Abstract
Objectives
Religious coping arguably prevents negative health outcomes for stressed persons. This study examined the moderating role of religious coping (positive, negative, and combined) in the connection of care recipient functional status with diurnal salivary cortisol patterns among dementia family caregivers.
Methods
Thirty African-American (AA) female dementia caregivers and 48 AA noncaregivers completed the Religious Coping (RCOPE) scale, Activities of Daily Living (ADL) scale and Revised Memory and Behavior Problem checklist (RMBPC) and collected five saliva samples daily (at awakening, 9am, 12pm, 5pm, and 9pm) for two straight days.
Results
Hierarchical regression tests with mean diurnal cortisol slope as the outcome illustrated surprisingly that higher combined and positive (but not negative) RCOPE scores were associated with increasingly flatter or worse cortisol slope scores for caregivers (but not non-caregivers). Of note, the RCOPE by RMBPC interaction was significant. Among caregivers who reported higher RMBPC scores, higher combined and positive (but not negative) RCOPE scores were unexpectedly associated with increasingly flatter cortisol slopes.
Conclusions
These results extend current findings by showing that being AA, a caregiver, and high in positive religious coping may predict increased daily stress responses, mainly for those with higher patient behavioral problems. Since religious coping is a central coping strategy for AA caregivers, it is vital that epidemiological assessments of religious coping in health and aging as well as tailored interventions focus on the unique reasons for this disparity.
Keywords: dementia, caregiving, coping, neuroendocrine function, ethnicity
About 20% of all adult caregivers care for someone aged 50 years or older who has dementia (1). Caregiver status, or the process of caring for others with debilitating diseases (e.g., dementia) can take a sustained toll on physical health and thus predict chronic disease outcomes (e.g., vascular disease) (2-8). Like so, disturbed daily hypothalamic-pituitary-adrenal cortex axis (HPA; e.g., flattened diurnal cortisol) levels are an established marker of future cardiovascular disease for high risk populations (3-8). Salivary cortisol is a valuable index of the accumulated health impact of daily stress as cortisol levels vary with a usual decrease in levels across the day and track along with major life stressors such as Alzheimer's disease and related dementia (ADRD) caregiver stress (3-8). However, less is known about how the daily HPA profiles of diverse ADRD caregivers is influenced by the combination of protective psychosocial factors such as religious coping (RCOPE) and experience with exceptionally difficult challenges of caregiving.
Religious Coping and Health
Religion and spirituality are used disproportionately by African-Americans (AAs) (compared to Whites) to cope with stressful demands and buffer risk for chronic health problems (9, 10). More RCOPE in the form of prayer, attendance at formal services, and/or strong belief systems, may provide a mentally mediated braking system that limits the adverse physiological impact of daily life stressors (11).
Conversely, recent research suggests that strong religious beliefs and experiences can also predict harm to health (12). For instance, on top of promoting helpful psychosocial effects, high religious beliefs can also generate feelings of shame and reduced self-esteem, which in turn is linked with increased risk for mental illness (11). As well, Haley et al. (13) found more functional disability among AA adults who endorsed extremes of involvement in personal religious activities (e.g., bible study, prayer). Finally, positive (e. g., optimistic religious appraisals of experiences) versus negative forms (e. g., punitive religious appraisals) of RCOPE are related to better mental and physical health status.
Religious Coping, Caregiver Stress and Health
Recent studies highlight the popularity of RCOPE among ADRD caregivers, notably non-Whites (5, 15-21). For instance, recent evidence shows that more religious non-White caregivers have better mental health, subjective well-being, and more positive attitudes toward the caregiver role (16, 18, 20, 21). RCOPE may be especially healthy for ADRD caregivers in the context of poor care recipient functional status (22). Yet more research needs to be done to confirm this trend.
Over of the course of ADRD, impaired care recipient function such as memory and behavior problems have major costs for recipients and caregivers (23). More impaired memory and behavior problems are linked with worse recipient Mini-Mental State Examination (MMSE) scores (24) and nursing home admissions (25), more depression from caregiving (7, 23) and dysregulated daily cortisol responses (2). Notably, AA (vs. White) caregivers have fewer negative judgments of troublesome behavior by impaired care recipients (15).
Moreover, numerous ADRD caregivers report care recipients who are impaired with activities of daily living (ADL; 26, 27), everyday activities normally performed for self-care (e.g., bathing). Impaired ADL predict higher risk for care recipients in the form of lower MMSE scores, and more hospitalizations and nursing home placement (27). For caregivers, impaired care recipient ADL are linked with higher depression (28, 29). So given the potent role of impaired care recipient function in caregiver health, a pertinent question is whether RCOPE buffers the physiological stress responses of diverse overwhelmed caregivers.
McCallum et al. (6) found that AA dementia family caregivers may experience stress more in terms of physiological reactivity rather than mental health outcomes. Thus, ADRD caregiver status challenges coping resources, and consequently may be a risk factor for chronic physical disorders for AAs who persevere in the caregiver role (3, 4, 30). One preventive resource for the deleterious health effects of caregiver stress may be RCOPE (16, 18). However, there is no published study examining the relationship between RCOPE and HPA axis profiles for diverse ADRD caregivers with more challenging care recipients.
Thus, a primary aim of this study was to show that for AA caregivers with highly impaired care recipients (i.e., high ADL and memory and behavioral problems, respectively), lower combined and positive RCOPE would predict flatter diurnal cortisol responses. The RCOPE by impaired care recipient function hypothesis is a culturally relevant and less pathologically oriented extension of traditional coping models of caregiving. Given the current mixed findings about the role of RCOPE in health outcomes, a secondary aim was to show that lower combined and positive RCOPE for caregivers (vs. non-caregivers) would predict flatter cortisol slope scores.
Method
Participants
Participants were AA (N = 30) female dementia caregivers who spent a minimum of ten hours per week helping a family member with memory loss and 48 AA noncaregivers. Women under the age of 50 were excluded as HPA response is moderated by age (31). Participants were recruited through the caregiver registry at University Memory and Aging Center of University Hospitals and Case Western Reserve University as well as flyers posted and presentations given at nearby senior homes. A more comprehensive account of our recruitment plan can be found in a separate report (32).
