Abstract
Background
Diabetes self-management education has an important role in diabetes management. The efficacy of education has been proven in several randomized trials. However, the status of diabetes education programs in real Korean clinical practice has not yet been evaluated in terms of patient compliance with the education prescription.
Methods
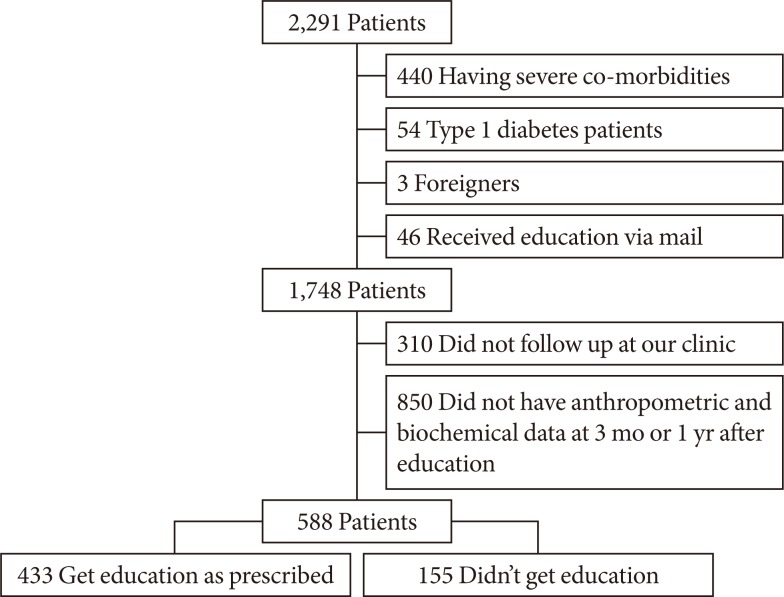
We retrospectively analyzed clinical and laboratory data from all patients who were ordered to undergo diabetes education during 2009 at Samsung Medical Center, Seoul, Korea (n=2,291). After excluding ineligible subjects, 588 patients were included in the analysis.
Results
Among the 588 patients, 433 received education. The overall compliance rate was 73.6%, which was significantly higher in the subjects with a short duration or living in a rural area compared to those with a long duration (85.0% vs. 65.1%, respectively; P<0.001) or living in an urban area (78.2% vs. 70.4%, respectively; P=0.037). The hemoglobin A1c decreased greater in the compliant group (from 7.84±1.54 at baseline to 6.79±1.06 at 3 months and 6.97±1.20 at 12 months after prescription in the compliant group vs. from 7.74±1.25 to 7.14±1.02 and 7.24±1.24 in the non-compliant group; P=0.001). The decrease in hemoglobin A1c was greater in the subjects with a short duration (P=0.032).
Conclusion
In our study a large percent of patients refuse to get education despite having a prescription from their physician. This refusal rate was higher in the patients with long-standing diabetes or in urban residence. Furthermore, education was more effective in patients with a short duration of diabetes in clinical practice.
Keywords: Diabetes mellitus, type 2; Education; Self care
INTRODUCTION
National survey data indicate that the increasing prevalence of diabetes is a global health problem that is causing a socioeconomic burden. The prevalence and incidence of diabetes has also been increasing in Korea [1]. The rising prevalence of diabetes mellitus is associated with increased socioeconomic burden due to the chronic complications of diabetes [2]. It is clear that the best way to delay the development of complications in any type of diabetes is intensive blood glucose control [3,4]. Maintenance of tight glycemic control is very difficult, and therefore there are several modalities to lower blood glucose level such as lifestyle modification, oral hypoglycemic agents and insulin. Among these, lifestyle modification via diabetes self-management education is recommended as a basic component of diabetes management in clinical practice [2]. Recently, it was demonstrated that diabetes education and self-management for newly diagnosed patients have better long-term clinical outcomes and cost effectiveness in the United Kingdom [5] and Korea [6]. Although education is such an important part of a treatment plan, there is a report that only 26.2% of elderly patients with diabetes have taken diabetes education classes in Korea. Since the subjects analyzed in the previous study were more than 65 years old, the ratio might not be true for the general population of patients with diabetes [7]. In another study to assess the epidemiologic characteristics of diabetes mellitus in Korea, using the Korean health insurance database, 60.6% of patients with diabetes did not receive an education [8]. In 2007, the status of diabetes education in Korea was assessed via survey using questionnaires from diabetes nurse educators who have diabetes educator certificates. It was reported that there are many education programs in Korea, and the investigator argued that we should make an effort to standardize and systematize the education programs [9]. However, diabetes education is not covered by the national medical insurance system in Korea. Furthermore, there have not been any reports on patient compliance with an education prescription in real clinical practice.
