SUMMARY
Purpose
A novel technique for transcrestal guided sinus lift elevation (TGSL), is described underlining the step by step surgical protocol.
Materials and methods
TGSL modified osteotome technique was planned by the NobelProcera® Software Planning Programm (Nobel Guide, Nobel Biocare AB) and performed by stereolitographic template. The depth of the planned osteotomy was determined precisely via cross-sectional images of the elevation site to facilitate puncture of the bony sinus floor without risk of perforation of the adherent sinus membrane. A customized drilling-osteotome protocol is used to raise the Schneiderian membrane to the final implant length.
Results
The sinus membrane is successfully elevated in all sites without any iatrogenic perforation.
Conclusions
The TGSL modified osteotome technique may provide a new option for minimally invasive transcrestal sinus surgery and may represent a safe method to increase bone volume in the atrophic posterior maxilla. The results of the present study would suggest that this new surgical technique may reduce patient morbidity and extend the indications for transcrestal maxillary sinus floor elevation.
Keywords: dental implants, computer guided flapless implant placement, sinus floor elevation, expanding-condensing osteotomes
RIASSUNTO
Finalità
Viene descritto il protocollo chirurgico step by step di una nuova tecnica per l’elevazione del seno mascellare (TGSL).
Materiali e metodi
La tecnica TGSL viene pianificata con l’ausilio del software NobelClinician (NobelBiocare AB) e realizzata con la dima stereolitografica prodotta dalla pianificazione computerizzata.La profondità dell’osteotomia nel sito di elevazione del seno viene valutata sulle sezioni cross e sulle ricostruzioni 3D per facilitare la frattura controllata del pavimento del seno eliminando il rischio di perforazione della membrana. Una sequenza individualizzata di osteotomi è utilizzata per sollevare in modo atraumatico la membrana di Schneider.
Risultati
La membrana sinusale è stata sollevata con successo in tutti i siti trattati e nessuna perforazione iatrogena si è verificata.
Conclusioni
La tecnica TGSL rappresenta una nuova opzione procedurale mini-invasiva per l’elevazione transcre-stale controllata del seno e può rappresentare una metodica a ridotta morbidità postoperatoria per incrementare il volume osseo nel mascellare atrofico posteriore.
Introduction
Alveolar bone resorption and pneumatization of the maxillary sinus reduce, in many cases, the available amount of bone for the placement of dental implants in the edentulous posterior maxilla (1,2). Techniques for internal bone augmentation of the maxillary sinus floor have been established to overcome this anatomical limitation (3–7). The elevation of the sinus membrane is accomplished via either a lateral (so-called Caldwell-Luc approach) or a transcrestal approach to the antrum. The transcrestal approach is advocated as “minimally invasive” because of the undisturbed vascularization of the graft and reduced postoperative morbidity. The main concern related to minimally invasive sinus augmentation is the small amount of bone height and therefore a conventional lateral approach should be preferred in patients with severely resorbed maxillae (8). Another great concern is the risk iatrogenic perforation of sinus membrane, as the elevation is not performed under direct optical control, and because of the limited access, there is no possibility to repair the torn membrane as in the lateral surgical approach. Various modifications to the original transcrestal sinus floor elevation technique have been reported in the literature to overcome these issues: membrane elevation by inflation of a balloon catheter (9,10) and the use of hydraulic pressure (11) or negative pressure (12). Aim of this work is to describe a new technique for flapless transcrestal elevation of the maxillary sinus floor via CAD-CAM surgical templates in combination with expander-condensing osteotomes (13).
Diagnostic and clinical procedures
Nowadays computer-guided flapless surgery for implant placement using stereolithographic templates is gaining popularity among clinicians and patients. The advantages of this surgical protocol are its minimally invasive nature, accuracy of implant placement, predictability, less post-surgical discomfort and reduced time required for definitive rehabilitation (14–17). The introduction of digital systems into the diagnostic routine, and their application using three dimensional data sets of the bone topography, have made it possible to reconcile the two central aspects of planning an ideal prosthetic solution with the given anatomic situation prior to implant surgery. Three-dimensional data from a computerized tomography (CT) scan or from digital volume tomography (DVT) scan after conversion in DICOM format (Digital Imaging and Communications in Medicine) can be represented, analyzed, and used for the subsequent fabrication of a surgical template with the help of special software applications. Such surgical guides are produced in a stereolithographic process using digital data (Nobel Guide, Nobel Biocare AB) and integrate the appropriate sleeves for the implant positioning. This offers considerable advantages for both the patient and the clinician. The available bone can be used optimally and bone grafting can be avoided, or planned in advance in the best possible way if a bone graft is necessary. This results in a predictable surgical outcome, and subsequently, a restorative treatment outcome (18).
