Article-at-a-Glance
Background
Contact with health care workers may be an important means of infection transmission between patients, yet little is known about patterns of patient contact with staff and visitors in hospitals. In a cross-sectional study, the frequency, type, and duration of contacts made by health care workers, other hospital staff, and visitors to patients in acute care settings were documented.
Methods
Patients were observed in seven units of three academic hospitals, with recording of each occurrence of someone’s entry into the patient’s room. The health care worker’s role, the duration of the visit, and the highest level of patient contact made were noted. Staff were also surveyed to determine their perception of how many patients per hour they come into contact with, how long they spend with patients, and the level of patient contact that occurs.
Findings
Hourly room entries ranged from 0 to 28 per patient (median, 5.5), and patients received visits from 0 to 18 different persons per hour (median, 3.5). Nurses made the most visits (45%), followed by personal visitors (23%), medical staff (17%), nonclinical staff (7%), and other clinical staff (4%). Visits lasted 1 to 124 minutes (median, 3 minutes for all groups). Persons entering patients’ rooms touched nothing inside the room, only the environment, the patient’s intact skin, or the patient’s blood/body fluids 22%, 33%, 27%, and 18% of the time, respectively. Medical staff estimated visiting an average of 2.8 different patients per hour (range, 0.5–7.0), and nursing staff estimated visiting an average of 4.5 different patients per hour (range, 0.5–18.0).
Conclusions
Examining patterns of patient contact may improve understanding of transmission dynamics in hospitals. New transmission models should consider the roles of health care workers beyond patients’ assigned nurses and physicians.
Health care–associated infections (HAIs) cause nearly 100,000 deaths and cost more than 24 billion dollars annually in the United States.1,2 Reducing HAIs, particularly those caused by multidrug-resistant organisms, is a major component of The Joint Commission’s National Patient Safety Goals.3*
Although many HAIs originate from patients’ own flora, some are acquired via horizontal transmission.4 Thus, unlike adverse events that are isolated to single patients, HAIs can have significant impacts at the hospital level.5 Direct and indirect contact with health care workers (HCWs) may be an important means of exposure to pathogens that cause HAIs.6 A 2005 review found that HCWs were the source of infection in 10% of outbreaks.7 HCWs care for many patients simultaneously and may serve as vectors in HAI transmission between patients.8 Patients have contact with many different HCWs, but limited information exists about how often, by whom, and to what degree patients are touched. A study conducted in a neonatal ICU suggests that nurses make more than half of all patient contacts and are most likely to touch patients’ skin and body fluids.9 However, this study did not assess whether most contacts were made by patients’ assigned nurses versus other nurses on the unit, and the patterns of patient contact observed may not be generalizable to other patient populations or care settings.9 Other studies have focused on the frequency and duration of patient contact but did not measure the number of different HCWs who visit patients’ rooms.10,11
Understanding patterns of patient contact has important implications, not only for infection prevention, but for other measures of quality and safety such as patient falls. The purpose of this study was to determine the frequency, type, and duration of contacts made by different HCWs, other hospital staff, and visitors to patients in acute care settings using direct observation and a survey of medical and nursing staff.
Methods
Sample and Setting
Observations were conducted from June through August 2010 in seven inpatient units within three hospitals of an academic medical center in New York City, as follows:
-
■
A medical ICU, surgical ICU, and general medical/surgical unit of a 692-bed adult tertiary care hospital
-
■
A medical/surgical ICU and general medical/surgical unit of a 283-bed pediatric acute care hospital
-
■
A medical/surgical ICU and general medical/surgical unit of a 221-bed community hospital
Procedure
Observational Study
Study procedures were approved by the Columbia University Medical Center Institutional Review Board. Seven observers who were not staff members on any of the observed units were trained by study investigators. During a one-hour training period, study investigators and observers collected data on the same patient and then compared findings to ensure > 95% agreement. Any discordant data were discussed until consensus was reached. Each observer conducted 20 hours of observations between the hours of 5:00 A.M. and 8:00 P.M. in one of the seven units. Observers selected at least two patients whose rooms could be viewed clearly and simultaneously. Using a standardized form, for each patient, observers recorded the date, start, and end time of observation period; unit, room, and bed numbers; and isolation status. Each time someone entered an observed patient’s room (or, in the case of shared rooms, a patient’s area, as indicated by curtain dividers) the observer recorded the person’s role in patient care, times of room entry and exit, and highest level of contact made in the room (touched nothing, touched patient’s environment only, touched patient’s intact skin only, touched patient’s blood or body fluids, or unknown). If contact with blood or body fluids was made, observers also recorded whether gloves were worn.
