Abstract
Sepsis and septic shock are characterized by prolonged inflammation and delayed resolution, which are associated with suppression of neutrophil apoptosis. The role of the intrinsic apoptotic pathway and intracellular factors in regulation of neutrophil apoptosis remain incompletely understood. We previously reported that the nuclear factor MNDA (myeloid nuclear differentiation antigen) is fundamental to execution of the constitutive neutrophil death program. During neutrophil apoptosis MNDA is cleaved by caspases and relocated to the cytoplasm. However, when challenged with known mediators of sepsis, human neutrophils of healthy donors or neutrophils from patients with sepsis exhibited impaired MNDA relocation/cleavage parallel with myeloid cell leukemia-1 (MCL-1) accumulation and suppression of apoptosis. MNDA knockdown in a model cell line indicated that upon induction of apoptosis, MNDA promotes proteasomal degradation of MCL-1, thereby aggravating mitochondrial dysfunction. Thus, MNDA is central to a novel nucleus-mitochondrion circuit that promotes progression of apoptosis. Disruption of this circuit contributes to neutrophil longevity, thereby identifying MNDA as a potential therapeutic target in sepsis and other inflammatory pathologies.
Keywords: MNDA, sepsis, neutrophils, MCL-1, mitochondria, internal apoptosis pathway, inflammation
INTRODUCTION
Different types of hematopoietic cells participate in the inflammatory response to microbial infection. Among them, circulating neutrophils are rapidly recruited into infected or injured tissues. They are the first line of defense against pathogens and are key regulators of the initial response to microbial infection. Effective removal of neutrophils from inflamed tissues is critical for timely resolution of inflammation. However, because of the disruption of neutrophil programmed cell death in inflammatory-related conditions, including sepsis, neutrophils persist in tissues and blood and portend poor prognosis. Here, we will discuss the recent discovery of a novel nuclear to mitochondrion circuit that is involved in the control of neutrophil apoptosis and disrupted during sepsis.
SEPSIS
Sepsis and septic shock (hereafter commonly referred as sepsis) are portent major medical challenges that result from a harmful host response to infection. Sepsis has a high prevalence and morbidity. At the beginning of this century, Angus et al. (2001) reported that, at the time, 9.3% of all cases of death in the USA was caused by sepsis. The incidence of sepsis was then evaluated as 3 cases per 1000 people, and 2.26 cases per 100 hospital-discharged patients. The mortality was estimated at 26.6% of all sepsis cases but, this percentage was significantly higher with elderly patients. The prevalence of this disease is increasing year after year despite advances in critical care. It is now considered to be the 10th leading cause of mortality in the United States (Melamed and Sorvillo, 2009).
Sepsis results from an inappropriate host response to infection. The initial stage of sepsis is usually considered to result from an exaggerated or dysregulated inflammatory response to infection (Pene et al., 2012). As sepsis persists, a shift toward immunosuppression is observed (Hotchkiss and Nicholson, 2006), concomitant with occurrence of organ failure and secondary infection. The severity of sepsis is frequently evaluated by various scoring systems, including the APACHE II (Acute Physiology and Chronic Health Evaluation II; Knaus et al., 1985) or SAPS II (Simplified Acute Physiology Score II; Le Gall et al., 1993) within the first 24 h of hospitalization. The score is based on measurements of vital parameters such as blood pressure, heart rate, respiratory rate, temperature, neutrophil count, etc. Intriguingly, both high and low blood neutrophil counts (neutrophilia and neutropenia, respectively) portend poor prognosis. Despite extensive efforts, specific molecular markers for identifying patients with high risk for sepsis or its more severe form, septic shock, have not been identified. Molecular markers with limited accuracy and specificity have been proposed for defining the stages of the disease. For instance, the prototypic acute-phase reactant C-reactive protein can be used as a marker of systemic inflammation during sepsis, whereas high-levels of procalcitonin are detectable at early stage of bacterial infection (Aalto et al., 2004).
NEUTROPHILS AND SEPSIS
Neutrophils are the first line of defense against pathogens. They generate different proteolytic enzymes as well as reactive oxygen species (ROS) and reactive nitrogen species (RNS) to destroy invading microorganisms following phagocytosis, or extracellulary by neutrophil extracellular trap (NET) formation (Papayannopoulos et al., 2010; Metzler et al., 2011).