In the present study, we focused on the current status of diabetes education in real clinical practice in a tertiary hospital in Korea, and we tried to analyze the refusal rate of diabetes education prescription and the efficacy of diabetes education according to the compliance with the education prescription. Furthermore, we investigated which clinical parameters affect the efficacy of diabetes education.
METHODS
Participants
In this retrospective study, we reviewed the charts of all patients who were prescribed diabetes self management education (DSME) in the Samsung Medical Center from January to December 2009 (n=2,991). The DSME was ordered by the treating physician because of inadequate glycemic control and the patients' ignorance of the disease. DSME was provided by 2 or more instructors from the diabetes education center in Samsung Medical Center. The instructors in our center are diabetes educators certified by the Korean Diabetes Association. These educated and licensed healthcare professionals included registered nurses, registered dietitians, pharmacists, and doctors. A basic session consists of 1 hour of education about the concept of diabetes and 1 hour about diet management. Intensive education includes one more session on exercise education. Upon conclusion of the sessions, the educator provides written curriculum reflecting current evidence and practice guidelines with criteria for evaluating outcomes.
Demographic characteristics including sex, age, disease duration, height, weight, laboratory data, and the patients' residential districts were retrieved from an electronic medical chart. Medication adjustment after diabetes education was assessed by review of electronic medical records. Increment of medication was defined as the increased dose of medication, adding another kind of agent, new start of medication or change to another kind of agent. The compliant group consisted of subjects who underwent education after prescription, and the non-compliant group consisted of subjects who refused to undergo the education course after receiving an education prescription. To evaluate the effect of the patients' residential districts on the education efficacy and patient compliance, we divided the whole subjects into urban or rural groups. The urban group included subjects who lived in the metropolis of Seoul, or the Incheon, Daejeon, Gwangju, Daegu, Ulsan, and Busan megalopolises. And the rural group consisted of subjects who did not live in either a metropolis or megalopolis. The study protocol was approved by the Ethics Committee of Samsung Medical Center.
Statistical analysis
The data collected were analyzed using IBM SPSS Statistic version 19.0 for Windows (IBM Co., New York, NY, USA). A statistical analysis to compare baseline characteristics between the groups was conducted using the Student's t-test. Chi-square analyses or Fisher's exact tests were performed to compare the ratio between groups. A mixed model was used to compare the change in hemoglobin A1c and body mass index after an education prescription.
RESULTS
Compliance with DSME prescription
The overall compliance rate for the education prescription during 2009 was 64.0% (1,467/2,291). From among 2,291 subjects, we included 588 patients who had their anthropometric and biochemical data checked 3 months after education and 1 year after education, in order to analyze the education efficacy (Fig. 1). After the exclusion of ineligible subjects, the compliance rate increased to 73.6% (433/588). The subjects who received education as ordered by their physician had a significantly higher rate of regular follow-up and execution of their laboratory checkup compared to the subjects who did not receive education. Among the 1,124 subjects who received the education, 433 subjects executed the laboratory checkup at 3 months and 12 months after the education prescription. On the other hand, there were only 155 subjects who completed the laboratory checkup among the 624 non-compliant subjects (P<0.001). There was a significant difference in the obedience rate between subjects in the urban group and rural group (70.4% [243/345] vs. 78.2% [190/243], respectively; P=0.037).
Fig. 1.
Enrollment of patients and the study design. Data represent the number of patients.
Change in hemoglobin A1c after receiving education
The baseline characteristics of the 588 subjects divided into two groups according to their compliance are shown in Table 1. There were no significant differences between the two groups for sex, age, body mass index, blood pressure, fasting blood glucose, and hemoglobin A1c. Medication adjustment after education prescription was not significantly different between the receiver of education and repudiator. In the compliant group, the medication was increased in 65.5% (284/433). In the non-compliant group, the medication was increased in 70.3% (109/155) (P=0.283). However, the duration of diabetes was significantly shorter in the compliant group compared to the non-compliant group (5.76±7.41 years vs. 7.14±7.29 years; P=0.002), and there were more rural residents in the compliant group (34.2% [53/155] in non-compliant group vs. 43.9% [190/433] in compliant group, P=0.037).
