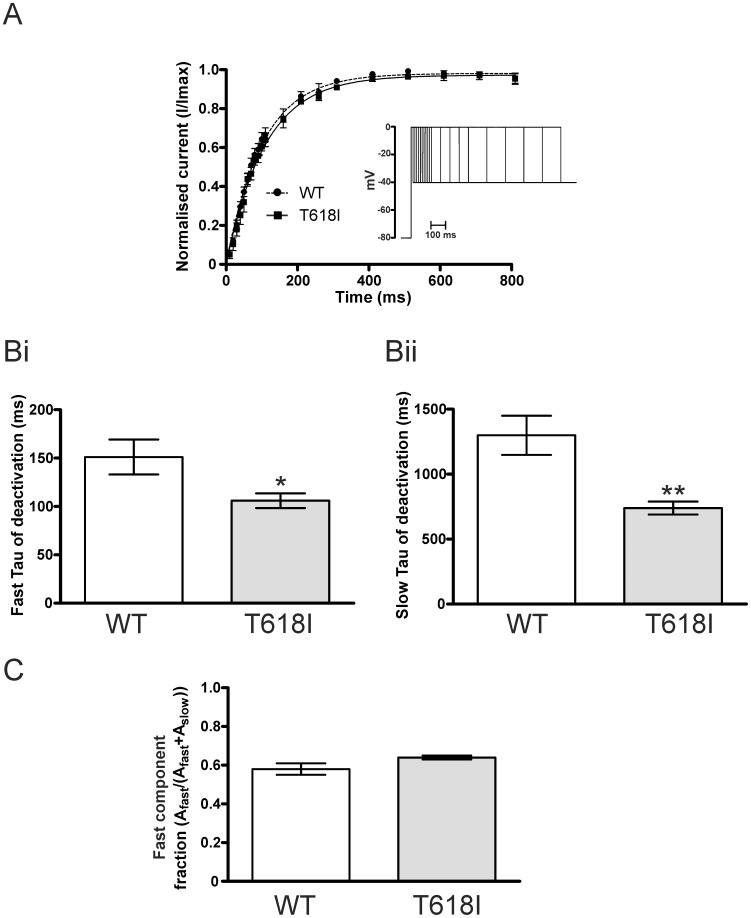
Effects of the T618I Mutation on IhERG under Action Potential Voltage Clamp
Figure 4Ai shows a representative record of WT IhERG elicited by a ventricular AP command (superimposed on the current trace in Figure 4Ai). As reported previously (e.g. [25], [30], [32]), the elicited current was comparatively small immediately on AP depolarisation, then increased progressively during the plateau phase of the AP, before declining during terminal repolarisation. Figure 4Aii shows similar recordings for T618I IhERG. The profile of current during the AP command differed from that for WT IhERG: current increased earlier during the AP command, peaking earlier during the AP plateau and then it declined during the latter part of the plateau phase. Figures 4Bi and Bii show representative normalized instantaneous current-voltage (I–V) relations for IhERG during the repolarising phase of the AP command. Peak outward current was positively shifted by ∼ +35 mV for T618I IhERG (from −30.7±1.2 mV for WT, to +5.1±2.1 mV for T618I hERG; P<0.001 versus WT). Example instantaneous conductance-voltage (G-V) relations (cf [16], [32], [33]) for WT- and T618I-hERG are shown in Figures 4Ci and Cii, respectively. As described previously [16], [32], [33], the macroscopic conductance of WT-hERG increased throughout the AP repolarisation phase, being maximal late in repolarisation (Figure 4Ci). In contrast, for T618I IhERG conductance increased steeply early in repolarisation (between ∼+20 and −20 mV) and then progressively declined as the membrane potential followed the direction of membrane repolarisation. Figure 4D shows mean data for the maximal amplitudes of WT and T618I IhERG during the applied ventricular AP command waveform, demonstrating a significantly greater (∼2-fold) maximal repolarising current when hERG channels incorporated the T618I hERG mutation. Considered collectively, the findings from our AP clamp experiments indicate that greater repolarising IhERG/IKr would be expected to occur earlier during ventricular APs in the setting of T618I-linked SQT1.
Figure 4. Action potential (AP) voltage clamp of WT and T618I IhERG.
(A) IhERG (after p/4 subtraction) elicited by ventricular AP command for WT (Ai) and T618I (Aii) IhERG. Currents are shown overlaid with the voltage protocol. (B) Instantaneous I–V relations for IhERG elicited in A for WT (Bi) and T618I (Bii) IhERG. Current during the repolarising phase of the AP are plotted. Arrows denote direction of repolarisation. (C) Instantaneous conductance-voltage (G–V) relations for IhERG elicited in A for WT (Ci) and T618I (Cii) IhERG during AP repolarisation, Arrows denote direction of repolarisation. (D) Magnitude of peak repolarising current during AP voltage clamp, plotted for WT (n = 14) and T618I (n = 19) IhERG. * denotes statistically significant difference from WT at p<0.05.