Observers classified each person entering a patient’s room into one of the following seven roles in patient care:
Nursing staff, which included the primary nurse assigned for that shift, as well as other nursing staff, which included nurse practitioners, registered nurses, licensed practical nurses, and nursing assistants
Medical staff, including physicians, physician assistants, and medical students
Other clinical staff, including physical therapists, respiratory therapists, and radiology and laboratory technicians
Nonclinical staff, including food services, housekeeping, and transportation
Personal visitors
Other
Unknown
Minutes were the smallest unit of time recorded, thus visits < 1 minute were recorded as having lasted 1 minute. If anyone was in the room when the observation period began, entry time was recorded as unknown; if anyone remained in the room at the end of the observation period, exit time was unknown. If someone entered a patient’s room multiple times during an observation period, observers marked their contacts to indicate that they were made by the same person.
Survey
Anonymous surveys were administered to a convenience sample of medical and nursing staff in each of the seven observed units while the observations were ongoing. Observers approached medical or nursing staff present on the unit at the time of observation and invited them to participate in the survey, regardless of whether or not they were observed entering or exiting a patient’s room. Respondents indicated their discipline (medicine or nursing) and estimated the average number of times per hour they entered patient-occupied rooms, the average number of different patients they contacted per hour, the proportion of their patient visits that lasted ≤ 1 minute, 2–5 minutes, 6–15 minutes, and ≥ 15 minutes, and the proportion of their patient visits in which the highest level of contact was nothing in the room, patient’s environment only, patient’s intact skin only, and patient’s blood or body fluids.
Data Analysis
Length of visit was calculated for each observed room entry. For observations in which room entry and/or exit time was not observed, the start and/or end times of the observation period were used to determine the minimum duration. The median and range of visit lengths were calculated overall and stratified to assess differences between pediatric and adult patients, isolated and nonisolated patients, patients in ICUs and patients in general medical/surgical units, and care role of visitor. Total visits made by hospital staff or personal visitors were calculated as a rate per hour for each patient and observation period. The number of different people entering a patient’s room per hour during each observation period was also determined. Statistical analyses were not performed because it is likely that some patients were observed during multiple sessions; thus observations may not have been independently sampled and statistical tests of independence and equality of means are not appropriate.
Results
Observational Study
Room Entries
A total of 3,250 room entries were recorded during 491.4 patient-hours of observation. Seventy-five percent of observations were conducted on pediatric patients, 41% were conducted on patients in ICUs, and 46% were conducted on patients with isolation precautions (Table 1, above). Patients were visited by 0–28 persons/hour (median, 5.5). There was little difference in visit frequency by isolation status or unit type, but pediatric patients experienced more visits per hour than did adult patients (median, 8.5 versus 5.0).
Table 1.
Entries into Patients’ Rooms by Patient Population, Isolation Status, and Unit Type
| Patient Population | Isolation Status | Unit Type | Total | ||||
|---|---|---|---|---|---|---|---|
| Adults | Children | Any Isolation | No Isolation | Intensive Care | General Medical/Surgical |
||
| Total patient hours observed | 120.4 | 371.0 | 223.9 | 267.5 | 200.6 | 290.8 | 491.4 |
| Total number of room entries per hour* |
5.0 (0–26.4) |
8.5 (1.0–28.0) |
5.0 (0–28.0) |
6.0 (0–26.4) |
6.0 (0–28.0) |
6.0 (0–20.6) |
5.5 (0–28.0) |
| Number of different people entering room per hour* |
3.0 (0–18.0) |
3.5 (0.5–9.0) |
3.0 (0–11.0) |
4.0 (0–18.0) |
3.5 (0–18.0) |
3.5 (0–11.3) |
3.5 (0–18.0) |
| Minutes spent in room by each individual* |
3.0 (1.0–124.0) |
3.0 (1.0–120.0) |
3.0 (1–124.0) |
3.0 (1–120.0) |
3.0 (1–120.0) |
3.0 (1–124.0) |
3.0 (1–124.0) |
Data presented are median (range).
