Abstract
Background:
The aims of this study were to determine the pattern and frequency of oral lesions and to compare the prevalence of HIV-related oral lesions in paediatric Nigerian patients on HAART with those not on HAART.
Materials and Methods:
All patients aged 15 years and below attending the Infectious Disease Clinic of Aminu Kano Teaching Hospital with a diagnosis of HIV were consecutively examined in a cross-sectional study over a 2-year period. Information was obtained by history, physical examinations, HIV testing, and enumeration of CD+ T cells. The results are presented. A P-value of <0.05 was considered significant.
Results:
A total of 105 children comprising 63 males and 42 female who met the inclusion criteria participated in the study, mean age in months was 53.3±42.2, with a mean of 3.4±2.2 for male and 2.8±1.8 for female respectively. Oral lesions occurred in 61.9% of the children Overall, 22 (21.0%) had at least one oral lesion, 43 (41.0%) had multiple lesion. The most common lesion was oral candidiasis (79.1%). The angular cheilitis (43.8%) variant was most frequent. The mean CD4 counts were 1138 cells/mm3, 913 cells/mm3 and 629 cells/mm3 for those without oral lesion, with single lesion and multiple oral lesions respectively. These differences were not statistically significant (ANOVA: F=0.185, df=2, 80, 82, P=0.831. Patients on HAART comprised about 61.9% and these were found to have reduced risk for development of such oral lesions as angular cheilitis (OR=0.76; 95% CI=0.56-1.02; P=0.03), pseudomembranous candidiasis (OR=0.71; 95% CI=0.54-0.94; P=0.024) and HIV-gingivitis (OR=0.59; 95% CI=0.46-0.75; P=0.001). HAART had some beneficial but insignificant effect on development of HIV-periodonttitis (OR=0.60; 95% CI=0.51-0.70; P=0.09). The chances of occurrence of other oral lesions were not significantly reduced by HAART (Kaposi sarcoma, OR=1.24; 95% CI=0.31-5.01; P=0.47, erythematous candidiasis, OR=1.13; 95% CI=0.62-2.06).
Conclusion:
HIV-related Oral lesions are frequently seen in HIV-infected Nigerian children. Paediatric patients receiving HAART had significantly lower prevalence of oral lesions, particularly oral candidiasis and HIV-gingivitis.
Keywords: HIV/AIDS, Nigeria, oral manifestations, paediatrics
INTRODUCTION
The HIV/AIDS pandemic has become a human, social, and economic disaster, with far reaching implications for individuals, communities, and countries. Of the 40 million people estimated to be infected with HIV by the end of 2004, children accounted for over 3 million of the total population.1 The progression of the disease is faster and more severe in children due to their developmental stage and to the immaturity of their immune system.2 Several manifestations including those of the oral tissues have been reported.3 The early diagnosis of these lesions as well as their complications should be viewed as important components in the management and treatment of affected children.3,4 Most published work on oral manifestations of HIV/AIDS is from the developed world with very little information from Africa where about 70% of HIV-infected persons reside.5 The prevalence of oral lesions varies among different authors from different parts of the globe, with figures as high as 63.0% in South African children6, Thailand7 (50.0%) and 41.7% among Nigerian children.8 Candidiasis has been consistently found to be the most common oral lesions associated with paediatric HIV/AIDS.8–10 Candidiasis in the paediatric age group range from 11.0% in Uganda11 to 63% in South Africa.6 The aims of this study were to determine the pattern and frequency of oral lesions and to compare the prevalence of HIV-related oral lesions in paediatric Nigerian patients on HAART with those not on HAART.
