Abstract
To delineate the critical features of platelets required for formation and stability of thrombi, thromboelastography and platelet aggregation measurements were employed on whole blood of normal patients and of those with Bernard-Soulier Syndrome (BSS) and Glanzmann’s Thrombasthenia (GT). We found that separation of platelet activation, as assessed by platelet aggregation, from that needed to form viscoelastic stable whole blood thrombi, occurred. In normal human blood, ristocetin and collagen aggregated platelets, but did not induce strong viscoelastic thrombi. However, ADP, arachidonic acid, thrombin, and protease-activated-receptor-1 and -4 agonists, stimulated both processes. During this study, we identified the genetic basis of a very rare double heterozygous GP1b deficiency in a BSS patient, along with a new homozygous GP1b inactivating mutation in another BSS patient. In BSS whole blood, ADP responsiveness, as measured by thrombus strength, was diminished, while ADP-induced platelet aggregation was normal. Further, the platelets of 3 additional GT patients showed very weak whole blood platelet aggregation toward the above agonists and provided whole blood thrombi of very low viscoelastic strength. These results indicate that measurements of platelet counts and platelet aggregability do not necessarily correlate with generation of stable thrombi, a potentially significant feature in patient clinical outcomes.
Introduction
An initial step in thrombus formation in the injured vascular endothelium is the adhesion of platelets to exposed subendothelial components, e.g., von Willebrand Factor (vWF), under high rates of shear, via the interaction of the platelet glycoprotein (GP) 1b/V/IX receptor complex with subendothelial vWF [1]. This tethering of platelets then promotes their firmer binding to subendothelial collagen (COL) fibers via platelet receptors, e.g., GPVI [2], [3] and integrin αIIβ1 [4]. During this process, platelets are activated, leading to platelet shape changes, aggregation, release of aggregation agonists, e.g., ADP and Ca2+, from dense granules, and release of other biologically active agents, e.g, growth factors, hemostasis agents, and adhesion proteins, from α-granules [5]. The elevation of intracellular Ca2+ results in enzymatic liberation of arachidonic acid (AA) from phospholipids, subsequently forming thromboxane A2 (TxA2), which induces platelet activation. Other signaling events occur as a result of agonist-platelet receptor interactions, one example being ADP interactions with its platelet receptor, P2Y12 [6], which results in activation of the integrin complex, αIIb/β3, the major fibrinogen receptor on platelets [7]. This step promotes platelet aggregation via fibrinogen bridging and thrombus growth.
Discrete steps of platelet activation have been studied in vitro by exogenous activators, e.g., ADP and AA. Additional studies employing gene-altered mice and patients with specific platelet dysfunctions, e.g., GPIb defects in Bernard Soulier Syndrome (BSS) [8], and αIIb/β3 abnormalities in Glanzmann’s Thrombasthenia (GT), have also been employed to establish mechanisms of platelet function. We propose that additional significant advances can be made by employing the critical end-point of whole blood thrombus-based examination of platelet function, in combination with platelet aggregation studies, which would expand knowledge on relationships between the receptor interactions leading to platelet aggregation and stable thrombus formation. We undertook such a study, with the aid of blood from very rare BSS and GT patients. The results of this investigation are reported herein.
Materials and Methods
Blood Collection
This study was designed to be consistent with the US CFR and ICH Guidelines on Good Clinical Practices. Venous human blood was collected by licensed phlebotomists from 10 normal males and females, two female BSS patients (BSS-1 and BSS-2), both heterozygous parents of one of the BSS (BSS-1M and BSS-2F) patients, one male GT (GT-1) patient, 2 female GT patients (GT-2 and GT-3), and the heterozygous mothers of the two female GT patients (GT-2M and GT-3M), none of whom reported interfering medications or recent platelet infusions. Polystyrene vacutainer tubes, containing either 3.2% sodium citrate (9∶1 v:v), 75 U of Na+-heparin, or 1.8 mg EDTA/ml, were used. CBCs and metabolic profiles were rapidly obtained on EDTA-treated blood. PT, aPTT, and fibrinogen levels were determined using Diagnostica Stago (Parsnippany, NJ) STArt kits and a STArt-8 hematology analyzer. IRB approval was obtained from Memorial Hospital of South Bend (MHSB) and informed consent forms were signed by all control and subject patients in accord with the Declaration of Helsinki.
