Abstract
Background
Little is known about why surrogate decision makers for patients with advanced illness often have overly optimistic expectations about prognosis.
Objective
To determine how surrogates interpret prognostic statements and to explore factors influencing surrogates’ interpretations of grim prognostic information.
Design
Multicenter, mixed-methods study.
Setting
Intensive care units of 3 hospitals in San Francisco, California.
Participants
80 surrogates of critically ill patients.
Measurements
Participants recorded their interpretation of 16 prognostic statements using a standard probability scale. Generalized estimating equations were used to determine whether participants interpreted statements more optimistically as the expressed probability of survival decreased. Fifteen surrogates whose responses exhibited this trend participated in a semistructured interview.
Results
Participants’ interpretations of prognostic statements expressing a low risk for death were relatively accurate, but interpretations of statements conveying a high risk for death were more optimistic than the actual meaning (P < 0.001; generalized estimating equation model). Interpretations of the statement “90% chance of surviving” did not differ from the actual meaning, but interpretations of “5% chance of surviving” were more optimistic and showed substantial variability (median, 90% [interquartile range, 90% to 95%; P = 0.11] vs. 15% [interquartile range, 5% to 40%; P < 0.001], respectively). Two main themes from the interviews explained this trend: surrogates’ need to register optimism in the face of a poor prognosis and surrogates’ belief that patient attributes unknown to the physician would lead to better-than-predicted outcomes.
Limitation
Surrogates’ interpretations were elicited in an experimental setting rather than during actual clinician–surrogate conversations.
Conclusion
Inaccurate interpretations of physicians’ prognostications by surrogates arise partly from optimistic biases rather than simply from misunderstandings.
Primary Funding Source
National Heart, Lung, and Blood Institute.
Surrogate decision makers for patients with advanced critical illness are frequently asked to determine whether use of life support is consistent with a patient’s values and goals. Answering this question requires a clear understanding of not only the patient’s values but also the likely outcomes of treatment. Previous research has shown that prognostic information affects decisions to withhold or withdraw life support (1–3). However, discordance about prognosis between physicians and surrogate decision makers in intensive care units (ICUs) is common (4, 5).
Medical commentators have often attributed this discordance to surrogates’ misunderstandings about physicians’ prognostications (4, 5). This is a plausible explanation because physicians use diverse types of language to disclose prognostic information (6), and previous studies have documented wide variation in how laypeople interpret qualitative prognostic statements (7–9). Although these findings have compelled some commentators to advocate for the use of numerical prognostic statements (10), it is uncertain whether numerical risk statements are interpreted more precisely than qualitative probability statements.
It is also possible that the prevalent physician–surrogate discordance about prognosis is due to other factors. For example, recent evidence suggests that different explanatory models of illness may contribute to discordance about prognosis (3, 11–13). Another possibility is that psychological processes, such as optimism or denial, may contribute. Recent studies assessing the expectations of participants in phase 1 and 2 clinical cancer trials for therapeutic benefit have demonstrated substantial overestimation of the likelihood of positive clinical response, which was driven in part by a need to “register optimism” (14, 15). The possibility that similar processes may be at play in the context of surrogate decision making about clinical care has not been systematically examined.
We therefore conducted this study to determine how surrogates interpret prognostic statements and to explore what factors influence surrogates’ interpretations of grim prognostications by physicians.
Methods
Design Overview
Between 3 June 2006 and 11 January 2009, we conducted a multicenter, mixed qualitative and quantitative study in 3 California hospitals. Investigators obtained consent from each patient’s attending physician before approaching potential participants. Written consent from participants was obtained before enrollment. Institutional review boards at each participating center approved all study procedures.
Setting and Participants
Hospital sites were the medical-surgical ICUs of a Veterans Affairs hospital, a tertiary academic hospital, and a public county hospital. Participants were eligible if they spoke English well enough not to require the use of an interpreter when interacting with health care providers; were at least 18 years of age; were involved in decision making for an incapacitated, critically ill patient; and were present in the hospital. Participants were excluded if they could not fill out a questionnaire and participate in an interview.