Procedure
The study was approved by the Institutional Review Board of University Hospitals of Cleveland, OH. Prospective participants were phoned and provided a synopsis of the protocol. All participants offered informed consent and data were received during in-home interviews. After the interview, an experienced research assistant explained and displayed the steps for self-collecting saliva samples. The interviewer next planned to return in three to seven days for the saliva samples. Once the interviewer collected the saliva samples, participants were paid $30 for their contribution to the study.
Measures
Salivary cortisol measurement
Participants collected saliva at home with “Salivette” devices (Sarstedt Co., Rommelsdorf, Germany) with a cotton swab placed in a plastic holder and housed inside a centrifuge tube. Participants were given cortisol kits with ten Salivettes with each one marked by day and time of measurement. Participants kept kits in their refrigerators. They were instructed to collect five saliva samples for two succeeding days at the subsequent times: after awakening, at 9 am, 12 noon, 5 pm, and 9 pm. The samples were mainly picked up by the research assistant the day after completion of the protocol and delivered to the General Clinic Research Center (GCRC) of University Hospitals. As salivary cortisol levels may vary by exercise, sleep patterns, and medication usage, each Salivette kit also included a form for participants to detail any unusual exercise, sleep, and medication patterns on the days that saliva samples were collected.
Laboratory methods
Salivary cortisol samples were examined twice monthly in a GCRC wet lab by immunoassay utilizing microtiter plates and were centrifuged at 3,000 rpm for 15 minutes. Cortisol levels were established using a time-based immunoassay with fluorometric end point detection (LIA), as illustrated elsewhere (31). Cross-assay coefficients of variation were < 10%. The findings are designated as micrograms per deciliter (μg/dL).
Sociodemographic measures
Demographic and caregiving-related data included age, ethnicity, education level (on a scale from one to five with the value “2” representing some college), menopausal status, duration of caregiving (in months), and primary caregiver status (yes or no).
Caregiving stressors
Care recipient functional status, reported by caregivers, was assessed with the Activities of Daily Living Scale (ADL)(33). Six items from the Activities of Daily Living Scale (Cronbach's alpha in the current sample = .90) measured the care recipient's ability to perform essential tasks of daily life independently (i.e., bathing, toileting, dressing, eating, oral/dental care, and transfer). Response options were, “1” no help, “2” some help, and “3” a lot of help needed. Scores were summed with higher scores suggesting more functional impairment. Total ADL scores could extend from six to 18 points. The current sample had an average of 10.79 (SD = 4.02) ADL problems.
The Revised Memory and Behavior Problems Checklist (RMBPC; 34) indexes the amount of worrisome problems related to memory, agitation, and depression that the patient has experienced in the past week. The RMBPC has excellent reliability and correlates with care recipient MMSE scores (24) and higher caregiver depression levels and fewer positive affective rewards from caregiving (23). The RMBPC has 24 items with response options extending from “not at all” (coded as a “0”) to “extremely” (coded as a “4”). Higher RMBPC scores suggest more problems for patients. This sample had an average RMBPC reaction score of 38.13 (SD = 15.01).
Religious Coping
The Religious Coping (RCOPE) scale assesses positive and negative RCOPE with difficult circumstances and includes 34 items (14). Response options extend from “0” not at all” to “3” a great deal”. 14 items from the RCOPE consists of two facets: 1) positive RCOPE, with items on spiritual relations and hopeful religious appraisals of events; and 2) negative RCOPE, with items on penalizing religious judgments and bitterness to God. Both subscales have shown outstanding internal consistency and validity (14). The present study also employed a combined “positive” RCOPE score rooted in the sum of the positive and (reverse-coded) negative subscales. In the present study, the mean combined RCOPE score of 22.78 (SD = 4.88) was consistent with prior findings.
Plan for statistical analysis
Log transformed mean diurnal cortisol slope scores were produced for each participant by calculating the slope of the eight cortisol scores over the two days and then multiplying that value by 1,000. The values for each time point were also evaluated but will not be included in the current paper for the sake of simplicity in analytical focus. More positive values which signify flatter daily cortisol slopes imply increased risk for chronic disease (35). Correlational analyses were run for cortisol response, sociodemographic, caregiving and psychosocial variables.
For hypothesis one, a secondary aim, hierarchical regression models (HMRs) were run by overall sample with daily cortisol slope scores as the dependent measure and predictor variables entered in the following order: step 1) RCOPE (combined score, positive, and negative, respectively) and caregiver status (yes or no), step 2) the interaction of RCOPE and caregiver status, and step 3) age and education. It was hypothesized that higher scores on combined and positive RCOPE for caregivers (vs. non-caregivers) would be linked with lower cortisol slope scores. More negative RCOPE, on the other hand, would be associated with flatter cortisol slope scores for caregivers (vs. non-caregivers). The HMR models were used to mean a simple multiple regression where variables were entered in a blocked fashion, to account for the role of RCOPE measures on cortisol slope scores and assess the roles of RCOPE and caregiver status in cortisol slope scores with and without the influence of age and education.
Group-based correlation analyses were run to resolve the pattern of significant HMR effects for the interactions of RCOPE and caregiver status. Using the Fisher r-to-z transformation, a parametric test, z scores were computed to assess the significance of difference between correlation coefficients [Fisher's z(diff)] of RCOPE with cortisol slope scores by caregiver status (36). A significant difference suggests that increasing RCOPE is associated with a different pattern of cortisol slope scores by caregiver status.
For hypothesis two, the primary aim, HMRs were run for caregivers with daily cortisol slope scores as the dependent measure and predictor variables entered in the following order: step 1) RCOPE (combined score, positive, and negative, respectively) and recipient functional status (RMBPC and ADL, respectively), step 2) the interaction of RCOPE and recipient functional status, and step 3) age, education, primary caregiver status, and duration of caregiving. It was hypothesized that higher scores on combined (hereafter called “RCOPE”) and positive RCOPE would predict more negative cortisol slope scores at higher levels of ADL and RMBPC, respectively. Dichotomous measures of ADL and RMBPC (based on median-splits) respectively were computed. Fisher's r-to-z transformation tests were run to resolve the pattern of significant HMR effects for the interactions of RCOPE and care recipient function.