Pharmacology of the T618I hERG Mutation
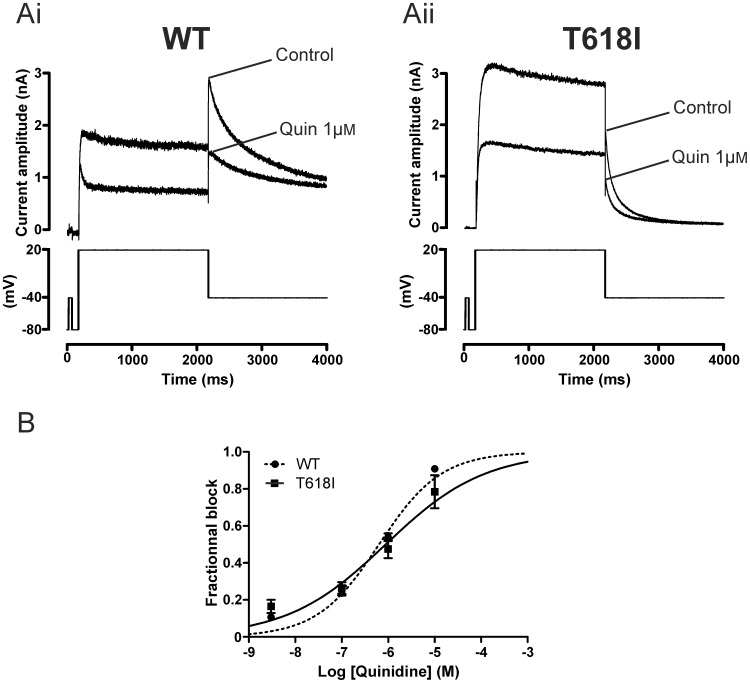
Figure 5A compares the response of WT and T618I IhERG to 1 µM of the Class Ia antiarrhythmic drug quinidine, using conventional voltage-clamp. Figures 5Ai and Aii show representative IhERG traces elicited by the voltage protocol shown in the lower panels (a standard depolarising step protocol used in previous studies of IhERG pharmacology from our laboratory (e.g. [23], [26], [34]). Tail current magnitude was measured relative to instantaneous current at −40 mV elicited by the brief (50 ms) depolarising step that preceded the voltage command to +20 mV in the absence and presence of the drug. 1 µM quinidine reduced WT IhERG markedly, with 53.9±2.1% (n = 13) inhibition of the IhERG tail evident (compatible with prior reports of a submicromolar IC50 under similar recording conditions [20], [35]). For T618I IhERG the reduction in current was similar to that seen for the WT current, with 1 µM quinidine reducing T618I tail current magnitude by 47.6±5.0% (n = 8; NS versus WT). A range of quinidine concentrations between 10 nM and 10 µM were tested and concentration response relations constructed as shown in Figure 5B. The derived IC50 for WT IhERG was 0.64 µM (for C.I. and nH values see Table 1) whilst for T618I IhERG the comparable value was 0.88 µM. Thus, the IC50 for IhERG tail block by quinidine for T618I IhERG was ∼ 1.4-fold that for WT IhERG (see also Table 1).
Figure 5. Effect of quinidine on WT and T618I IhERG under conventional voltage clamp.
(A) Upper traces show IhERG elicited by voltage protocol shown in the lower panel (applied continuously once every 12 s) in control solution and after exposure to 1 µM quinidine (Quin). Ai shows data for WT IhERG, whilst Aii shows data for T618I IhERG. (B) Concentration response relations for inhibition of WT and T618I IhERG by quinidine. Fractional inhibition of IhERG was assessed for IhERG tails at each of 4 concentrations (n = at least 5 cells per drug concentration). Steady-state effects were achieved within ∼2 minutes of drug application and measurements were made at ∼3 minutes.
Table 1. Pharmacology of the T618I hERG mutant studied with conventional voltage clamp.
| Drug | WT IhERG IC50 (µM) | WT IhERG nH | T618I IhERG IC50(µM) | T618I IhERG nH | Fold IC50 |
| Quinidine | 0.64 (C.I 0.51–0.79) | 0.65 (C.I 0.55–0.75) | 0.88 (C.I 0.41–1.88) | 0.41 (C.I 0.25–0.57) | 1.4 (0.8–2.4) |
| Disopyramide | 7.68 (C.I 6.32–9.34) | 0.87 (C.I 0.66–1.07) | 16.83 (C.I 8.56–33.09) | 0.47 (C.I 0.30–0.64) | 2.2 (1.4–3.5) |
| D-Sotalol | 112.2 (C.I 91.7–137.3) | 0.74 (C.I 0.57–0.91) | 356.6 (C.I 305.6–416.1) | 0.85 (C.I 0.70–1.00) | 3.2 (3.0–3.3) |
| Flecainide | 1.87 (C.I 1.56–2.25) | 0.81 (C.I 0.68–0.94) | 4.67 (C.I 3.06–7.13) | 0.58 (C.I 0.45–0.71) | 2.5 (2.0–3.2) |
IC50 and nH values shown are derived from fits to concentration-response relations in Figures 5 and 6, obtained from fractional inhibition of IhERG using a voltage step protocol (shown in Figures 5A and 6A). Columns show mean values and 95% confidence intervals (C.I). The right-hand column expresses the ratio of the T618I IC50 to the WT IC50 value, to one decimal place. The numbers in parentheses in the right hand column represent the range of ratio values for the ± C.Is for derived T618/WT IC50s.
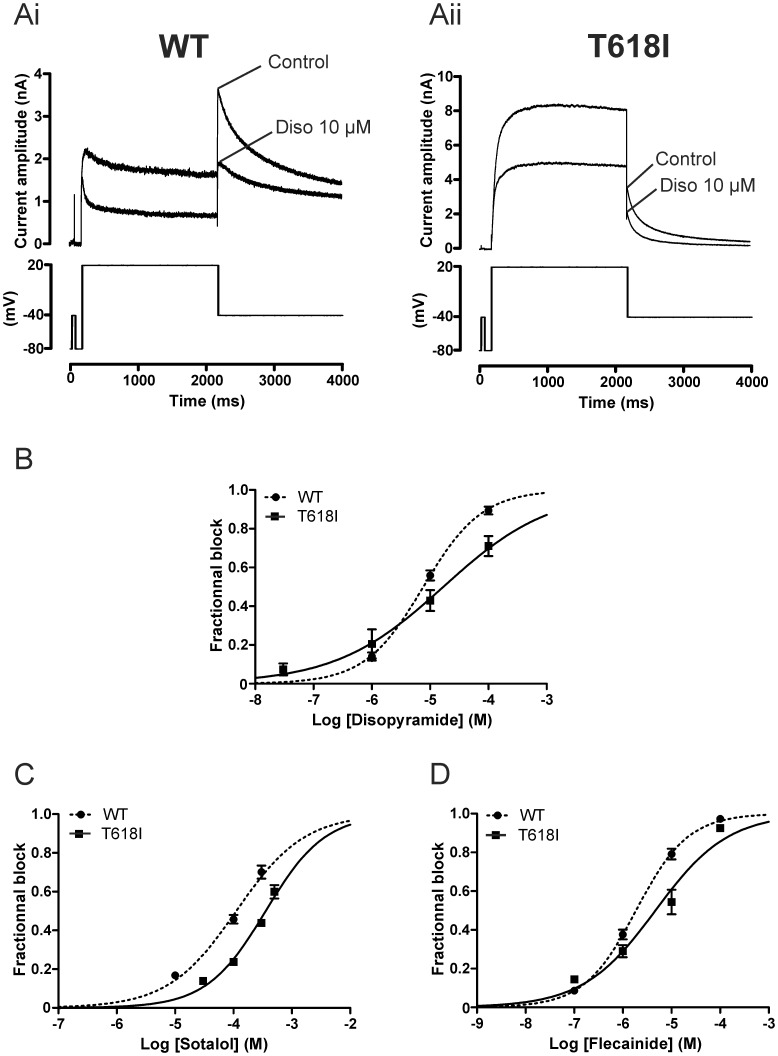
The Class Ia antiarrhythmic drug disopyramide has been found to be effective against the N588K IhERG SQT1 mutation [20], [21], but its effects on T618I hERG are unknown. Therefore we tested the effects of disopyramide on the T618I hERG mutant (Figure 6). Figures 6Ai and Aii show representative IhERG traces in the absence and presence of the drug, with the protocol shown in lower panels. As expected from previous studies [20], [26], [36], 10 µM disopyramide reduced WT IhERG by 55.9±2.6% (n = 13) whereas it reduced T618I IhERG by 42.9±5.4% (n = 5,p<0.05 versus WT). Three other disopyramide concentrations were tested on T618I mutant channels and concentration response relations constructed as shown in Figure 6B. For T618I IhERG the disopyramide IC50 was 16.83 µM whilst for WT IhERG inhibition the corresponding value was 7.68 µM. Thus, the IC50 for T618 IhERG tail inhibition by disopyramide was ∼2.2 fold that for the WT channel.