Sampling
Study investigators identified eligible surrogates of critically ill patients by screening on 1 day per week at each institution on a rotating basis. We developed a protocol for a standardized screening process in which 1 researcher walked through the ICU in an identical standardized pass to determine whether the surrogate for each patient was present in the ICU or waiting room. When we identified a surrogate, we contacted the patient’s attending physician for permission to approach the surrogate. Surrogates who agreed to participate completed study procedures in a private room adjacent to the ICU. At each institution where data were collected, beds are filled on a first-come, first-served basis. Researchers screened at each site for approximately 1 month and then rotated to the next site. We screened for a total of 62 weeks.
We estimated an enrollment of 80 participants to detect a 5-point difference between the mean interpretation and the actual meaning of the quantitative prognostic statement “50% chance of surviving,” assuming a power of 0.8, a 2-sided α value of 0.05, and an estimated SD of 15. Enrollment in the qualitative portion of the study was continued until thematic saturation was achieved. Thematic saturation is defined as the point at which no new themes or ideas emerge from additional interviews (16).
Questionnaire
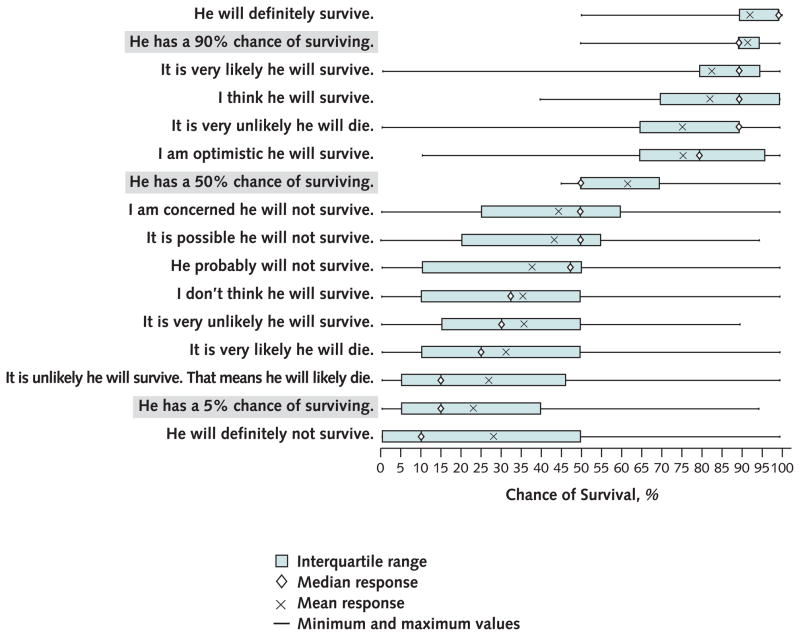
We selected 16 prognostic statements that are representative of the language used by physicians when discussing prognosis with surrogates, as identified in our earlier research (17, 18). Figure 1 shows the prognostic statements used in this study.
Figure 1.
Surrogate decision makers’ interpretations of physicians’ prognostic statements.
Before administering the questionnaire, investigators clarified with participants that all prognostic statements were hypothetical and unrelated to their loved one’s prognosis. Each prognostic statement was displayed individually on a page in the questionnaire with the phrase, “If a doctor says X, what does that mean to you?”, with X taking the place of a prognostic statement. For example, for the prognostic statement “He will definitely survive,” the questionnaire read: “If a doctor says ‘He will definitely survive’, what does that mean to you?” Below each statement was a standardized probability scale ranging from 0% to 100% in 10% increments, anchored on the left with the phrase “Will NOT survive (0% chance of survival)” and on the right with the phrase “Will survive (100% chance of survival).” Participants were instructed to place a mark on the probability scale corresponding to the patient’s chances of survival.
To avoid ordering bias in responses, prognostic statements were arranged in 3 random, computer-generated orderings. Researchers drew a number from an envelope to determine which ordering of the questionnaire the participant would receive.
Interviews
After participants completed the questionnaire, an investigator screened responses to identify instances in which participants’ interpretation of quantitative statements differed from the actual meaning. For example, for the statement “He has a 5% chance of surviving,” investigators screened for interpretations that differed positively or negatively from the expected response of 5%; those participants were invited to participate in a semistructured interview to elucidate the reasons for the discrepancy between the actual meaning of the prognostic statement and the participant’s interpretation. This interview occurred immediately after completion of the questionnaire.