Table 1.
Baseline characteristics according to compliance
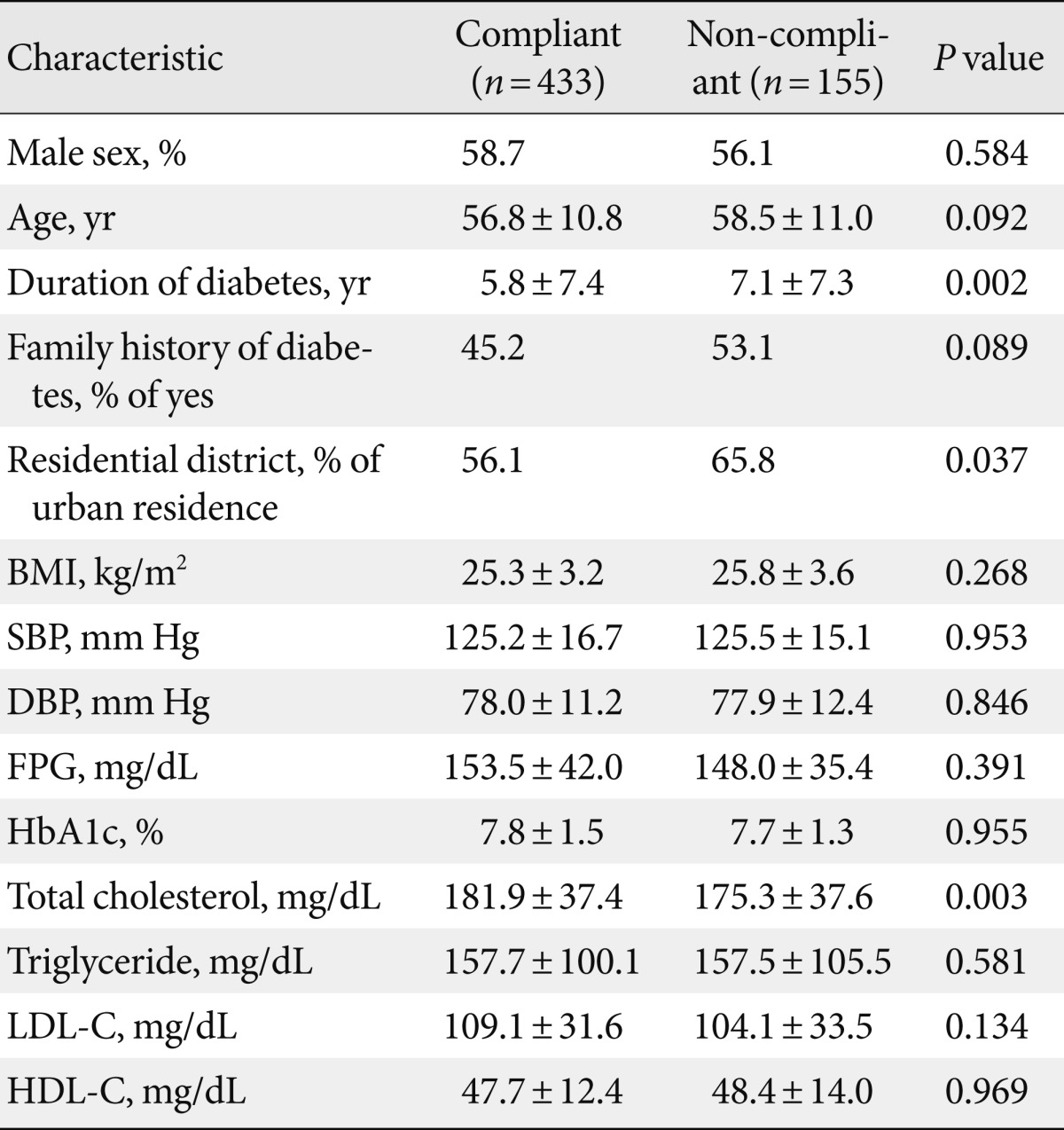
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
In both groups, hemoglobin A1c decreased significantly after an education prescription, regardless of compliance with the education prescription (from 7.74±1.25 at baseline to 7.14±1.02 at 3 months and 7.24±1.24 at 12 months after education in non-compliant group vs. from 7.84±1.54 at baseline to 6.79±1.06 at 3 months and 6.97±1.20 at 12 month after education), however the decrement was much bigger in the subjects who received education as prescribed. In addition, the hemoglobin A1c level was significantly lower in the educated subjects at 3 months and 1 year after the education session.