Blood Smears
Blood smears were fixed on slides with methanol, stained with Volu-Sol (Salt Lake City, UT) Dip Stain, and fixed with Volu-Sol Stain Solution. The washed and air-dried slides were coverslipped with Permount mounting medium (Electron Microscopy Sciences, Hatfield, PA) and examined microscopically. Platelet sizes, measured as the diameter at the longest axis, were acquired from the images. Each image contained 4–10 platelets/field, and 3–10 images/blood smear were obtained.
Sequencing of WBC DNA
Genomic DNA from WBC was used for PCR cloning of the exons. Traditional Sanger sequencing was accomplished using an ABI 3730×l 96-capillary sequencer with a variety of custom designed primers for the complete exon 2 of the GP1b gene (GPIBA), which contains the entire GPIb protein open reading frame (ORF), for BSS-1 and BSS-2. Similarly, to identify the genetic abnormalities in GT-1, primers were designed to amplify all 30 exons of the gene (ITGA2B) encoding the ORF of integrin αIIb (CD41) and all 15 exons of the gene (ITGB3) coding for the ORF of integrin β3 (CD61), along with the intron flanking regions of each exon to insure integrity of splice sites. 4Peaks software (Amsterdam, The Netherlands) was used for viewing and editing sequence trace files with a Mac OSX 10.6.6 system.
Clot Retraction
Control and subject blood samples were separately drawn into vacutainer serum tubes and allowed to stand vertically undisturbed for 30 min. A Nikon digital SLR camera suspended by a tripod, captured a picture of the specimen along the transverse plane looking vertically down the tube.
Flow Cytometric Analysis (FCA)
Staining of platelets
Staining of platelets from platelet rich plasma (PRP) was performed according to the protocol from BD Biosciences with slight modifications. Freshly drawn blood in heparin was centrifuged at 80×g for 20 min and the top PRP layer was gently removed and fixed with 2% paraformaldehyde at room temperature for 10 min. The platelets were treated 2× with wash solution (1% FBS/1X PBS) with centrifugation at 750×g for 10 min. After the final wash, the platelets were resuspended in 6 ml of this same solution. An aliquot of 100 µl platelets were utilized to label with rabbit-anti-human β3 antibody (1∶10 dilution) (#AP8672b, Abgent, San Diego, CA). This antibody recognizes the peptide region 740–769 at the C-terminal β3 region of GPIIIa. After 30 min at room temperature, the platelets were washed once and then incubated with donkey-anti-rabbit Alexa Fluor488-conjugated 2° antibody (Molecular Probes, Carlsbad, CA) in the dark for 30 min at room temperature.
Aliquots (100 µl) of fixed platelets were also labeled for different experiments with 0.125 µg each of FITC mouse anti-human αIIb antibody (#555466, BD Pharmingen, San Jose, CA), FITC mouse anti-human β3 antibody (#555753 BD Pharmingen), PE mouse anti-human GPIb antibody (#555473 BD Pharmingen), PE mouse anti-human α2b antibody (integrin β1) (#556049 BD Pharmingen), FITC mouse anti-human GPIa (integrin α2) (BD Pharmingen #555498), PE mouse IgG1 isotype control (#555749 BD Pharmingen), and FITC mouse IgG1 isotype control (#555748, BD Pharmingen). All labeled platelet suspensions platelets were finally washed once, resuspended in 1% paraformaldehyde, and analyzed by FCA.
FCA of labeled platelets
A 3 laser 9 color FACSAria III (BD Biosciences, San Jose, CA) was utilized for FCA of the labeled platelets using the FITC and PE channels. Acquisition and analysis were performed by gating on side scatter (SSC-H) and fluorescence (FITC-β3), setting the scales to logarithmic amplification. Cells in suspension were analyzed at a flow rate of 1 ml/sec and 10,000 events were recorded for analysis.
Thromboelastography (TEG)
For TEG analyses of recalcified whole blood, 20 µl of 0.2 M CaCl2 was added to 340 µl of citrated blood. Data were collected for 1.5–2.0 hr. Rapid thromboelastograms were obtained after addition of 20 µl of 0.2 M CaCl2 and 10 µl of the Rapid TEG kit mixture (Haemoscope, Niles, IL), containing reconstituted soluble human Tissue Factor (sTF)/kaolin/phospholipid, to 340 µl of citrated blood. Thrombin-enhanced thromboelastograms contained 1 unit thrombin (ERL, South Bend, IN)/20 µl 0.2 M CaCl2 and 340 µl of citrated blood. Kaolin-stimulated thromboelastograms were obtained using 1 ml of citrated whole blood and kaolin solution (Haemoscope). Then, 360 µl of blood was placed in the cup with 20 µl of 0.2 M CaCl2. To assess the competency of the human fibrinolytic system, 200 ng of human tissue-type plasminogen activator (htPA) ±5 mM ε-aminocaproic acid (EACA), was added to the reaction vessels along with the Ca2+/sTF/kaolin sample.
TEG data were collected using an automated Thromboelastograph 5000 (Haemoscope) and analyzed using Haemoscope TAS Version 4.3 Software. The hemostasis parameters obtained were: R, the time from the start of the reaction until the onset of thrombus formation; K20, the time from R to a 20-mm clot strength signal; A, the angle in degrees, which reflects the rate of clot formation; MAmax, the maximum amplitude (mm) attained, which is a reflection of the contributions of crosslinked fibrin and platelets to thrombus strength; and the fibrinolysis parameters, LY30 and LY60, which are the percent reductions of the area under the thromboelastograms from the time that MAmax is attained until 30 and 60 min, respectively, after MAmax.
Platelet Functionality in Thrombus Formation Measured by TEG
For TEG-based platelet analyses, 360 µl of the kaolin/blood sample was added to 20 µl of saline/20 µl of 0.2 M CaCl2. In a separate reaction cup, 10 µl of the Activator F kit (reptilase+human (h)FXIIIa) was mixed with 360 µl of heparinized blood to obtain the contribution to the MAmax of crosslinked fibrin alone (MAF). In other assays, 10 µl of Activator F and 360 µl of heparinized blood were employed, and either the recommended 10 µl of the ADP kit solution, 10 µl of the AA kit solution, 12 µl of 10 mg/ml ristocetin (RIST), 10 µl of 100 µg/ml of COL; 12 µl of 1 mM of the protease activated receptor (PAR)-1 agonist, PA-1 (H-SFLLRN-OH; Anaspec, Fremont, CA), or 12 µl of 20 mM PAR-4 agonist, PA-4 (H-GYPGKF-NH2; Anaspec), to activate platelets. The MAmax for the reaction obtained with each platelet activator - MAF provides MAP. The MAmax with Ca2+/kaolin - MAF, yields MAK. The % stimulations were calculated as: MAP/MAK×100.
Platelet Aggregometry
For human blood, 300 µl saline and 300 µl heparinized blood were mixed in the reaction cup of a Multiplate impedance aggregometer (Verum Diagnostica, Munich, Germany), followed by a 3 min incubation. Then, 20 µl of 0.2 mM ADP, 20 µl of 15 mM AA, 20 µl of 100 µg/ml COL, 50 µl of 10 mg/ml RIST, 20 µl of 1 mM PA-1, or 12 µl of 20 mM PA-4 were added and recordings initiated.
In all cases, measurements were recorded for 6 min and plotted by the software as arbitrary aggregation units (AU) versus time. The areas under each curve, from 0–6 min, were taken as the platelet aggregation response.
Results
BSS Patients
Two of these extremely rare patients were identified for study and were diagnosed in other facilities earlier in life.
