Abstract
Background
Systemic therapeutics targeting the peroxisome proliferator-activated receptors have been found to be beneficial in the treatment of diabetic retinopathy. In this paper, we provide a rationale for the use of these therapeutics as intraocular agents. In addition, we introduce the peroxisome proliferator-activated receptors and describe their functions in response to the drugs.
Discussion
Based on the evidence of large-scale clinical studies investigating the systemic administration of fenofibrate, this ligand for peroxisome proliferator-activated receptor-α is potentially a good candidate for intraocular delivery. Here, we describe the mechanisms by which it might be acting to improve diabetic retinopathy, its relative safety and we speculate on how it could be developed for intraocular delivery.
Summary
In this paper, we provide a rationale for the further investigation of peroxisome proliferator-activated receptor-α agonists as intraocular agents for the treatment of diabetic retinopathy.
Keywords: Diabetes, Diabetic retinopathy, Intraocular, Fenofibrate, TZDs, PPARs
Background
Diabetic retinopathy (DR) is a leading cause of blindness in adults, with some degree of DR occurring in nearly all type 1 diabetics and in the majority of type 2 diabetics [1]. Hitherto, it was thought that the only way to prevent the development and progression of DR was by tight control of blood sugar, plasma lipids and blood pressure [1]. However, it has since been shown that treatment of type 2 diabetics with lipid-lowering fenofibrates results in a significant reduction in the progression of DR which may be unrelated to any effect on plasma lipid levels [2,3]. A related class of compounds, the thiazolidinediones (TZDs), have been found to reduce progression to DR in at least one clinical trial [4]. Thus far, the beneficial effect of PPAR agonists on the retina has been observed following systemic delivery for the treatment of diabetic patients. It is our contention that the intraocular delivery of these agonists could specifically ameliorate DR.
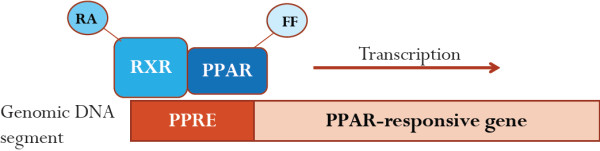
Fibrates and TZDs are agonists for two isoforms of nuclear receptor superfamily members, the peroxisome proliferator-activated receptors (PPARs) α and γ, respectively. PPARs are localised to the nucleus, where they interact with other proteins involved in gene expression, including various co-activator and co-repressor proteins [5]. In order for PPARs to induce gene expression, they must also interact with their co-activator, the retinoic X receptor (RXR), and then bind to a PPAR response element (PPRE) in a given gene Figure 1[6-9]. PPARs modulate the expression of numerous genes, including those involved in lipid metabolism, adipogenesis, inflammatory signalling and oxidative stress [9-11], in a tissue-dependent manner [12]. Importantly, PPARs also regulate the expression of themselves via a positive feedback mechanism [13,14] or through a co-operative system with other transcription factors [15,16].
Figure 1.
Agonist-bound PPARs induce gene expression. Activated PPARs must first associate with their co-receptor, retinoid X receptor (RXR), in order to modulate transcription of specific genes. RXR binds to its ligand, retinoic acid, and interacts with PPAR bound to an agonist (e.g. fibrates). Together, RXR and PPAR can then bind to a consensus sequence of nucleotides, known as the PPAR response element (PPRE). PPAR and RXR binding triggers expression of a responsive gene . Abbreviations: RA, retinoic acid, FF, fenofibrate.
