Abstract
Background
To evaluate the role of admission cardiotocography in intrapartum patients in detecting fetal hypoxia already present and to correlate the results of admission cardiotocography with perinatal outcome.
Materials and Methods:
It was a cross-sectional study conducted in the Labor and Maternity ward during the period 2007-2009. The study included 176 pregnant women (both high risk and low risk), admitted to the emergency department or through the outpatient department with period of gestation ≥36 weeks, in first stage of labor with fetus in cephalic presentation. All of them were subjected to an admission test, a 20 min recording of fetal heart rate and uterine contractions on cardiotocograph machine at the time of admission.
Results:
The results of the admission test were ‘reactive’ in 82.38%, ‘equivocal’ in 10.22%, and ‘ominous’ in 7.38% women. Women with the reactive admission test had low risk of intrapartum fetal distress (6.9%) as compared to 39.9% in the equivocal and 84.6% in the ominous group (P<0.001). Incidence of moderate to thick meconium stained liqor were more in ominous (61.5%) and equivocal group (33.3%) in compared to reactive group (4.8%) (P<0.001). Incidence of NICU admission was also significantly high (62%) in babies delivered from mother with ominous test group compared to those with equivocal (28%) and reactive test (3.45%) group babies. Neonatal mortality was also seen in babies born to mothers with equivocal (5.5%) and ominous (7.6%) admission test groups. Operative delivery for fetal distress was required in only 5.5% (8 of 145) woman of the reactive group, in 27.8% (5 of 18) woman of the equivocal group and in 84.6% (11 of 13) women of the ominous group.
Conclusion:
The admission cardiotocography is a simple non-invasive test that can serve as screening tool to detect fetal distress already present or likely to develop and prevent unnecessary delay in intervention. The test has high specificity and can help in ‘triaging’ fetuses in obstetric wards of developing countries with a heavy workload and limited resources.
Keywords: Admission test, cardiotocograph, fetal distress, fetal hypoxia, perinatal outcome
INTRODUCTION
Surveillance of the fetus during labor is important to ensure the delivery of a healthy baby in good condition with the minimum of intervention.1 Until the second half of 20th century, assessment of the fetal condition depended on very limited means: The growth of the uterus and its contents, the movement of the fetus perceived by the mother and the listening of the fetal heart beat with a mono or binauricular stethoscope.2
It was only when the fetal heart beat could be rather easily detected by means of ultrasound (USG) or through the application of direct electrocardiography, that cardiotocography (CTG) become popular as the method to monitor the condition of the fetus.3
Routine electronic monitoring of fetal heart rate (FHR) in labor has become an established obstetric practice in developed countries.4 Economic constraints in many parts of the world limit routine and continuous monitoring. In busy labor wards with few monitors, selection of the patients for continuous monitoring is necessary. Presently an antenatal risk classification is used for this purpose, recommending high-risk patients for continuous monitoring.5 Unfortunately, risk assessment profiles are often an insufficient tool for selection. Intrapartum fetal morbidity and mortality are not uncommon in low risk populations,4 and FHR changes and fetal acidosis might occur abruptly with the same as in high-risk group.6
Ingemarsson et al, described an alternative method of monitoring fetal heart rate during labor to pick the apparently women at risk whose fetus were compromised on admission or were likely to become compromised in labor—the Admission test (AT).7,8
The admission cardiotocogram is a short, usually 20 min, recording of the FHR immediately after admission to the labor ward.8 The main justification for admission cardiotocography is that the uterine contractions of labor put stress on the placental circulation; an abnormal tracing indicates a deficiency and hence identify fetal compromise at an early enough stage to allow intervention.9
The test was introduced as a risk screening in early labor, to detect the compromised fetus on admission and to select the women in need of continuous electronic fetal monitoring during labor.8,10 The test is commonly used for screening in many countries,11 and was introduced at a time when scientific knowledge about the test was scant, but trust in the benefits of EFM was great. No systematic assessments or evaluations were performed before the test was taken into widespread use.
The aim of our study was to evaluate the role of admission test in intrapartum patients in detecting fetal hypoxia already present at admission and to correlate the results of AT with perinatal outcome.