Health Care Worker Roles
As shown in Table 2 (page 563), the majority of visits were made by nursing staff (45%), followed by personal visitors (23%), medical staff (17%), nonclinical staff (8%), and other clinical staff (4%); patient care roles could not be determined for 3% of the visits. Only 836 (57%) of the 1,462 nursing staff visits were made by the patient’s primary nurse. Median visit length was similar for all HCWs and nonclinical staff but longer for personal visitors (2–3 minutes versus 14 minutes, respectively). Although at least half of the HCW visits were ≤ 3 minutes, some lasted at least 120 minutes for nursing staff, 72 minutes for medical staff, 45 minutes for other clinical staff, and 65 minutes for nonclinical staff (Table 2).
Table 2.
Minutes Spent in Patients’ Rooms During Eeach Observed Entry
| Care Role | N (%) of Total Entries | Median (Range) |
|---|---|---|
| Nursing staff* | 1,462 (45) | 2 (1–120) |
| Medical staff† | 558 (17) | 3 (1–72) |
| Other clinical staff‡ | 140 (4) | 3 (1–45) |
| Nonclinical staff§ | 245 (8) | 3 (1–65) |
| Personal visitors | 741 (23) | 14 (1–124) |
| All groups∥ | 3,250 (100) | 3 (1–124) |
Includes nurse practitioners, registered nurses, licensed practical nurses, and nursing assistants.
Includes physicians, physician assistants, and medical students.
Includes physical therapists, respiratory therapists, radiology technicians, and laboratory technicians.
Includes dietary/food service staff, housekeeping staff, and patient transportation staff.
Total includes room entries by people whose role could not be determined.
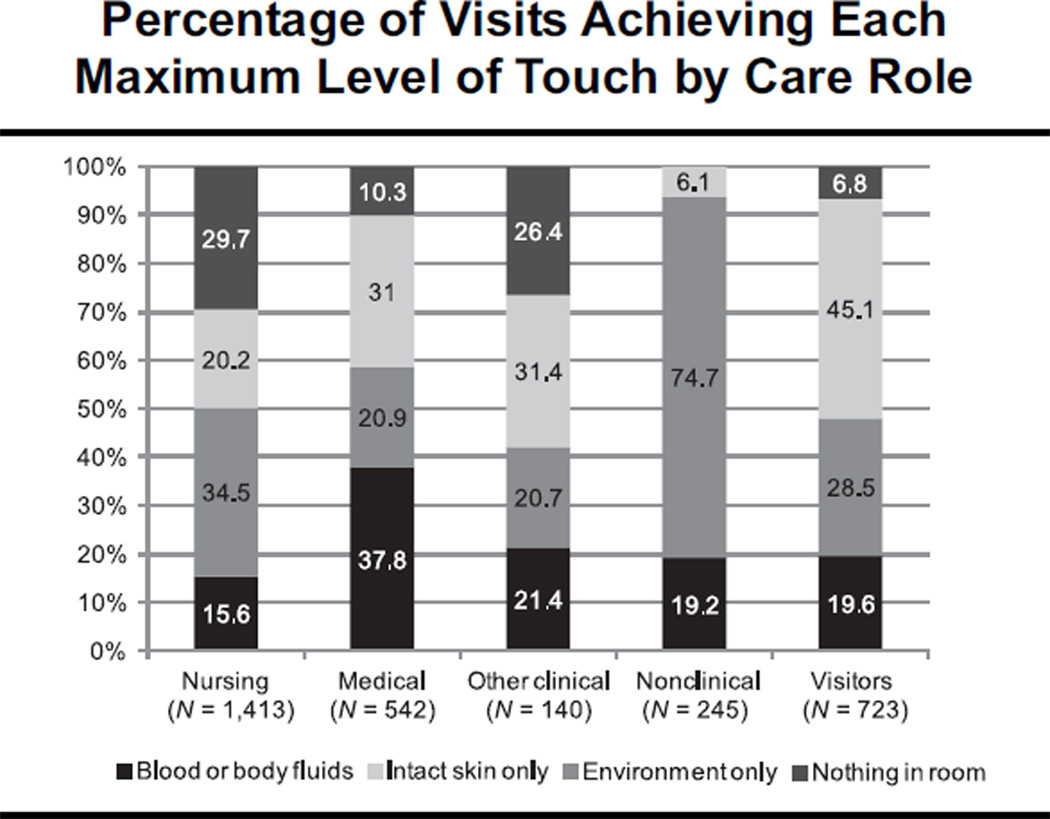
Contacts
It was common for hospital staff and visitors to enter patients’ rooms but not touch anything while inside: 21.6% of visits involved no physical contact with patients or their environments. However, these visits tended to be shorter visits (median length, 1 minute). Contact with patient environment only was the most common level of touch (33.5% of visits), followed by patient’s intact skin (27.1%) and patient’s blood or body fluids (17.8%). Figure 1 (page 564) shows the percentage of visits achieving each maximum level of touch by care role. While 94% of nursing staff, 96% of medical staff, and 97% of other clinical staff wore gloves while touching blood or body fluids, only 33% of personal visitors did. Glove use during blood/body fluid contact was more common for isolated patients (Table 3, page 565).