Note that the criterion for significance for the various HMR tests given the Type I error rate for multiple tests was p < .01. Values for effect size (i.e., Cohen's d) were computed using the t value for a significant HMR effect and the corresponding degrees of freedom (df).
Results
Group Demographics
Tables 1(a) and 1(b) show the descriptive statistics and correlations for the overall sample by caregiver status. There were no significant differences by caregiver status for any variable. Caregivers were not significantly different from non-caregivers on reports of post-menopausal status [40% vs. 60%; χ(2, 78) = 1.29; p < .52]. While 57% of caregivers reported being the primary caregiver, 67% reported caring for a parent.
Table 1.
| Table 1(a) Descriptives and correlations for caregivers (N = 30). SD: standard deviation. | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Min/Max | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| 1. Education | 2.7 (1.4) | 1 / 5 | - | .32 | .21 | .13 | .13 | −.02 | −.10 | −.02 | .11 |
| 2. Age (in years) | 58.2 (8.3) | 43 / 73 | - | −.01 | .12 | −.08 | −.29 | .16 | .04 | −.28 | |
| 3. Duration of care | 60.1 (54.4) | 7 / 216 | - | −.27 | −.39+ | −.04 | .20 | .30 | −.05 | ||
| 4. RCOPE | 25.4 (3.5) | 15 / 30 | - | .83* | −.62* | −.50* | −.31 | .35 | |||
| 5. Positive RCOPE | 11.9 (2.7) | 6 / 15 | - | −.09 | −.53* | −.48* | .40+ | ||||
| 6. Negative RCOPE | 1.4 (1.9) | 0 / 7 | - | .16 | −.09 | −.11 | |||||
| 7. RMBPC | 38.2 (15.2) | 6 / 70 | - | .07 | −.02 | ||||||
| 8. ADL | 11.2 (3.8) | 6 / 18 | - | −.24 | |||||||
| 9. Mean cortisol slope | −24.7 (8.9) | −42 / −10 | - | ||||||||
| Table 1(b) Descriptives and correlations for non-caregivers (N = 48). SD: standard deviation. | ||||||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Min/ Max | 1 | 2 | 3 | 4 | 5 | 6 | |
| 1. Education | 2.7 (1.6) | 1 /5 | - | −.59* | −.46* | −.35* | −.03 | .01 |
| 2. Age (in years) | 59.6 (10.7) | 43 / 83 | - | .37* | .29+ | .01 | −.17 | |
| 3. RCOPE | 24.1 (3.8) | 14 / 30 | - | .90* | .02 | −.10 | ||
| 4. Positive RCOPE | 10.6 (3.6) | 1 / 15 | - | .24 | .03 | |||
| 5. Negative RCOPE | 1.2 (1.2) | 0 / 4 | - | .26 | ||||
| 6. Mean cortisol slope | −25.8 (9.1) | −46 / −9 | - | |||||
Note: RCOPE = Religious coping; RMBPC = Revised memory and behavior problems; ADL = Activities of daily living.
Note: For education level, 1 = high school degree or less, 2 = some college, 3 = BA/BS degree, 4 = Master's degree or equivalent, 5 = post-Master's degree.
p < 0.01.
p < 0.05.
Note: Independent samples t-tests (two-tailed) for each variable by caregiver status showed that all p-values had a p > 0.09.
Note: The df = 76 for all t-tests except mean cortisol slope score (df = 68).
For caregivers, higher RCOPE was correlated with higher positive RCOPE scores but lower negative RCOPE and RMBPC scores. Higher positive RCOPE was unexpectedly correlated with higher cortisol slope scores, but shorter duration of caregiving and lower ADL and RMBPC scores.
For non-caregivers, higher RCOPE scores were correlated with older age. Higher positive RCOPE was correlated with older age and higher RCOPE scores. Also, higher education levels were correlated with younger age, lower RCOPE and positive RCOPE scores. Of note, while higher RCOPE was correlated with lower negative RCOPE scores for caregivers it was not for non-caregivers [Fisher's z(diff) = 3.06; p = .0022].
Caregiver Status, Religious Coping, and Cortisol
Surprisingly, as shown in step three of Table 2, increasing RCOPE scores were associated with flatter cortisol slope scores (d = .49). Caregiver status was associated with marginally flatter but non-significant cortisol slope scores than non-caregiver status (see Tables 1a and 1b). The RCOPE by caregiver status interaction term was marginal but not significant (see Table 2). Unexpectedly, as shown in Figure 1, higher RCOPE scores were correlated with flatter cortisol slope scores for caregivers, but not for non-caregivers. However, the two correlation coefficients were not significantly different.
Table 2.
Regression of demographics, caregiver status and religious coping (RCOPE) scores on daily cortisol slope scores.
| Step 1 | Step 2 | Step 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| R2 | R2 change | Sig. F Change | Partial r | t(β) | p | Partial r | t(β) | p | Partial r | t(β) | p | |
|
| ||||||||||||
| Step 1: (df = 2, 67) | .008 | .008 | .776 | |||||||||
| RCOPE | .064 | .526 | .601 | .238 | 1.986 | .051 | .249 | 2.059 | .044 | |||
| Caregiver status | −.046 | −.377 | .707 | .221 | 1.839 | .070 | .223 | 1.830 | .072 | |||
|
| ||||||||||||
| Step 2: (df = 1, 66) | .060 | .052 | .060 | |||||||||
| RCOPE × Caregiver status | −.229 | −1.913 | .060 | −.228 | −1.872 | .066 | ||||||
|
| ||||||||||||
| Step 3: (df = 2, 64) | .114 | .054 | .149 | |||||||||
| Age | −.240 | −1.979 | .052 | |||||||||
| Education | −.127 | −1.021 | .311 | |||||||||
Note: β = standardized beta coefficient.
Note: Supplemental Univariate ANOVA tests were run to assess if the unexpected direction of the findings in the caregiver group could be explained by higher engagement in negative religious coping that happens to be accompanied by higher positive coping in the same persons. The results in general were consistent with those above for caregivers with any combination including high positive religious coping associated with significantly flatter cortisol slope scores than any combination with low positive religious coping [p(t) < .07].