To ensure consistency, a single investigator conducted all interviews using a semistructured format. Participants’ responses to the quantitative prognostic statements (90%, 50%, and 5% chance of surviving) were placed in front of the participant. The participants were read the following standardized prompt: “Please take a moment and look at your responses. Can you tell me a bit about why you put the marks where you did?” The interviewer used techniques of cognitive interviewing (19) to pursue and clarify emergent themes as they arose.
Statistical Analysis
To determine whether a participant’s interpretation of quantitative prognostic statements differed from the actual meaning, we used the Wilcoxon signed-rank test for non-parametric data. For example, for the statement “5% chance of surviving,” the null hypothesis was that there was no difference between the median interpretation from participants and the actual meaning of the statement (5% chance of surviving).
To determine whether there was a trend toward increasingly optimistic interpretation of quantitative statements as the expressed risk for death increased, we used generalized estimating equations, which allowed us to account for the potential correlation within an individual participant’s responses. We also tested for differences in responses among the 3 quantitative prognostic statements by comparing the results from each of the 3 possible comparisons (for example, comparing the responses to “90% chance of surviving” with those to “50% chance of surviving” and the remaining 2 responses). We first standardized responses by subtracting each participant’s interpretation from the actual meaning of the prognostic statement and then divided the difference by the sample SD. All analyses were executed by using SAS software, version 9.2 (SAS Institute, Cary, North Carolina).
We used constant comparative methods to develop a framework to describe the reasons for surrogates’ interpretations of quantitative prognostic statements that diverged from the actual meaning. Constant comparison is a general method for developing theory inductively from data that are systematically gathered and analyzed; it is often used when existing conceptual frameworks are inadequate (19, 20). We implemented constant comparative methods as follows: Two investigators independently developed a preliminary framework by coding a subset of 5 interviews and, through a series of investigator meetings, arrived at consensus on the final coding framework (19, 21). This framework consisted of 4 codes, 1 for each of the themes described in Table 1.
Table 1.
Surrogates’ Explanations for Overly Optimistic Interpretations of Grim Prognostic Statements
| Need to express optimism |
| “I always hope for the best outcome for my husband. Even with [a] five percent chance of survival there is still hope. I hold onto hope strongly.” |
| “I guess I understand that [the patient] may eventually die … I guess I just have to hope more.” |
| Belief that patients’ fortitude will lead to better-than-predicted outcomes |
| “I do think that a person’s will to live and their ability to survive very stressful situations can have an impact on whether they are going to survive or not. And we are talking about my father in this case, not just any patient. I know that my father could do better than what the doctor is saying … and I think he will.” |
| Disbelief of physicians’ ability to prognosticate |
| “Ultimately I don’t think [doctors] can really know the percent chance of survival unless someone comes in dead.” |
| “Whenever you get into a percentage, that’s always an iffy proposition. I think any physician would probably tell you that if they say 35%’ to you that they’re not really giving you a real figure because they really couldn’t say … exactly.” |
| Interpretation of prognosis as a “gist” estimate rather than a precise estimate |
| “If the doctor says he has a 5% chance of surviving, I find that to be a very difficult statement. I don’t know what the doctor is referring to so I am just readjusting the statement in my own mind based on the understanding that there is small chance that the patient is going to make it. I am still not having the patient have a great chance of survival, but they have some.” |
| “I don’t give a lot of weight to the individual number. I tend not to trust the individual number as much as the overall feeling that [the physician] is conveying. When [the physician] says 90%, I’m not thinking 9 out [of] 10, I’m thinking that [the physician] is very confident but not entirely sure. So for me that is the important part, not the number. I want that meaning.” |
To assess intercoder reliability, 2 investigators coded a random sample of 50% of transcripts. We then used κ statistics to numerically measure intercoder agreement (22).
Role of the Funding Source
This research was supported by grants from the National Heart, Lung, and Blood Institute, the Greenwall Foundation, and the University of California Berkeley–University of California San Francisco Joint Medical Program. The authors had full responsibility in designing the study; collecting, analyzing, and interpreting the data; writing the manuscript; and deciding to submit the manuscript for publication.
