SUMMARY
Background and Aim
To assess the success rate of implants placed in atrophic ridges, regenerated by means of block bone grafts harvested from iliac crest, calvaria or intraoral donor sites (mandibular ramus, chin).
Methods and Materials
A systematic review of all prospective and retrospective studies analyzing the success rate of implants placed simultaneously or as a second surgery following ridge augmentation by means of onlay graft technique, compared with implants placed in pristine bone, was performed. To be included, studies had to involve at least five consecutively treated patients and to report clearly specified success criteria. It was also necessary a minimum follow-up period of six months, to allow the observation of potential biological complications during function, rather than early implant failures. In order to assess the success rate of implants in terms of health of periimplant tissues, implant stability, osteointegration and bone resorption, studies reporting only the survival rate of implants, were excluded.
Results
From 323 potentially relevant studies, 65 full-text publications were screened and eight were identified as fulfilling the inclusion criteria. The success rate of implants placed in onlay graft regenerated ridges ranged from 72,8% to 97% after follow-up periods ranging from 6 months to 10 years, with all the studies but two, reporting a success rate higher than 84% (range 84–97%).
Conclusion
The obtained data demonstrated that the success rate of implants placed in regenerated areas are very similar to those obtained in case of implants placed in pristine bone, and suggested that onlay graft augmentation is a quite predictable technique to allow the placement of implants in severely atrophic areas. Despite that, the current review revealed that there are not many studies providing data on the success rate of dental implants placed in onlay graft augmented ridges and demonstrated, on average, a poor methodological quality. So randomized controlled studies adopting standardized criteria to define success and failure of implants are required and data from this review must be considered indicative.
Keywords: dental implants, success rate, onlay graft, bone block, harvesting, ridge augmentation, delayed placement, immediate placement, human
RIASSUNTO
Contenuti e obiettivi
Valutare il successo degli impianti inseriti in creste atrofiche rigenerate per mezzo di innesti ossei a blocco prelevati dalla cresta iliaca, dalla calvaria o da siti donatori intraorali (ramo della mandibola, mento).
Materiali e metodi.
È stata eseguita una revisione sistematica di tutti gli studi (prospettici e retrospettivi) che hanno analizzato il successo di impianti posizionati, contemporaneamente o in un secondo intervento chirurgico, in creste atrofiche aumentate mediante la tecnica di innesto onlay, comparati con impianti posizionati in osso nativo che non necessitava di rigenerazione. Per essere inclusi, gli studi dovevano presentare almeno cinque pazienti trattati e dovevano designare precisi criteri di successo. Un periodo di follow-up minimo di sei mesi (dopo funzionalizzazione protesica) doveva essere presente, per consentire soprattutto l'osservazione di eventuali complicanze durante il carico piuttosto che fallimenti immediati. Al fine di valutare il successo degli impianti in termini di salute dei tessuti perimplantari, stabilità dell'impianto, osteointegrazione e riassorbimento osseo, sono stati esclusi dal presente lavoro tutti quegli studi studi che riportavano solo la sopravvivenza degli impianti.
Risultati
Dei 323 studi potenzialmente rilevanti, sono state esaminate 65 pubblicazioni full-text, di cui otto sono state identificate come rispondenti ai criteri di inclusione. Il successo degli impianti collocati in innesti onlay varia (follow-up da 6 mesi a 10 anni) dal 72,8% al 97%, ma in tutti gli studi, eccetto due, si è rilevata una percentuale di successo superiore al 84% (range 84–97%).
Conclusione
I dati analizzati dimostrano che il successo degli impianti collocati in aree rigenerate sono molto simili a quelli ottenuti in caso di impianti posizionati in osso nativo, e suggeriscono che l'aumento crestale con innesto onlay è una tecnica abbastanza predicibile per il posizionamento di impianti in aree atrofiche. Nonostante ciò, l'attuale revisione ha rivelato che non sono presenti molti studi con dati sul successo degli impianti osteointegrati posti in creste rigenerate con innesto onlay, dimostrando, inoltre, in media, una scarsa qualità metodologica degli stessi studi. Sono pertanto auspicabili e necessari studi controllati randomizzati che stabiliscano criteri uniformi per definire il successo o il fallimento degli impianti, ed i dati di questa revisione devono essere considerati indicativi.