PPARs are generally considered to be inactive until bound by a ligand [17]. Both endogenous ligands and synthetic agonists have been described for PPARα and γ. Endogenous ligands include fatty acids and lipid metabolites, such as prostaglandins and leukotrienes [18-21]. Interestingly, prostaglandins and leukotrienes are also known to be mediators of inflammation and oxidative stress [22,23]. Synthetic agonists for the different PPAR isoforms are similar in terms of chemical structure and molecular mass; in fact, there are several known dual agonists that activate both PPARα and PPARγ [24,25]. The aforementioned synthetic PPAR agonists, fibrates and TZDs, are structurally very similar. However, research shows that fenofibrate specifically acts via PPARα [26], whilst TZDs are known to specifically activate PPARγ [27-30]. Further, PPARα and PPARγ are also known to have distinct physiological roles [9,31]. While PPARα increases the uptake and beta-oxidation of fatty acids, as well as reduces the synthesis and secretion of triglycerides, PPARγ specifically induces adipogenesis and stimulates triglyceride storage [12]. PPARγ is thought to improve insulin sensitivity via its stimulatory effects on GLUT4 and adiponectin [31]. Although both PPARα and PPARγ have been found to inhibit inflammation, they do so within different cell types via distinct targets [10,12]. Compared to PPARα, PPARγ has broader anti-inflammatory activity due to targeting numerous transcription factors within more cell types than PPARα [12]. In particular, PPARγ has been found to function as an inhibitor of monocyte/macrophage function by blocking pro-inflammatory signals [32-34]. To date, PPAR agonists have been clinically utilised for the treatment of diabetes and dyslipidaemia due to their beneficial effects on insulin sensitivity and lipid metabolism.
The PPARγ agonists, TZDs, are prescribed for lowering blood glucose levels [35] but it is uncertain whether they could also reduce DR progression since there are no randomised clinical trials. However, there has been one retrospective review of diabetic patients receiving rosiglitazone which revealed a reduction in development of proliferative DR [4], although this paper was criticised because of unmatched controls [36]. TZDs have also been trialled in animal models and were found to reduce choroidal neovascularisation [37]. Interestingly, the TZDs in this study were given by intraocular injection, suggesting that this delivery route of PPAR agonists might also be efficacious in humans [37]. Against the use of TZDs in the treatment of DR are the findings that systemic administration of troglitazone in humans was associated with increased vascular endothelial growth factor (VEGF) expression [38] and with an increased risk of diabetic macular oedema (DMO) [39]. Although the latter has been challenged by subsequent studies [40], questions remain about the overall safety and efficacy of TZDs [9,41,42]. In addition to TZDs, newer PPARγ modulators are being developed which could have enhanced safety profiles [9,43]. Further scientific and clinical studies are needed to clarify the role of PPARγ in DR and to determine whether treatment with TZDs or novel PPARγ agonists would be beneficial. Currently, no PPARγ agonists are known to reduce DR progression to the same extent observed with fibrates.
Discussion
In the UK, under the NICE guidelines, fibrates are prescribed as a first-line therapy for diabetics with high serum triglycerides and are often given in combination with statins [35]. Recently, two large, randomised clinical trials showed an important secondary benefit of systemically-delivered fenofibrate on DR in type 2 diabetics. In the FIELD study, fenofibrate (200 mg/day) taken over five years reduced the need for laser photocoagulation to treat diabetic maculopathy by 36% and proliferative retinopathy by 32% [2]. Similar results were observed in the ACCORD Eye Study, wherein the use of fenofibrate along with simvastatin reduced progression of DR by 40% compared to simvastatin alone [3], with DR progression defined as a deterioration by three steps on the ETDRS severity scale. Importantly, in the FIELD study in particular, this benefit was independent of plasma lipid levels [2]. In addition, in both the FIELD and ACCORD studies, the benefit of fenofibrate was independent of glycaemic control. These findings could suggest that fenofibrate is having local effects within the eye not necessarily related to systemic metabolism.
Diabetic retinopathy is characterised by microangiopathy, which is thought to be caused by oxidative stress, advanced glycation end-products (AGEs), inflammatory mediators and endothelial cell death [44-46]. The beneficial effects of fenofibrate observed in the FIELD and ACCORD Eye studies could be due to reduced oxidative stress and inflammation, as well as effects on vascular function. Several studies have analysed the pharmacological mechanisms of fenofibrate individually. For example, fenofibrate has been shown to reduce circulating markers of oxidative stress in dyslipidaemic patients [47]. It has also been found to prevent inflammation by blocking AGE-induced NF-κB activation in animal models [48]. Fenofibrate has been found to ameliorate vascular function, improving blood flow in diabetics [49]. One recent study investigated the combined effects of fenofibrate on oxidative stress, inflammation and vascular tone in an animal model of diabetes [50]. This study found that fenofibrate improved vascular relaxation and increased expression of the antioxidant enzymes, superoxide dismutase and catalase [50]. Interestingly, they also observed a decrease in the level of a proinflammatory marker, myeloperoxidase (MPO) [50]. Importantly, a comprehensive screen of donated human retinal pigment epithelia (RPE) revealed that PPARα (the receptor for fenofibrate) was highly expressed while PPARγ was absent from the RPE [51]. Further, laboratory studies using human RPE cells under hyperglycaemic conditions found that fenofibrate reduced RPE monolayer permeability [52] via blocking activation of AMP-activated protein kinase (AMPK) [53,54] and the reduction in permeability was dose-dependent, indicating that intraocular delivery of fenofibrate could be highly efficacious. In summary, there is an expanding molecular basis for the positive effects of fenofibrate observed in the FIELD and ACCORD Eye studies.