Results
Participant Characteristics
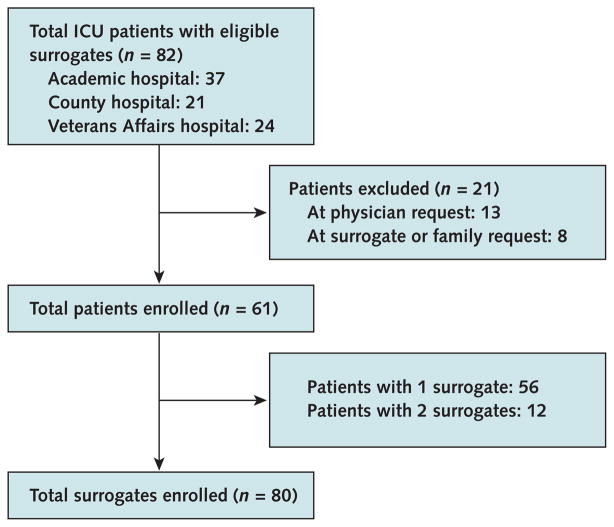
Among 82 total eligible patients, the families of 13 (16%) were not approached at the request of the attending physician and 8 (10%) surrogates declined to participate (Figure 2). The overall enrollment rate was 74%. In 12 cases, the patient’s family indicated that 2 individuals shared the responsibilities of surrogate decision making, and therefore we enrolled both surrogates. Table 2 describes the demographic characteristics of the participants and the patients.
Figure 2. Study flow diagram.
ICU = intensive care unit.
Table 2.
Surrogate and Patient Characteristics*
| Characteristic | Value |
|---|---|
| Surrogates (n = 80) | |
|
| |
| Mean age (SD), y | 53.8 (14.3) |
|
| |
| Sex | |
|
| |
| Male | 46 (58) |
|
| |
| Female | 34 (42) |
| Race or ethnicity† | |
|
| |
| Caucasian or white | 39 (48.8) |
|
| |
| African American or black | 16 (20) |
|
| |
| Hispanic or Latino | 13 (16.3) |
|
| |
| Asian | 7 (8.6) |
|
| |
| Native American | 3 (3.8) |
|
| |
| Other/undocumented | 3 (3.8) |
|
| |
| Pacific Islander | 1 (1.3) |
|
| |
| Relationship to patient | |
| Spouse/partner | 23 (28.8) |
|
| |
| Sibling | 16 (20) |
|
| |
| Child | 15 (18.8) |
|
| |
| Parent | 7 (8.8) |
|
| |
| Other relative | 7 (8.8) |
|
| |
| Other | 7 (8.8) |
|
| |
| Friend | 5 (6.3) |
| Level of education | |
|
| |
| 8th grade or less | 0 (0) |
|
| |
| Some high school | 6 (7.5) |
|
| |
| High school diploma or GED | 20 (25) |
|
| |
| Some college or trade school | 26 (32.5) |
|
| |
| 4-year college degree | 13 (16.3) |
|
| |
| Graduate or professional school | 15 (18.8) |
| Primary language‡ | |
|
| |
| English | 75 (93.7) |
|
| |
| Spanish | 8 (10) |
|
| |
| Other | 7 (9) |
|
| |
| Religious preference | |
| Christian | 25 (31.3) |
|
| |
| Protestant | 20 (25) |
|
| |
| Catholic | 12 (15) |
|
| |
| No religious affiliation | 10 (12.5) |
|
| |
| Other | 7 (8.8) |
|
| |
| Declined response | 6 (7.5) |
|
| |
| Importance of religion in everyday life§ | |
| Declined response | 8 (10) |
|
| |
| Not at all important | 4 (5) |
|
| |
| Not too important | 12 (15) |
|
| |
| Fairly important | 26 (32.5) |
|
| |
| Very important | 30 (37.5) |
| Patients (n = 61) | |
| Mean age (SD), y | 66.3 (18.2) |
| Sex | |
|
| |
| Male | 34 (56) |
|
| |
| Female | 17 (44) |
|
| |
| Admitting diagnosis | |
|
| |
| Heart failure/myocardial infarction | 19 (31) |
|
| |
| Intracranial aneurysm/hemorrhage | 7 (11) |
|
| |
| Sepsis/infection | 7 (11) |
|
| |
| Respiratory failure | 7 (11) |
|
| |
| Trauma | 5 (8) |
|
| |
| Renal failure | 5 (8) |
|
| |
| Gastrointestinal bleeding | 5 (8) |
|
| |
| Other | 6 (10) |
|
| |
| Race or ethnicity† | |
|
| |
| Caucasian or white | 30 (49) |
|
| |
| African American or black | 12 (20) |
|
| |
| Hispanic or Latino | 10 (16) |
|
| |
| Asian | 3 (5) |
|
| |
| Native American | 3 (5) |
|
| |
| Pacific Islander | 2 (3) |
|
| |
| Other/undocumented | 1 (2) |
Unless otherwise noted, values are numbers (percentages).
Sums are greater than the total surrogates or patients because some individuals identified with more than 1 race/ethnicity.
Sums are greater than the total surrogates or patients because some individuals cited more than 1 primary language.
Surrogates’ religiosity was assessed with the following question, answered on a 4-point Likert scale: How important are religious or spiritual beliefs in your everyday life?
Surrogates’ Interpretation of Prognostic Statements
Figure 1 illustrates participants’ interpretations of the 16 prognostic statements. Participants’ interpretations of both quantitative and qualitative prognostic statements varied substantially, as demonstrated by the wide inter-quartile ranges (IQRs).
Quantitative Prognostic Statements
Interpretation of the statement “90% chance of surviving” did not differ substantially from the expected response (median, 90% [IQR, 90% to 95%]; P = 0.11). Sixty percent of surrogates interpreted the statement accurately (that is, as indicating a 90% chance of surviving) and 26% answered more optimistically. Participants’ interpretation of the statement “50% chance of surviving” was more optimistic than expected (median, 50% [IQR, 50% to 70%]; P < 0.001). Fifty-nine percent of participants answered accurately and 40% answered more optimistically than the actual meaning. Participants’ interpretation of “5% chance of surviving” was more optimistic than the actual meaning and was interpreted with the most variability (median, 15% [IQR, 5% to 40%]; P < 0.001). Twenty-two percent of surrogates interpreted the statement accurately and 65% answered more optimistically than the actual meaning.
Fifteen percent (12 of 80) of participants interpreted all 3 numerical prognostic statements accurately. Thirteen percent (10 of 80) interpreted all 3 numerical prognostic statements more optimistically than the actual meaning. No participants (0%) interpreted all 3 numerical prognostic statements more pessimistically than the actual meaning. According to a generalized estimating equation, statements conveying a high or a very high risk for death (50% chance or 5% chance of surviving) were interpreted more optimistically than the statement expressing a low risk for death (90% chance of surviving; P < 0.001 for comparison). Optimism did not differ between the 5% and the 50% responses (P = 0.55).
Qualitative Explanations From Surrogates
Seven of 15 participants who completed the semistructured interviews reported being unaware of their trend toward overly optimistic interpretation of statements conveying a poor prognosis. Participants who were unaware of their overly optimistic interpretations often struggled to explain the observed findings. When shown her responses, 1 participant remarked that it was “very interesting and surprising.” Another stated, “I’m not coming up with good words to explain this [trend] because I was not aware I was doing this.” A defense contractor summarized her surprise in the following way: “I come out of a defense contractor background and I am very aware of all the variables in interpretation … But I don’t know how to explain this. You are going to have to ask me a couple more questions to figure this out.”
We identified 4 themes from participants’ comments in the semistructured interviews that explained their interpretations of prognostic statements, which are summarized in Table 1. Two themes address the trend toward overly optimistic interpretation of grim prognostic statements, including surrogates’ need to register optimism when patients are at high risk for death and surrogates’ belief that positive patient attributes lead them to outperform physicians’ grim prognostications. Two themes explain surrogates’ views that grim prognostic estimates should not necessarily be taken at face value.
To assess interrater reliability of the coding, we calculated κ statistics for each of the 4 themes. The mean κ statistic for the 4 themes was 0.83 (range, 0.81 to 0.87). A κ statistic greater than 0.8 represents excellent interrater reliability (22).
Discussion
This investigation points to several potential mechanisms beyond simple misunderstandings that may underlie the prevalent discordance between physicians and surrogates about prognosis in patients with advanced illness. The quantitative portion of the study revealed a systematic optimism bias in how surrogates interpret statements indicating a poor prognosis. The qualitative portion revealed several explanations for this finding, including surrogates’ need to register optimism when patients are at high risk for death and surrogates’ belief that positive patient attributes lead them to outperform physicians’ grim prognostications.