Introduction
Dental rehabilitation of either partially or totally edentulous patients with oral implants is nowadays the best method to restore oral aesthetic and function with predictable results (Adell et al. 1981, Albrektsson et al. 1986; van Steenberghe et al. 1989, 1990; Lindquist et al. 1996; Buser et al. 1997; Arvidson et al. 1998; Lekholm et al. 1999a; Weber et al. 2000; Leonhardt et al. 2002).
However, a minimum amount of bone width and height is an essential prerequisite for the successful placement of implants. Thus, unfavourable local conditions due to atrophy, trauma and periodontal disease, may provide insufficient bone volume or unfavourable interarch relationship, which doesn’t allow a correct and a prosthodontically guided positioning of dental implants.
Many different techniques have been developed to reconstruct deficient alveolar jaws for the placement of dental implants performed either in combination or in a second stage surgery after a period of healing. The present systematic review was carried out to analyze all publications reporting the success rate of implants placed in atrophic ridges, regenerated by means of block bone grafts harvested from iliac crest, calvaria or intraoral donor sites (mandibular ramus, chin) and to compare the obtained results with those of implants placed in pristine bone.
- Focused question:
“ In patients treated with horizontal and/or vertical ONLAY GRAFT augmentation, what are the clinical outcomes, in terms of implant SUCCESS, in comparison with implants placed in pristine bone?”
Material and methods
Inclusion and exclusion criteria were defined by the Authors, before the beginning of the study according to the following protocol:
- Inclusion criteria:
All studies published in English language, based on human subject, involving more than five consecutively treated patients, were considered.
All studies analyzing the success rate of endosseus implants placed in jaws augmented by means of block bone graftswere were included.
Studies needed to report on implants with at least 6 months of loading. Because this allows to observe biological complications during function rather than early implant failures.
Studies on smokers were included.
Studies on healthy patients were included.
- Exclusion criteria:
Publications that reported the same data of later publications by the same authors and systematic reviews were not considered.
Studies reporting the results of onlay graft augmentation not followed by implant placement and/or with a post-loading follow-up period lower than six months, were excluded.
Studies reporting only the survival rate of implants or with not enough specified success criteria were not included.
Studies on medically compromised patients were excluded.
Studies about major maxillofacial reconstructions following big tissue resections in case of tumours as well as bone defects related to congenital malformations (such as cleft lip and palate or major craniofacial malformations), were excluded.
-Types of interventions:
The following augmentation procedure was considered:
Onlay Graft augmentation, to reconstruct vertical and/or horizontal defects.
According to onlay graft technique, after the surgical exposure and the removal of any irregularity of the residual ridge, either autologous or homologous bone blocks, used alone or associated with particulated bone, are stabilized by means of small bone screws. A primary, tension-free closure must be achieved to prevent wound dehiscence and graft exposure. Autologous bone may be harvested from extraoral (calvaria, ala iliaca) or intraoral (mandibular ramus, chin) donor sites.
- Types of outcome measures:
Implant success:
even though not all the studies adopted the same success criteria, they were always well specified in the included publications and when possible, the following clinical and radiographic criteria were utilized to define implant success based on a combination of the success criteria previously defined by Albrektsson et al. (1986) and adapted by Buser and co-workers (1997) as well as Karoussis et al. (2004):
Absence of mobility (Buser et al. 1990).
Absence of persistent subjective complaints (pain, foreign body sensation and/or dysaesthesia) (Buser et al. 1990).
Absence of recurrent peri-implant infection with suppuration (Buser et al. 1990).
Absence of a continuous radiolucency around the implant (Buser et al. 1990).
No pocket probing depth (PPD)>5mm (Mombelli& Lang 1994, Bragger et al. 2001).
No PPD≥5mm and bleeding on probing (BOP) (Mombelli& Lang 1994).
During the first year, a 1.5mm of vertical bone resorption was accepted. After the first year of service, the annual vertical bone loss should not exceed 0.2mm (mesially or distally) (Albrektsson et al. 1986, Albrektsson&Isidor 1994).
- Search strategy:
The search strategy incorporated searching of electronic databases, supplemented by cross-checking bibliographies of relevant review articles. A search on MEDLINE and EMBASE was conducted up to January 2010.
