Abstract
Enterobacter aerogenes resistant to cefepime (MIC, 32 μg/ml) was isolated from a patient treated with cefepime for an infection caused by a strain of E. aerogenes overproducing its AmpC β-lactamase (MIC of cefepime, 0.5 μg/ml). The AmpC β-lactamase of the resistant strain had an L-293-P amino acid substitution and a high kcat/Km ratio for cefepime. Both of these modifications were necessary for resistance to cefepime.
Enterobacter aerogenes produces an inducible chromosome-encoded AmpC cephalosporinase (12). Some isolates display high-level resistance to β-lactams owing to overproduction of the AmpC cephalosporinase or production of an extended-spectrum β-lactamase (2, 4, 6). Constitutive overproduction of the AmpC cephalosporinase confers resistance to broad-spectrum cephalosporins except cefpirome and cefepime. These antibiotics rapidly penetrate gram-negative bacteria and have a high affinity for essential penicillin-binding proteins (7, 9). However, high-level resistance to cefepime (MIC, ≥32 μg/ml) has been reported in clinical isolates in which overproduction of the AmpC cephalosporinase was combined with a lack of porins (3, 5, 11). A novel mechanism of resistance to cefepime involving changes in the structure of the AmpC cephalosporinase was recently described. One genetic event described resulted in the deletion of six amino acids from the cephalosporinase of an Enterobacter cloacae CHE clinical isolate (1). The other two described were point mutations selected in vitro in Escherichia coli harboring the ampC gene of E. cloacae (V-298-E or L-293-P substitution) (10, 15).
We describe here the selection of a clinical isolate of E. aerogenes resistant to cefepime after treatment with this β-lactam. Sequence analysis of the cephalosporinase demonstrated the presence of the L-293-P substitution previously described in the in vitro mutant (15). A strain of E. aerogenes (Ear1) resistant to broad-spectrum cephalosporins was isolated in 2001 at the Lariboisière Hospital, Paris, France, from the bronchial aspirate of a patient admitted to the neurosurgical intensive care unit. This patient was treated for 2 days with ceftriaxone (1 g/day), which was then replaced with cefepime (2 g twice a day) for 14 days. One day after the completion of this course of treatment, a second isolate of E. aerogenes (Ear2), more resistant to β-lactams, was recovered from a plugged telescoping catheter, a jugular catheter, and a rectal swab. A strain of E. aerogenes (EarCOL) overproducing its AmpC cephalosporinase, isolated from another patient, was studied for comparison. Antibiotic susceptibility patterns were determined by the disk diffusion method with Mueller-Hinton agar (Bio-Rad, Marnes-la-Coquette, France), and MICs were determined by means of the E-Test (AB BioDisk, Solna, Sweden). E. aerogenes Ear1 was resistant to β-lactams (amoxicillin, ticarcillin, and piperacillin), including broad-spectrum cephalosporins such as ceftazidime and cefotaxime, but was susceptible to imipenem, cefepime, and moxalactam (Table 1). E. aerogenes Ear2 differed from Ear1 in also being resistant to cefepime (MIC 64 times higher than that for Ear1) and being more resistant to ceftazidime (MIC 5 times higher than that for Ear1) (Table 1). No synergy was observed in the double disk diffusion method, excluding the production of an extended-spectrum β-lactamase (www.sfm.asso.fr).
TABLE 1.
MICs of β-lactams against clinical isolates of E. aerogenes EarCOL, Ear1, and Ear2; their pNH5 transformants; E. coli DH5α harboring p-EarCOL, p-Ear1, and p-Ear2; and the E. coli DH5α recipient strain
| Strain | MIC (μg/ml)a
|
|||||||
|---|---|---|---|---|---|---|---|---|
| AMX | CF | CTX | CAZ | FEP | CPO | IPM | ATM | |
| E. aerogenes Ear1 | 512 | >256 | 32 | 96 | 0.5 | 0.5 | 0.25 | 16 |
| E. aerogenes Ear2 | 512 | >256 | 32 | 512 | 32 | 12 | 0.25 | 16 |
| E. aerogenes EarCOL | >256 | >256 | >32 | 128 | 0.75 | 1 | 0.75 | 16 |
| Ear1/pNH5 | 4 | 3 | 0.125 | 0.25 | 0.064 | 0.064 | 0.25 | 0.25 |
| Ear2/pNH5 | 4 | 3 | 0.25 | 0.5 | 0.5 | 0.25 | 0.38 | 0.25 |
| E. coli DH5α/p-EarCOL | 64 | >256 | 4 | 6 | 0.25 | 0.25 | 0.38 | 1 |
| E. coli DH5α/p-Ear1 | 32 | >256 | 8 | 16 | 1 | 0.5 | 0.25 | 1 |
| E. coli DH5α/p-Ear2 | 32 | >256 | 6 | 64 | 8 | 4 | 0.38 | 2 |
| E. coli DH5α | 1 | 3 | 0.025 | 0.094 | 0.025 | 0.025 | 0.19 | 0.032 |
AMX, amoxicillin; CF, cephalothin; CTX, cefotaxime; CAZ, ceftazidime; FEP, cefepime; CPO, cefpirome; IMP, imipenem; ATM, aztreonam.
The two isolates gave strictly identical XbaI pulsed-field gel electrophoresis patterns, in accordance with the criteria of Tenover et al. (14) (data not shown). Transformation of the Ear1 and Ear2 strains with pNH5, containing the ampD gene (8), resulted in a decrease in the MICs of all of the β-lactams tested: similar decreases were observed for cefotaxime and ceftazidime, although the MIC of cefepime was eight times higher (0.5 versus 0.06 μg/ml) for Ear2 than for Ear1 (Table 1). This result suggested that resistance to cefepime was associated with the ampC gene. Furthermore, the level of resistance to cefepime in Ear2/pNH5 was lower than that in Ear2 by a factor of 64, suggesting that overproduction of the cephalosporinase was involved in resistance to cefepime.
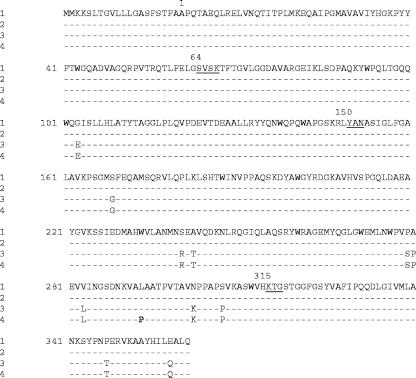
We used the published sequence of the E. aerogenes 97B ampC gene (12) to design primers E1 (5′-TGCGTGTCATAACATTATCCG-3′) and E2 (5′-AACCCGTAGCCCAGGTAAAC-3′) for amplification and sequencing of a 1,291-bp fragment (ampC gene with its promoter). The PCR products were cloned into the pCR-Blunt vector (Invitrogen, Cergy-Pontoise, France). Recombinant plasmids p-EarCOL, p-Ear1, and p-Ear2 were used to transform E. coli DH5-α. The MIC of cefepime in E. coli harboring p-Ear2 was 8 times higher than that for the p-Ear1 transformant and 32 times higher than that for the p-EarCOL transformant (Table 1). This result confirmed that resistance was conferred by the ampC gene. The sequences of the intercistronic ampC-ampR regions of the three isolates were 100% identical. The deduced amino acid sequences of the Ear1 and Ear2 cephalosporinases differed from those of EarCOL and E. aerogenes 97B (accession no. AF211348) by 11 identical substitutions. A twelfth substitution corresponding to the replacement of leucine-293 with a proline was identified only in the AmpC cephalosporinases of the Ear2 strain and the p-Ear2 transformant (Fig. 1). Thus, the observed level of resistance to cefepime in the p-Ear2 transformant resulted from this single base pair change. This substitution has been described by Vakulenko et al. in the in vitro AmpC variant, which displayed a level of resistance to cefepime similar to that observed in the p-Ear2 transformant (15). The cephalosporinases from Ear1 and Ear2 were purified and characterized as previously described (1). Both Ear1 and Ear2 produced large amounts of the cephalosporinase, 960 and 145 mU/mg of total protein, respectively, whereas ≤10 mU/mg of total protein is produced for inducible enzymes. However, Ear1 produced 6.6 times more enzyme than Ear2, consistent with the observations of Vakulenko et al. for the in vitro AmpC variant (15).
FIG. 1.
Multiple amino acid sequence alignment of the AmpC β-lactamases of the following strains: 1, E. aerogenes 97B (accession no. AF211348); 2, E. aerogenes EarCOL; 3, E. aerogenes Ear1; 4, E. aerogenes Ear2. Dashes indicate identical amino acids. Conserved residues of class C β-lactamases are underlined. The amino acid substitution in the Ear2 sequence is shown in boldface. Amino acids are numbered in accordance with the conventional numbering of E. cloacae P99, with the active-site serine at position 64.
On the basis of kcat values, the two β-lactamases were very similar and the data presented here are similar to what would be expected for class C enzymes. The most striking differences concerned the Km and Ki values for cephalosporins, which were generally much lower for the Ear2 enzyme. The lowest values were obtained with cephalothin and cefepime. In terms of the kcat/Km ratio, cefepime was hydrolyzed 15 times faster with the Ear2 cephalosporinase than with the Ear1 enzyme whereas the difference was much smaller for cefpirome (Table 2). The increase in this ratio resulted principally from the decrease in Km. These results are consistent with those reported by Vakulenko et al. (15). However, the Ear2 isolate was more resistant to cefepime owing to a combination of overproduction of the cephalosporinase and the ampC gene mutation. This mutation seems to have caused changes in the structure of the β-lactamase, leading to changes in the catalytic properties of the enzyme, resulting in an extension of the substrate spectrum to include cefepime. As suggested by Vakulenko et al., the structural change in the enzyme would result in more space being available to accommodate β-lactams, in particular cefepime and ceftazidime, increasing affinity and the hydrolysis rate (15). The amino acid leucine-293 is part of the S(N)KVALA sequence conserved in the AmpC β-lactamases of E. cloacae and E. aerogenes. This sequence, located close to the end of the H-10 helix in the three-dimensional structure of the cephalosporinase, is absent from the cephalosporinase of clinical isolate CHE (1). Moreover, Morosini et al. found, in the AmpC variant, a V-298-E substitution close to L-293 (10). The identified substitutions and deletion are located in the same region, suggesting that this region is a potential hot spot for determining resistance to cefepime. In conclusion, we report here the obtainment of a clinical isolate of Enterobacter sp. highly resistant to cefepime. As for the CHE clinical isolate, the high level of resistance to cefepime was associated with a combination of amino acid substitution in the AmpC cephalosporinase and overproduction of the β-lactamase. The strain was probably selected by the cefepime treatment used. Cefepime is a useful antibiotic for the treatment of infections caused by derepressed AmpC-producing enterobacteria (13). Our observations suggest that increases in the use of this β-lactam may result in the selection of strains producing extended-spectrum AmpC β-lactamases.
TABLE 2.
Kinetic parameters of β-lactamases produced by E. aerogenes clinical isolates Ear1 and Ear2 for various substrates
| Substrate | Ear1
|
Ear2
|
||||
|---|---|---|---|---|---|---|
| kcat (s−1) | Km (μm) | kcat/Km ratio | kcat (s−1) | Km (μm) | kcat/Km ratio | |
| Benzylpenicillin | 10 | 4.5 | 2.2 | 5 | 5.3 | 0.94 |
| Cephalothin | 190 | 36 | 5.2 | 50 | 7.0 | 7.1 |
| Cephaloridine | 240 | 230 | 1.04 | 255 | 96 | 2.65 |
| Cefotaxime | 0.15 | NDa | 0.15 | 10b | 0.015 | |
| Cefepime | 0.4 | 126 | 0.003 | 0.4 | 9.1 | 0.044 |
| Cefpirome | 0.3 | 25 | 0.01 | 0.5 | 23 | 0.022 |
| Ceftazidime | 16b | 9.8b | ||||
| Cefoxitin | 1.8b | 4.2b | ||||
High Ki value (>500 μM).
Ki value (micromolar).
Nucleotide sequence accession numbers
The EMBL accession numbers for the nucleotide sequences reported in this paper are AJ544161, AJ544162, and AJ544163.