The interdisciplinary work-flow is based on an accurate surgical and prosthetic patient examination. The maxillo-mandibular casts are mounted on an semi-individual articulator and a diagnostic waxup is performed. The implant position is assessed according to the final prosthetic volume and clinical anatomy of bone and soft tissues. The radiographic guide is planned to obtain the best stability covering the buccal, oral and occlusal aspects of the residual teeth. A full palatal flange is important to achieve an optimal stability of both radiographic and surgical template. The CT scan is performed according to the double scan protocol (Nobel Guide, Nobel Biocare AB). The DICOM data are elaborated by the NobelProcera® Software Planning Programm (Nobel Guide, Nobel Biocare AB). The virtual images are inspected with a three-dimensional viewer to investigate the surgical and prosthetic needs of the patient. The clinician is able to plan the final implant position after an accurate examination of the surgical site in all the different projections. The software tools guide the clinician to obtain an ideal surgical and prosthetic compromise in order to obtain a natural look restoration with a minimally invasive approach.
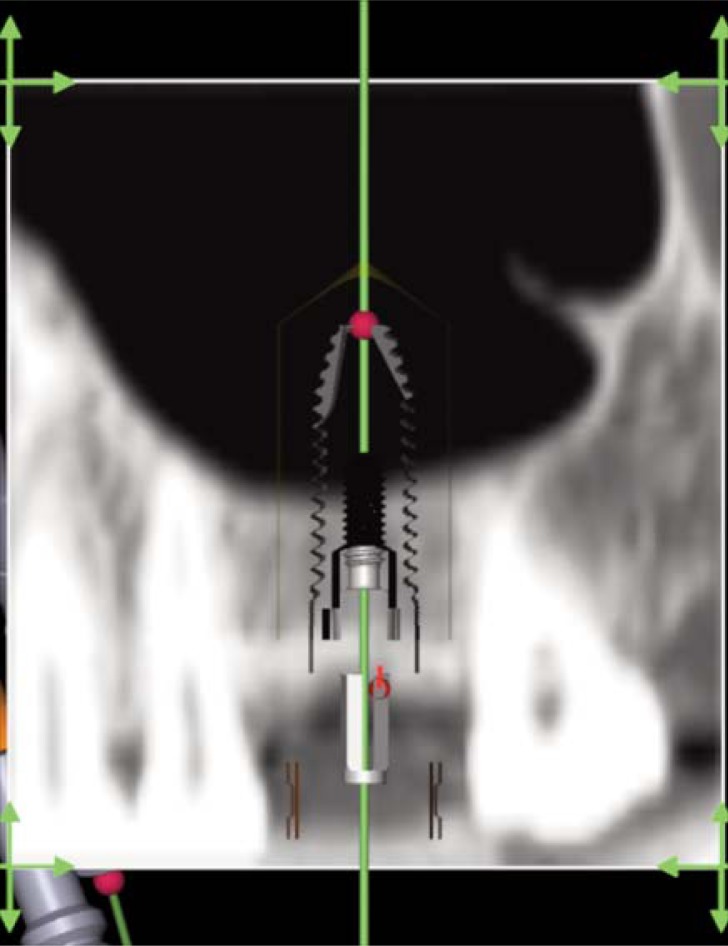
The depth of the planned osteotomy is determined precisely via cross-sectional images of the elevation site (Figs 1, 2,3), measuring on the 3D model the distance from the bone crest to the sinus floor along the implant axys. Once the treatment planning has been approved by the clinicians team, it is digitally sent to the NobelProcera® workstation (Nobel Biocare AB) to manufacture of a stereolithographic surgical template. Starting from this model the surgical template is produced in acrylic material on the basis of the radiographic guide, and containing metallic sleeves (corresponding to the location and inclination of the planned implants) in which removable stainless drill guides with varying inner diameters (corresponding precisely to the diamenters of the drills) can be fitted. The surgical template is checked for proper seating and secured in place by three horizontal stabilization pins. The stabilization of the surgical template is a key point to reproduce the virtual surgery in the mouth of the patient with high accuracy (19,20). The lost of accuracy may result from movements of the surgical guide during implant preparation. After the stabilization of the surgical template a flapless or a miniflap approach is performed at the planned elevation site. The puncture of the bony sinus floor is performed with a customized drilling protocol to the preplanned depth. The bone fracture is obtained by expanding condensing osteotomes in order to have the best control in this important step avoiding any risk of membrane perforation.
Figure 1.
Pre-Treatment Rx examination.