Figure 1.
Contact with patient environment only was the most common level of touch (33.5% of visits), followed by patient’s intact skin (27.1%) and patient’s blood or body fluids (17.8%).
Table 3.
Percentage of Contacts Made with Gloves While Touching Blood or Body Fluids of Isolated Versus Nonisolated Patients*
| Role in Patient Care† | Patients Not on Contact Isolation‡ | Patients on Contact Isolation |
|---|---|---|
| Nursing staff§ | 88 (144/164) | 99 (250/253) |
| Medical staff∥ | 95 (38/40) | 100 (16/16) |
| Other clinical staff# | 95 (18/19) | 100 (17/17) |
| Personal visitors | 7 (2/28) | 67 (14/21) |
Data are % of blood or body fluid contacts made with gloves (gloved blood or body fluid contacts/total blood or body fluid contacts).
Nonclinical staff made no blood/body fluid-level patient contacts.
Includes patients on airborne and droplet precautions.
Includes nurse practitioners, registered nurses, licensed practical nurses, and nursing assistants.
Includes physicians, physician assistants, and medical students.
Includes physical therapists, respiratory therapists, radiology technicians, and laboratory technicians.
Survey
Seventeen medical and 41 nursing staff completed the survey. Medical staff estimated visiting an average of 2.8 different patients per hour (range, 0.5–7.0), and nursing staff estimated visiting an average of 4.5 different patients per hour (range, 0.5–18.0). The medical and nursing staff who responded to the survey reported spending more time with patients during each encounter in comparison with the length of patient encounters observed in this study. Nursing and medical staff reported that only 10% (median) of their patient encounters lasted ≤ 1 minute, but 38% and 28% of the observed contacts were this short, respectively. Similarly, only 6% of observed visits were ≥ 15 minutes, while medical and nursing staff estimated that 20% and 10% of their visits were this long, respectively. When asked what proportion of their patient visits involved touching nothing in the room, the environment only, the patient’s intact skin only, and blood/body fluids, the median reported percentages were 5%, 20%, 30%, and 30%, respectively, for nursing staff and 20%, 15%, 40%, and 5%, respectively, for medical staff.
Discussion
The high frequency of patient contact observed in this study is encouraging for many measures of care quality and patient safety. The parity observed between isolated and nonisolated patents is particularly encouraging; previous studies indicated that isolated patients may be visited half as many times as nonisolated patients in the same unit.10,11 Frequent contact with HCWs can help to ensure timely identification of patient needs such as pain management, prevent adverse events such as falls, and improve overall patient satisfaction and emotional health during the hospital stay.12,13 Despite these benefits, frequent contact with HCWs and personal visitors may also increase patients’ risks of acquiring HAIs.