MATERIALS AND METHODS
The study conducted during the period 2007-2009, was a prospective, cross-sectional, single centered study at the Labor and maternity ward, Department of Obstetrics and Gynecology at Central Referral Hospital (CRH)—teaching hospital of Sikkim Manipal Institute of Medical Sciences (SMIMS), Gangtok, India. The study was approved by SMIMS ethics committee at the Central Referral Hospital. Written informed consent was obtained from the women who participated in the study. The procedures followed were in full accordance with the ethical standards laid down in the Declaration of Helsinki and its amendments.
The study included a total of 176 patients admitted to the emergency department or through the outpatient department with period of gestation ≥36 weeks, in first stage of labor with fetus in cephalic presentation. Women who were excluded from the study were USG confirmed lethal congenital anomaly of fetus, acute hypoxic states (such as abruption of placenta, cord prolapse, uterine scar rupture, etc.), multiple pregnancies, abnormal lie and presentation needing immediate caesarean section, and patients those who were identified for elective LSCS.
One hundred and seventy six pregnant women admitted in first stage of labor were recruited for this study. On admission, women's detail history including age, parity, antenatal care, menstrual, obstetric and medical history was documented. General physical examination was done. Per abdominal and bimanual examination were performed to determine the stages of labor, following which they were subjected to AT. Corometrics 170 CTG machine was used. A tracing was taken for 20 min with patient in a semilateral position in a separate room beside first stage labor room. The FHR traces thus obtained were categorized as reactive, equivocal or ominous as according to the classification proposed by National Institute of Clinical Excellence (NICE)—Clinical guideline September 2007.12
Following the AT, patients with reactive trace were monitored intermittently by auscultation for one minute every 30 min in first stage of labor and every 5 min in second stage of labor postcontraction. Cases with equivocal trace were placed on continuous CTG monitoring. In those with ominous tracings, appearance of late, significant variable or prolonged decelerations, delivery was hastened by operative or instrumental intervention depending upon stage of labor. After delivery, the liqor color, and Apgar score of each neonate were determined. Babies who were depressed at birth and whose Apgar was low (<7 at 5 min), their cord blood pH was estimated.
Fetus/neonate was considered to be distress if any one of the following were present.
Ominous FHR changes led to caesarean section (LSCS) or forceps/ventouse delivery
Presence of moderate–thick meconium stained liqor (MSL)
Apgar score at 5 min < 7
Umbilical cord arterial blood pH<7.2
Admission into neonatal intensive care unit (NICU) for birth asphyxia
Neonatal seizures within first 24–48 h
Incidence of intrapartum/neonatal mortality.
Statistical analysis
Data obtained from the study groups were analyzed and statistically verified by nonparametric Chi-square test (c2 test) with the use of computer software SPSS version 10. Statistic significance was calculated between groups with reactive, equivocal and ominous AT wherever possible. A P value of <0.05 was considered as the definition of statistical significance.
RESULTS
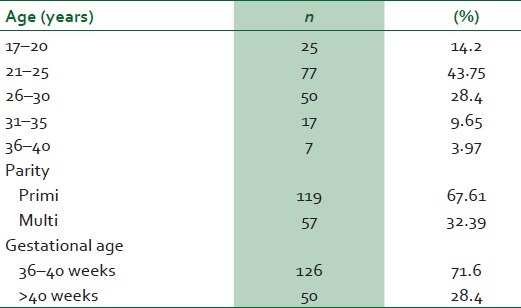
Majority of the women were primigravida (68%) between 21 and 30 years (72%) [Table 1]. Maximum 145 (82%) patients had reactive trace, 18 (10%) had equivocal trace, and where as thirteen of 176 patients (7.5%) had ominous trace on Admission test. Approximately 85% cases (11 of 13) with ominous trace on admission had fetal distress, where as nearly 39% (7 of 18) of those with equivocal AT and only 7% (10 of 145) with reactive AT had fetal distress. It is evident that incidence of fetal distress increase significantly with worsening of AT (P <0.001).
Table 1.