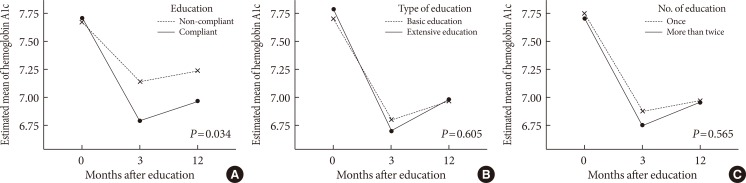
The hemoglobin A1c change after education was significantly different between the two groups after adjusting for age, sex, duration of diabetes, and the patients' residential districts (P=0.034). This difference between the compliance group and non-compliance group was also significant at 3 months after the education prescription (P=0.003) and 1 year after the education prescription (P=0.031) (Fig. 2A).
Fig. 2.
Change in hemoglobin A1c levels over 1 year after education prescription. (A) Differences in hemoglobin A1c change according to the education completion (P=0.0013). The continuous line refers to the subjects who obeyed the physicians' prescription to get the education. The dotted line refers to the subjects who refused to get the education in spite of their physicians' prescription. (B) The change in hemoglobin A1c levels according to type of education after education prescription (P=0.605). (C) The hemoglobin A1c change according to number of years after education (P=0.565).
The subjects who were more recently diagnosed with diabetes showed more compliance with the education and medication prescription, which can intensify the effect of the education. Therefore, we compared the ratio of newly diagnosed diabetes patient. The rate was 3.9% [6/155] in the non-compliant group, and 8.8% [38/433] in the compliant group (P=0.050). We reanalyzed the data after excluding the 44 subjects with newly developed diabetes, and the mode of hemoglobin A1c change after education prescription did not differ between the compliant subjects and the non-compliant subjects (P=0.127). However, hemoglobin A1c reduction after education prescription was significantly greater in the compliant group (0.57±1.13 vs. 0.98±1.42 at 3 months after the education prescription and 0.49±1.24 vs. 0.81±1.50 at 1 year after prescription; P=0.001 and P=0.020, respectively).