Neutrophils have the shortest life span among leukocytes and undergo constitutive programmed cell death (apoptosis). This process is essential for regulation of neutrophil homeostasis. Constitutive apoptosis renders neutrophils unresponsive to extracellular stimuli and allows their recognition and removal by macrophages (Savill et al., 2002; Gilroy et al., 2004). This process is critical for termination of the inflammatory response and tissue repair. Following discharging their function, at the inflammatory locus, extravasated neutrophils are though to predominantly undergo apoptosis. However, signals from the inflammatory milieu can either accelerate or suppress the cell death program, thereby affecting the fate of neutrophils (Gilroy et al., 2004). Suppressed neutrophil apoptosis is often detected in patients with inflammatory pathologies, including sepsis and septic shock and portends poor prognosis (Keel et al., 1997; Matute-Bello et al., 1997; Taneja et al., 2004). Exposure of neutrophils to inflammatory mediators such as GM-CSF, IL-8 or to bacterial constituents results in delayed apoptosis (El Kebir and Filep, 2010; Geering and Simon, 2011). Preserving neutrophil activities at the sites of infection may be required for complete elimination of invading pathogens, but could also aggravate injury to the host, resulting in persistent tissue damage. Therefore, the regulation of neutrophil apoptosis is critical to control the balance between their antimicrobial effectiveness and potential deleterious effect on tissues.
Signaling pathways promoting survival of neutrophils during sepsis are converging to control expression and degradation of key factors influencing the programmed cell death. In mature neutrophils, the anti-apoptotic protein myeloid cell leukemia-1 (MCL-1) and the pro-apoptotic protein Bcl2-associated X (BAX) are critical for the regulation of mitochondrial transmembrane potential (ΔΨm), and hence, activation of effector caspases (El Kebir and Filep, 2010; Geering and Simon, 2011; Milot and Filep, 2011). Since the control of mitochondrial transmembrane potential is central to the intrinsic apoptotic pathway, these discoveries placed forth the intrinsic apoptotic pathway in regulation of neutrophil apoptosis.
INTRINSIC APOPTOSIS PATHWAY AND MCL-1 IN NEUTROPHILS
MCL-1 is an anti-apoptotic factor of the Bcl-2 family. MCL-1 accumulation protects against formation of the BAK-BAX heterodimer on the external mitochondrial membrane and subsequent release of cytochrome c along with other molecules influencing apoptosis like SMAC/Diablo, endonuclease G, and AIF (apoptosis-inducing factor), from the mitochondrial inner membrane. Hence, MCL-1 protects ΔΨm and thus regulates the internal apoptotic pathway.
Unlike other members of the Bcl-2 family, MCL-1 protein has a short half-life and its levels of expression change substantially as neutrophils age and upon exposure of neutrophils to inflammatory mediators (Moulding et al., 2001; Craig, 2002). Indeed, MCL-1 protein expression inversely correlates with the degree of neutrophil apoptosis in both experimental models and clinical settings. Rapid loss in MCL-1 corresponds to development of apoptosis and MCL-1 knockdown results in dramatic decreases in the neutrophil lifespan (Moulding et al., 1998; Dzhagalov et al., 2007). Modification in Mcl-1 transcription accounts for most variation of MCL-1 expression observed upon stress conditions (Dong et al., 2011). At the transcription level, Mcl-1 is regulated by different transcription factors including MYC, NF-κB (RelA/p65), STAT5, and HIF-1α (Akgul et al., 2000; Negrotto et al., 2006; Beverly and Varmus, 2009; Thomas et al., 2010). RNA processing and protein accumulation/turnover are also important for regulation of MCL-1 expression (Bae et al., 2000). The turnover of MCL-1 results primarily from the proteasome activity (Zhong et al., 2005). MULE/Arf-BP1, an E3 ubiquitin ligase, ubiquitinates MCL-1 and subsequently enhances its proteasomal degradation (Zhong et al., 2005). This activity can be counterbalanced by the activity of the deubiquitinase USP9X which was demonstrated to deubiquitinate and thereby, to stabilize MCL-1 (Schwickart et al., 2010). However, surprisingly little is known about regulation of MCL-1. We have identified myeloid nuclear differentiation antigen (MNDA) as a regulator of the proteasomal degradation of MCL-1 (Fotouhi-Ardakani et al., 2010 and see below).