Figure 1.
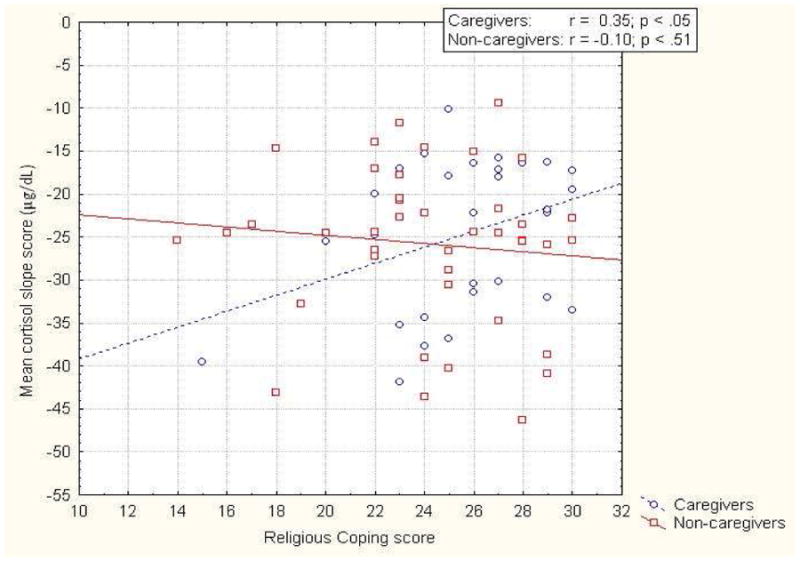
Correlation of religious coping score and mean diurnal cortisol slope score by caregiver status.
Note: Higher scores on religious coping indicate a strong belief and tendency by the caregiver to use spiritual or otherworldly forces to deal with life challenges.
Note: Fisher's z difference test for the two Religious coping and cortisol slope score correlation coefficents by caregiver status [Fisher's z(diff) = 1.83; p < .07].
As shown in Table 3(a), higher positive RCOPE scores were associated with flatter cortisol slope scores. The positive RCOPE by caregiver status interaction term was marginal but not significant in step two (see Table 3a). Unexpectedly, as shown in Figure 2(a), higher positive RCOPE scores predicted flatter cortisol slope scores for caregivers, but not for non-caregivers. However, the two correlation coefficients were not significantly different.
Table 3.
Regression of demographics, caregiver status and (A) positive and (B) negative religious coping (RCOPE) scores on daily cortisol slope scores.
| (A) | Step 1 | Step 2 | Step 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| R2 | R2 change | Sig. F Change | Partial r | t(β) | p | Partial r | t(β) | p | Partial r | t(β) | p | |
|
| ||||||||||||
| Step 1: (df = 2, 67) | .026 | .026 | .408 | |||||||||
| Positive RCOPE | .152 | 1.258 | .213 | .238 | 1.987 | .051 | .222 | 1.821 | .073 | |||
| Caregiver status | −.025 | −.208 | .836 | .195 | 1.616 | .111 | .176 | 1.431 | .157 | |||
|
| ||||||||||||
| Step 2: (df = 1, 66) | .069 | .042 | .089 | |||||||||
| Positive RCOPE × Caregiver status | −.208 | −1.727 | .089 | −.182 | −1.482 | .143 | ||||||
|
| ||||||||||||
| Step 3: (df = 2, 64) | .117 | .048 | .183 | |||||||||
| Age | −.224 | −1.841 | .070 | |||||||||
| Education | −.087 | −.696 | .489 | |||||||||
|
| ||||||||||||
| (B) | Step 1 | Step 2 | Step 3 | |||||||||
|
| ||||||||||||
| R2 | R2 change | Sig. F Change | Partial r | t(β) | p | Partial r | t(β) | p | Partial r | t(β) | p | |
|
| ||||||||||||
| Step 1: (df = 2, 67) | .008 | .008 | .763 | |||||||||
| Negative RCOPE | .068 | .556 | .580 | −.168 | −1.388 | .170 | −.209 | −1.708 | .092 | |||
| Caregiver status | −.055 | −.451 | .653 | −.172 | −1.415 | .162 | −.186 | −1.513 | .135 | |||
|
| ||||||||||||
| Step 2: (df = 1, 66) | .048 | .040 | .100 | |||||||||
| Negative RCOPE × Caregiver status | .201 | 1.669 | .100 | .235 | 1.938 | .057 | ||||||
|
| ||||||||||||
| Step 3: (df = 2, 64) | .108 | .059 | .127 | |||||||||
| Age | −.244 | −2.012 | .048 | |||||||||
| Education | −.096 | −.774 | .442 | |||||||||
Note: β = standardized beta coefficient.
Figure 2.
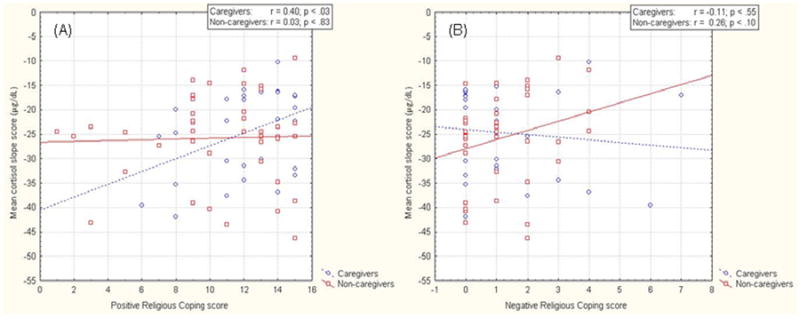
Correlation of A) positive and B) negative religious coping score and mean diurnal cortisol slope score by caregiver status for African-Americans.
Note: The Fisher's z difference test for the two Positive Religious coping and cortisol slope score correlation coefficents by caregiver status [Fisher's z(diff) = 1.55; p < .13].
Note: The Fisher's z difference test for the two Negative Religious coping and cortisol slope score correlation coefficents by caregiver status [Fisher's z(diff) = 1.48; p < .14].