To evaluate the efficacy of extensive DSME, which includes exercise education, we divided the compliant group into two groups (basic and extensive), and the baseline characteristics of the two groups are shown in Table 2. The age at the time of DSME prescription and the duration of diabetes were significantly different between the two groups.
Table 2.
Baseline characteristics according to type of education
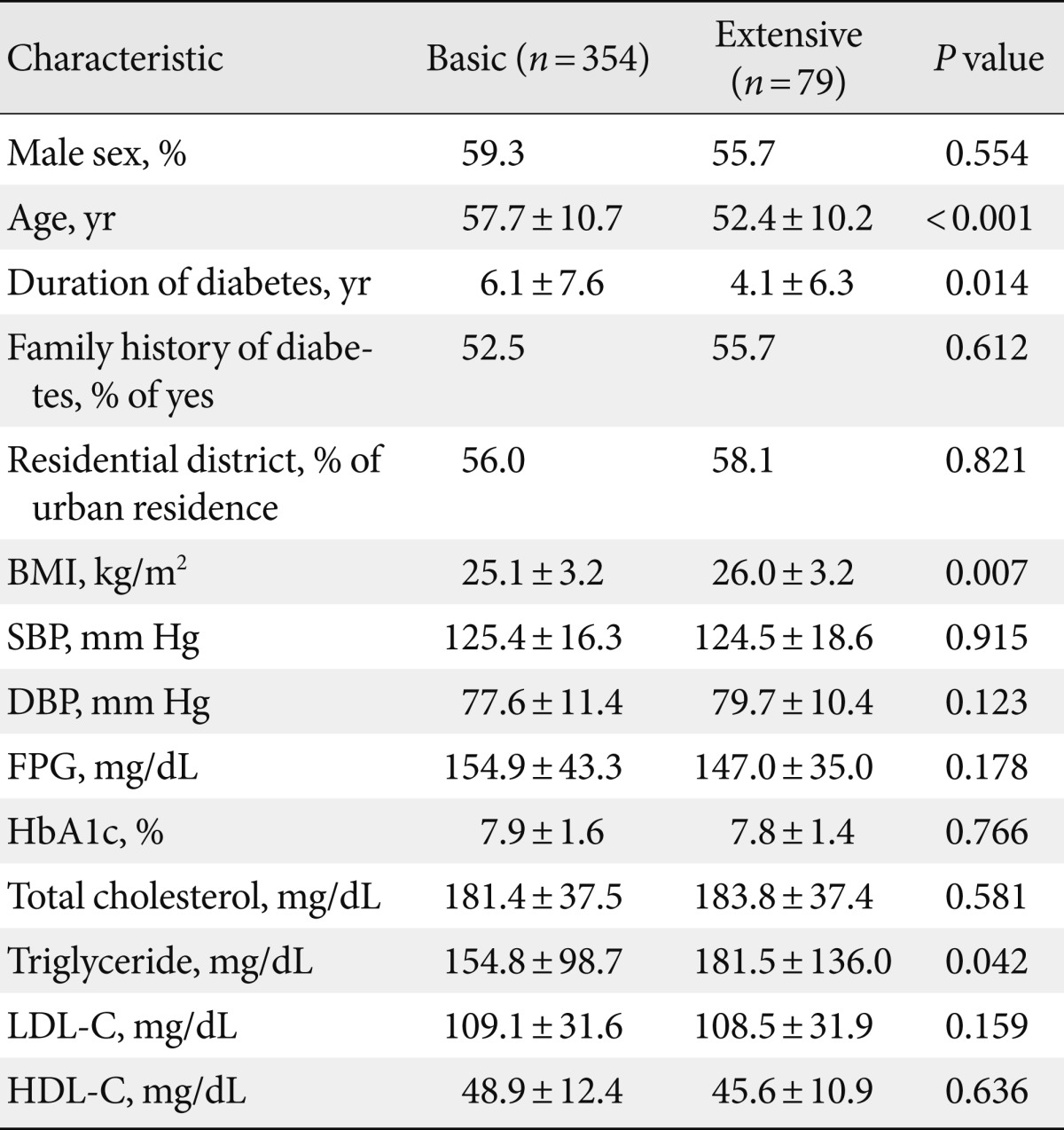
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
The hemoglobin A1c change in the basic education group was 7.86±1.57 before education, 6.82±1.07 at 3 months after education, and 6.97±1.19 at 12 months after education. In the extensive education group, the hemoglobin A1c change was 7.76±1.42 before education, 6.62±1.01 at 3 months after education, and 6.93±1.28 at 12 months after education (Fig. 2B). After adjustment for age and diabetes duration, the change in hemoglobin A1c between the basic group and the extensive group was compared. The hemoglobin A1c decrement between groups was not significantly different (P=0.501).
To evaluate the effect of follow-up education after the first DSME, we compared between the subjects who received the DSME once and the subjects who received the DSME more than twice. There were no significant differences between the two groups except for age and triglyceride level (Table 3). Follow-up education did not cause a significant difference in hemoglobin A1c levels after education, with adjustments for age and triglyceride levels (P=0.603) (Fig. 2C).