Recent studies have demonstrated a variety of opportunities whereby infectious organisms might be transferred from patients to HCWs or from HCWs to patients during routine care. One study showed that HCWs who touched body sites or bedside equipment contaminated with vancomycin-resistant enterococci (VRE) transferred the bacteria to more than 10% of previously VRE–negative sites that they subsequently touched.14 Another study of 13 patients with VRE stool colonization showed that either the bedrails or the bedside tables of 12 patients (92%) were contaminated with VRE, and HCWs’ gloves became contaminated after contacts with these surfaces for 6 of the patients (46%).15
Despite the fact that many hospitals implement isolation precautions for patients known to be infected or colonized with epidemiologically significant pathogens, institutions remain vulnerable to outbreaks for several reasons. First, the use of barrier precautions does not preclude the possibility of HCW– mediated transfer of organisms between patients; even if gloves and gowns are worn, HCWs’ hands can be contaminated during patient contact, while removing protective equipment after patient contact, or during contact with the patient’s environment after removing protective equipment.16,17 A second concern is that HCWs can come into contact with epidemiologically important organisms while caring for patients who are not isolated. For example, routine cleaning procedures may not completely decontaminate rooms between patients, so organisms harbored by previous occupants can remain in the environment after they have been discharged.18 It is also common for there to be a lag of up to several days between the time that an infection begins in a patient and the time that the infection is recognized and isolation precautions are implemented by the care team. Low compliance with recommendations to perform hand hygiene before and after all patient contacts, regardless of isolation status or glove use, is common and heightens the chances that pathogens will travel between patients’ rooms.19
Prolonged contact with health care environments is a known risk factor for acquisition of HAIs, but the factors that drive this phenomenon are not well understood.20,21 Confounding by health status may account for some of the observed relationship between length of hospital stay and risk of infection (that is, those who are sicker tend to stay longer and also have more independent risk factors for acquiring an infection), but this explanation does not account for the entirety of the association. One possibility is that there is a fixed risk associated with each HCW contact, and these risks accumulate additively during the course of a hospital stay. Quantifying and describing patient contacts may be essential for modeling the relationship between length of hospital stay and risk of infection. For example, this study suggests that modeling patient-to-patient transmission using only assigned nurses or physicians as vectors may be insufficient because nearly half of all nursing visits were made by nurses other than the patient’s primary nurse, and less than a quarter of all hospital staff visits were made by physicians.
The findings of this study highlight some important and underappreciated phenomena regarding possible routes of infection transmission in acute care facilities. A recent article by Schweon and Kirk22 illuminates the lack of recommendations for patient hand hygiene in long term care settings, where patient- to-patient interaction can be an important means of infection transmission. Our observations suggest that this may be an important gap in acute care settings, as well. Although our observers did not systematically record patient-to-patient contacts, there were many instances in which physical contact among patients occurred. Ambulatory patients visited one another’s rooms, sat on each other’s beds and chairs, and exchanged physical contact in common areas. The possible role of personal visitors in infection transmission may also be overlooked. Our observers noted many instances in which a patient’s personal visitor kissed, hugged, or assisted the patient’s roommate with walking, feeding, or some other activity. Visitors of isolated patients in single rooms may not don protective equipment appropriately or may fail to remove it when they leave patient rooms to visit common areas.23 In fact, the pediatric hospital observed in this study does not require the use of protective equipment such as gloves and gowns for visitors of isolated patients because use of these items may have a negative psychological impact on hospitalized children and interfere with routine family structure. This policy accounts for the low levels of glove use during blood and body fluid contacts made by visitors (Table 3). Visitor glove use during blood and body fluid contact with adult patients was 80%. Another notable piece of information provided by this study is the difference between HCWs’ perceived patterns of care and observed patterns of care. It has been hypothesized that HCWs may not perform hand hygiene before patient contact when they do not intend to touch the patient or environment while in the room. For this reason, infection prevention leadership often encourages hand hygiene before all patient room entries under the assumption that the need for direct patient contact may arise suddenly and unexpectedly. In this study, the percentage of patient encounters in which neither the patient nor his or her surroundings were touched was actually observed to be much higher than perceived by HCWs (16% versus 5% for nursing staff and 38% versus 20% for medical staff ). Thus, the mere act of entering a patient’s room does not always represent an indication to perform hand hygiene as defined by the World Health Organization. 24 Patients in this study were visited up to 28 times by as many as 18 different people per hour.