Note: The Fisher's z difference test for the two caregiver and cortisol slope score correlation coefficents by Positive vs. Negative Religious coping [Fisher's z(diff) = 1.94; p < .06].
The negative RCOPE by caregiver status interaction term was marginal but not significant in step three (see Table 3b). Unexpectedly, as shown in Figure 2(b), higher negative RCOPE scores predicted marginally flatter negative cortisol slope scores for non-caregivers, but no changes for caregivers. However, the two correlation coefficients were not significantly different.
Notably, for caregivers, while cortisol slope scores increased significantly with increasing positive RCOPE scores they were mostly flat across negative RCOPE scores (see Figures 2a & 2b). In the RCOPE and negative RCOPE models, older age was linked with flatter cortisol slopes (see Tables 2 and 3b).
Religious Coping, Care Recipient Functional Status, and Cortisol
As shown in Table 4, higher RCOPE scores were linked with flatter cortisol slope scores in step one (d = .80) but a marginal decrease in cortisol slope scores in step three (d = 0.62). The RCOPE by RMBPC interaction term was significant in step three (d = 1.15) (see Table 4). Unexpectedly, as shown in Figure 3, higher RCOPE scores were linked with flatter cortisol slope scores at high (but not low) RMBPC levels. However, the two RMBPC correlation coefficients were not significantly different. In step three, higher RMBPC scores were surprisingly associated with more negative cortisol slope scores (d = 1.02).
Table 4.
Regression of demographics, revised memory and behavior problems (RMBPC) score and religious coping (RCOPE) scores on daily cortisol slope scores.
| Step 1 | Step 2 | Step 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| R2 | R2 change | Sig. F Change | Partial r | t(β) | p | Partial r | t(β) | p | Partial r | t(β) | p | |
|
| ||||||||||||
| Step 1: (df = 2, 26) | .152 | .152 | .118 | |||||||||
| RCOPE | .389 | 2.150 | .041 | −.109 | −.551 | .587 | −.388 | −1.930 | .067 | |||
| RMBPC | .173 | .900 | .377 | −.255 | −1.320 | .199 | −.513 | −2.741 | .012 | |||
|
| ||||||||||||
| Step 2: (df = 1, 25) | .219 | .068 | .153 | |||||||||
| RCOPE × RMBPC | .283 | 1.473 | .153 | .558 | 3.085 | .006 | ||||||
|
| ||||||||||||
| Step 3: (df = 4, 21) | .628 | .409 | .003 | |||||||||
| Age | −.323 | −1.563 | .133 | |||||||||
| Education | .039 | .180 | .859 | |||||||||
| Primary caregiver? | .628 | 3.697 | .001 | |||||||||
| Duration of care | −.260 | −1.233 | .231 | |||||||||
Note: β = standardized beta coefficient.
Figure 3.
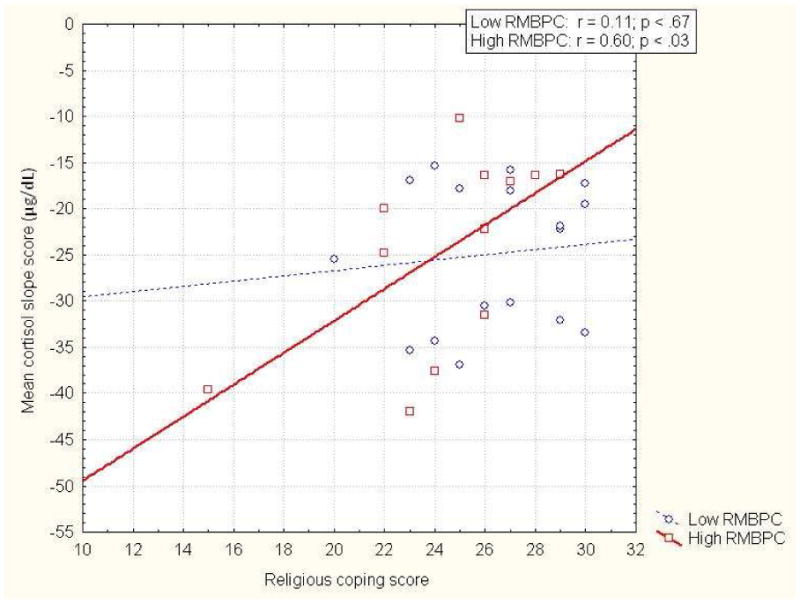
Correlation of religious coping score and mean diurnal cortisol slope score by dichotomized revised memory and behavioral problems checklist (RMBPC) score for African-American caregivers.
Note: High RMBPC levels represent increased care recipient behavioral problems.
Note: The Fisher's z difference test for the two Religious coping and cortisol slope score correlation coefficents by by RMBPC level [Fisher's z(diff) = 1.36; p < .18].
Surprisingly, as shown in step one of Table 5(a), increasing positive RCOPE scores were associated with flatter cortisol slope scores (d = .97). The positive RCOPE by RMBPC interaction term was significant in step three (d = .85) (see Table 5a). Unexpectedly, as shown in Figure 4(a), higher positive RCOPE scores were linked with flatter cortisol slope scores at high (but not low) RMBPC levels. However, the two RMBPC correlation coefficients were not significantly different.
Table 5.