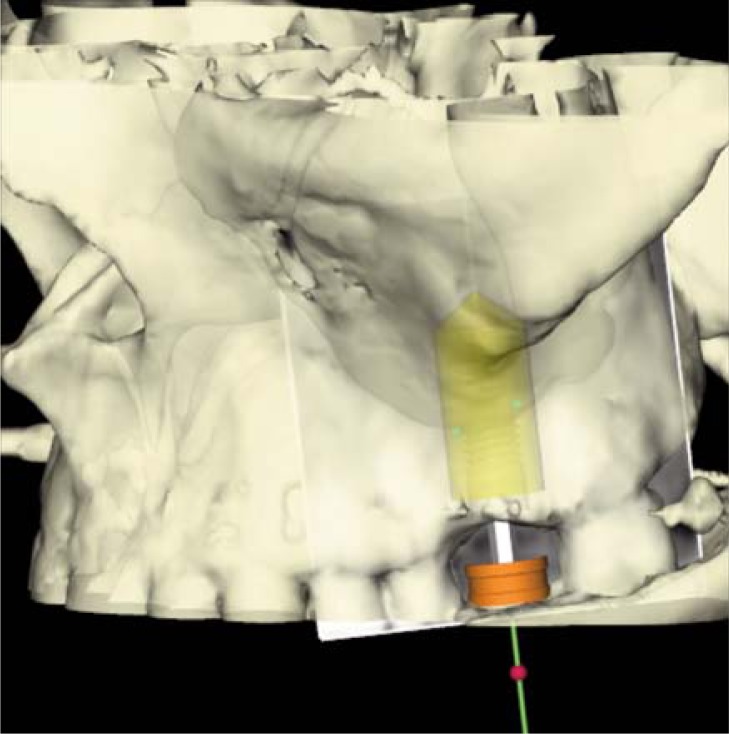
Figure 2.
3D planning and virtual surgery.
Figure 3.
Virtual surgery on TC cross section.
After that, the bony sinus floor was fractured by careful tapping using expanding-condensing osteotomes in order to have the best tactile feedback in this main step (21). To minimize or recover any injury to the Schneiderian membrane a spot of a biological glue (Tisseel, Baxter-Healthcare Corporation-Vienna/Austria) was applied at the planned depth (Fig. 4).
Figure 4.
Biological glue to preserve the schneiderian membrane.
A mean of 500 mg of grafting material (BiOss Collagene, Geistlech) was introduced and pressed into each implant site with the last osteotome working up to 1 mm to the sinus floor (Fig. 5). The hydraulic pressure exercised by the blood compressed by the grafting material, stretched the membrane and hold raised it for the law of Pascal. The mechanical and manual instruments didn’t violate in any case the sinus antrum to eliminate the risk of membrane tearing (Fig. 6). Once completed the desired membrane’s elevation the selected implant is placed via the guide sleeve of the surgical template. The immediate function is performed with an insertion torque over 40 Ncm (21).
Figure 5.
Transcrestal guide sinus grafting.
Figure 6.
Expanding condensing osteotome guide by the surgical template at the pre-planned depth.
The Rx examination after treatment (Fig. 7) confirmed the accuracy of the CAD-CAM planning and sinus lift procedure (Fig. 8).
Figure 7.
Rx examination after delivering the definitive restoration.
Figure 8.
2-years follow-up rx examination.
The definitive restoration is delivered after four months (Figs 9–10).
Figure 9.
Buccal view of the final restoration.
Figure 10.
Occlusal view of the final restoration.
Conclusions
The present study describes a new technique to elevate the maxillary sinus membrane with trans-crestal approach and simultaneous placement of endosseous implants using computer guided surgery in combination with expanding-condensing osteotomes. The advantages of the trans-crestal approach to the sinus are less alveolar resorption, better vascularization of the graft, minimal bleeding, and high patient acceptance due to its minimally invasive nature. Moreover the application of the expanding-condensing osteotomes protocol allows a safe membrane elevation in combination with an higher implant primary stability. The customized drilling protocol allows an accurate control of the working depth, reducing the risk of membrane perforation. The results of the present study would suggest that this new surgical technique may reduce patient morbidity and extend the indications for transcrestal maxillary sinus floor elevation.
This improves the predictability of sinus elevation, allowing for a better risk management and implant planning, customizing the grafting procedure according to the anatomical situation of the patient. Even if this new technique needs more investigations and follow-up up to date we have not reported any intrinsic limitation also in severely bone atrophy. These are the most important aspects of this technology, which may contribute to establish higher-quality standard in implantology.