Table 3.
Baseline characteristics according to number of education sessions
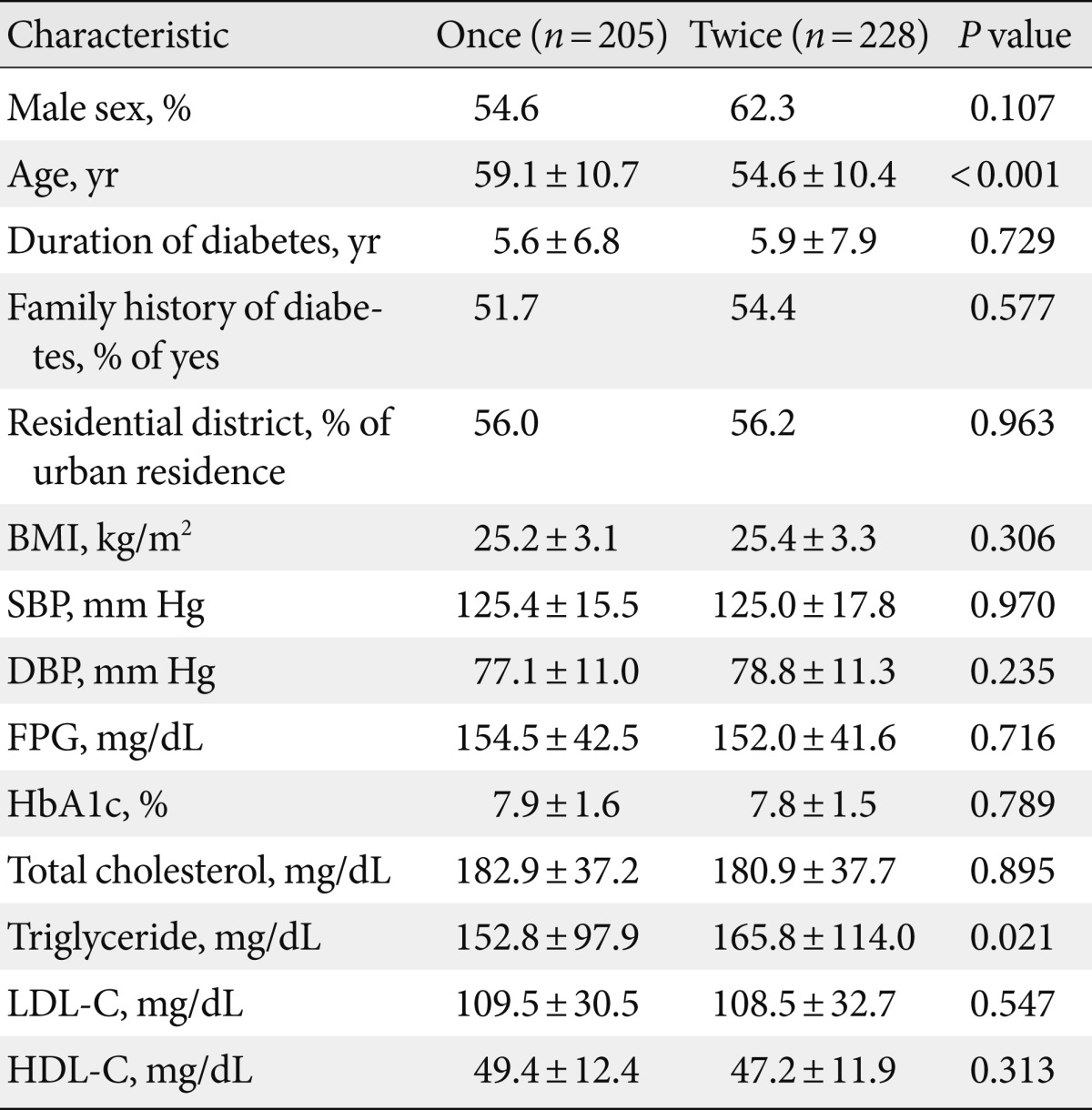
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
Subgroup analysis according to the duration of diabetes
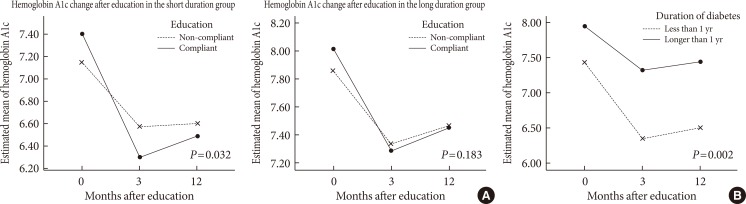
There was a significant difference in the percentage of patients with short duration of diabetes (less than 12 months) between the compliant and non-compliant groups (49.7% [215/433] vs. 22.6% [38/155], respectively; P<0.001). Because the duration of diabetes was associated with the compliance of education prescription, we divided the subjects into two groups. The first group consisted of the subjects with diabetes for less than 12 months (n=235), and the second group consisted of the subjects with diabetes for 12 months or more (n=335). The baseline characteristics of the four subgroups are shown in Table 4. The obedience rate was significantly higher in the short duration group compared with the other group (85.0% [215/253] vs. 65.1% [218/335]; P<0.001). Hemoglobin A1c level changes after education in both groups are summarized in Fig. 3. After education prescription, hemoglobin A1c decreased in every subgroup. The hemoglobin A1c change after education was compared between the compliant and non-compliant group in the subgroup of diabetes duration using a mixed model.
Table 4.
Baseline characteristics according to the duration of diabetes
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol.
Fig. 3.
(A) Differences in hemoglobin A1c change between the short duration group (P=0.032) and long duration group (P=0.183). (B) Change in hemoglobin A1c after education according to the duration of diabetes (P=0.002).