Patient BSS-1
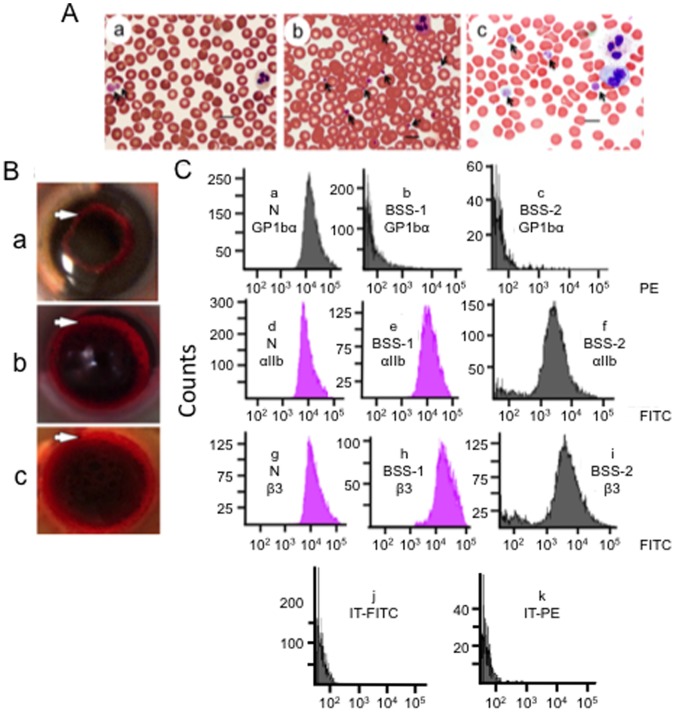
This patient is a 21-year old Caucasian female from a nonconsanguinous parental relationship, diagnosed with BSS at age 7, who has had numerous platelet transfusions throughout her life. At presentation to our facilities, her CBC was normal, except for platelet counts of 28K/µl-50K/µl on three occasions 2–3 months apart (Table 1). Her blood smears displayed large and giant platelets (Figure 1A–a; Table 1), with 72% >4 µm, compared to a normal control (Figure 1A–b; Table 1). Her plasma PT, aPTT, and fibrinogen levels were normal (Table 1), indicating that plasma-based hemostasis was unaffected by her disease.
Table 1. CBC and plasma hemostasis parameters.
| Human | Fibrinogen (mg/dl) | PT (sec) | aPTT (sec) | Plateletsc (×103/µl) | Hemoglobin (g/dl) | WBC (×103/µl) |
| Controlsa | 272±13 | 11.5±0.2 | 32.0±1.1 | 227±36 24%, 1–2 µmd 76%, 2–4 µmd | 13.9±0.4 | 7.1±0.5 |
| BSS-1b | 264; 261 | nd; 11.2 | 33.5; 29.4 | 37±7 28%, 1–2 µmd 68%, 2–4 µmd 4%, 4–8 µmd | 11.5; 11.7 | 5.8; 6.7 |
| BSS-2b | 384; 317; 351 | 10.9; 10.5; 10.4 | 24.9; 26.3; 26.3 | 59; 32 0; 14%, 1–2 µmd 17; 5%, 2–4 µmd 66; 38%, 4–8 µmd 17; 43%, 8–12 µmd | 13.6; 13.6 | 7.5; 9.3 |
| GT-1b | 402; 428; 390 | 9.9; 10.5; 10.2 | 24.7; 26.6; 25.6 | 130; 130; 117 3%, 1–2 µmd 53%, 2–4 µmd 43%, 4–6 µmd 2%, 6–8 µmd | 12.8; 13.5; 13.2 | 3.4; 3.5; 3.7 |
| GT-2 | 282 | 10.8 | 25.6 | 202 4%, 1–2 µmd 68%, 2–4 µmd 28%, 4–6 µmd | 11.2 | 8.7 |
| GT-3 | 337 | 10.2 | 27.0 | 224 3%, 1–2 µmd 72%, 2–4 µmd 25%, 4–8 µmd | 13.7 | 7.9 |
Normal human controls, N = 10.
Data are from separate blood draws >4 months apart.
Manual counts with Wright stain.
Average size distribution of platelets.
Figure 1. Platelets of BSS patients.
(A) Blood smears were stained with Volu-Sol Dip Stain. (a) BSS-1. The platelets (arrows) vary in size and exhibit a granular composition with a fuzzy coat. Giant platelets (>5 µm) are indicated by arrows. (b). Normal blood showing platelets (arrows) at 1–3 µm diameter. (c) BSS-2. Giant platelets (>5 µm) are indicated by arrows. The blood smears were viewed with a Nikon E600 Eclipse microscope containing a Plan Apo VC 100×/1.40 N.A. Oil lens, acquired with a Nikon DS Ri1 color digital camera via Nikon Elements AR 3.2 imaging software, and saved as TIFF files. Measurements of cells were obtained with the measurement tool of the Nikon Elements-AR 3.2 imaging software. The bars on all images represent 10 µm. (B) Whole blood clot retraction of (a) BSS-1, (b) normal human, and (c) BSS-2 clots. Similar rings of retraction (white arrows) are observed in normal control and BSS blood after 30 min. (C) Flow cytometric analysis of formaldehyde-fixed platelets of PRP from normal (N) blood and PRP from BSS-1 and BSS-2. Surface expression of platelet GPIbα (CD42b) in a (a) normal control. GPIbα is greatly reduced and similar to the isotype control in (b) BSS-1 and (c) BSS-2 platelets. Surface expression of integrin αIIb (CD41) in a (d) normal control, as well as (e) BSS-1 and (f) BSS-2 platelets. Surface expression of integrin β3(CD41) in αIIb/β3 in a (g) normal control, and (h) BSS-1 and (i) BSS-2 platelets. Normal-to-increased expression of integrin αIIb and the αIIb/β3 complex is observed in BSS platelets. (j, k) Isotype control for (j) FITC and (k) PE with normal platelets; BSS-1, BSS-2, GT-1, GT-2, and GT-3 platelets showed very similar controls.
Patient BSS-2
This patient is a 61-year old Hispanic female diagnosed with BSS at age 2, also frequently administered platelets for clinical procedures, but none within a month of her 3 visits to us that occurred 4 months apart. Her PT, aPTT, and fibrinogen levels were also normal (Table 1). While her WBC count was also normal, her blood sample also showed macrothrombocytopenia (Figure 1A–c; Table 1), with large (4–8 µm) and giant (>8 µm) platelets present, the latter comprising approximately 17% of her total platelets (Table 1).
Whole Clot Retraction of BSS Blood
Whole blood clot retraction studies, an important property of functional platelets, showed a clear clot retraction ring in control normal blood (Figure 1Bv), as well as for the blood of BSS-1 (Figure 1B–b), reflecting the formation of a thrombus that retracts from the sides of the tube. This property of platelets stimulates healthy wound healing, and suggests normal platelet function in this regard. Whole blood clot retraction for BSS-2 blood was also normal (Figure 1B–c).
Molecular Genetics of BSS Patients
Patient BSS-1
Based on our sequence analysis of the GPIBA gene of BSS-1, she was determined to be doubly heterozygous for GPIBA gene mutations. Of the genomic DNA clones tested, 6 showed deletion of a single nucleotide, G952 (numbered from the A1TG translation initiation site), altering translation to A318P (the Met at the translation initiation site is designated amino acid 1), followed by a frame-shift mutation (Figure 2A, B) and a stop codon beginning at sequence position-334. This GPIBA mutation has not been previously identified in BSS. After in silico reinsertion of G952 and translation, the protein showed two tandem exact 13-amino acid residues repeats, at amino acids 415–440, in the VNTR locus of the protein (allele C of GPIb). Variable numbers (1–4) of these polymorphic tandem exact VTNR repeats in GPIb have been reported [9]. Other polymorphisms have been noted in this protein and have assisted in tracking the genetic pools of the mutations leading to BSS. GPIb, associated with the G952 deletion in BSS-1, does not carry the RS polymorphism (T to C) at nucleotide-5 [10], the T161M protein polymorphism (Ko) [11], the silent EF polymorphism (C to T) at the 3rd nucleotide of N258 [10], or the silent KL polymorphism (A to G) at the 3rd nucleotide of R358 [10].
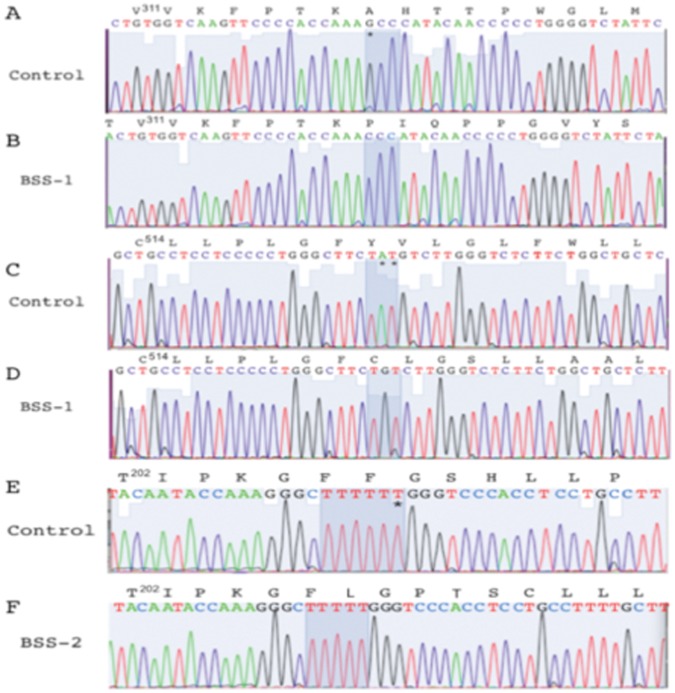
Figure 2. Nucleotide sequence of the mutated regions of GPIBA in BSS patients.
In each case, the sequence data are displayed for one example PCR clone within the GPIBA gene in the genome, along with the readouts of the nucleotides of the translated products. No uncertainties were noted in any clones sequenced in these regions. (A) Normal human GPIBA sequence of the region spanning amino acids V311–M326 of GP1b. (B) The 1st nucleotide (G*) of the codon for A318 is deleted in the paternal allele of BSS-1 (A), thus altering the reading frame of the protein. (C) Normal human GP1b sequence of the region spanning amino acids C514–L529. (D) The 2nd and 3rd nucleotides (A*T*) of the codon for Y521 are deleted in the maternal allele of BSS-1 (C), thus altering the reading frame of the protein. (E) Normal human GP1b sequence of the region spanning amino acids T202–V214. (F) A single T of the group of 6 T residues encoding F207–F208 of GP1b has been deleted (*) in both alleles of BSS-2 (E), altering the reading frame of the protein. The protein sequences are numbered from M1 of the ORF. The corresponding nucleotide sequences are numbered from the 1st residue of the ATG translation initiation sequence.
Another group of 9 clones, showed that two nucleotides (A1562–T1563) of GPIBA were deleted (Figure 2C,D), altering translation to Y521C in the transmembrane domain of the protein, followed by a frame-shift mutation, resulting in a stop codon at sequence position 602. This latter mutation has been reported in other BSS patients [12], [13]. The translated sequence of the protein, with in silico reinsertion of the two deleted nucleotides, showed it also to be allele C in the VNTR locus of GP1b. The gene associated with GPIBA[ΔA1562–T1563] carries the RS and KL polymorphisms, but not the Ko or EF polymorphisms, in common with the previous two patients described with this altered allele [12], [13]. No WT GPIBA subclones were found in the DNA of BSS-1.
Blood was obtained from the biological parents of BSS-1 for the study, and both proved to be carriers of one of the two mutations within the GPIBA gene of the daughter. Their sequence data were clear in that the paternal GPIBA mutant allele possessed GPIBA[ΔG952] (11/23 subclones), and its translation after reinsertion of G952 showed the protein to contain allele C in GPIb, but no other GPIBA polymorphism. The father of BSS-1 also carried WT GPIBA 12/23 subclones). The maternal GPIBA mutant allele possessed GPIBA[ΔA1562–T1563] (3/9 subclones), and, after in silico reinsertion of A1562–T1563 and translation, the protein also contained allele C of GPIBA, and the RS and KL polymorphisms. The maternal genomic DNA also possessed WT GPIBA (6/9 subclones). The CBCs of each parent were within normal limits, but the paternal manual platelet count was low at 39K/µl. Blood smears showed large platelets (34% 4–8 µm). The maternal platelet count was 174K/µl and platelet sizes were normal (95% 2–4 µm).
Patient BSS-2
Biological relatives of BSS-2 were unavailable. Nonetheless, we suspected the presence of a homozygous double deficiency of GPIBA, since her parents were 2nd cousins, as reported by BSS-2. Our sequence analysis of her GPIBA gene revealed one population of subclones (20 total), with a deletion of one T in a T-rich segment of the DNA, viz., C618TTTTTTG in control GPIBA and C618TTTTTG in the patient sample (Figure 2E,F), a mutation that has not been previously reported in BSS. This change generated a F208L mutation in the patient GPIb, followed by a frame-shift mutation in the gene resulting in a stop codon at sequence position 255. Examination of the remainder of the DNA and translated product, after in silico reinsertion of the deleted T, showed it to possess the C allele in the VTNR region of GPIBA, but not the RS, Ko, EF, or KL polymorphisms.
We thus conclude that the three allelic mutated GPIBA genes that are present in BSS-1 and BSS-2 originated from different founder lines, and BSS-1 represents an extremely rare case of a double heterozygote for two different GPIb inactivating mutations, resulting in BSS. There is no evidence of consanguinity in the family of BSS-1. Thus, this genetic trait resulted from a chance breeding of two different founder lines. To our knowledge, only one other double heterozygote for a GP1b-deficient BSS patient has been fully characterized, and contains separate allelic protein mutations of [C81R] (renumbered according to our system for consistency) and [W527stop] [14]. These published mutations differ from those described herein. On the other hand, BSS-2 is homogyzous for GPIBA inactivating mutations, also resulting in BSS, that originated from a consanguineous breeding of a single founder line, a more common occurrence in BSS.
FCA of BSS Platelets
PRP isolated from a normal control (N) showed the presence of the platelet surface receptors, GP1bα (Figure 1C-a), integrin αIIb (Figure 1C-d), and integrin β3 in αIIb/β3 (Figure 1C-g). On the other hand, PRP from BSS-1 and BSS-2 demonstrated the absence GP1bα (Figure 1C-b and Figure 1C-c). BSS-1 showed intact-to-increased amounts of integrins αIIb (Figure 1C-e) and β3 in αIIb/β3 (Figure 1C-h), and BSS-2 demonstrated near normal levels (>75%) of αIIb (Figure 1C-f) and β3 in αIIb/β3 (Figure 1C-i). Thus, the interaction of VWF with platelets is adversely affected by the loss of GP1bα, but contains both protein components of the fibrinogen receptor, αIIb/β3.
GT Patients
Three of these very rare patients were studied.
Patient GT-1
This 61-year old male, diagnosed with GT in the mid-1960s, is the offspring of nonconsanguineous parents. Only patient blood was available, since his parents are deceased and there are no siblings. Plasma-based coagulation assays for GT-1 were found to be within the normal range, although his fibrinogen level was at the high end of normal (Table 1). Platelet counts of GT-1 were at the lower limit of normal and, by manual counts, the size distributions of GT-1 platelets had components (45%) that were larger than normal (Table 1). The hemoglobin concentration of GT-1 was normal, while the WBC count was low (Table 1).
Patient GT-2
This patient is a female offspring of nonconsanguineous parents who was diagnosed with GT at 4 weeks of age. She was 20 years of age upon arrival to our facilities, accompanied by her biological mother (GT-2M), who did not show outward symptoms of GT, and did not report a history of the disease. GT-2M provided blood for this study. Plasma-based coagulation assays on GT-2 were found to be normal, as were platelet and WBC counts (Table 1). The size distribution of the platelets of GT-2 were similar to GT-1 and had a small population of large platelets (Table 1).