ROLE OF MITOCHONDRIA IN NEUTROPHIL APOPTOSIS
In neutrophils, mitochondria have an atypical function and their role seems to be restricted to apoptosis (van Raam and Kuijpers, 2009). This view has been nourished by the observation that neutrophils rely on glycolysis for energy formation and even for a long time mitochondria could not be detected in these cells. The electron transport chain is inefficient to transport electrons from complexes III to IV in neutrophils (van Raam et al., 2008). However, it is not to say that it exerts no activity in neutrophils since, inhibitors of the mitochondrial respiratory chain complex I can modulate the severity of lung injury evoked by LPS (Zmijewski et al., 2009). Enhanced production of H2O2 by neutrophils results in inhibition of IκB-α degradation hence preventing the activation of NF-κB, a key regulator of inflammatory gene expression in neutrophils (Zmijewski et al., 2008). Thus, the mitochondrial respiratory chain appears to be only partially active in neutrophils.
MNDA: A KEY COMPONENT OF A NOVEL NUCLEUS TO MITOCHONDRION CIRCUIT
Different factors exerting their activity in the nucleus have been reported to participate in and influence the internal apoptosis pathway. While some nuclear proteins including E2F1, STAT3, HIF-1α, and NF-κB are well known to regulate expression of genes encoding pro- or anti-apoptotic factors, other nuclear proteins like MNDA, p53, p21/WAF1, proliferating cell nuclear antigen (PCNA), nur77, SHP, and possibly p73, have been reported or proposed to act as nuclear signals (transducers) to influence the intrinsic apoptotic pathway upon relocation or specific cytoplasmic accumulation (Chipuk et al., 2003; Dumont et al., 2003; Mihara et al., 2003; Wang, 2005; Fotouhi-Ardakani et al., 2010; Witko-Sarsat et al., 2010; Milot and Filep, 2011). Some of these factors have been reported to directly affect pro- or anti-apoptotic factors and hence, apoptosis. MNDA is one of them.
Myeloid nuclear differentiation antigen is a human hematopoietic specific factor of the HIN-200 family. This family of factors is composed of the functionally related proteins IFI16, AIM2, IFIX, and MNDA (Choubey and Panchanathan, 2008). MNDA localizes predominantly to the nucleus and is expressed mainly in myeloid cells. It has been suggested that MNDA may function as a master regulator of monocytic and granulocytic lineages (Novershtern et al., 2011). Recently, MNDA has been proposed to be a transcription factor (Suzuki et al., 2012). Like other members of the HIN-200 family, MNDA contains a pyrin/PAAD/DAPIN domain that mediates binding between proteins involved in apoptotic and inflammatory signaling pathways (Fairbrother et al., 2001). It also contains a HIN-200 domain, which is thought to promote protein–protein (Dawson and Trapani, 1996; Choubey and Panchanathan, 2008) and protein–DNA interactions (Jin et al., 2012). MNDA gene regulation is influenced by interferons (Choubey and Panchanathan, 2008). MNDA was initially proposed to regulate myeloid cell differentiation as well as development of sporadic myelodysplastic syndrome (Briggs et al., 2006).
The potential implication of MNDA in regulation of apoptosis in myeloid cells and in inflammation has been directly assessed in neutrophil granulocytes (Fotouhi-Ardakani et al., 2010). In bone marrow-derived and mature neutrophils, MNDA is predominantly located in the nucleus. In neutrophils undergoing apoptosis, MNDA is cleaved by caspases, presumably caspase-3, and relocated to the cytoplasm. However, the cleavage of MNDA is likely not required for its cytoplasmic accumulation since the full-length MNDA could also be detected in the cytoplasm. Culture of human neutrophils with inflammatory mediators, like bacterial constituents and platelet-activating factor, promotes their survival and indicates a clear correlation between the degree of neutrophil apoptosis and MNDA cleavage as well as cytoplasmic accumulation. These findings suggest that MNDA could participate in regulation of apoptosis in neutrophils.
A causal relationship between MNDA and apoptosis has been established in a model cell line, the promyelocytic leukemia cell line HL-60, which expresses endogenous MNDA (Duhl et al., 1989; Savli et al., 2002). We created two MNDA-deficient HL-60 cell lines by the stable genomic integration of vectors encoding specific small hairpin RNA (shRNA). In these engineered model cell lines, knockdown of MNDA partially protected HL-60 cells against genotoxic stress-induced apoptosis, markedly attenuated activation of caspase-3, but not caspase-8, and prevented mitochondrial dysfunction (Fotouhi-Ardakani et al., 2010). These observations identify MNDA as a modulator of the intrinsic (mitochondrial) pathway of apoptosis.
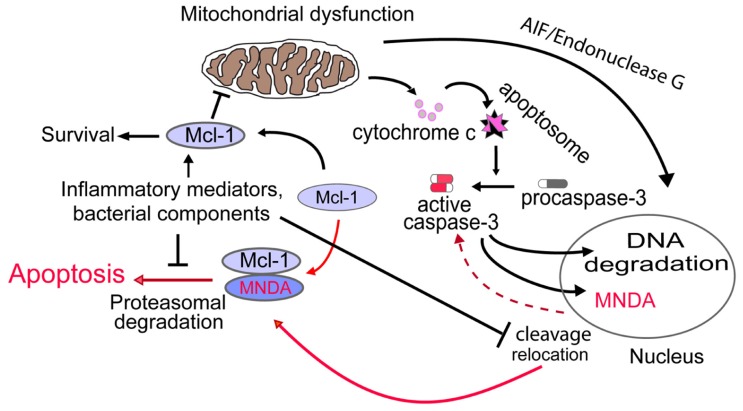
The importance of the anti-apoptotic factor MCL-1 in control of ΔΨm and neutrophil apoptosis (Moulding et al., 1998; Dzhagalov et al., 2007) led us to interrogate whether MNDA could influence the internal pathway of apoptosis via MCL-1. Interestingly, we found that: (i) MNDA co-immunoprecipitates with MCL-1; and (ii) after induction of apoptosis, MCL-1 accumulation was greatly enhanced in MNDA-deficient HL-60 cells compared to MNDA proficient HL-60 cells (Fotouhi-Ardakani et al., 2010). Similar results were obtained in the presence of the protein synthesis inhibitor cycloheximide, suggesting that MNDA influences the turnover of MCL-1 protein. Since MCL-1 turnover is mainly regulated by proteasomal degradation (Zhong et al., 2005), we blocked the proteasome activity with MG132 and found that under such condition, MNDA failed to affect MCL-1 accumulation. These findings confirm that the rapid fall in MCL-1 expression is due to proteasomal degradation and indicate that, when present, MNDA promotes proteasomal degradation of MCL-1. By contrast, MNDA knockdown slowed down MCL-1 turnover and rendered HL-60 cells resistant to genotoxic stress-induced apoptosis, indicating that MNDA regulation of MCL-1 degradation is required for the execution of the constitutive cell death program. Collectively these findings indicate that cytoplasmic accumulation of MNDA is not merely a consequence, but rather an important mechanism promoting apoptosis in HL-60 cells and likely, in mature human neutrophils (Figure 1).
FIGURE 1.
Proposed model for MNDA regulation of neutrophil apoptosis. Cytoplasmic relocation and cleavage of MNDA results in aggravation of mitochondrial dysfunction through promotion of proteasomal degradation of MCL-1. Activation of this novel nucleus-mitochondrion circuit would then accelerate execution of the apoptotic death program. Conversely, prevention of MNDA relocation and cleavage would prolong neutrophil survival by retarding apoptosis. The mechanisms by which bacterial components and/or inflammatory modulators could negatively influence MNDA relocation and cleavage and hence, interfere with this nuclear-mitochondrial circuit remains to be defined. Broken line indicates yet undefined mechanism.
It is not known whether co-immunoprecipitation of MNDA and MCL-1 resulted from direct protein–protein interaction or which region(s) of MNDA is(are) required for this association. However, the MNDA PAAD/DAPIN/Pyrin domain, which is common to different proteins involved in apoptosis and inflammation, and/or the HIN-200 domain that mediates protein–protein interactions (Asefa et al., 2004) could be critical for the MNDA interaction with MCL-1. Indeed, the PAAD/DAPIN/Pyrin domain was shown to promote self-association of MNDA (Xie et al., 1997), and might also mediate association with other proteins. For instance, IFI16, which contains a PAAD/DAPIN/Pyrin domain, interacts with p53, thereby modulating senescence and apoptosis (Song et al., 2008). In mice, members of the HIN-200 family were shown to promote inflammation through interacting with NF-κB (Min et al., 1996). These results demonstrate that a member of the HIN-200 family or a protein with the PAAD/DAPIN/Pyrin domain co-immunoprecipitates with an anti-apoptotic protein of the Bcl-2 family to regulate apoptosis. It remains to be investigated whether this mechanism is common to all MNDA expressing cells including hematopoietic progenitors (Briggs et al., 2006).
ROLE FOR MNDA DURING SEPSIS
It is well established that neutrophils isolated from the peripheral blood of healthy volunteers undergo apoptosis when cultured for 24–48 h in vitro. By contrast, under the same conditions of culture, neutrophils of patients with sepsis exhibit markedly prolonged survival due to suppressed apoptosis (Keel et al., 1997; Matute-Bello et al., 1997; Fotouhi-Ardakani et al., 2010; Paunel-Gorgulu et al., 2012). The enhanced neutrophil longevity is associated with preserved ΔΨm and inversely correlates with cytoplasmic accumulation of MNDA (Fotouhi-Ardakani et al., 2010). As predicted from the comprehensive study on MNDA in model cell lines (see above), during neutrophil apoptosis MNDA is relocated from the nucleus to the cytoplasm whereby it directly interacts with MCL-1 and promotes its proteasomal degradation (Figure 1). Although the signaling pathways involved in these events have not been elucidated, MNDA remains sequestered in the nucleus of neutrophils of patients in sepsis (Fotouhi-Ardakani et al., 2010). Consistently, culture of neutrophils from healthy volunteers with LPS, bacterial DNA, or platelet-activating factor partially replicated the abnormalities seen in the clinical samples, including the sequestration of MNDA to the nucleus (Fotouhi-Ardakani et al., 2010). Most interestingly, similar results were obtained when neutrophils of healthy donors were cultured in presence of serum from sepsis patient (Fotouhi-Ardakani et al., 2010). These findings suggest that neutrophils integrate yet unidentified cues from the inflammatory milieu, which would prevent the cytoplasmic relocation and/or accumulation of MNDA, events that favor neutrophil apoptosis. Although our pilot clinical study was not powered to assess outcome, we noted that patients who had died exhibited markedly suppressed neutrophil apoptosis with minimal or complete absence of MNDA translocation and/or cleavage in neutrophils. Suppressed apoptosis in circulating neutrophils may contribute to neutrophilia, which predicts a poor prognosis, whereas delayed apoptosis in emigrated or trapped neutrophils contributes to aggravation of tissue injury, in particular damage to the airways (Matute-Bello et al., 1997; Hotchkiss and Nicholson, 2006). Apoptotic neutrophils sequester cytokines during endotoxin shock in mice (Ren et al., 2008) and thus may contribute to resolution of sepsis. Conversely, failure of neutrophils to undergo timely apoptosis would likely impair this pro-resolution effect. Clearly, additional studies are required to assess the precise role of MNDA in facilitating resolution of inflammation.
In conclusion, cytoplasmic accumulation of MNDA plays an important role in the progression of apoptosis. This represents a novel mechanism whereby MNDA, which predominantly localizes to the nucleus, regulate MCL-1 degradation and consequently mitochondrial function following its accumulation in the cytoplasm. The investigation of MNDA in neutrophils demonstrates that prevention of cytoplasmic MNDA accumulation likely contributes to suppressed apoptosis of neutrophils in patients with sepsis. Therefore, targeting MNDA may have a therapeutic potential for the treatment of sepsis and other inflammatory disorders.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by grants from the Lymphoma and Leukemia Society of Canada (to Eric Milot) and MOP-67054 and MOP-97742 from the Canadian Institutes of Health Research (to János G. Filep). Eric Milot is scholar of the FRQS.
REFERENCES
- Aalto H., Takala A., Kautiainen H., Repo H. (2004). Laboratory markers of systemic inflammation as predictors of bloodstream infection in acutely ill patients admitted to hospital in medical emergency. Eur. J. Clin. Microbiol. Infect. Dis. 23 699–704 [DOI] [PubMed] [Google Scholar]
- Akgul C., Turner P. C., White M. R., Edwards S. W. (2000). Functional analysis of the human MCL-1 gene. Cell. Mol. Life Sci. 57 684–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angus D. C., Linde-zwirble W. T., Lidicker J., Clermont G., Carcillo J., Pinsky M. R. (2001). Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit. Care Med. 29 1303–1310 [DOI] [PubMed] [Google Scholar]
- Asefa B., Klarmann K. D., Copeland N. G., Gilbert D. J., Jenkins N. A., Keller J. R. (2004). The interferon-inducible p200 family of proteins: a perspective on their roles in cell cycle regulation and differentiation. Blood Cells Mol. Dis. 32 155–167 [DOI] [PubMed] [Google Scholar]
- Bae J., Leo C. P., Hsu S. Y., Hsueh A. J. (2000). MCL-1S, a splicing variant of the antiapoptotic BCL-2 family member MCL-1, encodes a proapoptotic protein possessing only the BH3 domain. J. Biol. Chem. 275 25255–25261 [DOI] [PubMed] [Google Scholar]
- Beverly L. J., Varmus H. E. (2009). MYC-induced myeloid leukemogenesis is accelerated by all six members of the antiapoptotic BCL family. Oncogene 28 1274–1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs R. C., Shults K. E., Flye L. A., Mcclintock-treep S. A., Jagasia M. H., Goodman S. A., et al. (2006). Dysregulated human myeloid nuclear differentiation antigen expression in myelodysplastic syndromes: evidence for a role in apoptosis. Cancer Res. 66 4645–4651 [DOI] [PubMed] [Google Scholar]
- Chipuk J. E., Maurer U., Green D. R., Schuler M. (2003). Pharmacologic activation of p53 elicits Bax-dependent apoptosis in the absence of transcription. Cancer Cell 4 371–381 [DOI] [PubMed] [Google Scholar]
- Choubey D., Panchanathan R. (2008). Interferon-inducible Ifi200-family genes in systemic lupus erythematosus. Immunol. Lett. 119 32–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig R. W. (2002). MCL1 provides a window on the role of the BCL2 family in cell proliferation, differentiation and tumorigenesis. Leukemia 16 444–454 [DOI] [PubMed] [Google Scholar]
- Dawson M. J., Trapani J. A. (1996). HIN-200: a novel family of IFN-inducible nuclear proteins expressed in leukocytes. J. Leukoc. Biol. 60 310–316 [DOI] [PubMed] [Google Scholar]
- Dong L., Jiang C. C., Thorne R. F., Croft A., Yang F., Liu H., et al. (2011). Ets-1 mediates upregulation of Mcl-1 downstream of XBP-1 in human melanoma cells upon ER stress. Oncogene 30 3716–3726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhl D. M., Gaczynski M., Olinski R., Briggs R. C. (1989). Intranuclear distribution of the human myeloid cell nuclear differentiation antigen in HL-60 cells. J. Cell. Physiol. 141 148–153 [DOI] [PubMed] [Google Scholar]
- Dumont P., Leu J. I., Della pietra A. C., III, George D. L., Murphy M. (2003). The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat. Genet. 33 357–365 [DOI] [PubMed] [Google Scholar]
- Dzhagalov I., St John A., He Y. W. (2007). The antiapoptotic protein Mcl-1 is essential for the survival of neutrophils but not macrophages. Blood 109 1620–1626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Kebir D., Filep J. G. (2010). Role of neutrophil apoptosis in the resolution of inflammation. Sci. World J. 10 1731–1748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother W. J., Gordon N. C., Humke E. W., O’Rourke K. M., Starovasnik M. A., Yin J. P., et al. (2001). The PYRIN domain: a member of the death domain-fold superfamily. Protein Sci. 10 1911–1198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fotouhi-Ardakani N., Kebir D. E., Pierre-charles N., Wang L., Ahern S. P., Filep J. G., et al. (2010). Role for myeloid nuclear differentiation antigen in the regulation of neutrophil apoptosis during sepsis. Am. J. Respir. Crit. Care Med. 182 341–350 [DOI] [PubMed] [Google Scholar]