Regression of demographics, revised memory and behavior problems (RMBPC) score and (A) positive and (B) negative religious coping (RCOPE) scores on daily cortisol slope scores. Note: β = standardized beta coefficient.
| (A) | Step 1 | Step 2 | Step 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| R2 | R2 change | Sig. F Change | Partial r | t(β) | p | Partial r | t(β) | p | Partial r | t(β) | p | |
|
| ||||||||||||
| Step 1: (df = 2, 26) | .209 | .209 | .047 | |||||||||
| Positive RCOPE | .457 | 2.622 | .014 | −.123 | −.618 | .542 | −.208 | −.976 | .340 | |||
| RMBPC | .237 | 1.246 | .224 | −.258 | −1.336 | .194 | −.345 | −1.683 | .107 | |||
|
| ||||||||||||
| Step 2: (df = 1, 25) | .287 | .078 | .112 | |||||||||
| Positive RCOPE × RMBPC | .313 | 1.649 | .112 | .445 | 2.278 | .033 | ||||||
|
| ||||||||||||
| Step 3: (df = 4, 21) | .623 | .336 | .007 | |||||||||
| Age | −.287 | −1.371 | .185 | |||||||||
| Education | −.080 | −.367 | .717 | |||||||||
| Primary caregiver? | .609 | 3.517 | .002 | |||||||||
| Duration of care | −.043 | −.196 | .847 | |||||||||
|
| ||||||||||||
| (B) | Step 1 | Step 2 | Step 3 | |||||||||
|
| ||||||||||||
| R2 | R2 change | Sig. F Change | Partial r | t(β) | p | Partial r | t(β) | p | Partial r | t(β) | p | |
|
| ||||||||||||
| Step 1: (df = 2, 26) | .013 | .013 | .845 | |||||||||
| Negative RCOPE | −.112 | −.577 | .569 | .154 | .777 | .444 | .439 | 2.242 | .036 | |||
| RMBPC | −.005 | −.027 | .979 | .107 | .538 | .595 | .466 | 2.413 | .025 | |||
|
| ||||||||||||
| Step 2: (df = 1, 25) | .059 | .046 | .278 | |||||||||
| Negative RCOPE × RMBPC | −.216 | −1.108 | .278 | −.519 | −2.780 | .011 | ||||||
|
| ||||||||||||
| Step 3: (df = 4, 21) | .533 | .474 | .004 | |||||||||
| Age | −.274 | −1.304 | .206 | |||||||||
| Education | .129 | .596 | .557 | |||||||||
| Primary caregiver? | .627 | 3.688 | .001 | |||||||||
| Duration of care | −.346 | −1.689 | .106 | |||||||||
Figure 4.
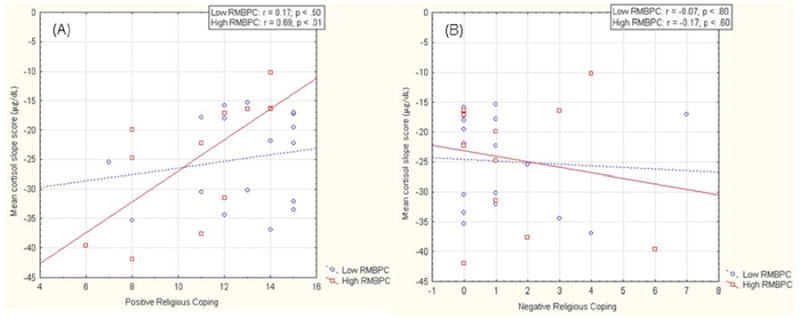
Correlation of A) positive and B) negative religious coping score and mean diurnal cortisol slope by dichotomized revised memory and behavioral problems checklist RMBPC score for African-American (AA) caregivers.
Note: The Fisher's z difference test for the two Positive Religious coping and cortisol slope score correlation coefficents by RMBPC level [Fisher's z(diff) = 1.58; p < .12].
Note: The Fisher's z difference test for the two Negative Religious coping and cortisol slope score correlation coefficents by RMBPC level [Fisher's z(diff) = 0.24; p < .82].
Note: At high RMBPC level, the Fisher's z difference test for the two Religious coping (Positive vs. Negative) and cortisol slope score correlation coefficents [Fisher's z(diff) = 2.16; p < .04].
As shown in step three of Table 5(b), increasing negative RCOPE (d = .83) and RMBPC (d = .90) scores were each associated with flatter cortisol slope scores. The negative RCOPE by RMBPC interaction term was significant in step three (d = 1.03) (see Table 5b); although there were no significant trends in cortisol slope scores by negative RCOPE and RMBPC level (see Figure 4b). However, increasing positive (but not negative) RCOPE scores were associated with increasingly flatter cortisol slope scores at high RMBPC levels (see Figures 4a & 4b). In each model primary caregiver status was linked with more negative cortisol slope scores (Mean = − 28.63 ± 8.86) than secondary caregiver status (Mean = − 19.21 ± 5.40).
Unlike RMBPC, ADL did not moderate the role of RCOPE measures in cortisol slope scores. Neither of the ADL [t(27) = − .73; p < .41], RCOPE [t(27) = .66; p < .51], or ADL by RCOPE [t(27) = − .44; p < .66] effects was significant. As well, neither of the positive RCOPE [t(27) = 1.75; p < .09], ADL by positive RCOPE [t(27) = − .62; p < .54], negative RCOPE [t(27) = − .55; p < .54] or ADL by negative RCOPE [t(27) = − 1.05; p < .30] effects was significant.
Conclusions
Surprisingly, positive (but not negative) RCOPE was associated with increasingly flatter cortisol slope scores for caregivers (but not non-caregivers). Thus, there is something about positive RCOPE that is linked with riskier cortisol responses for caregivers. Why? Perhaps the unique challenges of ADRD caregiving for AA caregivers require a wider range RCOPE that entails more negative religious appraisals. Overly optimistic appraisals may be discordant with some stressful aspects of ADRD caregiving.
That said the finding that positively religious AA caregivers who scored high (vs. low) on care recipient problems showed flatter cortisol slopes suggests taking a more optimistic religious perspective surprisingly appears counterproductive stress-wise for overwhelmed caregivers. Why? Perhaps an overly optimistic religious approach is discordant with the overwhelming burden and negativity that high RMBPC caregivers manage on a daily basis. It may be illogical and anxiety-provoking to invest positive religious appraisals (e.g., “everything will be fine”) when one's care recipient is having severe issues that require a wide range of emotion-focused coping strategies. Thus, inclusion of the more negative approach may be a better match for the unusually high demands that high RMBPC caregivers must overcome and may prompt more immediate conflict resolution efforts.
Overall the results suggest that 1) traditional linear models of religion in health have limitations, 2) RCOPE and health is not one size fits all for AAs and 3) religious AAs with demanding care recipients may not have complementary coping resources that religious Whites may have. Relevant coping resources (e.g., social support) may protect one from the acute side effects of caregiver stress. Given the refuge of religious institutions for those under distress (9), AAs at disproportionately high health risk are likely to score higher on RCOPE. Thus, the critical question becomes: Is the ethnic disparity found in cortisol responses a product of unique (and potentially adverse) forms of RCOPE or unique health risks among highly religious AAs? Along these lines, Kosberg et al. (19) found that AA caregivers scored higher on religious and denial coping than White caregivers suggesting that highly religious AA caregivers may indeed be using less effective coping methods to deal with daily stressors.
Also, the literature commonly interprets RCOPE responses as more stable behaviors (9, 11). However, causality is a persistent issue in the study of religion and health. Thus, greater RCOPE among AA caregivers could be the result of those individuals having worse functioning patients and are thus pursuing religious orientation to better cope with those demands.
Additionally, AAs experience higher psychosocial stress than Whites (37). Daily stressors such as perceived discrimination and economic insecurity have excessively negative health effects for AA versus White caregivers (4). Since AA adults show worse health status at each stage of adulthood than their White counterparts (37-39) the former group may be especially vulnerable to the perils of caregiver stress. For instance, young AA adults show flatter daily cortisol slopes than their White counterparts (35).
A few limitations of the study include the lack of White caregivers, a scarcity of wide-ranging measures of daily HPA response, and the need for more comprehensive measurement of religious and spiritual coping with ADRD caregivers. White caregivers will be added in future longitudinal studies including a wider range of psychosocial measures. Given other potential confounding variables that may sway daily HPA responses we plan to add assessments such as specific psychological measures (e.g., active coping, neuroticism, hope, and bias in caregiver ratings, 40), blood chemistry, and health behaviors.
Overall, these findings suggest that the role of RCOPE in daily physiological stress response in AA caregivers is contingent on contextual influences and the positivity of RCOPE. For AA female caregivers with taxing care recipient problems, optimizing RCOPE may reduce risk for chronically dysregulated HPA responses. Future studies will focus on relevant coping skills interventions that consider religious support resources for burdened AA caregivers.
Acknowledgments
We would like to acknowledge the ADRC/NIA for awarding grant #AG08012 to T. J. McCallum, Ph.D., through the University Memory and Aging Center of University Hospitals and Case Western Reserve University. We also acknowledge partial grant support from the NIH (M01 RR000080) to the General Clinical Research Center of University Hospitals.
The authors show appreciation to the staff of the General Clinical Research Center of University Hospitals for helpful consultation and aid in completing salivary cortisol assays.
Footnotes
No Disclosures to Report
Poster presented at the American Psychosomatic Society meeting in Portland, OR (March 2010).
Contributor Information
Marcellus M. Merritt, Department of Psychology & Center on Age and Community, University of Wisconsin Milwaukee, Box 413, Milwaukee, WI 53201, merrittm@uwm.edu, Phone: 414-229-6145, Fax: 414-229-5219
T. J. McCallum, Department of Psychological Sciences, Case Western Reserve University
References
- 1.Alzheimer's Association National Alliance for Caregiving. Families Care: Alzheimer's Caregiving in the United States. Chicago, IL: Alzheimer's Association and Bethesda National Alliance for Caregiving; 2004. [Google Scholar]
- 2.de Vugt ME, Nicolson NA, Aalten P, et al. Behavioral problems in dementia patients and salivary cortisol patterns in caregivers. J Neuropsychiatry Clin Neurosci. 2005;17:201–207. doi: 10.1176/jnp.17.2.201. [DOI] [PubMed] [Google Scholar]
- 3.Dilworth-Anderson P, Goodwin PY, Williams SW. Can culture help explain the physical health effects of caregiving over time among African American caregivers? J Gerontol B Psychol Sci Soc Sci. 2004;59:S138–S145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- 4.Gallagher-Thompson D, Shurgot GR, Rider K, et al. Ethnicity, stress, and cortisol function in Hispanic and non-Hispanic white women: A preliminary study of family dementia caregivers and noncaregivers. Am J Geriatr Psychiatry. 2006;14:334–342. doi: 10.1097/01.JGP.0000206485.73618.87. [DOI] [PubMed] [Google Scholar]
- 5.Liptzin B, Tuis J. Biomarkers in geriatric psychiatry: The promise and the reality. Am J Geriatr Psychiatry. 2011;19:759–762. doi: 10.1097/JGP.0b013e31822bec2c. [DOI] [PubMed] [Google Scholar]
- 6.McCallum TJ, Sorocco KH, Fritsch T. Mental health and diurnal salivary cortisol patterns among African American and European American female dementia family caregivers. Am J Geriatr Psychiatry. 2006;14:684–693. doi: 10.1097/01.JGP.0000225109.85406.89. [DOI] [PubMed] [Google Scholar]
- 7.Schulz R, Beach SR, Hebert RS, et al. Spousal suffering and partner's depression and cardiovascular disease: the Cardiovascular Health Study. Am J Geriatr Psychiatry. 2009;17:246–254. doi: 10.1097/JGP.0b013e318198775b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wahbeh H, Kishiyama SS, Zajdel D, et al. Salivary cortisol awakening response in mild Alzheimer disease, caregivers, and noncaregivers. Alzheimers Dis Assoc Disord. 2008;22:181–183. doi: 10.1097/WAD.0b013e31815a9dff. [DOI] [PubMed] [Google Scholar]
- 9.Krause N. The social milieu of the church and religious coping responses: A longitudinal investigation of older whites and older Blacks. Int J Psychol Relig. 2010;20:109–129. doi: 10.1080/10508611003608007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stolley JM, Buckwalter KC, Koenig HG. Prayer and religious coping for caregivers of persons with Alzheimer's disease and related disorders. Am J Alzheimers Dis Other Dementias. 1999;14:181–191. [Google Scholar]