The search strategy for MEDLINE and EMBASE used a combination of MeSH terms and text words. The following keywords were used: “Implants”, “Dental Implants”, “Osseointegrated Implants”, “Oral Implants”, “Implant Supported Prosthesis”, “Transmucosal Implants”, “Alveolar Ridge Augmentation”, “Lateral Ridge Augmentation”, “Alveolar Ridge Atrophy”, “Regeneration”, “Bone Regeneration”, “Guided Bone Regeneration”, “Guided Tissue Regeneration”, “Barrier Membranes”, “Membranes”, “Bone Substitutes”, “Autogenous Bone Grafts”, “Allograft”, “Xenograft”, “Calvarial Bone Graft”, “Iliac Crest Graft”, “Chin Bone Grafts”, “Onlay Bone Grafts”, “Implant Outcomes”, “success rate”.
To exclude some non-relevant studies “NOT (“trauma” OR “tumor” OR “injuries” OR “cancer” OR “animal”)” was added to the research.
Studies published in English language were included.
- Selection criteria and data extraction:
The research resulted in a great amount of published studies about the topic, so a three stage screening process was performed.
At first, all the titles were screened to eliminate irrelevant publications, reviews articles and animal studies; then, all abstracts of publications selected during the first screening were analyzed, excluding studies based on the number of patients, the intervention and the outcome characteristic. In the last stage, through the analysis of the whole selected full texts, the study eligibility was based on the predetermined inclusion and exclusion criteria.
- Data synthesis and analysis:
A table with data from all the included studies was created and the results were discussed.
Results
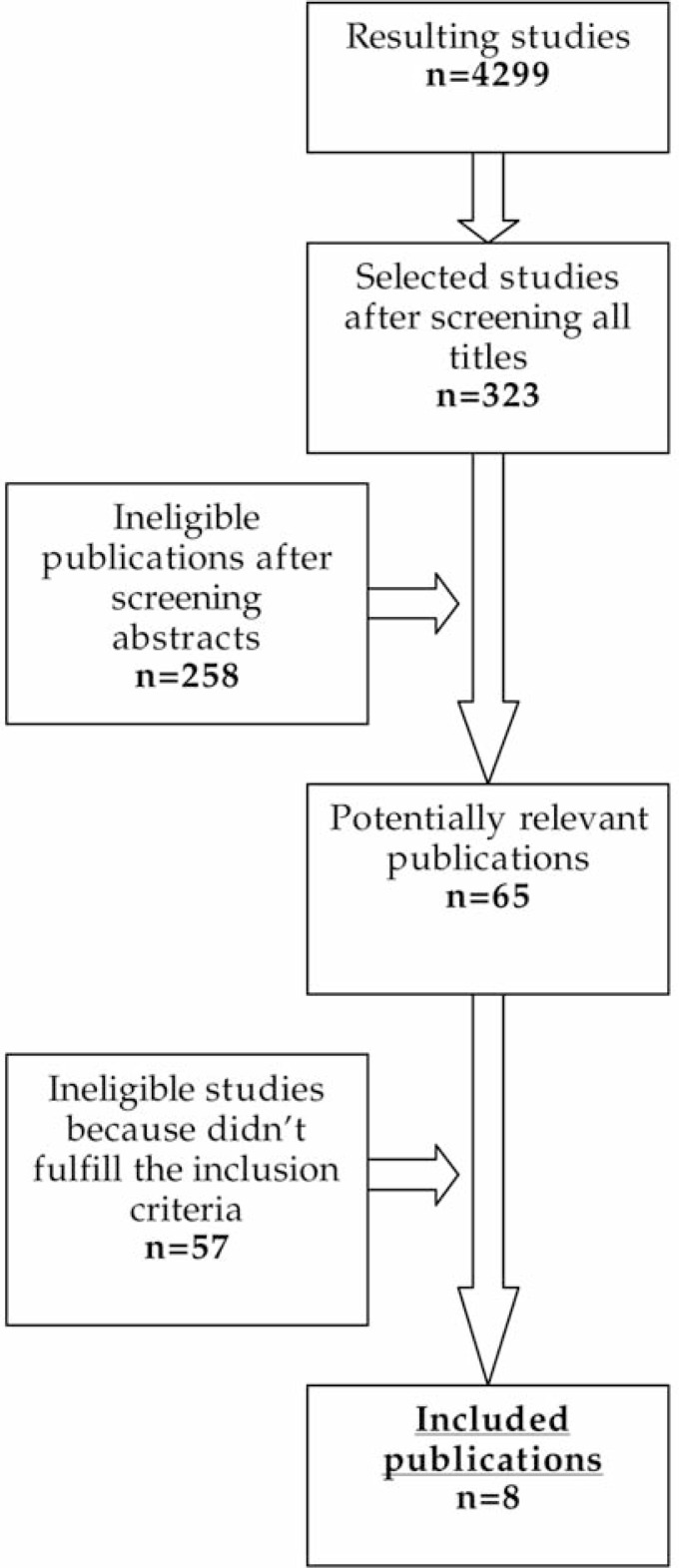
Included studies (Fig.1)
Figure 1.