Compliance with the education prescription significantly decreased hemoglobin A1c in the short duration group (P=0.032), however there was no significant change in hemoglobin A1c in the long duration group (P=0.183) (Fig. 3A). In the 433 subjects who received the DSME, hemoglobin A1c change was compared between the groups divided according to diabetes duration. The analysis revealed that the decrement in hemoglobin A1c was more evident in the subjects with short duration (P=0.002) (Fig. 3B). In the subgroup of short diabetes duration, medication adjustment after education prescription was not significantly different between the receiver of education and education repudiator (58.7% [128/253] vs. 48.8% [20/48]; P=0.238). We also performed the subgroup analysis according to the patients' residential districts, because the compliance rate was different between the urban and rural groups. However, the hemoglobin A1c decrement after education was not different between the two groups (P=0.932).
Body weight and lipid profile change after education was evaluated in the same way as hemoglobin A1c, and neither was significantly different between the compliant and non-compliant groups (data not shown).
DISCUSSION
This study was performed to investigate the rate of compliance with education prescription and to analyze the effect of diabetes education. To assess the education compliance rate, we divided the enrolled subjects into two groups. The first group included patients who finished their education as ordered and the other included patients who refused to undergo the education session even though their physician prescribed DSME. To investigate the effect of completing diabetes education, we compared two patient groups after education prescription, with an adjustment for diabetes duration.
The effectiveness and importance of diabetes education has been evaluated several times in Korea [10] and worldwide [11] and the results of a metaanalysis have already shown that education has beneficial effects in terms of improving glycemic control, weight, and lipid profiles [12]. Therefore, diabetes education has been regarded as a key component of diabetes management for a long time [2], and its importance has been growing. As a result, authorities have suggested that there should be national standards for DSME [13]. Moreover, it has been reported that the education of patients with a shorter duration of diabetes resulted in a better long-term clinical outcome and cost-effectiveness in the United Kingdom [5] and higher adherence to self-care activities and better glycemic control in Korea [6]. On the other hand, diabetes education has not been evaluated recently, especially with a focus on compliance with an education prescription in clinical practice.
In 2009, there were more than 2,000 patients who were ordered to get DSME in our center. Among the patients who were prescribed to receive education, the proportion of patients who received education was 64.0%. Interestingly, the proportion of patients who received education was lower in megalopolis locations. Although we could not assess the reasons why about 36.0% of the patients refused to undergo diabetes education in this study, we can assume that it was caused by a lack of comprehension about the importance of DSME or due to economic problems of the patients [14], because education is not covered by national health insurance in Korea. There have been two descriptive studies in Korea which have mentions about the percent of the patients who had ever had the opportunity to get diabetes education among the whole diabetic patients. In those studies, it was reported that only 26.2% or 39.4% of the patients with diabetes had attended diabetes education classes [8,9]. In those two reports, it was unclear whether diabetes education had been recommended to the subjects who had not received an education. In our study 36.0% of the patients refused to attend a class of DSME even though their treating physician prescribed and recommended the education. These findings suggest that a low DSME education rate in the Korean diabetic population might be explained partially by the patients' refusal to get the education. Moreover, we found that educated subjects tended to revisit the clinic regularly and showed better adherence to the evaluation plan. The percentage of regular clinic visits in the compliant group was 38.5%, while it was only 24.8% in the non-compliant group (P<0.001). Therefore, treating physicians should encourage their patients to undergo DSME.
Between the compliant and non-compliant group, there was a significant difference in the duration of diabetes. To adjust for the effect of diabetes duration, we divided the subjects according to the duration of diabetes. This adjustment revealed that compliance with the education prescription in patients with diabetes for more than 1 year failed to show a significant improvement in hemoglobin A1c compared with patients who ignored the education prescription. The results of the present study correspond well with those of an earlier report from the U.K. The Prospective Diabetes Study (UKPDS) suggested that glycemic control rates among individuals with diabetes decreases with disease duration [15].
Our study had some limitations. It was a retrospective non-randomized study, so there are several confounding factors for which we cannot adjust. Client education can enhance medication compliance, but medication compliance cannot be assessed in this study, so better glycemic control was caused by better medication compliance in the educated group. Moreover, the patients who did not undergo the education might have a tendency to ignore other recommendations from their doctor; therefore those tendencies might enhance the positive effect of completing the education. Another problem is that we failed to show the efficacy of either intensive education or follow-up education. It has been reported that the type of education can cause differences in diabetes control [16]. This discrepancy should be reevaluated in a larger study. Finally, the results of this study are limited to a single center experience.