Compared to other currently available PPAR agonists, fenofibrate appears to have a better safety profile. Fenofibrate has been prescribed for many years and is generally well-tolerated, with only 2% of patients discontinuing use due to side-effects [55]. There have been concerns that long-term use of fenofibrates might be associated with an increased risk of cardiovascular disease, particularly in those with renal impairment [56]. However, assessment of data from the FIELD study did not support this, providing further evidence for the safety profile of fenofibrate [56]. Given the findings of the large-scale FIELD and ACCORD Eye studies, fenofibrate has been found to reduce progression of DR and has not been associated with drug safety issues, making it a good candidate for potential intraocular delivery.
To our knowledge, the intraocular delivery of fenofibrate has not yet been examined. Therefore, animal and clinical trials are needed to determine if this delivery method would be suitable for the prevention and treatment of DR. The pharmacokinetics of these agonists in the eye is unknown. To date, fenofibrate has been formulated for oral delivery and is converted by esterases into the active compound, fenofibric acid [57]. Fenofibric acid has a half-life of 16 h and reaches a steady-state level in the circulation within five days of the commencement of treatment [55]. Given this need for esterase conversion, the delivery of a pre-activated form of fenofibrate into the eye could be more effective. One example of such a fenofibrate derivative is ABT-335, which is a choline salt of fenofibric acid and does not require esterase processing [55]. Such a readily bioactive drug could be better suited to intraocular delivery than the fenofibrate parent compound.
Should treatment with fenofibrate alone prove beneficial in the management of DR, combination therapies could then be examined. For example, it is now widespread practice to treat DMO with intraocular injections of anti-VEGF therapeutics [58-62]. While treatment with anti-VEGF is effective, it requires frequent injections [58,62-64]. This represents a burden on the patients and the healthcare delivery services. It is conceivable that intraocular anti-VEGF therapies could be combined with fenofibrate in the same injection, which might reduce the frequency of injections and therefore represent an improved treatment strategy. Whether the combination of fenofibrate and anti-VEGF agents will be viable for co-administration would need to be examined.
The goal of this paper is to provide a rationale for the intraocular injection of PPAR agonists, particularly fenofibrate or its derivatives, and to encourage further research in this area.
Summary
· The ACCORD and FIELD Eye studies showed a significant beneficial effect on DR in diabetics treated with systemic fenofibrates.
· There is evidence from one study that intraocular delivery of TZDs is effective in treating CNV in an animal model, suggesting that PPAR agonists can be biologically active in the eye.
· Relative expression levels in the RPE suggest that PPARα agonists might be more beneficial than PPARγ agonists for the treatment of DR.
· There is emerging molecular evidence for the beneficial effects of PPARα agonists in the treatment of DR that goes beyond an improvement in plasma lipid levels.
· The commonplace treatment of DR with intraocular anti-VEGF agents could be used to facilitate PPARα agonist delivery. In other words, fibrates could be delivered concurrently with anti-VEGF using the same injection.
Abbreviations
AGE: Advanced glycation end-products; CNV: Choroidal neovascularisation; DMO: Diabetic macular oedema; DR: Diabetic retinopathy; NF-κB: Nuclear factor-κB; PPAR: Peroxisome proliferator-activated receptor; PPRE: PPAR response element; RPE: Retinal pigment epithelium; RXR: Retinoic X receptor; TZDs: Thiazolidinediones; VEGF: Vascular endothelial growth factor.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
The authors contributed equally to the analysis, design and writing of the article.
Authors’ information
Dr. Maxwell Treacy is an engineer and trainee in ophthalmology. Dr. Tara Hurst is a biochemist, specialising in the innate immune response and viral modulation of cellular pathways.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Maxwell P Treacy, Email: max@treacy.ie.
Tara P Hurst, Email: tara.hurst@ntu.ac.uk.
Acknowledgements
The authors would like to thank Grace Hurst for critically reviewing the manuscript.
References
- Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy: a systematic review. J Am Med Assoc. 2007;298:902–916. doi: 10.1001/jama.298.8.902. [DOI] [PubMed] [Google Scholar]
- Keech AC, Mitchell P, Summanen PA, O'Day J, Davis TM, Moffitt MS, Taskinen MR, Simes RJ, Tse D, Williamson E, Merrifield A, Laatikainen LT, d'Emden MC, Crimet DC, O'Connell RL, Colman PG. FIELD study investigators. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet. 2007;370:1687–1697. doi: 10.1016/S0140-6736(07)61607-9. [DOI] [PubMed] [Google Scholar]
- ACCORD Study Group and ACCORD Eye Study. Effects of medical therapies on retinopathy progression in Type 2 Diabetes. N Engl J Med. 2010;363:233–244. doi: 10.1056/NEJMoa1001288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen LQ, Child A, Weber GM, Folkman J, Aiello LP. Rosiglitazone and Delayed Onset of Proliferative Diabetic Retinopathy. Arch Ophthalmol. 2008;126:793–799. doi: 10.1001/archopht.126.6.793. [DOI] [PubMed] [Google Scholar]
- Kota BP, Huang THW, Roufogalis BD. An overview on biological mechanisms of PPARs. Pharmacol Res. 2005;51:85–94. doi: 10.1016/j.phrs.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Issemann I, Prince RA, Tugwood JD, Green S. The retinoid X receptor enhances the function of the peroxisome proliferator activated receptor. Biochimie. 1993;75:37–47. doi: 10.1016/0300-9084(93)90084-6. [DOI] [PubMed] [Google Scholar]
- Schoonjans K, Peinado-Onsurbe J, Lefebvre AM, Heyman RA, Briggs M, Deeb S, Staels B, Auwerx J. PPARα and PPARγ activators direct a distinct tissue-specific transcriptional response via a PPRE in the lipoprotein lipase gene. EMBO J. 1996;15:5336–5348. [PMC free article] [PubMed] [Google Scholar]
- Varanasi U, Chu R, Huang Q, Castellon R, Yeldandi AV, Reddy JK. Identification of a peroxisome proliferator-responsive element upstream of the human peroxisomal fatty acyl coenzyme A oxidase gene. J Biol Chem. 1996;271:2147–2155. doi: 10.1074/jbc.271.4.2147. [DOI] [PubMed] [Google Scholar]
- Ciudin A, Hernández C, Simó R. Update on cardiovascular safety of PPARgamma agonists and relevance to medicinal chemistry and clinical pharmacology. Curr Top Med Chem. 2012;12:585–604. doi: 10.2174/156802612799436632. [DOI] [PubMed] [Google Scholar]
- Varga T, Czimmerer Z, Nagy L. PPARs are a unique set of fatty acid regulated transcription factors controlling both lipid metabolism and inflammation. Biochim Biophys Acta. 2011;1812:1007–1022. doi: 10.1016/j.bbadis.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalik L, Auwerx J, Berger JP, Chatterjee VK, Glass CK, Gonzalez FJ, Grimaldi PA, Kadowaki T, Lazar MA, O'Rahilly S, Palmer CN, Plutzky J, Reddy JK, Spiegelman BM, Staels B, Wahli W. International Union of Pharmacology. LXI. Peroxisome Proliferator-Activated Receptors. Pharmacol Rev. 2006;58:726–741. doi: 10.1124/pr.58.4.5. [DOI] [PubMed] [Google Scholar]
- Moraes L, Piqueras L, Bishop-Bailey D. Peroxisome proliferator-activated receptors and inflammation. Pharmacol Ther. 2006;110:371–385. doi: 10.1016/j.pharmthera.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Lazar MA. Becoming fat. Genes Dev. 2002;16:1–5. doi: 10.1101/gad.964002. [DOI] [PubMed] [Google Scholar]
- Li Y, Lazar MA. Differential gene regulation by PPARγ Agonist and constitutively active PPARγ2. Mol Endocrinol. 2002;16:1040–1048. doi: 10.1210/me.16.5.1040. [DOI] [PubMed] [Google Scholar]
- Aleshin S, Grabeklis S, Hanck T, Sergeeva M, Reiser G. Peroxisome proliferator-activated receptor (PPAR)-γ positively controls and PPARα negatively controls cyclooxygenase-2 expression in rat brain astrocytes through a convergence on PPARβ/δ via mutual control of PPAR expression levels. Mol Pharmacol. 2009;76:414–424. doi: 10.1124/mol.109.056010. [DOI] [PubMed] [Google Scholar]
- Kim JE, Chen J. Regulation of peroxisome proliferator–activated receptor-γ activity by mammalian target of rapamycin and amino acids in adipogenesis. Diabetes. 2004;53:2748–2756. doi: 10.2337/diabetes.53.11.2748. [DOI] [PubMed] [Google Scholar]
- Green S, Tugwood JD, Issemann I. The molecular mechanism of peroxisome proliferator action: a model for species differences and mechanistic risk assessment. Toxicol Lett. 1992;64/65:131–139. doi: 10.1016/0378-4274(92)90182-j. [DOI] [PubMed] [Google Scholar]
- Forman BM, Chen J, Evans RM. Hypolipidemic drugs, polyunsaturated fatty acids, and eicosanoids are ligands for peroxisome proliferator-activated receptors α and δ. PNAS. 1997;94:4312–4317. doi: 10.1073/pnas.94.9.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliewer SA, Sundseth SS, Jones SA, Brown PJ, Wisely GB, Koble CS, Devchand P, Wahli W, Willson TM, Lenhard JM, Lehmann JM. Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors α and γ. PNAS. 1997;94:4318–4323. doi: 10.1073/pnas.94.9.4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krey G, Braissant O, L'Horset F, Kalkhoven E, Perroud M, Parker MG, Wahli W. Fatty acids, eicosanoids, and hyoplipidemic agents identified as ligands of peroxisome proliferator-activated receptors by coactivator-dependent receptor ligand assay. Mol Endocrinol. 1997;11:779–791. doi: 10.1210/me.11.6.779. [DOI] [PubMed] [Google Scholar]
- Wilson TM, Lehmann JM, Kliewer SA. Discovery of ligands for the nuclear peroxisome proliferator-activated receptors. Ann N Y Acad Sci. 1996;804:276–83. doi: 10.1111/j.1749-6632.1996.tb18622.x. [DOI] [PubMed] [Google Scholar]
- Stables MJ, Gilroy DW. Old and new generation lipid mediators in acute inflammation and resolution. Prog Lipid Res. 2011;50:35–51. doi: 10.1016/j.plipres.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Ullery JC, Marnett LJ. Protein modification by oxidized phospholipids and hydrolytically released lipid electrophiles: investigating cellular responses. Biochim Biophys Acta. 2012;1818:2424–2435. doi: 10.1016/j.bbamem.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonstad S, Retterstøl K, Ose L, Ohman KP, Lindberg MB, Svensson M. The dual peroxisome proliferator-activated receptor α/γ agonist tesaglitazar further improves the lipid profile in dyslipidemic subjects treated with atorvastatin. Metabolism Clinical and Experimental. 2007;56:1285–1292. doi: 10.1016/j.metabol.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Cavender MA, Lincoff AM. Therapeutic potential of aleglitazar, a new dual PPAR-α/γ agonist: implications for cardiovascular disease in patients with diabetes mellitus. Am J Cardiovasc Drugs. 2010;10:209–216. doi: 10.2165/11539500-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Guerre-Millo M, Gervois P, Raspé E, Madsen L, Poulain P, Derudas B, Herbert JM, Winegar DA, Willson TM, Fruchart JC, Berge RK, Staels B. Peroxisome proliferator-activated receptor α activators improve insulin sensitivity and reduce adiposity. J Biol Chem. 2000;275:16638–16642. doi: 10.1074/jbc.275.22.16638. [DOI] [PubMed] [Google Scholar]
- Elbrecht A, Chen Y, Cullinan CA, Hayes N, Leibowitz M, Moller DE, Berger J. Molecular Cloning, Expression and Characterization of Human Peroxisome Proliferator Activated Receptors γ1 and γ2. Biochem Biophys Res Commun. 1996;224:431–437. doi: 10.1006/bbrc.1996.1044. [DOI] [PubMed] [Google Scholar]
- Johnson TE, Holloway MK, Vogel R, Rutledge SJ, Perkins JJ, Rodan GA, Schmidt A. Structural requirements and cell-type specificity for ligand activation of peroxisome proliferator-activated receptors. J Steroid Biochem Mol Biol. 1997;63:1–8. doi: 10.1016/S0960-0760(97)00064-2. [DOI] [PubMed] [Google Scholar]
- Staels B, Schoonjans K, Fruchart JC, Auwerx J. The effects of fibrates and thiazolidinediones on plasma triglyceride metabolism are mediated by distinct peroxisome proliferator activated receptors (PPARs) Biochimie. 1997;79:95–99. doi: 10.1016/S0300-9084(97)81497-6. [DOI] [PubMed] [Google Scholar]
- Young PW, Buckle DR, Cantello BCC, Chapman H, Clapham JC, Coyle PJ, Haigh D, Hindley RM, Holder JC, Kallender H, Latter AJ, Lawrie KWM, Mossakowska D, Murphy GJ, Cox LR, Smith SA. Identification of high affinity binding sites for the insulin sensitizer rosiglitazone (BRL-49653) in rodent and human adipocytes using a radioiodinated ligand for peroxisome proliferator-activated receptor. J Pharmacol Exp Ther. 1998;284:751–759. [PubMed] [Google Scholar]
- Ferré P. The biology of peroxisome proliferator-activated receptors: relationship with lipid metabolism and insulin sensitivity. Diabetes. 2004;53:S43–S50. doi: 10.2337/diabetes.53.2007.S43. [DOI] [PubMed] [Google Scholar]
- Jiang C, Ting AT, Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998;391:82–86. doi: 10.1038/34184. [DOI] [PubMed] [Google Scholar]
- Ricote M, Li AC, Willson TM, Kelly CJ, Glass CK. The peroxisome proliferator-activated receptor-γ is a negative regulator of macrophage activation. Nature. 1998;391:79–82. doi: 10.1038/34178. [DOI] [PubMed] [Google Scholar]
- Hevener AL, Olefsky JM, Reichart D, Nguyen MT, Bandyopadyhay G, Leung HY, Watt MJ, Benner C, Febbraio MA, Nguyen AK, Folian B, Subramaniam S, Gonzalez FJ, Glass CK, Ricote M. Macrophage PPARγ is required for normal skeletal muscle and hepatic insulin sensitivity and full antidiabetic effects of thiazolidinediones. J Clin Invest. 2007;117:1658–1669. doi: 10.1172/JCI31561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE Guideline CG87. Type 2 Diabetes - newer agents (partial update of CG66) (CG87) http://www.nice.org.uk/CG87.
- Shen LQ, Child A, Weber GM, Folkman J, Aiello LP. Rosiglitazone and Delayed Onset of Proliferative Diabetic Retinopathy. Arch Ophthalmol. 2008;126:793–799. doi: 10.1001/archopht.126.6.793. [DOI] [PubMed] [Google Scholar]
- Chu SH, Li AH. Association of proliferative diabetic retinopathy with insulin use and microalbuminuria. Arch Ophthalmol. 2010;128:147–148. doi: 10.1001/archophthalmol.2009.372. [DOI] [PubMed] [Google Scholar]
- Murata T, He S, Hangai M, Ishibashi T, Xi XP, Kim S, Hsueh WA, Ryan SJ, Law RE, Hinton DR. Peroxisome proliferator-activated receptor-γ ligands inhibit choroidal neovascularization. Invest Ophthalmol Vis Sci. 2000;41:2309–2317. [PubMed] [Google Scholar]
- Emoto M, Anno T, Sato Y, Tanabe K, Okuya S, Tanizawa Y, Matsutani A, Oka Y. Troglitazone Treatment Increases Plasma Vascular Endothelial Growth Factor in Diabetic Patients and Its mRNA in 3 T3-L1 Adipocytes. Diabetes. 2001;50:1166–1170. doi: 10.2337/diabetes.50.5.1166. [DOI] [PubMed] [Google Scholar]
- Fong DS, Contreras R. Glitazone use associated with diabetic macular edema. Am J Ophthalmol. 2009;147:583–586. doi: 10.1016/j.ajo.2008.10.016. [DOI] [PubMed] [Google Scholar]
- Ambrosius T, Danis RP, Goff DC, Greven CM, Gerstein HC, Cohen RM, Riddle MC, Miller ME, Buse JB, Bonds DE, Peterson KA, Rosenberg YD, Perdue LH, Esser BA, Seaquist LA, Felicetta JV, Chew EY. ACCORD Study Group: Lack of association between thiazolidinediones and macular edema in type 2 diabetes. Arch Ophthalmol. 2010;128:312–318. doi: 10.1001/archophthalmol.2009.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palee S, Chattipakorn S, Phrommintikul A, Chattipakorn N. PPARγ activator, rosiglitazone: Is it beneficial or harmful to the cardiovascular system? World Journal of Cardiology. 2011;3:144–152. doi: 10.4330/wjc.v3.i5.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachek LI, Yuzefovych LV, Ledoux SP, Julie NL, Wilson GL. Troglitazone, but not rosiglitazone, damages mitochondrial DNA and induces mitochondrial dysfunction and cell death in human hepatocytes. Toxicol Appl Pharmacol. 2009;240:348–354. doi: 10.1016/j.taap.2009.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpino PA, Goodwin B. Diabetes area participation analysis: a review of companies and targets described in the 2008–2010 patent literature. Expert Opin Ther Pat. 2010;20:1627–1651. doi: 10.1517/13543776.2010.533171. [DOI] [PubMed] [Google Scholar]
- Bhatwadekar AD, Glenn JV, Li G, Curtis TM, Gardiner TA, Stitt AW. Advanced glycation of fibronectin impairs vascular repair by endothelial progenitor cells: implications for vasodegeneration in diabetic retinopathy. Investigative Ophthalmology & Vision Science. 2008;49:1232–1241. doi: 10.1167/iovs.07-1015. [DOI] [PubMed] [Google Scholar]
- Peppa M, Uribarri J, Vlassara H. Glucose, advanced glycation end products, and diabetes complications: what is new and what works. Clinical Diabetes. 2003;4:186–187. [Google Scholar]
- Miranda S, González-Rodríguez Á, García-Ramírez M, Revuelta-Cervantes J, Hernández C, Simó R, Valverde AM. Beneficial effects of fenofibrate in retinal pigment epithelium by the modulation of stress and survival signaling under diabetic conditions. J Cell Physiol. 2012;227:2352–2362. doi: 10.1002/jcp.22970. [DOI] [PubMed] [Google Scholar]
- Dong Y, Steffen BT, Cao J, Tsai AK, Ordovas J, Straka R, Zhou X, Kabagambe E, Hanson NQ, Arnett D, Tsai MY. Effects of fenofibrate on plasma oxidized LDL and 8-isoprostane in a sub-cohort of GOLDN participants. Atherosclerosis. 2011;214:422–425. doi: 10.1016/j.atherosclerosis.2010.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomizawa A, Hattoria Y, Inoueb T, Hattoria S, Kasaia K. Fenofibrate suppresses microvascular inflammation and apoptosis through adenosine monophosphate–activated protein kinase activation. Metabolism. 2011;60:513–522. doi: 10.1016/j.metabol.2010.04.020. [DOI] [PubMed] [Google Scholar]
- Koh KK, Quon MJ, Rosenson RS, Chung WJ, Han SH. Vascular and metabolic effects of treatment of combined hyperlipidemia: focus on statins and fibrates. Int J Cardiol. 2008;124:149–159. doi: 10.1016/j.ijcard.2007.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olukman M, Sezer ED, Ulker S, Sozmen EY, Cınar GM. Fenofibrate treatment enhances antioxidant status and attenuates endothelial dysfunction in streptozotocin-induced diabetic rats. Exp Diabetes Res. 2010. Article ID 828531. [DOI] [PMC free article] [PubMed]
- Dwyer MA, Kazmin D, Hu P, McDonnell DP, Malek G. Nuclear receptor atlas of human retinal pigment epithelial cells: potential relevance to age-related macular degeneration. Mol Endocrinol. 2011;25:360–372. doi: 10.1210/me.2010-0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau K, Roy S, Guo W, Hernández C, Villarroel M, Simó R, Roy S. Fenofibric acid reduces fibronectin and collagen type IV overexpression in human retinal pigment epithelial cells grown in conditions mimicking the diabetic milieu: functional implications in retinal permeability. Invest Ophthalmol Vis Sci. 2011;52:6348–6354. doi: 10.1167/iovs.11-7282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarroel M, Garcia-Ramírez M, Corraliza L, Hernández C, Simó R. Fenofibric acid prevents retinal pigment epithelium disruption induced by interleukin-1β by suppressing AMP-activated protein kinase (AMPK) activation. Diabetologia. 2011;54:1543–1553. doi: 10.1007/s00125-011-2089-5. [DOI] [PubMed] [Google Scholar]
- Kim J, Ahn JH, Kim JH, Yu YS, Kim HS, Ha J, Shinn SH, Oh YS. Fenofibrate regulates retinal endothelial cell survival through the AMPK signal transduction pathway. Exp Eye Res. 2007;84:886–893. doi: 10.1016/j.exer.2007.01.009. [DOI] [PubMed] [Google Scholar]
- Filippatos T, Milionis HJ. Treatment of hyperlipidaemia with fenofibrate and related fibrates. Expert Opin Investig Drugs. 2008;17:1599–1614. doi: 10.1517/13543784.17.10.1599. [DOI] [PubMed] [Google Scholar]
- Ting RD, Keech AC, Drury PL, Donoghoe MW, Hedley J, Jenkins AJ, Davis TM, Lehto S, Celermajer D, Simes RJ, Rajamani K, Stanton K. FIELD Study Investigators: Benefits and Safety of Long-Term Fenofibrate Therapy in People With Type 2 Diabetes and Renal Impairment: The FIELD Study. Diabetes Care. 2012;35:218–225. doi: 10.2337/dc11-1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pubchem CID 3339: Fenofibrate - Compound Summary. http://pubchem.ncbi.nlm.nih.gov/summary/summary.cgi?cid=3339.
- Bandello F, Cunha-Vaz J, Chong NV, Lang GE, Massin P, Mitchell P, Porta M, Prünte C, Schlingemann R, Schmidt-Erfurth U. New approaches for the treatment of diabetic macular oedema: recommendations by an expert panel. Eye (London) 2012;26:485–493. doi: 10.1038/eye.2011.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simó R, Hernández C. Intravitreous anti-VEGF for diabetic retinopathy: hopes and fears for a new therapeutic strategy. Diabetologia. 2008;51:1574–1580. doi: 10.1007/s00125-008-0989-9. [DOI] [PubMed] [Google Scholar]
- Nicholson BP, Schachat AP. A review of clinical trials of anti-VEGF agents for diabetic retinopathy. Graefes Archive for Clinical and Experimental Ophthalmology. 2010;248:915–930. doi: 10.1007/s00417-010-1315-z. [DOI] [PubMed] [Google Scholar]
- Abu El-Asrar AM, Al-Mezaine HS. Saudi Journal of Opthalmology. 2011. pp. 113–122. [DOI] [PMC free article] [PubMed]
- Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, Sutter F, Simader C, Burian G, Gerstner O, Weichselberger A. RESTORE study group: The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118:615–625. doi: 10.1016/j.ophtha.2011.01.031. [DOI] [PubMed] [Google Scholar]
- Nguyen QD, Shah SM, Heier JS, Do DV, Lim J, Boyer D, Abraham P, Campochiaro PA. READ-2 Study Group: Primary End Point (Six Months) Results of the Ranibizumab for Edema of the Macula in Diabetes (READ-2) study. Ophthalmology. 2009;116:2175–2181. doi: 10.1016/j.ophtha.2009.04.023. [DOI] [PubMed] [Google Scholar]