Limitations
This study had several limitations common to observational research, and our team made efforts to reduce bias when feasible. It is possible that observers were unable to accurately determine the level of patient contact or caregiver role for all patient encounters from their vantage points, although observers recorded any data point on which they were not fully confident as “missing” and clarified HCWs’ roles in patient care (for example, confirming whether someone was a nurse versus a respiratory therapist) by asking the caregivers directly. The convenience sample design resulted in the underrepresentation of early morning, late evening, and weekend hours, which could have biased the results if the volume or nature of patient contact differs by time of day or day of week. Moreover, we did not sample any overnight hours (between 8:00 p.m. and 5:00 a.m), so these results may not be representative of patient contacts averaged throughout a 24-hour hospital stay. This study also did not distinguish between various ranks and responsibilities of personnel within care roles, which may limit the utility of these data for fully understanding patterns of care in various types of nursing units. For example, registered nurses are usually assigned to provide care to two or more specific patients, depending on acuity, while nursing assistants might attend to all patients on the unit. Similarly, attending physicians and medical residents will likely differ in the level and type of contact they have with patients. Still, these data serve as a substitute for more in-depth observations in which HCWs are followed and all of their activities are recorded; such studies are logistically challenging and costly. Characterizing the activities of floating staff, who could potentially introduce pathogens present in one unit to other units, may be fundamentally important for tracking infections at the facility level. It is likely that some of the staff observed in this study were float staff, but this was not tracked because of the anonymous nature of the observations.
The number of medical and nursing staff recruited to complete the questionnaire on perceived patient contacts was low because participation was limited to staff present on the unit during the times of observation. The inclusion criteria for survey completion also limit the generalizability of the findings because staff on services that round on multiple nursing units may experience very different patterns of care. Another limitation of the survey was that participation was voluntary, and respondents may have differed from nonrespondents in their perceived patterns of care.
Conclusions
Given the importance of frequent HCW–patient interaction for ensuring safe, quality care, limiting contacts is certainly not in the best interest of the patient or care team. Studying patterns of contact, however, can potentially improve understanding of how transmission occurs and play an important role in efforts to mitigate infection risk by changing work-flow patterns to reduce opportunities for transmission, emphasizing the importance of compliance with standard precautions and isolation precautions, and informing structural and staffing architecture in hospital wards.
Acknowledgments
This work was funded in part by a grant from the National Institute of Nursing Research, National Institutes of Health (R01 NR010822). The authors thank unit staff for their participation and Gerard Dela Cruz, RN, MA, for assistance with data collection.
Footnotes
NPSG.07.03.01. Implement evidence-based practices to prevent health care–associated infections due to multidrug-resistant organisms in acute care hospitals. Note: This requirement applies to, but is not limited to, epidemiologically important organisms such as methicillin-resistant Staphylococcus aureus (MRSA), Clostridium difficile (CDI), vancomycin-resistant enterococci (VRE), and multidrug-resistant gram-negative bacteria.
Contributor Information
Bevin Cohen, Center for Interdisciplinary Research to Reduce Antimicrobial Resistance, Columbia University School of Nursing, New York City..
Sandra Hyman, Perioperative Services, New York-Presbyterian Hospital, Columbia University Medical Center, New York City..
Lauren Rosenberg, College of Physicians & Surgeons, Columbia University, New York City..
Elaine Larson, Pharmaceutical and Therapeutic Research, and Associate Dean for Research, Columbia University School of Nursing..
References
- 1.Klevens RM, et al. Estimating health care-associated infections and deaths in US hospitals, 2002. Public Health Rep. 2007;122(2):160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Centers for Disease Control and Prevention. [Accessed Oct. 22, 2012];The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. 2009 Mar; http://www.cdc.gov/HAI/pdfs/hai/Scott_CostPaper.pdf.