Flow of studies through the review.
The investigation resulted in 4299 titles in total. Following the first stage screening of titles, 323 potentially relevant studies were identified and then, after the second stage screening, 65 full-text publications were obtained and analyzed, resulting in 8 articles fulfilling the inclusion criteria.
None of these 8 studies had a control group, in fact this review revealed that up to the date in which the research was performed there were not RCT (randomized controlled clinical trials) or CCT (controlled clinical trials) focusing on the success rate of implants placed in ONLAY grafted areas, whereas there are only few controlled studies reporting the survival rate. Therefore, the review included only prospective and retrospective cohort studies.
Ridge augmentation
Elo et al. (2009) in their study provide data about the positioning, both in mandible and maxilla, of 65 autogenous bone grafts harvested from the anterior iliac crest, the retromolar area, the tibia and the chin. The onlay technique allowed in this case the positioning of 184 implants.
In the study by Chiapasco et al. 2007, the values of vertical augmentation following the positioning of bone blocks harvested from calvaria in the area of anterior mandible (residual bone height < 5mm), are reported.
The mean bone augmentation obtained after the reconstruction procedure is 8–11 mm, with a mean resorption lower than 10% at the moment of implant positioning (6 months after the bone grafting surgery). Another study by the same Author (Chiapasco et al. 2007) provides data about the reconstruction of atrophic mandibles by means of bone blocks harvested from the mandible ramous. The mean bone gain after the procedure is 4,6 mm and the mean bone resorption before the implant positioning (4–5 months after the augmentation procedure) is 0,6 mm. After a post-loading follow up of 1 year the mean bone resorption is 0,3 mm, and after 2 and 4 years it is respectively 0,9 and 1,1 mm.
E. van der Meij et al. (2005) provide data about the positioning of bone blocks harvested from the iliac crest. The grafts have been positioned in the atrophic anterior mandibles of 17 patients, and the mean bone gain is 8,5 mm (mean augmentation of 95%).The implants (2 for each patient) have been positioned simultaneously with the grafts and the mean bone resorption after a mean post-loading follow up period of 4 years is 15%.
Chiapasco et al. (1999) in their study report data about the augmentation of atrophic maxillary and mandibular ridges by means of bone blocks harvested from either extraoral (calvaria and iliac crest) or intraoral (mandibular ramus, chin) donor sites. The mean width value before reconstruction was 2,7 mm and an average bone gain of 4 mm at the time of implant installation was recorded.
In a study by Nystrom et al. 2004, data about the augmentation of atrophic maxillary ridges by means of bone blocks harvested from the iliac crest in 30 consecutively treated patients, are reported. The implants (a total of 177) have been inserted simultaneously with the grafts and followed foran observation period of 10 years. The resorption results higher in the first three years after function and becomes stable in the following years, without other significant losses.
Triplett et al. (1996), in their study, analyze not only the success rate of dental implants placed in grafted areas, but also the success of the augmentation procedure.32 grafts have been positioned (29 harvested from the iliac crest and 3 from calvaria) in patients with atrophic ridges. After a minimum one year follow up period, 5 of the 32 grafts failed, resulting in a success of the augmentation procedure of 84,3%. In the end, Isaksson et al. (1992) reported data about the positiong in atrophic maxillas of 2 monocortical bone blocks of 4x1x1 cm harvested from the iliac crest. The mean bone resorption ranges from 0,7 and 0,9 mm 6 months after the fixture positioning and from 0,9 and 1 mm after a function period of 32–64 months.
Implants survival and success rate
In the study by Elo et al. (2009) the positioning of 184 implants in autogenous bone-grafted sites is described. A success rate (according to Albrektsson’s criteria) of 97% referred to a minimum post-loading follow up of 36 months is reported.
Chiapasco et al. (2007), in their study, report a success rate (according to Albrektsson’s criteria) of 95,7% and a survival rate of 100% (post-loading follow up of 12–24 months), referring to the positioning of 23 implants inserted in a second stage surgery after bone reconstuction.
In the other study by Chiapasco et al. (2007), data about the delayed positioning (4–5 months after the vertical regeneration procedure) of 19 implants in the mandible are reported. The success rate (according to Albrektsson’s criteria) after 24–48 months of function is 89,5%, with a survival rate of 100%.
In the study by E. van der Meij et al. (2005), data about the immediate positioning of 34 implants (2 for each patient) in the area of anterior mandible simultaneously with vertical bone augmentation by means of bone blocks harvested from the iliac crest are reported. The success rate (PPD < 5 mm and absence of periimplant radiolucency) after a mean post-loading follow up of 4 years, is 88,2%.
Chiapasco et al. (1999) in their study report data about the positioning of 44 implants placed in onlay grafted areas in a second stage surgery. After a minimum post-loading follow-up of 18 months the implant success rate (according to Alberktsson’s criteria) is 90,9%, with a survival rate of 100%.
In the study by Nystrom et al. (2004),177 implants placed simultaneously with the augmentation procedure by means of bone blocks harvested from the iliac crest.
After a follow up period of 10 years, a success rate (absence of mobility and absence of periimplant radiolucency) of 72,8% is reported. Some failures occurred, referring to the first three years after the implants positioning only in three patients, related to soft tissues traumas in the grafting area, with subsequent dehiscence during the healing period.
Triplett et al. (1996) report a success rate (absence of mobility, absence of periimplant radiolucency, absence of persistent subjective complaints, absence of suppuration), referring to 65 implants inserted simultaneously with the augmentation procedure, of 84,6%; and a success rate, referring to 110 implants placed in a second stage surgery after the ridge augmentation procedure (after a healing period of 6–9 months) of 88,2%.
In the study by Isaksson et al. (1992), 46 implants are inserted in the atrophic maxillas simultaneously with the positioning of bone blocks harvested from the iliac crest. A success rate (absence of mobility, absence of periimplant radiolucency, absence of suppuration) of 83% is reported, with the majority of failures occurring in the period between the positioning of the fixtures and the positiong of the abutments. These data suggest that ONLAY graft procedure is a quite reliable ridge augmentation technique, that allows to obtain high values of implants success-rate. However, it would not have been correct to answer to the focused question of this review, by means of the analysis of the included articles alone, but it was necessary to refer to studies reporting data about the success rate of implants placed in pristine bone (Adell et al. 1990; Chaytor et al 1991; Quirynen et al. 1992; Lekholm et al. 1994; Bragger et al. 1996; Lindquist et al. 1996; Buser et al. 1997; Arvidson et al. 1998; Behneke et al. 2000; Weber et al. 2000; Leonhardt et al. 2002); in these publications, bone resorption values and success rate of dental implants according to the limits proposed by Albrektsson et al. were reported, with cumulative success ranging from 89% to 98.9% after follow-up periods ranging from 3 to 15 years.
From the analysis of the 6 studies included in this review, resulted that the success rate of implants placed in ONLAY graft augmented ridges ranged from 72,8% and 97% after follow-up periods ranging from 6 months to 10 years, with all the studies but two, reporting a success rate higher than 84% (range 84–97%).
According to this data, there was not significant difference between the success rate of implants placed in ONLAY graft regenerated areas and that of implants placed in pristine bone.
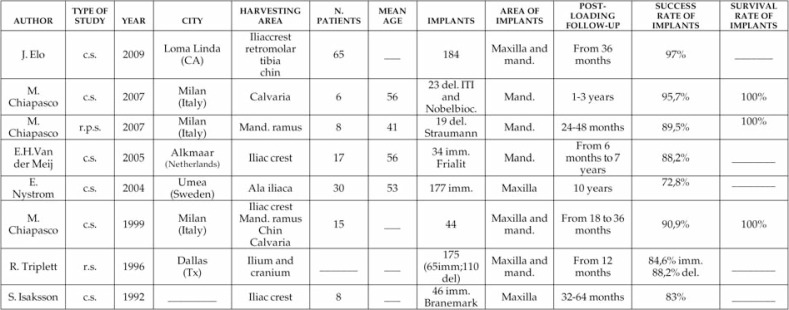
However, due to the significant heterogeneity of the obtained results, meta-analysis was not performed and the synthesis of the data was determined from the evidence table alone (Fig.2).
Figure 2.
Success rate of implants placed in ONLAY graft augmented sites. Characteristics of the included studies.
Discussion and conclusion
The analysis of the literature reveals that there are not many studies fulfilling the inclusion criteria of the present systematic review because a great amount of studies do not adopt well defined success criteria of dental implants placed in ONLAY GRAFT augmented areas. That’s why the present systematic review can only include 8 studies.
Data reported in the literature seem to demonstrate that onlay graft procedures are a reliable means for obtaining sufficient bone in case of vertical and/or horizontal defects of partially edentulous patients. So augmentation of jaw bone through the positioning of onlay grafts should be considered a reliable surgical technique to obtain bone formation and to place dental implants where otherwise it would not be possible.
In conclusion, considering the great variation of the surgical techniques and considering that very often the included studies do not specify the place and extension of the treated defects it is not possible to obtain a unique significant data about the success of onlay graft technique.
To focus on the question of the present systematic review, it is important to define the difference between the concept of survival and that of success rate. Sometimes, implants that could be considered “survived” do not satisfy the essential criteria that define the success rate of them. The survival rate of an implant is defined as its presence in the bone into the mouth. Van Steenberghe defined as survival rate “the proportion of implants still in place in a specific time, even if they do not have any function” (Van Steenberghe et al. 1999). That’s to say that either an implant that is not in function or an implant with a significant bone loss or with signs of radiolucency and/or inflammation is a survived implant. This may represent a limit in evaluating the reliability of onlay graft regeneration technique, because a high implant survival rate may not correspond to a success of the technique itself, considering that an implant can remain stable and osseointegrated even if the total amount of regenerated tissue after the surgical procedure has been resorbed.
For these reasons in this review only studies reporting well-defined implant’s success criteria were included.
The outcomes from the present review suggest that onlay graft is a quite reliable ridge augmentation technique, that allows to obtain high values of implants success-rate.
Due to the significant heterogeneity of the considered parametres in these studies, meta-analysis was not performed and the synthesis of the data was determined from the evidence table alone (Fig.2).
The analysis of available publications demonstrated, on average, the lack of universally established implant success criteria. And even if these criteria were satisfied, a control group was always absent and the post-loading follow up was often too short.
These considerations limit the results of this systematic review, but focus on the necessity in literature of studies reporting well-defined implant success rate criteria, with at least 5 years of post loading follow up, and (if possible) involving a control group. The obtained data demonstrated that onlay graft regeneration is a predictable technique to allow the placement of implants in atrophic areas. Despite that, studies with well-defined implant success criteria after a longer follow-up are required.
References
- Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981 1981 Dec;10(6):387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- Adell R, Eriksson B, Lekholm U, Brånemark PI, Jemt T. A long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. International Journal of Oral & Maxillofacial Implants. 1990;5:347–359. [PubMed] [Google Scholar]
- Albrektsson T, Zarb G, Worthington PMD, Eriksson AR. The long term efficacy of currently used dental implants: a review and proposed criteria of success. International Journal of Oral & Maxillofacial Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- Albrektsson T, Isidor F. Consensus report of session IV. In: Lang NP, Karring T, editors. Proceedings of the 1st European Workshop on Periodontology. 1994. pp. 365–369. [Google Scholar]
- Arvidson K, Bystedt H, Frykholm A, von Konow L, Lothigius E. Five-year prospective follow-up report of Astra Tech Implant Systemin the treatment of edentulous mandibles. Clinical Oral Implants Research. 1998;9:225–234. doi: 10.1034/j.1600-0501.1998.090403.x. [DOI] [PubMed] [Google Scholar]
- Behneke A, Behneke N, d’Hoedt T. The longitudinal clinical effectiveness of ITI solidscrew implants in partially edentulous patients: a 5-year follow-up report. International Journal of Oral & Maxillofacial Implants. 2000;15:633–645. [PubMed] [Google Scholar]
- Bragger U, Aeschlimann S, Burgin W, Hämmerle CH, Lang NP. Biological and technical complications and failures with fixed partial dentures FPD) on implants and teeth after four to five years of function. Clinical Oral Implants Research. 2001;12:26–34. doi: 10.1034/j.1600-0501.2001.012001026.x. [DOI] [PubMed] [Google Scholar]
- Chaytor DV, Zarb GA, Schmitt A, Lewis DW. The longitudinal effectiveness of osseointegrated dental implants. The Toronto study: bone level changes. International Journal of Periodontics & Restorative Dentistry. 1991;11:1134–1145. [PubMed] [Google Scholar]
- Chiapasco M, Gatti C, Gatti F. Immediate loading of dental implants placed in severely resorbed edentulous mandibles reconstructed with autogenouscalvarialgrafts. Clin Oral Implants Res. 2007 Feb;18(1):13–20. doi: 10.1111/j.1600-0501.2006.01293.x. [DOI] [PubMed] [Google Scholar]
- Chiapasco M, Zaniboni M, Rimondini L. Autogenousonlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a 2–4-year prospective study on humans. Clin Oral Implants Res. 2007 Aug;18(4):432–40. doi: 10.1111/j.1600-0501.2007.01351.x. Epub 2007 May 14. [DOI] [PubMed] [Google Scholar]
- Elo JA, Herford AS, Boyne PJ. Implant success in distracted bone versusautogenous bone-grafted sites. J Oral Implantol. 2009;35(4):181–4. doi: 10.1563/1548-1336-35.4.181. [DOI] [PubMed] [Google Scholar]
- Isaksson S, Alberius P. Maxillary alveolar ridge augmentation with onlay bone-grafts and immediate endosseous implants. J Craniomaxillofac Surg. 1992 Jan;20(1):2–7. doi: 10.1016/s1010-5182(05)80187-8. [DOI] [PubMed] [Google Scholar]
- Lekholm U, van Steenberghe D, Herrmann I, Bolender C, Folmer T, Gunne J, Henry P, Higuchi K, Laney WR. Osseointegrated implants in the treatment of partially edentulous jaws: a prospective 5-year multicenter study. International Journal of Oral & Maxillofacial Implants. 1994;9:627–635. [Google Scholar]
- Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, van Steenberghe D. Survival of the Brånemark implant in partially edentulous jaws: a 10-year prospective multicenter study. International Journal of Oral & Maxillofacial Implants. 1999;14:639–645. [PubMed] [Google Scholar]
- Leonhardt A, Gröndahl K, Bergstrom C, Lekholm U. Long-term follow-up of osseointegrated titanium implants using clinical, radiographic and microbiological parameters. Clinical Oral Implants Research. 2002;13:127–132. doi: 10.1034/j.1600-0501.2002.130202.x. [DOI] [PubMed] [Google Scholar]
- Lindquist LW, Carlsson GE, Jemt TA. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants. Clinical results and marginal bone loss. Clinical Oral Implants Research. 1996;7:329–336. doi: 10.1034/j.1600-0501.1996.070405.x. [DOI] [PubMed] [Google Scholar]
- Nyström E, Ahlqvist J, Gunne J, Kahnberg KE. 10-year follow-up of onlay bone grafts and implants in severely resorbed Maxillae. Int J Oral Maxillofac Surg. 2004 Apr;33(3):258–62. doi: 10.1006/ijom.2003.0512. [DOI] [PubMed] [Google Scholar]
- Quirynen M, Naert I, van Steenberghe D, Nys L. A study of 589 consecutive implants supporting complete fixed prostheses. Part I: periodontal aspects. Journal of Prosthetic Dentistry. 1992;68:655–663. doi: 10.1016/0022-3913(92)90383-l. [DOI] [PubMed] [Google Scholar]
- Triplett RG, Schow SR. Autologous bone grafts and endosseous implants: complementary techniques. J Oral Maxillofac Surg. 1996 Apr;54(4):486–94. doi: 10.1016/s0278-2391(96)90126-3. [DOI] [PubMed] [Google Scholar]
- van der Meij EH, Blankestijn J, Berns RM, Bun RJ, Jovanovic A, Onland JM, Schoen J. The combined use of two endosteal implants and iliac crest onlay grafts in the severely atrophic mandible by a modified surgical approach. Int J Oral Maxillofac Surg. 2005 Mar;34(2):152–7. doi: 10.1016/j.ijom.2004.05.007. [DOI] [PubMed] [Google Scholar]
- Weber HP, Crohin CC, Fiorellini JP. A 5-year prospective clinical and radiographic study of non-submerged dental implants. ClinicalOralImplantsResearch. 2000;11:144–153. [PubMed] [Google Scholar]