Perhaps the most intriguing finding of our study is the systematic bias in how surrogates interpreted grim prognostic statements. The fact that surrogates were able to accurately interpret numerical statements expressing a high probability of a good outcome, but not those expressing a high risk for death, suggests that simple misunderstandings of numerical risk information are unlikely to explain the discordance. The qualitative portion of the study pointed to psychological biases rather than misunderstandings as the cause. In aggregate, these findings challenge the prevailing assumption in the medical literature that discordance between physicians and surrogates about prognosis is due largely to unclear disclosure by physicians or simple misunderstandings by surrogates (5, 23, 24). These findings imply that helping surrogates attain realistic expectations about patients’ likely outcomes will be more complex than simply giving clear information.
We identified cognitive and psychological factors affecting how surrogates process risk information that may contribute to their overly optimistic expectations. Some surrogates seem to doubt physicians’ ability to accurately predict death. This is not necessarily irrational in light of the complexity in predicting ICU outcomes and the empirical evidence documenting physicians’ inaccuracy in prognostication (25). This finding alone does not fully explain surrogates’ optimistic interpretations, because skepticism about accuracy should result in a random distribution of interpretations rather than systematic optimism. Second, some surrogates reported that the positive attributes of the patient would help them outperform physicians’ expectations. This may express a valid insight about patient characteristics unknown to physicians. Alternatively, it may represent a cognitive bias known as illusory superiority, unrealistic optimism, or the “Lake Wobegon effect,” a cognitive bias that leads people to overestimate, in relation to others, their likelihood of experiencing positive outcomes and avoiding negative outcomes (26).
Another theme emerging during the semistructured interviews that explained surrogates’ overly optimistic interpretations of grim prognostic information was their need to express optimism. This need may represent a coping strategy to help surrogates confront the emotional difficulty of having a critically ill loved one. Alternatively, it may represent an element of “magical thinking” that there is a causal link between the prognostic estimate they record and the patient’s outcome (27). Sulmasy and colleagues (14) recently documented a similar phenomenon among participants enrolled in phase 1 and 2 clinical trials. They found that participants recorded expectations of benefit that far exceeded what could reasonably be expected in early-phase clinical trials, which seemed to be due to participants’ belief that optimism is performative or the notion that positive thoughts and expectations may actually improve the chances of benefit (14).
We found that some surrogates were not aware that they were interpreting physicians’ prognostications in optimistic ways. This suggests that the discordance about prognosis between physician and surrogates may be difficult to successfully remedy in clinical encounters without a great deal of awareness and skill by clinicians. This is especially important because not all optimism is ethically benign. In the context of surrogate decision making, unrealistic optimism may lead to decisions that do not reflect the true values of the patient. For example, if self-protection makes a surrogate emotionally unable to acknowledge when a patient has a very poor prognosis, the surrogate may request ongoing use of life support when the patient’s values suggest that a transition to comfort measures only is more appropriate.
Previous studies have reported that laypersons interpret qualitative probability statements in highly variable ways (8, 28), causing many to advocate for the use of quantitative language when communicating risk in the medical setting (10). Our findings of wide variability in how numerical statements are interpreted suggest that the magnitude of benefit in using numbers may not be as great as previously thought. Furthermore, the qualitative results reveal that for some surrogates it is the “gist” of the prognostic information (that is, the take-home message), rather than the exact numerical value, that is useful for decision making. In light of the emerging importance of gist to decision making (29, 30), as well as the frequent lack of precision in clinicians’ prognostic estimates for patients with advanced illness, there may be merit to exploring risk-communication strategies that focus on conveying the gist of the information rather than on assuring verbatim understanding of very precise prognostications.
Our study has several limitations. First, we asked surrogates to interpret hypothetical prognostic statements in a questionnaire format. This may not fully replicate the circumstances and emotional responses that arise in actual clinician–family encounters. However, all participants were actively engaged in surrogate decision making for a critically ill patient, which increases the likelihood that participants’ responses capture those experienced by surrogates in ICUs. Second, we interviewed only a subset of 15 participants about their inaccurate interpretations of quantitative prognostic statements. It is possible that interviewing a larger subset would have yielded more reasons to explain our trend or further clarified our findings. However, we reached a point of thematic saturation (16), suggesting that this is unlikely. Third, there are inherent limitations in individuals’ reported explanations for complex behaviors (31). Therefore, mechanisms other than those reported by participants could also have contributed. Fourth, we enrolled participants only within the ICU or waiting room. Surrogates who are frequently present in the hospital might differ from those who are infrequently in the hospital. Fifth, there is no gold standard for measuring individuals’ risk perceptions; we chose the probability scale because it is widely used and allows for simple statistical analysis. Finally, we studied surrogate decision makers rather than patients; it is unknown whether patients experience a different cognitive and psychological process that affects risk perception.