In this study we found a number of patients refused to receive the DSME in spite of the education being prescribed by their physician. The refusal rate was higher in the patients with longstanding diabetes and urban residence. However, there should be further investigation into the factors affecting the patients' compliance such as academic educational status, socioeconomic status, and cost of education. We also found that earlier education is more effective in real clinical practice. After DSME prescription, educated subjects were more likely to have a change in hemoglobin A1c compared to the subjects who refused to get the education. Since the duration of diabetes was significantly shorter in subjects who followed their physicians' order to get the education, a tendency of hemoglobin A1c decrement was reanalyzed with an adjustment for the duration of diabetes. These beneficial effects on hemoglobin A1c decrement after education persisted after adjusting for the duration of diabetes mellitus. In our study, education in patients with diabetes for more than 1 year failed to make a significant improvement in hemoglobin A1c compared with the patients who ignored the education prescription. Therefore, our data support the importance of implementing early DSME for patients with diabetes. To make patients complete the education, physicians should make an effort to encourage patients to finish the education session. In addition, we need to investigate the reason for education refusal and focus more on reducing the rate of non-compliance with education prescriptions in clinical practice.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–308. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Standards of medical care in diabetes: 2011. Diabetes Care. 2011;34(Suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 4.The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995;44:968–983. [PubMed] [Google Scholar]
- 5.Gillett M, Dallosso HM, Dixon S, Brennan A, Carey ME, Campbell MJ, Heller S, Khunti K, Skinner TC, Davies MJ. Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cost effectiveness analysis. BMJ. 2010;341:c4093. doi: 10.1136/bmj.c4093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ko SH, Park SA, Cho JH, Shin KM, Lee SH, Song KH, Park YM, Ahn YB. Influence of the duration of diabetes on the outcome of a diabetes self-management education program. Diabetes Metab J. 2012;36:222–229. doi: 10.4093/dmj.2012.36.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noh JH, Kim SK, Cho YJ, Nam HU, Kim IJ, Jeong IK, Choi MG, Yoo HJ, Ahn YH, Bae HY, Jang HC. Current status of diabetes management in elderly Koreans with diabetes. Diabetes Res Clin Pract. 2007;77(Suppl 1):S71–S75. doi: 10.1016/j.diabres.2007.01.047. [DOI] [PubMed] [Google Scholar]
- 8.Park SW, Kim DJ, Min KW, Baik SH, Choi KM, Park IB, Park JH, Son HS, Ahn CW, Oh JY, Lee J, Chung CH, Kim J, Kim H. Current status of diabetes management in Korea using National Health Insurance database. J Korean Diabetes Assoc. 2007;31:362–367. [Google Scholar]
- 9.Lee JR, Kim SA, Yoo JW, Kang YK. The present status of diabetes education and the role recognition as a diabetes educator of nurses in Korea. Diabetes Res Clin Pract. 2007;77(Suppl 1):S199–S204. doi: 10.1016/j.diabres.2007.01.057. [DOI] [PubMed] [Google Scholar]
- 10.Oh JA, Kim HS, Yoon KH, Choi ES. A telephone-delivered intervention to improve glycemic control in type 2 diabetic patients. Yonsei Med J. 2003;44:1–8. doi: 10.3349/ymj.2003.44.1.1. [DOI] [PubMed] [Google Scholar]
- 11.Scain SF, dos Santos BL, Friedman R, Gross JL. Type 2 diabetic patients attending a nurse educator have improved metabolic control. Diabetes Res Clin Pract. 2007;77:399–404. doi: 10.1016/j.diabres.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 13.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, Siminerio LM, Weinger K, Weiss MA. National standards for diabetes self-management education. Diabetes Care. 2012;35(Suppl 1):S101–S108. doi: 10.2337/dc12-s101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–820. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turner RC, Cull CA, Frighi V, Holman RR UK Prospective Diabetes Study (UKPDS) Group. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49) JAMA. 1999;281:2005–2012. doi: 10.1001/jama.281.21.2005. [DOI] [PubMed] [Google Scholar]
- 16.Choi MJ, Yoo SH, Kim KR, Bae YM, Ahn SH, Kim SS, Min SA, Choi JS, Lee SE, Moon YJ, Rhee EJ, Park CY, Lee WY, Oh KW, Park SW, Kim SW. Effect on glycemic, blood pressure, and lipid control according to education types. Diabetes Metab J. 2011;35:580–586. doi: 10.4093/dmj.2011.35.6.580. [DOI] [PMC free article] [PubMed] [Google Scholar]