REFERENCES
- 1.Barnaud, G., R. Labia, L. Raskine, M. J. Sanson-Le Pors, A. Philippon, and G. Arlet. 2001. Extension of resistance to cefepime and cefpirome associated to a six amino acid deletion in the H-10 helix of the cephalosporinase of an Enterobacter cloacae clinical isolate. FEMS Microbiol. Lett. 195:185-190. [DOI] [PubMed] [Google Scholar]
- 2.Bosi, C., A. Davin-Regli, C. Bornet, M. Mallea, J. M. Pages, and C. Bollet. 1999. Most Enterobacter aerogenes strains in France belong to a prevalent clone. J. Clin. Microbiol. 37:2165-2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charrel, R. N., J. M. Pages, P. De Micco, and M. Mallea. 1996. Prevalence of outer membrane porin alteration in β-lactam-antibiotic-resistant Enterobacter aerogenes. Antimicrob. Agents Chemother. 40:2854-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Gheldre, Y., N. Maes, F. Rost, R. De Ryck, P. Clevenbergh, J. L. Vincent, and M. J. Struelens. 1997. Molecular epidemiology of an outbreak of multidrug-resistant Enterobacter aerogenes infections and in vivo emergence of imipenem resistance. J. Clin. Microbiol. 35:152-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fung-Tomc, J. C., E. Gradelski, E. Huczko, T. J. Dougherty, R. E. Kessler, and D. P. Bonner. 1996. Differences in the resistant variants of Enterobacter cloacae selected by extended-spectrum cephalosporins. Antimicrob. Agents Chemother. 40:1289-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galdbart, J. O., F. Lemann, D. Ainouz, P. Feron, and N. Lambert-Zechowsky. 2000. TEM-24 extended-spectrum β-lactamase producing Enterobacter aerogenes: long-term clonal dissemination in French hospitals. Clin. Microbiol. Infect. 6:316-323. [DOI] [PubMed] [Google Scholar]
- 7.Hancock, R. E. W., and F. Bellido. 1992. Factors involved in the enhanced efficacy against gram-negative bacteria of fourth-generation cephalosporins. J. Antimicrob. Chemother. 29(Suppl. A):1-6. [DOI] [PubMed] [Google Scholar]
- 8.Honore, N., M. H. Nicolas, and S. T. Cole. 1989. Regulation of enterobacterial cephalosporinase production: the role of a membrane-bound sensory transducer. Mol. Microbiol. 3:1121-1130. [DOI] [PubMed] [Google Scholar]
- 9.Kessler, R. E., M. Bies, R. E. Buck, D. R. Chisholm, T. A. Pursiano, Y. H. Tsai, M. Misiek, K. E. Price, and F. Leitner. 1985. Comparison of a new cephalosporin, BMY 28142, with other broad-spectrum β-lactam antibiotics. Antimicrob. Agents Chemother. 27:207-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morosini, M. I., M. C. Negri, B. Shoichet, M. R. Baquero, F. Baquero, and J. Blazquez. 1998. An extended-spectrum AmpC-type beta-lactamase obtained by in vitro antibiotic selection. FEMS Microbiol. Lett. 165:85-90. [DOI] [PubMed] [Google Scholar]
- 11.Piddock, L. J. V., and E. A. Traynor. 1991. β-Lactamase expression and outer membrane protein changes in cefpirome-resistant and ceftazidime-resistant gram-negative bacteria. J. Antimicrob. Chemother. 28:209-219. [DOI] [PubMed] [Google Scholar]
- 12.Preston, K. E., C. C. A. Radomski, and R. A. Venezia. 2000. Nucleotide sequence of the chromosomal ampC gene of Enterobacter aerogenes. Antimicrob. Agents Chemother. 44:3158-3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanders, W. E., Jr., J. H. Tenney, and R. E. Kessler. 1996. Efficacy of cefepime in the treatment of infections due to multiply resistant Enterobacter species. Clin. Infect. Dis. 23:454-461. [DOI] [PubMed] [Google Scholar]
- 14.Tenover, F. C., R. D. Arbeit, R. V. Goering, P. A. Mickelsen, B. E. Murray, D. H. Persing, and B. Swaminathan. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233-2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vakulenko, S. B., D. Golemi, B. Geryk, M. Suvorov, J. R. Knox, S. Mobashery, and S. A. Lerner. 2002. Mutational replacement of Leu-293 in the class C Enterobacter cloacae P99 β-lactamase confers increased MIC of cefepime. Antimicrob. Agents Chemother. 46:1966-1970. [DOI] [PMC free article] [PubMed] [Google Scholar]