In conclusion, our data point to causes beyond simple misunderstandings that explain the discordance between physicians and surrogates about prognosis in patients with advanced illness. Accordingly, interventions to improve this element of decision making will probably require attention not only to the clarity with which risk information is conveyed but also to the emotional and psychological factors that affect how individuals process such information. Clinicians who communicate with surrogate decision makers in the care of incapacitated patients should be aware of the diverse causes for discordance about prognosis; researchers should develop and test communication strategies designed to attend to the emotional and cognitive biases that arise in surrogate decision making.
Context
How do surrogate decision makers interpret information about patient prognosis?
Contribution
In this multicenter study, 80 surrogates of critically ill patients were asked to use a probability scale to interpret 16 prognostic statements. Their interpretations of statements about low risk for death were reasonably accurate; however, interpretations of statements that conveyed a high risk for death, such as “a 5% chance of surviving,” were more optimistic than the actual meaning of the statement.
Caution
Statements were hypothetical and not based on actual clinician–surrogate conversations.
Implication
Surrogates may have optimistic biases that interfere with their interpretation of negative or dire prognostic information.
—The Editors
Acknowledgments
The authors thank Baruch Fischhoff, PhD, Department of Social and Decision Sciences, Carnegie Mellon University, for thoughtful comments on earlier drafts of this manuscript.
Grant Support: By grants from the National Heart, Lung, and Blood Institute (R01HL094553), the Greenwall Foundation, and the University of California Berkeley–University of California San Francisco Joint Medical Program.
Footnotes
Potential Conflicts of Interest: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M11-2047.
Reproducible Research Statement: Study protocol: Available from Dr. White (whitedb@upmc.edu). Statistical code and data set: Available to other investigators or approved individuals through written agreement by contacting Dr. White (whitedb@upmc.edu).
Author Contributions: Conception and design: L.S. Zier, D.B. White. Analysis and interpretation of the data: L.S. Zier, P.D. Sottile, S.Y. Hong, L.A. Weissfield, D.B. White.
Drafting of the article: L.S. Zier, L.A. Weissfield, D.B. White.
Critical revision of the article for important intellectual content: L.S. Zier, P.D. Sottile.
Final approval of the article: L.S. Zier, P.D. Sottile, D.B. White.
Provision of study materials or patients: L.S. Zier.
Statistical expertise: L.S. Zier, S.Y. Hong, L.A. Weissfield.
Obtaining of funding: L.S. Zier, D.B. White.
Administrative, technical, or logistic support: L.S. Zier.
Collection and assembly of data: L.S. Zier.
References
- 1.Lloyd CB, Nietert PJ, Silvestri GA. Intensive care decision making in the seriously ill and elderly. Crit Care Med. 2004;32:649–54. doi: 10.1097/01.ccm.0000115636.29294.2f. [DOI] [PubMed] [Google Scholar]
- 2.Murphy DJ, Burrows D, Santilli S, Kemp AW, Tenner S, Kreling B, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330:545–9. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- 3.Zier LS, Burack JH, Micco G, Chipman AK, Frank JA, White DB. Surrogate decision makers’ responses to physicians’ predictions of medical futility. Chest. 2009;136:110–7. doi: 10.1378/chest.08-2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274:1591–8. [PubMed] [Google Scholar]
- 5.Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–9. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 6.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. The language of prognostication in intensive care units. Med Decis Making. 2010;30:76–83. doi: 10.1177/0272989X08317012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazur DJ, Hickam DH. Patients’ interpretations of probability terms. J Gen Intern Med. 1991;6:237–40. doi: 10.1007/BF02598968. [DOI] [PubMed] [Google Scholar]
- 8.Nakao MA, Axelrod S. Numbers are better than words. Verbal specifications of frequency have no place in medicine. Am J Med. 1983;74:1061–5. doi: 10.1016/0002-9343(83)90819-7. [DOI] [PubMed] [Google Scholar]
- 9.Ohnishi M, Fukui T, Matsui K, Hira K, Shinozuka M, Ezaki H, et al. Interpretation of and preference for probability expressions among Japanese patients and physicians. Fam Pract. 2002;19:7–11. doi: 10.1093/fampra/19.1.7. [DOI] [PubMed] [Google Scholar]
- 10.Paling J. Strategies to help patients understand risks. BMJ. 2003;327:745–8. doi: 10.1136/bmj.327.7417.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boyd EA, Lo B, Evans LR, Malvar G, Apatira L, Luce JM, et al. It’s not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38:1270–5. doi: 10.1097/CCM.0b013e3181d8a217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182:905–9. doi: 10.1164/rccm.201002-0262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zier LS, Burack JH, Micco G, Chipman AK, Frank JA, Luce JM, et al. Doubt and belief in physicians’ ability to prognosticate during critical illness: the perspective of surrogate decision makers. Crit Care Med. 2008;36:2341–7. doi: 10.1097/CCM.0b013e318180ddf9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sulmasy DP, Astrow AB, He MK, Seils DM, Meropol NJ, Micco E, et al. The culture of faith and hope: patients’ justifications for their high estimations of expected therapeutic benefit when enrolling in early phase oncology trials. Cancer. 2010;116:3702–11. doi: 10.1002/cncr.25201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jansen LA, Appelbaum PS, Klein WM, Weinstein ND, Cook W, Fogel JS, et al. Unrealistic optimism in early-phase oncology trials. IRB. 2011;33:1–8. [PMC free article] [PubMed] [Google Scholar]
- 16.DeMaio TJRJ. Cognitive interviewing techniques: in the lab and in the field. In: Schwarz N, Sudman S, editors. Answering Questions: Methodology for Determining Cognitive and Communicative Processes in Survey Research. San Francsico: Jossey-Bass; 1996. pp. 177–96. [Google Scholar]
- 17.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med. 2007;35:442–8. doi: 10.1097/01.CCM.0000254723.28270.14. [DOI] [PubMed] [Google Scholar]
- 18.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. The language of prognostication in intensive care units. Med Decis Making. 2010;30:76–83. doi: 10.1177/0272989X08317012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Strauss AL, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 20.Glaser BG, Strauss AL. Discovery of Grounded Theory. Chicago: Adline; 1967. [Google Scholar]
- 21.Charmaz KC. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- 22.Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2. Boston: Little, Brown; 1991. [Google Scholar]
- 23.Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–94. doi: 10.1097/CCM.0b013e3181ab86ed. quiz 2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teno JM, Fisher E, Hamel MB, Wu AW, Murphy DJ, Wenger NS, et al. Decision-making and outcomes of prolonged ICU stays in seriously ill patients. J Am Geriatr Soc. 2000;48:S70–4. doi: 10.1111/j.1532-5415.2000.tb03144.x. [DOI] [PubMed] [Google Scholar]
- 25.Meadow W, Pohlman A, Frain L, Ren Y, Kress JP, Teuteberg W, et al. Power and limitations of daily prognostications of death in the medical intensive care unit. Crit Care Med. 2011;39:474–9. doi: 10.1097/CCM.0b013e318205df9b. [DOI] [PubMed] [Google Scholar]
- 26.Hoorans V. Self-enhancement and superiority biases in social comparison. European Review of Social Psychology. 1993;4:113–139. [Google Scholar]
- 27.Blackhall LJ, Murphy ST, Frank G, Michel V, Azen S. Ethnicity and attitudes toward patient autonomy. JAMA. 1995;274:820–5. [PubMed] [Google Scholar]
- 28.Robertson WO. Quantifying the meanings of words. JAMA. 1983;249:2631–2. [PubMed] [Google Scholar]
- 29.Reyna VF. Theories of medical decision making and health: an evidence-based approach. Med Decis Making. 2008;28:829–33. doi: 10.1177/0272989X08327069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reyna VF. A theory of medical decision making and health: fuzzy trace theory. Med Decis Making. 2008;28:850–65. doi: 10.1177/0272989X08327066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nisbett R, Wilson T. Telling more than we can know: verbal reports on mental process. Psychological Review. 1977;84:231–259. [Google Scholar]