- 3.The Joint Commission. 2013 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oak Brook, IL: Joint Commission Resources; 2012. [Google Scholar]
- 4.Weinstein RA. Epidemiology and control of nosocomial infections in adult intensive care units. Am J Med. 1991 Sep 16;91(3B):179S–184S. doi: 10.1016/0002-9343(91)90366-6. [DOI] [PubMed] [Google Scholar]
- 5.Hansen S, et al. Closure of medical departments during nosocomial outbreaks: Data from a systematic analysis of the literature. J Hosp Infect. 2007;65(4):384–353. doi: 10.1016/j.jhin.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Halwani M, et al. Cross-transmission of nosocomial pathogens in an adult intensive care unit: Incidence and risk factors. J Hosp Infect. 2006;63(1):39–46. doi: 10.1016/j.jhin.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Gastmeier P, et al. How outbreaks can contribute to prevention of nosocomial infection: Analysis of 1,022 outbreaks. Infect Control Hosp Epidemiol. 2005;26(4):357–361. doi: 10.1086/502552. [DOI] [PubMed] [Google Scholar]
- 8.Eveillard M, et al. Measurement and interpretation of hand hygiene compliance rates: Importance of monitoring entire care episodes. J Hosp Infect. 2009;72(3):211–217. doi: 10.1016/j.jhin.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 9.Cohen B, et al. Factors associated with hand hygiene practices in two neonatal intensive care units. Pediatr Infect Dis J. 2003;22(6):494–499. doi: 10.1097/01.inf.0000069766.86901.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirkland KB, Weinstein JM. Adverse effects of contact isolation. Lancet. 1999 Oct 2;354(9185):1177–1178. doi: 10.1016/S0140-6736(99)04196-3. [DOI] [PubMed] [Google Scholar]
- 11.Evans HL, et al. Contact isolation in surgical patients: A barrier to care? Surgery. 2003;134(2):180–188. doi: 10.1067/msy.2003.222. [DOI] [PubMed] [Google Scholar]
- 12.Bourgault AM, et al. Circle of excellence: Does regular rounding by nursing associates boost patient satisfaction? Nurs Manage. 2008;39(11):18–24. doi: 10.1097/01.NUMA.0000340814.83152.35. [DOI] [PubMed] [Google Scholar]
- 13.Meade CM, Bursell AL, Ketelsen L. Effects of nursing rounds: On patients’ call light use satisfaction, and safety. Am J Nurs. 2006;106(9):58–70. doi: 10.1097/00000446-200609000-00029. [DOI] [PubMed] [Google Scholar]
- 14.Duckro AN, et al. Transfer of vancomycin-resistant enterococci via health care worker hands. Arch Intern Med. 2005 Feb 14;165(3):302–307. doi: 10.1001/archinte.165.3.302. [DOI] [PubMed] [Google Scholar]
- 15.Ray AJ, et al. Nosocomial transmission of vancomycin-resistant enterococci from surfaces. JAMA. 2002 Mar 20;287(11):1400–1401. doi: 10.1001/jama.287.11.1400. [DOI] [PubMed] [Google Scholar]
- 16.Tenorio AR, et al. Effectiveness of gloves in the prevention of hand carriage of vancomycin-resistant Enterococcus species by health care workers after patient care. Clin Infect Dis. 2001 Mar 1;32(5):826–829. doi: 10.1086/319214. [DOI] [PubMed] [Google Scholar]
- 17.Snyder GM, et al. Detection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci on the gowns and gloves of healthcare workers. Infect Control Hosp Epidemiol. 2008;29(7):583–589. doi: 10.1086/588701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect. 2009;73(4):378–385. doi: 10.1016/j.jhin.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 19.Pittet D, Boyce JM. Hand hygiene and patient care: Pursuing the Semmelweis legacy. Lancet Infect Dis. 2001;1(0):9–20. [Google Scholar]
- 20.Delgado-Rodríguez M, et al. Hospital stay length as an effect modifier of other risk factors for nosocomial infection. Eur J Epidemiol. 1990;6(1):34–39. doi: 10.1007/BF00155546. [DOI] [PubMed] [Google Scholar]
- 21.Tess BH, et al. Incidence of hospital-acquired infection and length of hospital stay. Eur J Clin Microbiol Infect Dis. 1993;12(2):81–86. doi: 10.1007/BF01967579. [DOI] [PubMed] [Google Scholar]
- 22.Schweon SJ, Kirk J. A realistic approach towards hand hygiene for long-term care residents and health care personnel. Am J Infect Control. 2011;39(4):336–338. doi: 10.1016/j.ajic.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 23.Clock SA, et al. Contact precautions for multidrug-resistant organisms: Current recommendations and actual practice. Am J Infect Control. 2010;38(2):105–111. doi: 10.1016/j.ajic.2009.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. [Accessed Oct 22, 2012];WHO Guidelines on Hand Hygiene in Health Care. 2009 http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf.