Abstract
AIM
To describe a simple modification of fashioning the mucosal flap for endonasal endoscopic dacryocystorhinostomy (EES-DCR) in Asians and investigate its efficacy.
METHODS
A total of 120 patients with unilateral primary chronic dacryocystitis (PCD) were randomized into two groups: the new shaped nasal mucosal flap group (group A) and the removed nasal mucosal flap group (group B). All patients underwent standard EES-DCR. Patients in group A were performed a new shaped nasal mucosal flap covering the bared bone around the opened sac and those in group B was removed the nasal mucosal flap uncovering the bared bone. Patients were followed up for one year. The occurrence of granulation tissue, the proliferation of scar tissue and success rate of EES-DCR was compared.
RESULTS
In the present study, complete postoperative data were acquired from 54 patients in group A and from 57 patients in group B. During process of review, the occurrence of granulation tissue was at the ostium margins account for 15% (8/54) in group A and 39% (22/57) in group B (P<0.05). At the one-year review, scar tissue was present in 5 patients in group A compared with 18 in group B (P<0.05). The success rate of EES-DCR was 98% (53/54) in group A and 84% (48/57) in group B (P<0.05).
CONCLUSION
The simple modification of fashioning nasal mucosal flap can effectively cover the bared bone around the opened sac and reduce formation of granulation tissue, lessen the risk of scar tissue formation and closure of ostium, thus improve the success rate of EES-DCR in Asians.
Keywords: mucosal flap, endonasal endoscopic dacryocystorhinostomy, chronic dacryocystitis
INTRODUCTION
Recently, the endonasal endoscopic approach for dacryocystorhinostomy (EES-DCR) has become increasingly popular over the external dacryocystorhinostomy (Ex-DCR) approach. However, the success rate for EES-DCR has been inferior to the Ex-DCR[1],[2]. It seems that the key to improving the success rate of EES-DCR is to attempt to replicate the Ex-DCR procedure as closely as possible, namely exact anastomosis of the nasal mucosa and lacrimal sac[3]-[6]. There were several different measures to perform anastomosis of the nasal mucosa and lacrimal sac. Such as U-shaped[4]-[6], L-shaped nasal mucosal flap[7], free nasal mucosal flap[8] and preservation of whole nasal mucosal flap appositing to lacrimal sac[9]. However, the majority of anastomosis was based on white patients. In our experience, the EES-DCR for Asians is more difficult than for whites. We reasoned that the difficulty might be attributable to the anatomic differences in the intranasal structures between the races. Asians has a low nasal bridge and a thicker frontal process of the maxilla. Creating a large bony ostium requires extensive removal of the frontal process of the maxilla during EES-DCR. It is therefore inevitable that a portion of the bone at the frontal process of the maxilla will remain exposed at the completion of the operation. This can lead unwanted formation of granulation and scar tissue around the ostium. The technique of U-shaped and L-shaped nasal mucosal flap, sacrificed the most of the central part of the flap. It is hardly to cover the more widely exposed bone. Furthermore, the small portion of nasal mucosal flap is easily tearing or even loss. Mahendran et al[8] introduced the other option of using a free mucosal flap to cover the bare bone in patients undergoing EES-DCR. However, there were also some problems, such as time-consuming, flap mobility and survive of free flap on the bared bone. Considering above problems, we conducted a simple modification of fashioning nasal mucosal flap during the standard EES-DCR. This modification simplifies the technically challenge, perseveres most of nasal mucosal flap to cover the bared bone and avoids the flap mobility and loss.
The present study aimed to investigate whether the new modification technique can reduce formation of granulation tissue, lessen the risk of closure of ostium and improve success of EES-DCR in Asians.
SUBJECTS AND METHODS
Subjects
This prospective study was performed at the Eye Hospital of Wenzhou Medical College from December 2009 and October 2011. Ethical approval was obtained from the Institutional Review Board and informed consent was obtained from all subjects, in accordance to the tenets of the declaration of Helsinki. All consecutive patients with unilateral primary chronic dacryocystitis (PCD) were included in the study. The diagnosis of PCD was made on the basis of a history of epiphora with purulent discharge and regurgitation on nasolacrimal irrigation. We excluded patients with acute dacryocystitis, a previous history of physical scars, previous lacrimal surgery, eyelid malposition including ectropion or entropion, and previous facial fractures or nasal diseases, such as polyps and chronic sinusitis, and follow up of less than one year.