References
- 1.Watzek G, Weber R, Bernhart T, Ulm C, Haas R. Treatment of patients with extreme maxillary atrophy using sinus floor augmentation and implants: Preliminary results. Int J Oral Maxillofac Surg. 1998;27:428–434. doi: 10.1016/s0901-5027(98)80031-3. [DOI] [PubMed] [Google Scholar]
- 2.Ferrigno N, Laureti M, Fanali S. Dental implants placement in conjunction with osteotome sinus floor elevation: A 12-year lifetable analysis from a prospective study on 588 ITI implants. Clin Oral Implants Res. 2006;17:194–205. doi: 10.1111/j.1600-0501.2005.01192.x. [DOI] [PubMed] [Google Scholar]
- 3.Rossi A, Chiapasco M. Il rialzo del seno mascellare a scopo implantologico: classificazione del deficit osseo, tecniche di trattamento e biomateriali impiegabili. Implantologia Orale. 2004;1:41–57. [Google Scholar]
- 4.Chiapasco M, et al. Il rialzo del seno mascellare a scopo implantologico. Implantologia Orale. 2005;1:9–30. [Google Scholar]
- 5.Tatum H., Jr Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986;30:207–229. [PubMed] [Google Scholar]
- 6.Summers RB. The osteotome technique. Part 3: Less invasive methods of elevating the sinus floor. Compend Contin Educ Dent. 1994;15:698–708. 247–253. [PubMed] [Google Scholar]
- 7.Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 8.Engelke W, Capobianco M. Flapless sinus floor augmentation using endoscopy combined with CT scan-designed surgical templates: Method and report of 6 consecutive cases. Int J Oral Maxillofac Implants. 2005;20:891–897. [PubMed] [Google Scholar]
- 9.Soltan M, Smiler DG. Antral membrane balloon elevation. J Oral Implantol. 2005;31:85–90. doi: 10.1563/0-773.1. [DOI] [PubMed] [Google Scholar]
- 10.Kfir E, Kfir V, Mijiritsky E, Rafaeloff R, Kaluski E. Minimally invasive antral membrane balloon elevation followed by maxillary bone augmentation and implant fixation. J Oral Implantol. 2006;32:26–33. doi: 10.1563/782.1. [DOI] [PubMed] [Google Scholar]
- 11.Chen L, Cha J. An 8-year retrospective study: 1,100 patients receiving 1,557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol. 2005;76:482–491. doi: 10.1902/jop.2005.76.3.482. [DOI] [PubMed] [Google Scholar]
- 12.Suguimoto RM, Trindade IK, Carvalho RM. The use of negative pressure for the sinus lift procedure:A technical note. Int J Oral Maxillofac Implants. 2006;21:455–458. [PubMed] [Google Scholar]
- 13.De Vico G, Bonino M, Spinelli D, Pozzi A, Barlattani A. Indicazioni e limiti all’utilizzo degli espanso-compattatori in implantologia orale. ORAL& Implantology. 2009;II(1) [Google Scholar]
- 14.Malo, et al. The use of computer guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow-up period of thirtheen months. J Prosth Dent. 2007. Jun, pp. 26–3415. [DOI] [PubMed]
- 15.van Steenberghe, et al. Flapless insertion of immediately loaded implants in maxillae. Clinical Implant Dentistry and Related Research. 2005;7(1):111–12016. [Google Scholar]
- 16.Marquardt P, et al. Three-Dimensional Navigation in Implant Dentistry. The European Journal Of Esthetic Dentistry. 2007 spring;2(1) [PubMed] [Google Scholar]
- 17.Pozzi A, Gargari M, Barlattani A. La tecnologia CADCAM nella riabilitazione implantoprotesica del paziente edentulo con un approccio biomimetico individualizzato. ORAL & Implantology. 2008;I(1):6–19. [Google Scholar]
- 18.Widmann G, Bale RJ. Accuracy in computer-aided implant surgery. A review. Int J Oral Maxillofac Implants. 2006;21:305–313. [PubMed] [Google Scholar]
- 19.Jung RE, Schneider D, et al. Computer Technology Applications in Surgical Implant Dentistry: A Systematic Review. JOMI. 2009. [PubMed]
- 20.Eggers G, et al. Accuracy of Template-Based Dental Implant Placement. The International Journal of Oral & Maxillofacial Implants. 2009;24(3):447–454. [PubMed] [Google Scholar]
- 21.Pozzi A, De Vico G, Spinelli D, Sannino G, Barlattani A. A novel technique for minimally invasive sinus grafting with immediate implant insertion and loading. IADR, 2011; San Diego, California. [Google Scholar]