Demographic and clinical characteristics
Seven patients with reactive AT had mod-thick MSL liqor, only 2 babies (28.57%) in this group had Apgar score <7 at 5 min and all babies were admitted to NICU. Six cases in the equivocal group had mod-thick MSL of which 4 (66.7%) babies had 5 min Apgar <7, where as in ominous group out of 8 cases who had mod-thick MSL, 6 babies had Apgar score<7 at 5 min, and all the (100%) babies in both the groups were admitted to NICU.
Co-relation between mod-thick MSL liqor and 5 min Apgar was poor (only 28.57%) in reactive group, but the association between two was greater as the AT result worsened (75% in ominous AT). But there was strong co-relation of Apgar score <7 at 5 minute and admission to NICU in all the groups [Table 2].
Table 2.
Correlation of fetal/neonatal outcomes with admission test
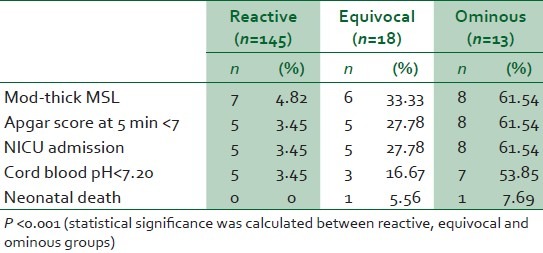
Incidence of birth asphyxia was lower (3.45%) in patients with reactive AT group than those with ominous AT trace (54%), when measured by Apgar score <7 at 5 min and/cord blood pH <7.2. Neonatal mortality was also seen in patients with equivocal trace (5.5%) and ominous AT traces (7.6%) [Table 2].
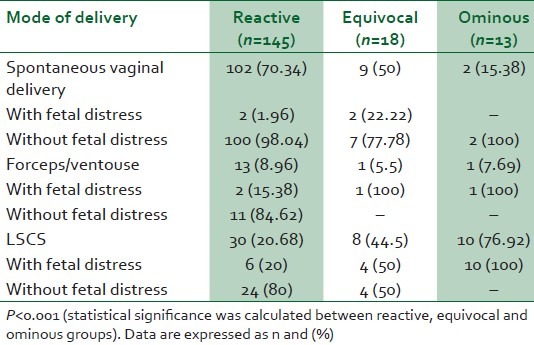
Nearly 70% cases with reactive AT had spontaneous vaginal delivery. Only 5.5% (8 out of 145) patients underwent instrumental or operative delivery in this group for fetal distress, while in the rest of the instrumental or operative deliveries indication was other than fetal distress. Fifty percent of the patients with equivocal AT had spontaneous vaginal delivery and other 50% had instrumental or operative delivery. Five of 18 (27.8%) patients in this group had operative delivery for fetal distress. In the ominous group 15.38% patients had spontaneous vaginal delivery, while 84.62% (11 out of 13) patients underwent instrumental/operative delivery for fetal distress [Table 3].
Table 3.
Mode of delivery with the results of the admission test and occurrence of fetal distress
The AT had high specificity (91%) and negative predictive value (93%), however, sensitivity and positive predictive value was low (63% and 55%, respectively).
DISCUSSION
In 1989, American Congress of Obstetricians and Gynecologist (ACOG) indicated that “fetuses of laboring women could be assessed by electronic fetal monitoring or by intermittent auscultation of fetal heart tones”.13 Auscultation, however, is necessarily intermittent, subjective and difficult to verify and document. Also in the Third World Countries like India, with busy labor wards and a minimum staff, sole reliance on auscultation is often ineffective.
EFM can detect hypoxia early and unnecessary delay in intervention can be avoided. It is a noninvasive recordable method of fetal monitoring and is a highly logical solution to the undeniable human factors/human lapses of manual fetal monitoring of labor.
Uterine contraction serve as a functional stress to the fetus; a short tracing of FHR on admission in labor ward may thus detect fetal intrauterine hypoxia already present on admission and may have some predictive value for hypoxia that may develop during labor. Based on this assumption 20 minute EFM on admission has been used as labor admission test.8
In the present study 6.9% babies from mother with reactive AT group, 38.8% babies from equivocal group, and 84.6% babies from ominous group showed evidence of fetal distress. Similar observation was made by Kusthagi et al,14 Ingemarsson et al,8 reported lowest 0.9% fetal distress in reactive group, and 50% in the ominous group. In the present study incidence of NICU admission was highest in patients with ominous AT (62%), compared to those with reactive (3.5%) and equivocal AT (27.8%). Similar rates of NICU admission were reported by Perveen et al,15 i.e., 66.67% NICU admission in ominous group and 6.6% in reactive group.
In the present study, we observed women with the reactive AT had low risk (3.45%) of developing intrapartum fetal hypoxia and significantly high risk in the ominous group (54%) when assessed by Apgar score and/ cord blood pH <7.2. Libiran MJ et al,16 also concluded that a reassuring trace is associated with low risk, (6.5%) for asphyxia when measured by Apgar score and/umbilical cord blood pH, while ominous trace is associated with high (50%) risk, for asphyxia.
In our study we noted high specificity (91%) of the admission test. Ingemarsson et al,8 also reported a very high 99.4% specificity in their studies. The high specificity of the AT means that a normal test accurately excludes adverse fetal status at the time of testing.
In this study, we did not differentiate the high-risk pregnancies from low risk. As a broad statement, on the basis of the results of this study we found that AT is useful in predicting fetal outcome in general obstetrics population. Swedish guidelines published in the year 200117 also recommend the test in all women irrespective of risk factors.
The admission CTG therefore has two potential roles. It can be used as a screening test in early labor to detect compromised fetuses on admission and to select the women in need of continuous fetal electronic monitoring during labor.18 Detractors of electronic fetal monitoring like Impey et al,19 believe that neonatal outcome is not significantly improved by the use of admission testing as compared to intermittent fetal heart rate auscultation during labor. Thacker et al,20 also feel that the use of electronic fetal monitoring is of limited effectiveness and carries an increased risk of interventions. According to them increased information at admission will not necessarily lead to better clinical outcomes. This may be true in developed countries with a population provided comprehensive antenatal care and receiving personal attention during labor. But in developing countries with inadequate antenatal care, an AT has a role in obstetric units with a heavy workload (>10 000 deliveries/year) with limited resources in ‘triaging’ fetuses by providing a ‘snap-shot’ view of fetal well-being at the time of admission in labor.21
The AT cannot be expected to predict the development of any acute asphyxial insult during the course of labor. In the absence of such acute events, an adverse fetal outcome is unlikely if the AT is normal. The result of admission CTG testing can be used to identify patients likely to develop adverse fetal outcomes and help in optimal utilization of limited labor room resources. This is particularly relevant in situations where the antenatal attendance and follow-up has been inadequate.
Ten patients with reactive AT had fetal distress in labor. It was found that in all of them admission test-delivery interval was prolonged (varied from 8 to 23 h). It can be explained from the fact that an AT cannot be expected to predict fetal distress after several hours of labor with other influential factors like problems of the cord, prolonged labor, etc., which may become operational as labor progress. So in cases where admission test delivery interval is expected to be more than 8 h, it is good to repeat CTG to detect fetal distress.
Further studies are required to define specific time interval to repeat CTG to detect fetal distress and to minimize the false negatives. Future research should emphasize on defining the role of AT in patients with specific pregnancy complications. Studies are also required to determine the convenient supplemental diagnostic modalities, which can enhance the positive predictive value of an equivocal/abnormal AT.
CONCLUSION
The admission cardiotocography is a simple noninvasive test that can serve as a screening tool to detect fetal distress already present or likely to develop and prevent unnecessary delay in intervention. Thus it helps in preventing fetal morbidity and mortality. As the test has high specificity, it has role in obstetric wards of developing countries with a heavy workload and limited resources to help in ‘triaging’ fetuses.
ACKNOWLEDGMENTS
The authors would like to thank Prof. (Dr.) B.K Kanungo (Head, Department of Obstetrics and Gynecology, SMIMS and Central Referral Hospital), all the RMOs, nursing staff of Labor and Maternity ward and all the patients who participated, making this study possible.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Whittle MJ, Martin WL. Fetal monitoring in labor. In: Chamberlain G, steer P, editors. Turnbull's obstetrics. London: Churchill Livingstone; 2001. [Google Scholar]
- 2.De Snoo K. Leerboek der Verloskunde (Text book of Obstetrics) Groningen: Wolters; 1946. [Google Scholar]
- 3.Neilson J. Cardiotocography during labor. BMJ. 1993;306:347–8. doi: 10.1136/bmj.306.6874.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingemarsson E. Routine electronic fetal monitoring during labor. Acta Obstet Gynecol Scand Suppl. 1981;99:1–29. doi: 10.3109/00016348109156940. [DOI] [PubMed] [Google Scholar]
- 5.Zuspan F, Quilligan EJ, James JD, van Geijn HP. Predictors of intrapartum fetal distress: The role of electronic fetal monitoring. Am J Obstet Gynecol. 1979;135:287–91. doi: 10.1016/0002-9378(79)90691-4. [DOI] [PubMed] [Google Scholar]
- 6.Edington T, Sibanda J, Beard RW. Influence on clinical practice of routine intrapartum fetal monitoring. Br Med J. 1975;3:341–3. doi: 10.1136/bmj.3.5979.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schifrin BS, Foye G, Amato J, Kates R, MacKenna J. Routine fetal monitoring in the antepartum period. Obstet Gynecol. 1979;54:21–5. doi: 10.1097/00006250-197907000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Ingemarsson I, Arulkumaran S, Ingemarsson E, Tambyraja RL, Ratnam SS. Admission test: A screening test for fetal distress in labor. Obstet Gynecol. 1986;68:800–6. [PubMed] [Google Scholar]
- 9.Prentice A, Lind T. Fetal heart rate monitoring in labour–too frequent intervention, too little benefit? Lancet. 1997;2:1375–7. doi: 10.1016/s0140-6736(87)91266-9. [DOI] [PubMed] [Google Scholar]
- 10.Phelan JP. Labor admission test. Clin Perinatol. 1994;21:879–85. [PubMed] [Google Scholar]
- 11.Berglund S, Nordström L. National survey (Sweden) of routines for intrapartum fetal surveillance. Acta Obstet Gynecol Scand. 2001;80:552–3. [PubMed] [Google Scholar]
- 12.Intrapartum care. NICE Clinical guideline No. 55. London: National Institute for Health and Clinical Excellence; 2007. National Institute for health and clinical excellence; pp. 44–5. [Google Scholar]
- 13.Intrapartum fetal heart monitoring. Technical bulletin No. 132. Washington, DC: American College of Obstetricians and Gynecologist; 1989. American College of Obstetricians and Gynecologists. [Google Scholar]
- 14.Kushtagi P, Shashibala N. Labor Admission test-an effective risk screening tool. J Indian Med Assoc. 2002;100:234–6. [PubMed] [Google Scholar]
- 15.Shakira P, Haleema H. Effectiveness of Admission test. J Dow Univ Health Sci. 2007;1:205. [Google Scholar]
- 16.Libiran MJ, Solis MS, Santos RR, Baga EB. Admission test as predictor of intrauterine fetal asphyxia. Philipp J Obstet Gynecol. 1999;3:143–9. [PubMed] [Google Scholar]
- 17.Nordström L, Waldenström U. Handläggning av normal födsel (Management of normal labour) Stockholm: Socialstyrelsen; 2001. [Google Scholar]
- 18.Blix E, Reinar L M, Klovning A, Oian P. Prognostic value of the labor admission test and its effectiveness compared with auscultation only: A systematic review. Br J Obstet Gynaecol. 2005;112:1595–604. doi: 10.1111/j.1471-0528.2005.00766.x. [DOI] [PubMed] [Google Scholar]
- 19.Impey L, Reynolds M, MacQuillan K, Gates S, Murphy J, Shell O. Admission cardiotocography: A randomized controlled trial. Lancet. 2003;361:465–70. doi: 10.1016/S0140-6736(03)12464-6. [DOI] [PubMed] [Google Scholar]
- 20.Thacker SB, Stroup DF. Revisiting the use of the electronic fetal monitor. Lancet. 2003;361:445–6. doi: 10.1016/S0140-6736(03)12465-8. [DOI] [PubMed] [Google Scholar]
- 21.Chandraharan E, Sabaratnam A. Electronic fetal heart rate monitoring in current and future practice. J Obstet Gynecol India. 2008;58:121–30. [Google Scholar]