Figure 6. Effect of disopyramide, D-sotalol and flecainide on WT and T618I IhERG under conventional voltage clamp.
(A) Upper traces show IhERG elicited by voltage protocol shown in the lower panel in control solution and after exposure to 10 µM disopyramide (Diso). Ai shows data for WT IhERG, whilst Aii shows data for T618I IhERG. Note different current scales in Ai and Aii. (B) Concentration response relations for inhibition of WT and T618I IhERG by disopyramide. Fractional inhibition of IhERG was assessed for IhERG tails at each of 3 concentrations for WT IhERG (n = 5 cells at 1 µM; 13 at 10 µM and 5 at 100 µM; incorporating data from [26], with additional data from a further 8 experiments for 10 µM disopyramide) and 4 for T618I IhERG (n = 4 to 5 cells per concentration). (C) Concentration response relations for inhibition of WT and T618I IhERG by D-sotalol. Fractional inhibition of IhERG was assessed for IhERG tails at each of 3 sotalol concentrations for WT IhERG (n = 5 to 9 cells at each concentration) and 4 for T618I IhERG (n = 5 to 6 cells per concentration). (D) Concentration response relations for inhibition of WT and T618I IhERG by flecainide. Fractional inhibition of IhERG was assessed for IhERG tails at each of 4 flecainide concentrations for WT IhERG (n = 5 to 12 cells per concentration) and T618I IhERG (n = 5 to 6 cells per concentration).
Similar experiments were also conducted with the Class III antiarrhythmic drug D-sotalol and the Class Ic antiarrhythmic drug flecainide. Figures 6C and 6D show the concentration-response relations for inhibition of WT and T618I IhERG by these drugs. For D-sotalol (Figure 6C) the derived IC50 for WT IhERG was 112.2 µM whilst for T618I IhERG the comparable value was 356.6 µM (∼3.2-fold that for WT IhERG). For flecainide, the derived IC50 for WT IhERG was 1.87 µM whilst that for T618I IhERG was 4.67 µM (∼ 2.5-fold that for WT IhERG). Results obtained under conventional voltage clamp for all four drugs are summarized in Table 1.
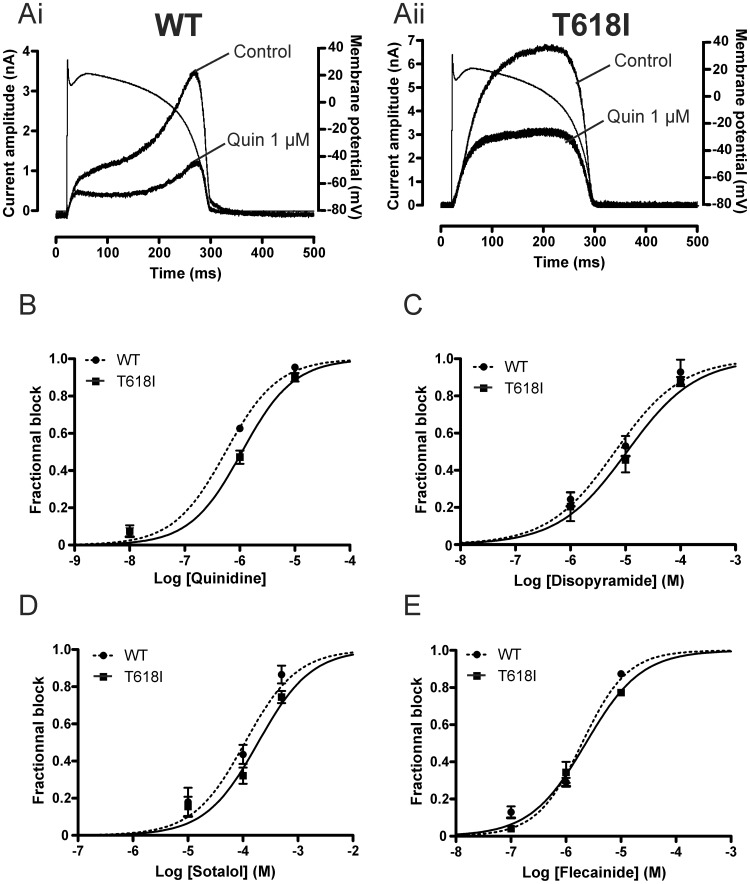
The limited data currently available on T618I hERG pharmacology appear to suggest some difference in the effect of the mutation on inhibition of pulse and tail currents by 1 µM quinidine and 500 µM sotalol, during conventional voltage clamp [24]. Ventricular APs involve dynamic changes in membrane potential that influence the profile of observed current; therefore we conducted additional experiments in which concentration-response relations for the 4 drugs examined under conventional voltage clamp were also determined from ventricular AP clamp experiments. For these, the percentage of inhibition of peak IhERG during the AP waveform for three different drug concentrations was calculated for each drug. Concentration-response relations were then constructed as shown in Figure 7. Figures 7Ai and Aii show representative current traces for WT and T618I IhERG in the presence and absence of quinidine; the ventricular AP command is superimposed over each set of traces. In this example, 1 µM quinidine reduced maximal IhERG during repolarisation by 67% for WT IhERG and 56% for T618I IhERG. Figures 7B–E show concentration-response curves for inhibition of maximal IhERG during repolarisation by quinidine, disopyramide, sotalol and flecainide (Figures 7B–E respectively), whilst Table 2 summarises numerical data for IC50 and nH values. The derived IC50 values for WT and T618I IhERG inhibition by quinidine (Figures 7A,B) were, respectively, 0.55 µM and 1.09 µM (∼2.0 fold the WT value). For disopyramide (Figure 7C), the WT IhERG IC50 was 6.47 µM and that for T618I IhERG was 10.65 µM (1.6-fold the WT value). For D-sotalol (Figure 7D) the IC50 for WT IhERG was 109.5 µM, whilst that for T618I IhERG was 189.2 µM (∼1.7-fold that for WT IhERG). Finally, we found flecainide (Figure 7E) to inhibit WT and T618I IhERG with an IC50 of 1.96 µM and of 2.29 µM (1.2 fold the WT value) respectively. Thus, under AP clamp all four drugs exhibited comparatively modest attenuation of their inhibitory action with the T618I mutation.
Figure 7. Pharmacology of WT and T618 IhERG under AP voltage clamp.
(A) Shows representative traces (after p/4 subtraction) of WT (Ai) and T618I (Aii) IhERG elicited by AP voltage clamp protocol (overlain) in control solution and after exposure to 1 µM quinidine. Note different current scales in Ai and Aii. AP commands were applied at 1 Hz. (B–D) Concentration response relations for inhibition of WT and T618I peak repolarising current observed during AP clamp by quinidine (B; 3 concentrations tested, n = 4 to 5 cells per concentration); disopyramide (C; 3 concentrations tested, n = 4 to 5 cells per concentration); D-sotalol (D; 3 concentrations tested, n = 4 to 5 cells per concentration); flecainide (E; 3 concentrations tested, n = 4 to 5 cells per concentration).
Table 2. Pharmacology of the T618I hERG mutant studied with action potential voltage clamp.
| Drug | WT IhERG IC50 (µM) | WT IhERG nH | T618I IhERG IC50(µM) | T618I IhERG nH | Fold IC50 |
| Quinidine | 0.55 (C.I 0.43–0.71) | 0.91 (C.I 0.65–1.18) | 1.09 (C.I 0.82–1.46) | 0.92 (C.I 0.59–1.26) | 2.0 (1.9–2.1) |
| Disopyramide | 6.47 (C.I 3.76–11.12) | 0.71 (C.I 0.40–0.99) | 10.65 (C.I 5.73–19.80) | 0.69 (C.I 0.35–1.05) | 1.6 (1.5–1.8) |
| D-Sotalol | 109.5 (C.I 70.7–169.6) | 0.92 (C.I 0.47–1.37) | 189.2 (C.I 133.3–268.6) | 0.90 (C.I 0.56–1.25) | 1.7 (1.6–1.9) |
| Flecainide | 1.96 (C.I 1.49–2.59) | 1.05 (C.I 0.79–1.30) | 2.29 (C.I 1.72–3.05) | 0.86 (C.I 0.67–1.05) | 1.2 (1.1–1.2) |
IC50 and nH values shown are derived from fits to concentration-response relations in Figure 7, obtained from fractional inhibition of IhERG using a voltage step protocol (shown in Figure 7A). Columns show mean values and 95% confidence intervals (C.I). The right-hand column expresses the ratio of the T618I IC50 to the WT IC50 value, to one decimal place. The numbers in parentheses in the right hand column represent the range of ratio values for the ± C.Is for derived T618/WT IC50s.
Discussion
To our knowledge, the present study is the first to have established the effects of the T618I hERG mutation on the profile of IhERG during physiological waveforms. Although limited (single concentration) in vitro data have been reported for racemic sotalol and quinidine [24], the present study is the first to provide concentration response data for any drug against T618I hERG and it is also the first to provide any in vitro data for T618I IhERG inhibition by disopyramide, D-sotalol and flecainide.
Effects of the T618I Mutation on IhERG
Although the recent study by Sun and colleagues is the first report of the occurrence of the T618I hERG mutation in a clinical context [24], one other investigation has utilised this mutation in the study of the role of a nearby S5 residue (H562) that is able to interact with the pore helix [37]. In that study, T618I IhERG was shown to exhibit both increased currents at positive voltages and reduced tail currents compared to pulse currents following positive voltage commands [37]. These features are in accord with the subsequent report by Sun and colleagues and with our own data. However, Lees-Miller and colleagues reported a significant (>+30 mV) positive shift in IhERG activation V0.5 for T618I hERG [37], whilst Sun et al. reported a small (∼−5 mV) negative shift in activation V0.5 compared to WT IhERG [24]. Both studies were conducted using HEK cells for hERG channel expression, whilst Lees Miller et al. performed measurements at 36°C [37] and the recording temperature for the study by Sun et al. was not given [24]. Thus, the reason for the apparently opposite observations in the two studies in respect of activation V0.5 is not clear. In our experiments, using a similar expression system and recording at 37°C, there was a +15 mV shift in activation V0.5, which is in good qualitative agreement with the findings of Lees Miller et al. [37], but differs from the negative activation shift of V0.5 reported by Sun and colleagues [24]. However, unlike Lees-Miller et al. [37] and in accord with Sun and colleagues [24], we saw a significant effect of the mutation on IhERG deactivation time-course, with both τf and τs time constants of T618I IhERG deactivation smaller than those for WT IhERG. Also in accord with Sun and colleagues [24], we did not observe any significant alteration to the rate of IhERG activation for the T618I hERG mutant. The shift in voltage dependence of IhERG inactivation (availability) seen here (Figures 3A,B) is in qualitative agreement with positive shifted inactivation reported by Sun et al. [24], as is the positively shifted region of negative slope in the end pulse I-V relation (Figure 1C). However, the extent of positive shift in inactivation V0.5 (∼+23–25 mV) seen here was smaller than that reported by Sun and colleagues (∼+50 mV); the reason for this difference is at present not clear. Nevertheless. the shift steady-state inactivation seen here is demonstrably sufficient to lead to a significant functional impact: ‘window current’ calculations based on our derived activation and inactivation V0.5 and k values revealed significant augmentation, as well as positively shifted peak, of the IhERG window for T618I hERG when compared with WT hERG (Figure 3C). Slowing of time-dependent development of inactivation of IhERG (Figure 3D) may have a synergistic effect in permitting greater IhERG to flow. A modulatory effect of the T618I mutation on IhERG inactivation is not entirely unexpected, given that mutation of the nearby S620 residue (to S620T) has been established to abolish hERG channel inactivation (e.g. [38], [39]), although in contrast to the S620T mutation it is clear that the T618I mutation produces a more modest, partial attenuation of IhERG inactivation.
Pharmacology of T618I hERG
It is well established that the inactivation process is important for binding to the hERG channel of a range of drugs, but it is also the case that not all drugs are equally dependent upon inactivation for binding to the channel to occur (e.g. [18], [20], [21], [38]–[42]). The SQT1 N588K mutation has been shown to lead to markedly elevated IC50 values for IhERG blockade by methanesulphonanilide compounds including sotalol (20-fold WT IhERG IC50 for D-sotalol) and E-4031 (∼11.5-fold WT IhERG IC50), whilst those for quinidine (∼3.5–6-fold WT IhERG IC50) and disopyramide (1.5-fold WT IhERG IC50) are comparatively little affected [18], [20]. In the present study, the T618I hERG mutation elevated the IC50 for D-sotalol by ∼3 fold under conventional voltage clamp, which is substantially less than that seen for N588K hERG [18]. With a voltage protocol similar to that used in the present study, IhERG N588K hERG availability was found to be positively shifted by ∼+62 mV [16]. In the present study, the shift in the voltage dependence of T618I IhERG inactivation was +∼23-+25 mV. It therefore seems likely that the smaller effect of the T618I mutation in attenuating IhERG block by D-sotalol can be attributed to the ability of the T618I channel to inactivate to a greater extent than has been found to be the case for N588K hERG. In this regard, it is noteworthy that the results of experiments in which different inactivation mutations have been combined in order to titrate hERG inactivation suggest that IhERG blocking potency is not related to inactivation in a linear fashion. Thus, for both quinidine and disopyramide single mutations that reduced macroscopic IhERG inactivation to ∼20% produced only modest (1.5 and 3.5 fold) reductions in the potency of disopyramide and quinidine, whilst double-mutations that reduced inactivation to <10% led to elevations of IC50 by 6.5 and 7-fold respectively [21]. For T618I hERG in this study, the IC50 for quinidine under conventional voltage clamp was ∼ 1.4 that of the WT channel, whilst for disopyramide it was ∼2.2-fold that of the WT channel. The attenuation of IhERG inactivation by the T618I mutation therefore appears to be insufficient to interfere dramatically with drug binding. At the same time, the greater effect of this mutation on disopyramide’s potency under conventional voltage clamp than that seen previously for the N588K mutation (which impairs inactivation to a greater extent than does T618I [15], [16], [21], [24]) suggests that other effects of the mutation on channel conformation as well as upon inactivation per se may contribute to its overall effect on disopyramide binding. To our knowledge there are no prior data available on effects of inactivation-attenuating hERG mutants on IhERG blocking potency of flecainide. A prior study from our laboratory has shown that the characteristics of flecainide inhibition of WT IhERG are qualitatively similar to those of the Class Ia antiarrhythmic quinidine and of another Class Ic drug, propafenone [35]. Given that quinidine, disopyramide and propafenone have all been shown to exhibit comparatively little dependence on hERG channel inactivation to exert their inhibitory effects [20], [21], [36], [42] and also that the T618I mutation produced only a modest effect on IhERG blocking potency in this study, it seems reasonable to conclude that hERG channel inactivation is not a major determinant of flecainide potency against hERG. Further experiments on attenuated inactivation mutants are required to determine unequivocally whether or not this is the case.
We also compared between WT and T618I hERG the potency of IhERG inhibition under AP clamp, for each of the drugs studied under conventional voltage clamp. It is known that drug inhibitory potency against IhERG can vary depending on stimulus protocol [34], [43], [44]. In our experiments, both stimulus waveform (step versus AP command) and stimulus frequency (repetitive pulsing once every 12 s versus once every second -to apply APs at a physiological rate) differed between the protocols used to obtain the data in Figures 6 and 7. However, the IC50 values for WT IhERG inhibition by any of the drugs studied did not differ greatly between conventional and AP clamp protocols (see Tables 1 and 2). In general, however, differences between IC50 values obtained with conventional and AP clamp protocols were greater for T618I hERG, although the C.I range for IC50s with the two protocols showed either some overlap (quinidine, disopyramide, D-sotalol) or little separation (flecainide). The range of T618I/WT IC50 ratio values was found to be somewhat smaller (1.2–2.0) under AP clamp than under conventional voltage clamp (1.4–3.2), with a marked reduction in this for D-sotalol. Contributory factors to this may be intrinsic voltage-dependence of inhibition [34]–[36] together with the occurrence (and hence measurement) of peak IhERG at a comparatively positive voltage for T618I compared to WT IhERG during the AP waveform (and compared to the measurement voltage (−40 mV) for T618I IhERG tails under conventional voltage clamp), and a greater sensitivity of drug block to duty-cycle (rate) for the mutant. On the basis of our findings, future detailed investigation of effects of T618I hERG kinetics on channel block are likely to be instructive in this regard, though are beyond the intended scope of the present study.
One puzzling aspect of our pharmacology data is that for the Class I drugs studied, nH values derived from concentration-response relations obtained under conventional voltage clamp were substantially lower (<0.5 for quinidine and disopyramide) for T618I than for WT IhERG, whilst this was not the case under AP clamp (compare Tables 1 and 2). The low nH values under conventional voltage clamp do not appear to be attributable to voltage-drop down uncompensated series resistance for T618I IhERG recordings: estimated voltage drop was lower for quinidine (2.31±0.37 mV; n = 16) than for D-sotalol (7.61±0.37 mV; n = 21), although the nH value was higher for D-sotalol than for quinidine (Table 1). On the other hand, were the marked reduction in nH for quinidine and disopyramide strongly reflective of altered drug-channel interaction due to the T618I mutation it might be anticipated also to occur for data from AP clamp experiments and this was not the case. The basis for the apparently low nH for quinidine and disopyramide for T618I IhERG remains unexplained at the present time. Arguably, the more (patho)physiologically relevant pharmacological data are those obtained under AP clamp at a physiologically relevant rate; the major conclusion from those data (Figure 6 and Table 2) is that under these conditions the T618I mutation did not produce a large attenuation of inhibitory potency for any drug studied.
Clinical Relevance
In this study we observed that, under AP clamp, T618I mutant IhERG exhibited an altered current profile, peaking earlier during the AP plateau than was the case for WT IhERG. Previous studies in which the SQT1 N588K hERG mutant has been studied under ventricular AP clamp have shown an inverted U or bow-shaped current profile peaking at ∼+20 mV, consistent with the occurrence of little inactivation over physiologically relevant membrane potentials [13], [15], [16], [33]. The N588K hERG mutation produces a greater attenuation of IhERG inactivation than does T618I hERG and our AP clamp data are suggestive of an electrophysiological phenotype for T618I hERG during the ventricular AP that is intermediate between those of WT and N588K IhERG. Accordingly, the effect of the T618I mutation in accelerating ventricular AP repolarisation can also be predicted to be less than that of N588K hERG. This is in agreement with the less extensive QTc interval shortening for SQT1 patients with the T618I mutation (mean in affected individuals of 316 ms) [24] than those with the N588K mutation (QTc of ≤ 300 ms in the first two SQT1 genotyped families [13] and a QT of 230 ms in the proband of a third family [14]). The normally slow deactivation of IKr/IhERG can contribute to resting membrane conductance and protection from premature depolarisation immediately after completion of ventricular AP repolarisation; in pathological settings accelerated IKr deactivation may increase excitability early in diastole [30], [45]. Whether or not the faster deactivation of T618I than WT hERG is able to contribute abbreviated refractory period and susceptibility to programmed simulation (as clinically observed for SQT1 patients with the T618I mutation [24]) remains to be established, but warrants future in silico investigation [30], [46].
A first line treatment for the SQTS is the use of implantable defibrillators (ICDs) to protect against sudden death, although ICD use itself carries the risk of inappropriate shocks [47]. A recent report of long term follow up of SQTS patients noted that 58% of patients with ICDs had device-related complications [48]. The same report [48] notes that the T618I SQT1 mutation has now been found in a second family in addition to that originally identified by Sun and colleagues [24]. Pharmacological therapy is therefore attractive both for patients in whom ICDs are not fitted and as an adjunct therapy to reduce arrhythmic events and restore QT intervals towards normal. Our findings extend those previously obtained at a single (>70% blocking) quinidine concentration [24]; collectively the full concentration response data obtained with both conventional voltage and AP clamp protocols indicate that quinidine largely retains its potency against T618I IhERG. The available in vitro data therefore indicate that quinidine is likely to be beneficial in T618I-linked SQT1. Concordant with this, hydroquinidine has recently been reported to have a positive effect on QTc intervals in T618I hERG carriers [48]. However, whilst the available evidence from long-term follow up of SQTS patients is that (hydro)quinidine is also effective in arrhythmia prophylaxis [48], diminishing availability of quinidine [49] makes it attractive to find alternative pharmacological therapies for use in SQTS patients. Disopyramide is effective against the N588K mutation in vitro [20] and has shown benefits in SQT1 patients [19]. Our experiments indicate that although there is a modest reduction in disopyramide potency for T618I IhERG both during conventional and AP voltage protocols, our data indicate that some IhERG/IKr blockade can nevertheless be expected to occur within the clinical concentration range (∼6–8 µM; [50]). Thus, disopyramide may be worthy of investigation as a potential treatment for T618I-linked SQT1. Sun et al. have suggested that T618I hERG carriers may be less resistant to drugs like sotalol than had been previously found for N588K-linked SQT1 [24]. Our data with D-sotalol, particularly those obtained under AP voltage clamp, support this proposition; the reduction in IhERG blocking potency of D-sotalol by T618I hERG appears to be substantially less than that produced by N588K hERG [18]. It is possible, therefore, that sotalol may be worthy of clinical investigation for T618I-linked SQT1. Future in vitro work may also be warranted to determine whether higher affinity methanesulphonanilide Class III drugs than sotalol that are in clinical use (ibutilide, dofetilide) are able to exert some inhibition of T618I at clinically relevant concentrations. Of particular note, flecainide was found to exert marked inhibition of both WT and T618I IhERG at concentrations relevant to clinical serum levels (0.5 to 2.4 µM; [51]), with little difference between WT and T618I IhERG IC50 under AP clamp. Flecainide has been tested previously in a group of SQT1 (N588K hERG) patients unresponsive to sotalol but responsive to hydroquinidine [52]. In that study it was found to produce a small prolongation of QT interval in some patients, which was largely attributable to QRS interval lengthening [52]. To our knowledge, comparable data are lacking in patients with the T618I hERG SQT1 mutation. However, on the basis of our findings flecainide may warrant investigation in this group. Sun and colleagues have also provided evidence that a >70% blocking concentration of quinidine reduces the inactivation shift for T618I IhERG [24]. However, in our AP clamp experiments none of the drugs studied produced any consistent correction of T618I IhERG profile during a physiological waveform; this suggests that potential benefits of the drugs studied here for QT intervals in patients with the T618I hERG mutation are likely to be attributable to reduction in total repolarising IhERG/IKr, without restoration of the current’s normal time- and voltage- dependent profile during ventricular APs.
Acknowledgments
The authors thank Mrs Lesley Arberry for technical assistance.
Funding Statement
The authors thank the British Heart Foundation for funding (AEH: PG/10/96; DM: FS/11/59; YZ: PG/10/17). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Sanguinetti MC, Jurkiewicz NK (1990) Two components of cardiac delayed rectifier K+ current. J Gen Physiol 96: 195–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tamargo J, Caballero R, Gomez R, Valenzuela C, Delpon E (2004) Pharmacology of cardiac potassium channels. Cardiovasc Res 62: 9–33. [DOI] [PubMed] [Google Scholar]
- 3. Sanguinetti MC, Jiang C, Curran ME, Keating MT (1995) A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. Cell 81: 299–307. [DOI] [PubMed] [Google Scholar]
- 4. Trudeau MC, Warmke JW, Ganetzky B, Robertson GA (1995) HERG, an inward rectifier in the voltage-gated potassium channel family. Science 269: 92–95. [DOI] [PubMed] [Google Scholar]
- 5. Weirich J, Antoni H (1998) Rate-dependence of antiarrhythmic and proarrhythmic properties of class I and class III antiarrhythmic drugs. Basic Res Cardiol 93 S1: 125–132. [DOI] [PubMed] [Google Scholar]
- 6. Witchel HJ, Hancox JC (2000) Familial and acquired long QT syndrome and the cardiac rapid delayed rectifier potassium channel. Clinical and Experimental Pharmacology and Physiology 27: 753–766. [DOI] [PubMed] [Google Scholar]
- 7. Sanguinetti MC, Mitcheson JS (2005) Predicting drug-hERG channel interactions that cause acquired long QT syndrome. TIPS 26: 119–124. [DOI] [PubMed] [Google Scholar]
- 8. Hancox JC, McPate MJ, El Harchi A, Zhang YH (2008) The hERG potassium channel and hERG screening for drug-induced torsades de pointes. Pharmacology and Therapeutics 119: 118–132. [DOI] [PubMed] [Google Scholar]
- 9. Sanguinetti MC, Tristani-Firouzi M (2006) hERG potassium channels and cardiac arrhythmia. Nature 440: 463–469. [DOI] [PubMed] [Google Scholar]
- 10. Modell SM, Lehmann MH (2006) The long QT syndrome family of cardiac ion channelopathies: a HuGE review. Genet Med 8: 143–155. [DOI] [PubMed] [Google Scholar]
- 11. Schimpf R, Wolpert C, Gaita F, Giustetto C, Borggrefe M (2005) Short QT syndrome. Cardiovasc Res 67: 357–366. [DOI] [PubMed] [Google Scholar]
- 12. Maury P, Extramiana F, Sbragia P, Giustetto C, Schimpf R, et al. (2008) Short QT syndrome. Update on a recent entity. Arch Cardiovasc Dis 101: 779–786. [DOI] [PubMed] [Google Scholar]
- 13. Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, et al. (2004) Sudden death associated with short-QT syndrome linked to mutations in HERG. Circulation 109: 30–35. [DOI] [PubMed] [Google Scholar]
- 14. Hong K, Bjeerregaard P, Gussak I, Brugada R (2005) Short QT syndrome and atrial fibrillation caused by mutation in KCNH2. J Cardiovas Electophysiol 16: 394–396. [DOI] [PubMed] [Google Scholar]
- 15. Cordeiro JM, Brugada R, Wu YS, Hong K, Dumaine R (2005) Modulation of IKr inactivation by mutation N588K in KCNH2: a link to arrhythmogenesis in short QT syndrome. Cardiovas Res 67: 498–509. [DOI] [PubMed] [Google Scholar]
- 16. McPate MJ, Duncan RS, Milnes JT, Witchel HJ, Hancox JC (2005) The N588K-HERG K+ channel mutation in the ‘short QT syndrome’: mechanism of gain-in-function determined at 37°C. Biochem Biophys Res Comm 334: 441–449. [DOI] [PubMed] [Google Scholar]
- 17. Giustetto C, Di MF, Wolpert C, Borggrefe M, Schimpf R, et al. (2006) Short QT syndrome: clinical findings and diagnostic-therapeutic implications. Eur Heart J 27: 2440–2447. [DOI] [PubMed] [Google Scholar]
- 18. Wolpert C, Schimpf R, Giustetto C, Antzelevitch C, Cordeiro JM, et al. (2005) Further insights into the effect of quinidine in short QT syndrome caused by a mutation in HERG. J Cardiovas Electophysiol 16: 54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schimpf R, Veltmann C, Giustetto C, Gaita F, Borgreffe M (2007) In vivo effects of mutant HERG K+ channel inhibition by disopyramide in patients with a short QT-1 syndrome: a pilot study. J Cardiovas Electophysiol 18: 1157–1160. [DOI] [PubMed] [Google Scholar]
- 20. McPate MJ, Duncan RS, Witchel HJ, Hancox JC (2006) Disopyramide is an effective inhibitor of mutant HERG K+ channels involved in variant 1 short QT syndrome. J Mol Cell Cardiol 41: 563–566. [DOI] [PubMed] [Google Scholar]
- 21. McPate MJ, Duncan RS, Hancox JC, Witchel HJ (2008) Pharmacology of the short QT syndrome N588K-hERG K+ channel mutation: differential impact on selected class I and class III antiarrhythmic drugs. Br J Pharmacol 155: 957–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hassel D, Scholz EP, Trano N, Friedrich O, Just S, et al. (2008) Deficient zebrafish ether-a-go-go-related gene channel gating causes short-QT syndrome in zebrafish reggae mutants. Circulation 117: 866–875. [DOI] [PubMed] [Google Scholar]
- 23. Zhang YH, Colenso CK, Sessions RB, Dempsey CE, Hancox JC (2011) The hERG K+ channel S4 domain L532P mutation: characterization at 37°C. Biochim Biophys Acta 1808: 2477–2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sun Y, Quan XQ, Fromme S, Cox RH, Zhang P, et al. (2011) A novel mutation in the KCNH2 gene associated with short QT syndrome. J Mol Cell Cardiol 50: 433–441. [DOI] [PubMed] [Google Scholar]
- 25. Zhou Z, Gong Q, Ye B, Fan Z, Makielski JC, et al. (1998) Properties of HERG channels stably expressed in HEK 293 cells studied at physiological temperature. Biophys 74: 230–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. El Harchi A, Zhang YH, Hussein L, Dempsey CE, Hancox JC (2012) Molecular determinants of hERG potassium channel inhibition by disopyramide. J Mol Cell Cardiol 52: 185–195. [DOI] [PubMed] [Google Scholar]
- 27. El Harchi A, McPate MJ, Zhang YH, Zhang H, Hancox JC (2009) Action potential clamp and chloroquine sensitivity of mutant Kir2.1 channels responsible for variant 3 short QT syndrome. J Mol Cell Cardiol 137: 83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Levi AJ, Hancox JC, Howarth FC, Croker J, Vinnicombe J (1996) A method for making rapid changes of superfusate whilst maintaining temperature at 37°C. Pflugers Arch 432: 930–937. [DOI] [PubMed] [Google Scholar]
- 29.Sanguinetti MC, Curran ME, Spector PS (1995). Block of delayed rectifier K+ channels as an antiarrhythmic mechanism. In: Vereecke J, van Bogaert PP, Verdonck F, editors. Potassium channels in normal and pathological conditions. Leuven University Press. p. 151–66.
- 30. Du CY, Adeniran I, Cheng H, Zhang YH, El Harchi, et al. (2010) Acidosis Impairs the Protective Role of hERG K+ Channels Against Premature Stimulation. J Cardiovasc Electrophysiol 21: 1160–1169. [DOI] [PubMed] [Google Scholar]
- 31. Smith PL, Baukrowitz T, Yellen G (1996) The inward rectification mechanism of the HERG cardiac potassium channel. Nature 379: 833–836. [DOI] [PubMed] [Google Scholar]
- 32. Hancox JC, Levi AJ, Witchel HJ (1998) Time course and voltage dependence of expressed HERG current compared with native ‘rapid’ delayed rectifier K current during the cardiac ventricular action potential. Pflugers Archiv - European Journal of Physiology 436: 843–853. [DOI] [PubMed] [Google Scholar]
- 33. McPate MJ, Zhang H, Adeniran I, Cordeiro JM, Witchel HJ, et al. (2009) Comparative effects of the short QT N588K mutation at 37°C on hERG K+ channel current during ventricular, Purkinje fibre and atrial action potentials: an action potential clamp study. J Physiol Pharmacol 60: 23–41. [PubMed] [Google Scholar]
- 34. Milnes JT, Witchel HJ, Leaney JL, Leishman DJ, Hancox JC (2010) Investigating dynamic protocol-dependence of hERG potassium channel inhibition at 37°C: Cisapride versus dofetilide. J Pharmacol Toxicol Methods 61: 178–191. [DOI] [PubMed] [Google Scholar]
- 35. Paul AA, Witchel HJ, Hancox JC (2002) Inhibition of heterologously expressed HERG potassium channels by flecainide and comparison with quinidine, propafenone and lignocaine. Br J Pharmacol 136: 717–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Paul AA, Witchel HJ, Hancox JC (2001) Inhibition of HERG potassium channel current by the Class 1a antiarrhythmic agent disopyramide. Biochem Biophys Res Comm 280: 1243–1250. [DOI] [PubMed] [Google Scholar]
- 37. Lees-Miller JP, Subbotina JO, Guo J, Yarov-Yarovoy V, Noskov SY, et al. (2009) Interactions of H562 in the S5 helix with T618 and S621 in the pore helix are important determinants of hERG1 potassium channel structure and function. Biophys 96: 3600–3610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Perrin MJ, Kuchel PW, Campbell TJ, Vandenberg JI (2008) Drug binding to the inactivated state is necessary but not sufficient for high-affinity binding to human ether-à-go-go-related gene channels. Mol Pharmacol 74: 1443–1452. [DOI] [PubMed] [Google Scholar]
- 39. Ficker E, Jarolimek W, Kiehn J, Baumann A, Brown AM (1998) Molecular determinants of dofetilide block of HERG K channels. Circ Res 82: 386–395. [DOI] [PubMed] [Google Scholar]
- 40. Weerapura M, Hebert TE, Nattel S (2002) Dofetilide block involves interactions with open and inactivated states of HERG channels. Pflugers Arch 443: 520–531. [DOI] [PubMed] [Google Scholar]
- 41. Numaguchi H, Mullins FM, Johnson JP Jr, Johns DC, Po SS, et al. (2000) Probing the interaction between inactivation gating and Dd-sotalol block of HERG. Circ Res 87: 1012–1018. [DOI] [PubMed] [Google Scholar]
- 42. Lees-Miller JP, Duan Y, Teng GQ, Duff HJ (2000) Molecular determinant of high affinity dofetilide binding to HERG1 expressed in Xenopus oocytes: involvement of S6 sites. Molecular Pharmacology 57: 367–374. [PubMed] [Google Scholar]
- 43. Kirsch GE, Trepakova ES, Brimecombe JC, Sidah SS, Erickson HD, et al. (2004) Variability in the measurement of hERG potassium channel inhibition: effects of temperature and stimulus pattern J Pharmacol Toxicol Methods. 50: 93–101. [DOI] [PubMed] [Google Scholar]
- 44. Yao JA, Du X, Lu D, Baker RL, Daharsh E, et al. (2005) Estimation of potency of hERG inhibitors: impact of voltage protocol and temperature. J Pharmacol Toxical Methods 52: 146–153. [DOI] [PubMed] [Google Scholar]
- 45. Lu Y, MahautSmith MP, Varghese A, Huang CLH, Kemp PR, et al. (2001) Effects of premature stimulation on HERG channels. J Physiol 537 3: 843–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Adeniran I, McPate MJ, Witchel HJ, Hancox JC, Zhang H (2011) Increased vulnerability of human ventricle to re-entrant excitation in hERG-linked variant 1 short QT syndrome. PLoS Comput Biol 7(12): e1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schimpf R, Wolpert C, Bianchi F, Giustetto C, Gaita F, et al. (2003) Congenital short QT syndrome and implantable cardioverter defibrillator treatment: inherent risk for inappropriate shock delivery. J Cardiovasc Electrophysiol 14: 1273–1277. [DOI] [PubMed] [Google Scholar]
- 48. Giustetto C, Schimpf R, Mazzanti A, Scrocco C, Maury P, et al. (2011) Long-term follow-up of patients with short QT syndrome. J Am Coll Cardiol 58: 587–595. [DOI] [PubMed] [Google Scholar]
- 49. Viskin S, Antzelevitch C, Marquez MF, Belhassen B (2007) Quinidine: a valuable medication joins the list of ‘endangered species’. Europace 9(12): 1105–1106. [DOI] [PubMed] [Google Scholar]
- 50. Zema MJ (1984) Serum drug concentration and adverse effects in cardiac patients after administration of a new controlled-release disopyramide preparation. Ther Drug Monit 6: 192–198. [DOI] [PubMed] [Google Scholar]
- 51. Breindahl T (2000) Therapeutic drug monitoring of flecainide in serum using high-performance liquid chromatography and electrospray mass spectrometry. J Chromatogr B Biomed Sci Appl 746: 249–254. [DOI] [PubMed] [Google Scholar]
- 52. Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, et al. (2004) Short QT syndrome: Pharmacological treatment. J Am Coll Cardiol 43: 1494–1499. [DOI] [PubMed] [Google Scholar]