Surgical technique of standardized EES-DCR
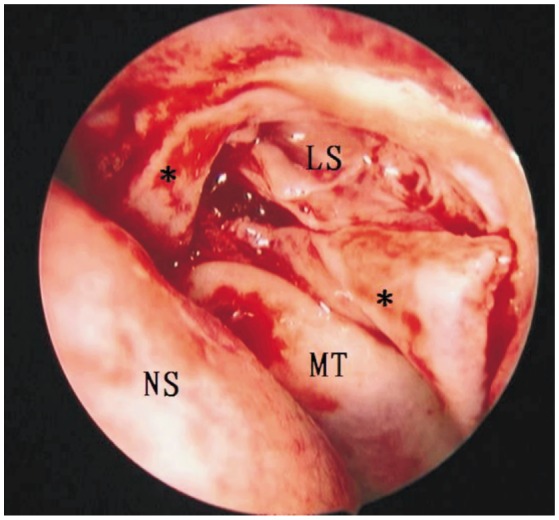
All patients underwent standard EES-DCR, which was performed by a single surgeon (WW). Before surgery, all patients were randomly divided by independent member of staff into two groups. Patients in group A was preserved nasal mucosal flap which was trimmed into a V-shaped and covered the bared bone around the opened sac, and those in group B was removed the nasal mucosal flap. All patients were subjected to a standardized EES-DCR mainly as described by Wu et al[10]. In summary, a mixture of 2mL of 2% lidocaine and epinephrine (1:100 000) was injected into the lateral nasal wall in addition to an external anterior ethmoidal nerve block and an infraorbital nerve block. Under direct visualization with a 45° 4-mm endonasal endoscope (Karl Storz, Tuttlingen, Germany), the lateral nasal mucosa was incised in the region of the lacrimal sac fossa and produced a mucosal flap hinged on a posterior base. An osteotomy (8mm×10mm in size) was created using an angled (15°) coarse diamond burr attached to a microdebrider (XPS3000, Medtronic Xomed, Minneapolis, MN, USA) and/or a Hajek-Koffler forward-biting punch. Further, the medial wall of the lacrimal sac was tented with the Bowman's lacrimal probe and vertical incised from top to bottom creating a “C” shaped lacrimal sac flap. In group A, a soft tissue scissor is used to remove less of the central part of the flap leaving the upper and lower limb of this flap to cover the raw bone above and below the opened sac. This flap is called V-shaped mucosal flap (Figure 1). In group B, the nasal mucosal flap was removed. Finally, pieces of Merogel (Medtronic Xomed, UK) pack were carefully covered over the mucosal flap anastomosis to keep it in position in two groups.
Figure 1. Left nasal cavity. Application of V-shaped mucosal flap during EES-DCR (black asterisk), using a soft tissue scissor to remove less of the central part of the flap leaving the upper and lower limb of this flap (black asterisk) to cover the raw bone above and below the opened sac. NS, nasal septum; MT, middle turbinate; LS, lacrimal sac.
Post-operative care and follow-up
Post-operatively, 5 days of oral antibiotics and a topical mixture of antibiotic and steroid eye drops for 1 month were prescribed. Irrigation and spray of the nasal cavity with saline were performed to prevent crust formation. Follow-up reviews were 1 week, 2 weeks, 1 month, 3, 6, and 12 months after operation. At each follow-up appointment, regular nasal endoscopic examinations were performed to investigate the wound healing and remove crusts and granulations (if any), and the granulation or scar tissue formation in the process of mucosal healing were recorded. Lacrimal irrigation was used to confirm the patency of ostium. Surgical success was defined as absence of epiphora and purulent discharge together with a patent lacrimal system, one year post-operatively. If lacrimal obstruction was occurred at any time point during the follow-up period, the patient was considered a surgical failure.
Statistical Analysis
All statistical analysis was performed using SPSS version 16 (SPSS Inc, Chicago, IL). Group means of primary data of the patients were compared with an independent sample t -test. Success rates of EES-DCR, the scar tissue formation around the ostium at one-year review and the occurrence of granulations at the ostial margins during the process of review were evaluated with Pearson' χ2-test. P<0.05 was considered as statistically significant in all tests.
RESULTS
We randomly assigned 120 patients with unilateral PCD into two groups. In group A, 2 patients failing to perform the mucosal flap and 4 patients failing to complete the follow-up were excluded from this study. In group B, 1 patient had complicated heavy nasal bleeding within the first week following surgery, 2 patients failing to complete the follow-up. Therefore, we included 54 patients in group A and 57 patients in group B. Between two groups, there were no statistically differences in patient age, sex and history of symptoms (Table 1).
Table 1. Patient characteristics for both groups in the study.
| Characteristics | Group A | Group B | P |
| n | 54 | 57 | |
| Age (a) | 44.5±14.2 | 47.5±14.0 | 10.816 |
| Gender (M/F) | 6/48 | 6/51 | 20.921 |
| Eye sides (R/L) | 31/23 | 38/19 | 20.315 |
| History (a) | 3.80±4.32 | 4.96± 3.84 | 10.215 |
Group A= standard EES-DCR with V-shaped nasal mucosal flap; Group B= standard EES-DCR without V-shaped nasal mucosal flap; 1Statistical analysis performed with the unpaired independent samples t test; 2Statistical analysis performed with the Chi-square test.
During the process of review, the occurrence of granulation tissue was at the ostial margins account for 15% (8/54) in group A and 39% (22/57) in group B (P<0.05). At the one-year review, scar tissue was present in 5 patients in group A compared with 18 in group B. The success rate of EES-DCR was 98% (53/54) in group A and 84% (48/57) in group B (P<0.05).
The causes of surgical failure have showed in Table 2. In group A, 1 patient had a failed outcome because of excessive formation of granulation tissue around the intranasal ostium. In group B, 9 patients had a failed outcome because of excessive formation of granulation or/and scar tissue.
Table 2. Causes of surgical failure.
| Causes | Group A | Group B |
| Scar tissue formation | 0 | 2 |
| Granulation tissue formation | 1 | 4 |
| Granulation and scar tissue formation | 0 | 3 |
DISCUSSION
Performing EES-DCR in Asian patients with a low nasal bridge is sometimes more difficult than in white patients with a higher nasal bridge. This is because that the height and length of the nasal bone has a negative correlation with the thickness of the frontal process of the maxilla[11].Nevertheless, creating a large bony ostium requires extensive removal of the frontal process of the maxilla during EES-DCR. It is therefore inevitable that a portion of the bone at the frontal process of the maxilla will remain exposed at the completion of the operation. Especially, Asian patients with thicker frontal process of the maxilla leave more widely region of bared bone after surgery. This can lead unwanted formation of granulation tissue and scar tissue around the ostium, thus results in failure of EES-DCR. Therefore, it is very important for Asian patients to perform mucosal flap technology to cover bared bone during EES-DCR. Although there were many methods to perform mucosal flap technology, the majority of method based on the lacrimal system of Whites anatomically and presented guidelines for EES-DCR. For example, the powered endoscopic DCR with a U-shaped nasal mucosal flap described by Wormald[4] is a well-established technique, with comparable success rates to external methods. It entails the use of soft tissue scissor to remove most of the central part of the flap. However, accurate fashioning of the U-shaped flap can be difficult for Asians with narrow nasal cavity due to various factors including excessive flap mobility, poor surgical field. The free mucosal flap technology[8] was also advised to apply in EES-DCR, but this technique is unsuitable for Asians with narrow nasal cavity. Therefore, we introduced a new technique of fashioning a V-shaped nasal mucosal flap to cover the bared bone around the sac. This technique preserved most of part of the nasal mucosal flap to cover the bared bone as possible and reduced the mucosal flap mobility.
The present study showed that, at the one-year review, the success rate of EES-DCR reached 98% (53/54) in group A, as opposed to control group B (84%, 48/57). We observed that the rate of granulation and scar tissue formation was lower in group A, with a lower incidence of ostial failure than in control group B. These results suggest that the preservation of the nasal mucosa and fashioning of a nasal V-shaped flap, apposing well to the lacrimal sac flap and covering the bared bone, can reduce the formation of granulation tissue and lessen the risk for subsequent scar and closure of the ostium. Thus, this technique improves the success rate of EES-DCR in Asian patients. The present result is consistent with previous studies[3]-[5]. Tsirbas and Wormald[4] described a technique that involving the preservation of the nasal mucosa and fashioning of a U-shaped nasal mucosal flap, apposing well to the lacrimal sac flap and covering the bared bone. They reported anatomic success rate of 91%. Sonkhya et al[12] indicated that creation of lacrimal and nasal mucosal flap results in primary intention healing with minimal risk of granulation tissue formation and therefore achieved a good success rate of 92%. However, Ramakrishnan et al[13] suggested that preservation of mucosal flap may not be essential in achieving successful outcomes. They removed the mucosal flap raised early in the procedure and eliminated the redundant lacrimal sac edges at the conclusion of the procedure with anatomic success rate of 93%. Kansu et al[14] conducted a comparison study of surgical outcomes EES-DCR with or without mucosal flaps. The result indicated that the closure of bare bone with nasal mucosal flap and an anastomosis between the lacrimal sac mucosa and the nasal mucosa decreases the formation of granulation tissue. But there is no significant difference of success rate. We propose that these limited effects observed with mucosal flap may be explained by the large bony ostium and less portion of bared bone during EES-DCR in white people. Asians have a low nasal bridge and a thicker frontal process of the maxilla. The special characteristics restricted to create a large bony ostium and allowed to expose more portion of bared bone. Hence the technique that preservation of nasal mucosa and exact anastomosis of the nasal mucosa and lacrimal sac is more important for Asian patients to improve the success rate.
In conclusion, the simple modification of fashioning a “V-shaped” nasal mucosal flap can easily manipulate in Asian patients and preserver most of mucosal flap to cover the exposed bone. This mucosal flap technique reduces formation of granulation tissue, lessens the risk of scar tissue formation and closure of ostium, and thus improves the success rate of EES-DCR.
Footnotes
Foundation item: 2011 Guangdong Province Natural Science Fund, China (No.S2011010004186)
REFERENCES
- 1.Hartikainen J, Grenman R, Puukka P, Seppä H. Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy. Ophthalmology. 1998;105(6):1106–1113. doi: 10.1016/S0161-6420(98)96015-8. [DOI] [PubMed] [Google Scholar]
- 2.Woog JJ, Kennedy RH, Custer PL, Kaltreider SA, Meyer DR, Camara JG. Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2001;108(12):2369–2377. doi: 10.1016/s0161-6420(01)00945-9. [DOI] [PubMed] [Google Scholar]
- 3.Wormald PJ. Powered endoscopic dacryocystorhinostomy. Laryngoscope. 2002;112(1):69–72. doi: 10.1097/00005537-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Tsirbas A, Wormald PJ. Endonasal dacryocystorhinostomy with mucosal flaps. Am J Ophthalmol. 2003;135(1):76–83. doi: 10.1016/s0002-9394(02)01830-5. [DOI] [PubMed] [Google Scholar]
- 5.Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Br J Ophthalmol. 2003;87(1):43–47. doi: 10.1136/bjo.87.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Otolaryngol Clin North Am. 2006;39(5):1019–1036. doi: 10.1016/j.otc.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Trimarchi M, Giordano Resti A, Bellini C, Forti M, Bussi M. Anastomosis of nasal mucosal and lacrimal sac flaps in endoscopic dacryocystorinostomy. Eur Arch Otorhinolaryngol. 2009;266(11):1747–1752. doi: 10.1007/s00405-009-1002-z. [DOI] [PubMed] [Google Scholar]
- 8.Mahendran S, Stevens-King A, Yung MW. How we do it: the viability of free mucosal grafts on exposed bone in lacrimal surgery a prospective study. Clin Otolaryngol. 2006;31(4):324–327. doi: 10.1111/j.1749-4486.2006.01170.x. [DOI] [PubMed] [Google Scholar]
- 9.Codère F, Denton P, Corona J. Endonasal dacryocystorhinostomy: a modified technique with preservation of the nasal and lacrimal mucosa. Ophthal Plast Reconstr Surg. 2010;26(3):161–164. doi: 10.1097/IOP.0b013e3181b80af6. [DOI] [PubMed] [Google Scholar]
- 10.Wu W, Yan W, MacCallum JK, Tu Y, Jiang AC, Yang Y, Xiao T, Li J, Wang Q, Qu J. Primary treatment of acute dacryocystitis by endoscopic dacryocystorhinostomy with silicone intubation guided by a soft probe. Ophthalmology. 2009;116(1):116–122. doi: 10.1016/j.ophtha.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 11.Woo KI, Maeng HS, Kim YD. Characteristics of intranasal structures for endonasal dacryocystorhinostomy in asians. Am J Ophthalmol. 2011;152(3):491–498. doi: 10.1016/j.ajo.2011.02.019. [DOI] [PubMed] [Google Scholar]
- 12.Sonkhya N, Mishra P. Endoscopic transnasal dacryocystorhinostomy with nasal mucosal and posterior lacrimal sac flap. J Laryngol Otol. 2009;123(3):320–326. doi: 10.1017/S0022215108003897. [DOI] [PubMed] [Google Scholar]
- 13.Ramakrishnan VR, Hink EM, Durairaj VD, Kingdom TT. Outcomes after endoscopic dacryocystorhinostomy without mucosal flap preservation. Am J Rhinol. 2007;21(6):753–757. doi: 10.2500/ajr.2007.21.3095. [DOI] [PubMed] [Google Scholar]
- 14.Kansu L, Aydin E, Axci S, Kal A, Gedik S. Comparison of surgical out comes of endonasal dacryocystorhinostomy with or without mucosal flaps. Auris Nasus Larynx. 2009;36(5):555–559. doi: 10.1016/j.anl.2009.01.005. [DOI] [PubMed] [Google Scholar]