- 11.Levin JS. Religion and health: is there an association, is it valid, and is it causal? Soc Sci Med. 1994;38:1475–1482. doi: 10.1016/0277-9536(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 12.O'Connell C, Edwards C, Pearce M, et al. Religious coping and pain associated with Sickle cell disease: Exploration of a non-linear model. J African Am Stud. 2009;13:1–13. [Google Scholar]
- 13.Haley C, Koenig H, Bruchett B. Relationship between private religious activity and physical functioning in older adults. J Relig Health. 2001;40:305–312. [Google Scholar]
- 14.Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;4:56. 519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Haley WE, Gitlin LN, Wisniewski SR, et al. Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: findings from the REACH study. Aging Ment Health. 2004;8:316–329. doi: 10.1080/13607860410001728998. [DOI] [PubMed] [Google Scholar]
- 16.Hebert RS, Dang Q, Schulz R. Religious beliefs and practices are associated with better mental health in family caregivers of patients with dementia: findings from the REACH study. Am J Geriatr Psychiatry. 2007;15:292–300. doi: 10.1097/01.JGP.0000247160.11769.ab. [DOI] [PubMed] [Google Scholar]
- 17.Jones-Cannon S, Davis BL. Coping among African-American daughters caring for aging parents. ABNF J. 2005;16:118–123. [PubMed] [Google Scholar]
- 18.Leblanc AJ, Driscoll AK, Pearlin LI. Religiosity and the expansion of caregiver stress. Aging Ment Health. 2004;8:410–421. doi: 10.1080/13607860410001724992. [DOI] [PubMed] [Google Scholar]
- 19.Kosberg JI, Kaufman AV, Burgio LD, et al. Family caregiving to those with dementia in rural Alabama: racial similarities and differences. J Aging Health. 2007;19:3–21. doi: 10.1177/0898264306293604. [DOI] [PubMed] [Google Scholar]
- 20.Morano CL, King D. Religiosity as a mediator of caregiver well-being: Does ethnicity make a difference? J Gerontol Soc Work. 2005;45:69–84. doi: 10.1300/J083v45n01_05. [DOI] [PubMed] [Google Scholar]
- 21.Picot SJ, Debanne SM, Namazi KH, et al. Religiosity and perceived rewards of Black and White caregivers. Gerontologist. 1997;37:89–101. doi: 10.1093/geront/37.1.89. [DOI] [PubMed] [Google Scholar]
- 22.Toth-Cohen S. Factors influencing appraisal of upset in black caregivers of persons with Alzheimer disease and related dementias. Alzheimer Dis Assoc Disord. 2004;18:247–255. [PubMed] [Google Scholar]
- 23.Roth DL, Burgio LD, Gitlin LN, et al. Psychometric analysis of the Revised Memory and Behavior Problems Checklist: factor structure of occurrence and reaction ratings. Psychol Aging. 2003;18:906–915. doi: 10.1037/0882-7974.18.4.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Gaugler JE, Wall MM, Kane RL, et al. Does caregiver burden mediate the effects of behavioral disturbances on nursing home admission? Am J Geriatr Psychiatry. 2011;19:497–506. doi: 10.1097/JGP.0b013e31820d92cc. [DOI] [PubMed] [Google Scholar]
- 26.Mausbach BT, Aschbacher K, Patterson TL, et al. Avoidant coping partially mediates the relationship between patient problem behaviors and depressive symptoms in spousal caregivers. Am J Geriatr Psychiatry. 2006;14:299–306. doi: 10.1097/01.JGP.0000192492.88920.08. [DOI] [PubMed] [Google Scholar]
- 27.Carey EC, Walter LC, Lindquist K, et al. Development and validation of a functional morbidity index to predict mortality in community-dwelling elders. J Gen Intern Med. 2004;19:1027–1033. doi: 10.1111/j.1525-1497.2004.40016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joling KJ, van Hout HPJ, Schellevis FG, et al. Incidence of depression and anxiety in the spouses of patients with dementia: A naturalistic cohort study of recorded morbidity with a 6-year follow-up. Am J Geriatr Psychiatry. 2010;18:146–153. doi: 10.1097/JGP.0b013e3181bf9f0f. [DOI] [PubMed] [Google Scholar]
- 29.Onder G, Finne-Soveri H, Soldato M, et al. Distress of caregivers of older adults receiving home care in European countries: results from the AgeD in Home Care Study. Am J Geriatr Psychiatry. 2009;17:899–906. doi: 10.1097/JGP.0b013e3181b4beef. [DOI] [PubMed] [Google Scholar]
- 30.Merritt MM, McCallum TJ, Fritsch T. How much striving is too much? John Henryism active coping predicts worse daily cortisol responses for African American but not White female dementia family caregivers. Am J Geriatr Psychiatry. 2011;19:451–460. doi: 10.1097/JGP.0b013e3181eaffa4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 1999;61:197–204. doi: 10.1097/00006842-199903000-00012. [DOI] [PubMed] [Google Scholar]
- 32.McCallum T, Arlien C. Enhancing the matching model of recruitment with focus groups. Aging Ment Health. 2006;10:312–318. doi: 10.1080/13607860500409781. [DOI] [PubMed] [Google Scholar]
- 33.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 34.Teri L, Truax P, Logsdon RG, et al. Assessment of behavioural problems in dementia: The revised memory and behavior problems checklist. Psychol Aging. 1992;7:622–631. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- 35.Cohen S, Schwartz JE, Epel E, et al. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med. 2006;68:41–50. doi: 10.1097/01.psy.0000195967.51768.ea. [DOI] [PubMed] [Google Scholar]
- 36.Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- 37.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. Am J Public Health. 2008;98:S29–S37. doi: 10.2105/ajph.98.supplement_1.s29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cooper C, Tandy AR, Balamurali TB, et al. A systematic review and meta-analysis of ethnic differences in use of dementia treatment, care, and research. Am J Geriatr Psychiatry. 2010;18:193–203. doi: 10.1097/JGP.0b013e3181bf9caf. [DOI] [PubMed] [Google Scholar]
- 39.Conner KO, Copeland VC, Grote NK, et al. Mental health treatment seeking among older adults with depression: The impact of stigma and race. Am J Geriatr Psychiatry. 2010;18:531–543. doi: 10.1097/JGP.0b013e3181cc0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schulz R, Cook TB, Beach SR, et al. Magnitude and causes of bias among family caregivers rating Alzheimer disease patients. Am J Geriatr Psychiatry. doi: 10.1016/j.jagp.2012.10.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]