- Geering B., Simon H. U. (2011). Peculiarities of cell death mechanisms in neutrophils. Cell Death Differ. 18 1457–1469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilroy D. W., Lawrence T., Perretti M., Rossi A. G. (2004). Inflammatory resolution: new opportunities for drug discovery. Nat. Rev. Drug Discov. 3 401–416 [DOI] [PubMed] [Google Scholar]
- Hotchkiss R. S., Nicholson D. W. (2006). Apoptosis and caspases regulate death and inflammation in sepsis. Nat. Rev. Immunol. 6 813–822 [DOI] [PubMed] [Google Scholar]
- Jin T., Perry A., Jiang J., Smith P., Curry J. A., Unterholzner L., et al. (2012). Structures of the HIN domain:DNA complexes reveal ligand binding and activation mechanisms of the AIM2 inflammasome and IFI16 receptor. Immunity 36 561–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel M., Ungethum U., Steckholzer U., Niederer E., Hartung T., Trentz O., et al. (1997). Interleukin-10 counterregulates proinflammatory cytokine-induced inhibition of neutrophil apoptosis during severe sepsis. Blood 90 3356–3363 [PubMed] [Google Scholar]
- Knaus W. A., Draper E. A., Wagner D. P., Zimmerman J. E. (1985). APACHE II: a severity of disease classification system. Crit. Care Med. 13 818–829 [PubMed] [Google Scholar]
- Le Gall J. R., Lemeshow S., Saulnier F. (1993). A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270 2957–2963 [DOI] [PubMed] [Google Scholar]
- Matute-Bello G., Liles W. C., Radella F., II, Steinberg K. P., Ruzinski J. T., Jonas M., et al. (1997). Neutrophil apoptosis in the acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 156 1969–1977 [DOI] [PubMed] [Google Scholar]
- Melamed A., and Sorvillo F. J. (2009). The burden of sepsis-associated mortality in the United States from 1999 to 2005: an analysis of multiple-cause-of-death data. Crit. Care 13 R28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler K. D., Fuchs T. A., Nauseef W. M., Reumaux D., Roesler J., Schulze I., et al. (2011). Myeloperoxidase is required for neutrophil extracellular trap formation: implications for innate immunity. Blood 117 953–959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihara M., Erster S., Zaika A., Petrenko O., Chittenden T., Pancoska P., et al. (2003). p53 has a direct apoptogenic role at the mitochondria. Mol. Cell 11 577–590 [DOI] [PubMed] [Google Scholar]
- Milot E., Filep J. G. (2011). Regulation of neutrophil survival/apoptosis by Mcl-1. Sci. World J. 11 1948–1962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min W., Ghosh S., Lengyel P. (1996). The interferon-inducible p202 protein as a modulator of transcription: inhibition of NF-kappa B, c-Fos, and c-Jun activities. Mol. Cell. Biol. 16 359–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulding D. A., Akgul C., Derouet M., White M. R., Edwards S. W. (2001). BCL-2 family expression in human neutrophils during delayed and accelerated apoptosis. J. Leukoc. Biol. 70 783–792 [PubMed] [Google Scholar]
- Moulding D. A., Quayle J. A., Hart C. A., Edwards S. W. (1998). Mcl-1 expression in human neutrophils: regulation by cytokines and correlation with cell survival. Blood 92 2495–2502 [PubMed] [Google Scholar]
- Negrotto S., Malaver E., Alvarez M. E., Pacienza N., D’Atri L. P., Pozner R. G., et al. (2006). Aspirin and salicylate suppress polymorphonuclear apoptosis delay mediated by proinflammatory stimuli. J. Pharmacol. Exp. Ther. 319 972–979 [DOI] [PubMed] [Google Scholar]
- Novershtern N., Subramanian A., Lawton L. N., Mak R. H., Haining W. N., Mcconkey M. E., et al. (2011). Densely interconnected transcriptional circuits control cell states in human hematopoiesis. Cell 144 296–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papayannopoulos V., Metzler K. D., Hakkim A., Zychlinsky A. (2010). Neutrophil elastase and myeloperoxidase regulate the formation of neutrophil extracellular traps. J. Cell Biol. 191 677–691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paunel-Gorgulu A., KIrichevska T., Logters T., Windolf J., Flohe S. (2012). Molecular mechanisms underlying delayed apoptosis in neutrophils from multiple trauma patients with and without sepsis. Mol. Med. 18 325–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pene F., Grimaldi D., Zuber B., Sauneuf B., Rousseau C., EL Hachem C., et al. (2012). Toll-like receptor 2 deficiency increases resistance to Pseudomonas aeruginosa pneumonia in the setting of sepsis-induced immune dysfunction. J. Infect. Dis. 206 932–942 [DOI] [PubMed] [Google Scholar]
- Ren Y., Xie Y., Jiang G., Fan J., Yeung J., Li W., et al. (2008). Apoptotic cells protect mice against lipopolysaccharide-induced shock. J. Immunol. 180 4978–4985 [DOI] [PubMed] [Google Scholar]
- Savill J., Dransfield I., Gregory C., Haslett C. (2002). A blast from the past: clearance of apoptotic cells regulates immune responses. Nat. Rev. Immunol. 2 965–975 [DOI] [PubMed] [Google Scholar]
- Savli H., Aalto Y., Nagy B., Knuutila S., Pakkala S. (2002). Gene expression analysis of 1,25(OH)2D3-dependent differentiation of HL-60 cells: a cDNA array study. Br. J. Haematol. 118 1065–1070 [DOI] [PubMed] [Google Scholar]
- Schwickart M., Huang X., Lill J. R., Liu J., Ferrando R., French D. M., et al. (2010). Deubiquitinase USP9X stabilizes MCL1 and promotes tumour cell survival. Nature 463 103–107 [DOI] [PubMed] [Google Scholar]
- Song L. L., Alimirah F., Panchanathan R., Xin H., Choubey D. (2008). Expression of an IFN-inducible cellular senescence gene, IFI16, is up-regulated by p53. Mol. Cancer Res. 6 1732–1741 [DOI] [PubMed] [Google Scholar]
- Suzuki T., Nakano-ikegaya M., Yabukami-okuda H., De Hoon M., Severin J., Saga-Hatano S., et al. (2012). Reconstruction of monocyte transcriptional regulatory network accompanies monocytic functions in human fibroblasts. PLoS ONE 7:e33474 10.1371/journal.pone.0033474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taneja R., Parodo J., Jia S. H., Kapus A., Rotstein O. D., Marshall J. C. (2004). Delayed neutrophil apoptosis in sepsis is associated with maintenance of mitochondrial transmembrane potential and reduced caspase-9 activity. Crit. Care Med. 32 1460–1469 [DOI] [PubMed] [Google Scholar]
- Thomas L. W., Lam C., Edwards S. W. (2010). Mcl-1; the molecular regulation of protein function. FEBS Lett. 584 2981–2989 [DOI] [PubMed] [Google Scholar]
- van Raam B. J., Kuijpers T. W. (2009). Mitochondrial defects lie at the basis of neutropenia in Barth syndrome. Curr. Opin. Hematol. 16 14–19 [DOI] [PubMed] [Google Scholar]
- van Raam B. J., Sluiter W., De Wit E., Roos D., Verhoeven A. J., Kuijpers T. W. (2008). Mitochondrial membrane potential in human neutrophils is maintained by complex III activity in the absence of supercomplex organisation. PLoS ONE 3:e2013 10.1371/journal.pone.0002013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. Y. (2005). Nucleo-cytoplasmic communication in apoptotic response to genotoxic and inflammatory stress. Cell Res. 15 43–48 [DOI] [PubMed] [Google Scholar]
- Witko-Sarsat V., Mocek J., Bouayad D., Tamassia N., Ribeil J. A., Candalh C., et al. (2010). Proliferating cell nuclear antigen acts as a cytoplasmic platform controlling human neutrophil survival. J. Exp. Med. 207 2631–2645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Briggs J. A., Briggs R. C. (1997). MNDA dimerizes through a complex motif involving an N-terminal basic region. FEBS Lett. 408 151–155 [DOI] [PubMed] [Google Scholar]
- Zhong Q., Gao W., Du F., Wang X. (2005). Mule/ARF-BP1, a BH3-only E3 ubiquitin ligase, catalyzes the polyubiquitination of Mcl-1 and regulates apoptosis. Cell 121 1085–1095 [DOI] [PubMed] [Google Scholar]
- Zmijewski J. W., Lorne E., Banerjee S., Abraham E. (2009). Participation of mitochondrial respiratory complex III in neutrophil activation and lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 296 L624–L634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmijewski J. W., Lorne E., Zhao X., Tsuruta Y., Sha Y., Liu G., et al. (2008). Mitochondrial respiratory complex I regulates neutrophil activation and severity of lung injury. Am. J. Respir. Crit. Care Med. 178 168–179 [DOI] [PMC free article] [PubMed] [Google Scholar]