MATERIALS AND METHODS
Patients attending the Aminu Kano Teaching Hospital (AKTH) paediatric specialist out-patient clinic and diagnosed with HIV infection between January 2005 and December 2006 were the subjects of this study. Referred patients from screening centers in the adjoining states, who were confirmed sero-positive in AKTH, within the same period, were also recruited into the study. Approval for this study was obtained from the ethics committee of the hospital. The study protocol was adequately explained to the parents or guardian after which a written informed consent was obtained for selected participants. All patients whose parents or guardian refused participation were withdrawn from the study. HIV sero-positive status was determined by a repeatedly reactive sample on ELISA screening in addition to a positive confirmatory test by the Western immunoblot. Information on risk factors such as history of blood transfusion, circumcision, scarification, and sero-positive status of parents were also recorded. Examination of the orofacial tissues for each patient was carried out by two dental surgeons pretrained in the diagnosis of oral manifestations of HIV/ AIDS. The criteria described by Greespan et al.12 for diagnoses of oral lesions in HIV/AIDS were adopted. Information collected was captured on the WHO13 recording form for oral HIV/AIDS. Statistical analysis was carried out using SPSS version 13 software (Chicago, IL). Mean, standard deviation, range, and percentages were used to describe quantitative and qualitative data respectively. Comparative statistics was done using the Student t-test, ANOVA, and odd ratio as appropriate. A P-value of less than 0.05 was considered significant.
RESULTS
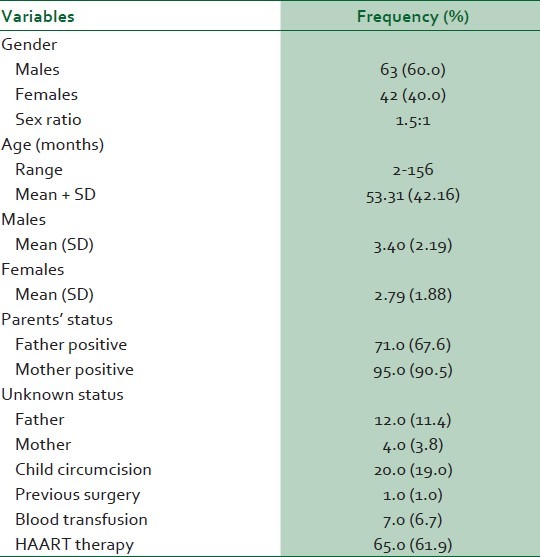
A total of 105 patients were seen over this period of study. Of these, male accounted for 63 (60%) and female 42 (40%), giving a M:F of 1.5:1. Their age ranged from 2 to 156 months with an overall mean age of 53.3±42.2 (3.40±2.2 for male and 2.8±1.8 for female). About half the patients (47.61%), were up to 40 months or below followed by the 41-60 months age group (15.24%), Table 1. There was no statistical significant difference in the mean age for males and females (t=1.481, df=103, P=0.142). When considering the potential risk factors for the transmission of HIV/AIDS, child circumcision accounted for 19.0%, previous surgery (1.0%), blood transfusion (6.7%) and 90.5% of the mothers were positive for HIV while 67.6% of the fathers were positive. HIV sero-negative status was 21.0% and 5.7% for fathers and mothers respectively [Table 2].
Table 1.
Distribution of subjects by age-grouping and sex
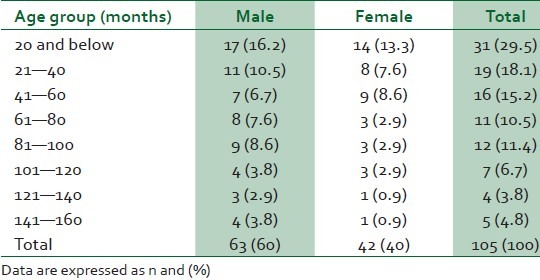
Table 2.
Demographic, risk factors, and treatment characteristics of subjects
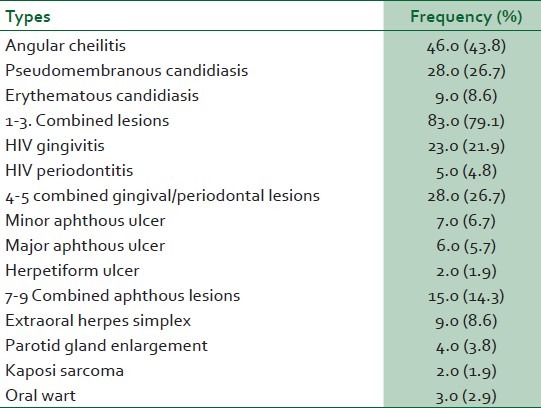
The distribution of oral lesions is shown in Table 3. Overall, 22 (21.0%) had at least one oral lesion, 43 (41.0%) had multiple lesions. The most common lesion was candidiasis (79.1%) and the angular cheilitis (43.8%) variant was most frequent. Other lesions were HIV gingivitis (21.9%), apthous ulcer (14.3%), extraoral herpes (8.6%), HIV periodontitis (4.8%), parotid enlargement (3.8%), Kaposi sarcoma (1.9%), and oral wart (2.9%). There were no oral lesions in 38.1% of the patients. The mean CD4 counts were 1138 cells/mm3, 913 cells/mm3 and 629 cells/mm3 for those without oral lesion, with single lesion and multiple oral lesions respectively. These differences were not statistically significant (ANOVA: F=0.185, df=2, 80, 82, P=0.831).
Table 3.
Distribution of oral lesion in patients
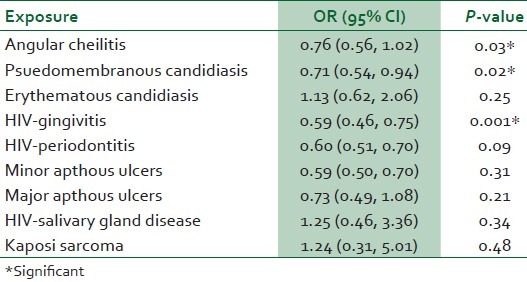
Of the 105 patients, 65 (61.9%) were on HAART. The duration of use of HAART ranged from 1 to 12 months, with about 60.0% having been on treatment for 1-6 months. Patients on HAART had reduce risk for development of such oral lesions as angular cheilitis (OR=0.76; 95% CI=0.56-1.02; P=0.03), pseudomembranous candidiasis (OR=0.71; 95% CI=0.54-0.94; P=0.024) and HIV-gingivitis (OR=0.59; 95% CI=0.46-0.75; P=0.001). Use of HAART showed some beneficial but insignificant effect on the prevalence of HIV periodontitis (OR=0.60; 95% CI=0.51-0.70; P=0.09). The chances of occurrence of other oral lesions were not significantly reduced by HAART (Kaposi sarcoma, OR=1.24; 95% CI=0.31-5.01; P=0.47, erythematous candidiasis, OR=1.13; 95% CI=0.62-2.06; P=0.25) [Table 4].
Table 4.
Effect of HAART on prevalence of oral lesions
The HAART regimen in this study was combinations of stavudine, lamivudine, and nevirapine.
DISCUSSION
Majority of the parents were HIV-positive highly suggestive that mother-to-child transmission was the dominant mode of transmission of the virus to infected children. This agrees with earlier reports in the literature.12–14 Other presumed modes of transmission were child circumcision and blood transfusion.
The prevalence of oral lesion in the present study (61.9%), while comparable to the 63.0% reported among South African children6 was a little higher than that of Thailand7 (50.0%) and American children (53.6%),15 and much higher than a previous study from Nigeria.8 These varying prevalence values could be attributed to racial, social, and geographical variations in disease presentations.8 Candidiasis has been consistently found to be the most common oral lesions associated with HIV/AIDS.9,10,16–18 Candidiasis in the paediatric age group range from 11.0% in Uganda11 to 63% in South Africa6 which is lower than the prevalence rate of 79.1% obtained from the present study. Our prevalence value for oral candidiasis also differ sharply from the result of a similar study from North Central Nigeria which reported 45.0% prevalence value among their study population.8
In contrast to most reports where the pseudomembranous variant was the most frequently seen candida infection,2,11,17–20 angular cheilitis was most common in this study, accounting for 43.8% compared with pseudomembranous candidiasis which accounted for 26.7%. The presence of HIV infection is also associated with increased prevalence of gingival/periodontal diseases which accounted for 26.7% of oral lesions in the present study. This value is higher than that reported by Bosco and Birman2 in Brazillian children, but comparable to those of Leggott21 and Fonseca et al.22
Gingival/periodontal lesions were previously reported from our environment, including Kano in northwest Nigeria, as the second most common oral lesions in adult Nigerian HIV infected patients.23,24 Interestingly, gingival/periodontal lesion was also the most common after candidiasis among children examined in the same centre. Periodontal lesions and gingivitis have been reported to be more prevalent in Africa and Asia due to poor nutrition and inadequate oral hygiene practices.18 This result contrast sharply from other studies in which HIV-salivary gland disease was second to candididal infection.10,16 Hamza et al.25 found parotid enlargement to be the most common presentation followed by candidiasis in HIV infected children in Tanzania. Salivary gland disease in the present study accounted for only 3.8% which is lower than the 7% in Ugandan Children17 and the 50% in South Africa.18 Ulcerations, which are commonly observed in AIDS, have received numerous nomenclatures. Recurrent apthous ucerations, nonspecific ulcers, unidentified ulcerations and ghost ulcerations are some of the terms used in description of oral ulcers.2,22 Reported prevalence rates of recurrent oral ulcerations in HIV infection varies partly because accurate definitive diagnosis and classification is difficult due to its varied etiology.2,22 The prevalence of 14.3% for aphthous ulceration in the present study is comparable with the 14% reported in South Africa18 and much higher than the 1% reported in Brazil.22 Less common oral lesions in HIV infected children include Kaposi sarcoma, non- Hodgkin lymphoma and oral hairy leukoplakia.25 In the present study Kaposi sarcoma was found in only 2 (1.9%) out of the 105 children examined. No case of non-Hodgkin lymphoma and hairy leukoplakia was reported in this series. The prevalence of these lesions in children differs sharply from that reported in adult populations where a higher prevalence is the normal finding.21,26 The differences may be explained in terms of geographical variations in the clinical presentations of oral lesions in both children and adults infected with HIV/AIDS.
Patients of different age groups have been reported to respond differently to highly active antiretroviral therapy (HAART) with respect to prevalence of oral lesions. In adults, there has been a decrease in the prevalence of oral candidiasis, oral hairy leukoplakia, and HIV-associated periodontal disease27,28 In children variable effects of HAART on oral lesions have been observed. While some authors reported significant reduction in prevalence of oral lesions,8,29,30 others did not observe any changes in the occurrence of HIV-related oral lesions in children receiving HAART.23,31,32 The result of the present study shows that HAART in HIV infected children significantly reduces the prevalence of angular cheilitis, psuedomembranous candidiasis, and HIV gingivitis. These lesions may possibly be used as prognostic indicators of response to HAART in children.
CONCLUSION
Oral lesions are frequently seen in HIV-infected Nigerian children. Candidiasis is the most common oral lesion associated with HIV/AIDS in the paediatric population in this environment. The clinical picture, however, differs from those reported from other parts of Africa as well as other regions of the world in that parotid enlargement is not as prominent as it is in these regions. Early recognition of these lesions and institution of appropriate treatment will go a long way in reducing the high mortality associated with HIV/AIDS in children. Children on HAART had significantly lower prevalence of oral lesions, particularly oral candidiasis and HIV-gingivitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.AIDS epidemic update. Geneva: UNAIDS/WHO; 2004. Dec, UNAIDS/Who Health Organization. [Google Scholar]
- 2.Bosco VL, Birman EG. Oral manifestations in children with AIDS and in controls. Pesqui Odontol Bras. 2002;16:7–11. doi: 10.1590/s1517-74912002000100002. [DOI] [PubMed] [Google Scholar]
- 3.dos Santos Pinheiro R, França TT, Ribeiro CM, Leão JC, de Souza IP, Castro GF. Oral manifestations in human immunodeficiency virus infected children in highly active antiretroviral therapy era. J Oral Pathol Med. 2009;38:613–22. doi: 10.1111/j.1600-0714.2009.00789.x. [DOI] [PubMed] [Google Scholar]
- 4.Chigurupati R, Raghavan SS, Studen-Pavlovich DA. Pediatric HIV infection and its oral manifestations: a review. Pediatr Dent. 1996;18:106–13. [PubMed] [Google Scholar]
- 5.Dixon S, McDonald S, Roberts J. The impact of HIV and AIDS on Africa's economic development. BMJ. 2002;324:232–4. doi: 10.1136/bmj.324.7331.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Collaborative Study. Children born to women with HIV-1 infection: Natural history and risk of transmission. Lancet. 1991;327:253–60. [PubMed] [Google Scholar]
- 7.Akpede GO, Ambe JP, Rabasa AI, Akuhwa TR, Ajayi BB, Akoma MA, et al. Presentation and outcome of HIV-infection in hospitalized infants and other children in north-eastern Nigeria. East Afr Med J. 1997;74:21–7. [PubMed] [Google Scholar]
- 8.Olaniyi TO, Sunday P. Oral Manifestations of HIV infection in 36 Nigerian children. J Clin Pediatr Dent. 2005;30:89–92. doi: 10.17796/jcpd.30.1.a75w1602n0x6577r. [DOI] [PubMed] [Google Scholar]
- 9.Ramos-Gomez F. Dental consideration for the pediatric AIDS/HIV patient. Oral Dis. 2002;8:49–54. doi: 10.1034/j.1601-0825.2002.00012.x. [DOI] [PubMed] [Google Scholar]
- 10.Naido S, Chikte U. Oro-facial manifestations in paediatric HIV: A comparative study of institutionalized hospital outpatients. Oral Dis. 2004;10:13–8. doi: 10.1046/j.1354-523x.2003.00973.x. [DOI] [PubMed] [Google Scholar]
- 11.Coogan MM, Greeenspan J, Challacombe SJ. Oral lesions in infection with human immunodeficiency virus. Bull World Health Organ. 2005;83:700–6. [PMC free article] [PubMed] [Google Scholar]
- 12.Greenspan JS, Barr CE, Sciubba JJ, Winkler JR. Oral manifestations of HIV infection: Definitions, diagnostic criteria and principles of therapy. Oral Surg Oral Med Oral Pathol. 1992;73:142–4. doi: 10.1016/0030-4220(92)90185-s. [DOI] [PubMed] [Google Scholar]
- 13.Krammer IR, Pindborg JJ, Bezrouukov V, Infirri JS. Guide to epidemiology and diagnosis of oral mucosal diseases and conditions. World Health Organization. Community Dent Oral Epidemiol. 1980;8:1–16. doi: 10.1111/j.1600-0528.1980.tb01249.x. [DOI] [PubMed] [Google Scholar]
- 14.Scott GB, Hutto C, Makuch RW, Mastrucci MT, O’Connor T, Mitchell CD, et al. Survival in children with perinatally acquired human immunodeficiency virus type 1 infection. N Engl J Med. 1989;321:1791–6. doi: 10.1056/NEJM198912283212604. [DOI] [PubMed] [Google Scholar]
- 15.Holmes HK, Stephen LX. Oral lesions in developing countries. Oral Dis. 2002;8:40–3. doi: 10.1034/j.1601-0825.2002.00010.x. [DOI] [PubMed] [Google Scholar]
- 16.Reichart PA, Khongkhunthian P, Bendick C. Oral manifestations in HIV-infected individuals from Thailand and Cambodia. Med Microbiol Immunol. 2003;192:157–60. doi: 10.1007/s00430-002-0168-4. [DOI] [PubMed] [Google Scholar]
- 17.Ramos-Gomez FJ, Flaitz C, Catapano P, Murray P, Milnes AR, Dorenbaum A. Classification, diagnostic criteria and treatment recommendation for orofacial manifestations in HIV-infected paediatric patients. Collaborative Workshop on Oral Manifestations of Paeditric HIV infections. J Clin Pediatr Dent. 1999;23:85–96. [PubMed] [Google Scholar]
- 18.Chen JW, Flaitz CM, Wullbrandt B, Sexton J. Association of dental health parameters with oral lesions prevalence in human immunodeficiency virus-infected Romanian children. Pediatr Dent. 2003;25:479–84. [PubMed] [Google Scholar]
- 19.Ranganathan K, Hemalatha R. Oral Lesions in HIV infection in developing countries: An overview. Adv Dent Res. 2006;19:63–8. doi: 10.1177/154407370601900113. [DOI] [PubMed] [Google Scholar]
- 20.Bakaki P, Kayita J, Moura Machado JE, Coulter JB, Tindyebwa D, Ndugwa CM, et al. Epidemiologic and clinical features of HIV-infected and HIV-uninfected Ugandan children younger than 18 months. J Acquir Immune Defic Syndr. 2001;28:35–42. doi: 10.1097/00042560-200109010-00006. [DOI] [PubMed] [Google Scholar]
- 21.Leggott PJ. Oral manifestations of HIV infection in children. Oral Surg Oral Med Oral Pathol. 1992;73:187–92. doi: 10.1016/0030-4220(92)90193-t. [DOI] [PubMed] [Google Scholar]
- 22.Fonseca R, Cardoso AS, Pomarico IP. Frequency of oral manifestations in children with human immunodefiency virus. Quintessence Int. 2000;31:419–22. [PubMed] [Google Scholar]
- 23.Arotiba JT, Adebola RA, Iliyasu, Babashani M, Shokunbi WA, Ladipo MMA Z, et al. Oral manifestations of HIV/AIDS infection in Nigerian patients. Nig J Surg Research. 2005;7(12):176–181. [Google Scholar]
- 24.Taiwo OO, Okeke EN, Otoh EC, Danfillo IS. Oral manifestations of HIV/AIDS infection in Nigerian patients. Niger J Med. 2005;7:176–81. [Google Scholar]
- 25.Hamza OJ, Matee MI, Simon EN, Kikwilu E, Moshi MJ, Mugusi F, et al. Oral manifestations of HIV infection in children and adults receiving highly active anti-retroviral therapy [HAART] in Dar es Salam, Tanzania. Oral Health. 2006;6:12. doi: 10.1186/1472-6831-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Santos LC, Castro GF, de Souza IP, Oliveire RH. Oral manifestations related to immunosuppression degree in HIV-positive children. Braz Dent J. 2001;12:135–138. [PubMed] [Google Scholar]
- 27.Greenspan JS, Greenspan D. The epidemiology of the oral lesions of HIV infections in developed world. Oral Dis. 2002;8(suppl 2):34–9. doi: 10.1034/j.1601-0825.2002.00009.x. [DOI] [PubMed] [Google Scholar]
- 28.Ramírez-Amador V, González M, de la Rosa E, Esquivel L, Volkow P, Ochoa FJ, et al. Oral findings in Mexican AIDS patients with cancer. J Oral Pathol Med. 1993;22:87–91. doi: 10.1111/j.1600-0714.1993.tb00050.x. [DOI] [PubMed] [Google Scholar]
- 29.Greenwood I, Zakrzewska JM, Robinson PG. Changes in the prevalence of HIV- associated mucosa disease at a dedicated clinic over 7 years. Oral Dis. 2002;8:90–4. doi: 10.1034/j.1601-0825.2002.1o787.x. [DOI] [PubMed] [Google Scholar]
- 30.Bendick C, Scheifele C, Reichart PA. Oral Manifestations in 101 Cambodian patients with HIV infection and AIDS. J Oral Pathol Med. 2002;31:1–4. doi: 10.1034/j.1600-0714.2002.310101.x. [DOI] [PubMed] [Google Scholar]
- 31.Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ. Changing prevalence of oral manifestations human immune-deficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:299–304. doi: 10.1016/s1079-2104(00)70092-8. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt-Westhausen AM, Priepke F, Bergmann FJ, Reichart PA. Decline in the rate of oral opportunistic infections following introduction of highly active anti-retroviral therapy. J Oral Pathol Med. 2000;29:336–41. doi: 10.1034/j.1600-0714.2000.290708.x. [DOI] [PubMed] [Google Scholar]