Patient GT-3
This 16-year old Caucasian female was diagnosed with GT at age 3 years because of frequent and severe nosebleeds. She also has a history of bruising very easily. This patient has had one platelet transfusion because of nosebleeds (age uncertain). At various times, GT-3 has been administered rFVIIa, amicar, and tranexamic acid for nosebleeds. Apparently, she was provided rFVIIa elsewhere for self-administration when needed. She is taking low dose estrogen and reports recent normal menstrual cycles. Plasma coagulation parameters, as well as CBCs, were normal (Table 1) and her cells showed a small population of slightly larger platelets >4 µm. GT-3 was accompanied to our facilities by her asymptomatic mother (GT-3M), who also volunteered blood for this study.
Molecular Genetics of GT Patients
Patient GT-1
Genetic analyses had not been previously performed on patient GT-1. Thus, nucleotide sequences of all exons of the ITGA2B (integrin αIIb) and ITGB3 (integrin β3) were determined on this patient. In total, the primers designed provided amplicons covering all exons and splice sites in both genes and about 50% of the introns. These sequences were compared to those of ITGA2B and ITGB3 in the GenBank database.
We did not find mutations in ITGA2B exons. As with WT ITGA2B, introns 5 and 8 were flanked by the GC-AG dinucleotide donor and acceptor sequences at their 5′ and 3′ termini, respectively. The GC-AG splice site is the major (∼1%) variant of the standard GT-AG (99%) sequences found at intron flanking positions, and is recognized by the spliceosome [15]. Thus, ITGA2B appears genetically intact in this patient. The ITGB3 gene showed two high frequency mutations in its exons in the patient samples. In one, a [G30,612C] alteration (Figure 3A, B) occurred (numbered from the A1TG translation initiation site) located in exon 4, which is the 2nd nucleotide of the DNA codon (CGG) for R131 in WT-β3 integrin (the Met at the translation initiation site is amino acid 1). This mutation yields the DNA codon, CCG, translating to P131, thus providing the mutated protein, integrin β3[R131P]. This same change occurred in 6/11 subclones sequenced, suggesting that this mutation is present on one allele of the patient. A total of 5/11 subclones showed the WT codon for amino acid R131 at this location, thus demonstrating that the β3 is heterozygous for the [R131P] mutation, which likely occurred from one parent. All introns were flanked by the standard consensus dinucleotide sequences, GT-AG, at the 5′ and 3′ termini of the introns, respectively, in at least 8/8 subclones sequenced.
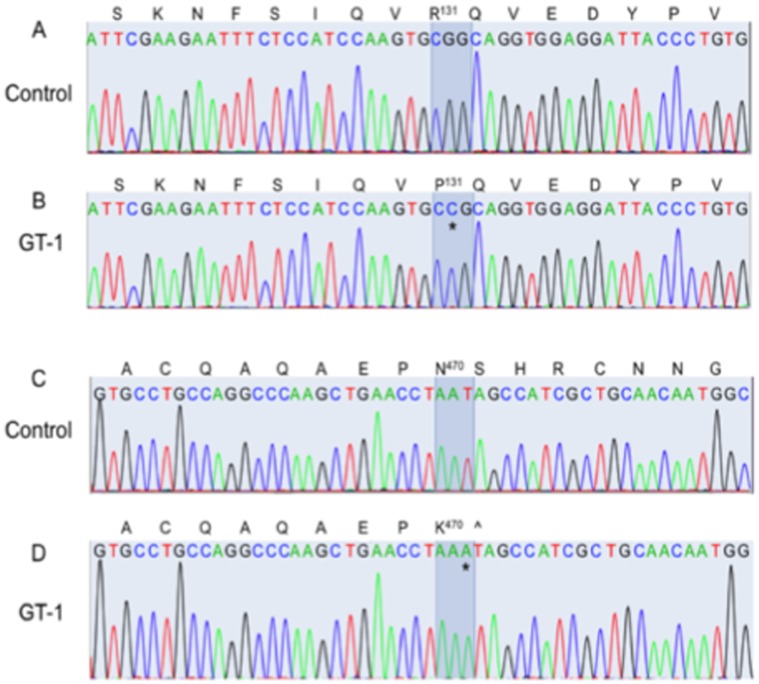
Figure 3. Nucleotide sequence of the mutated regions of the ITGA2B and ITGB3 integrin genes in GT patients.
(A–D) GT-1. In each case, the sequence data are displayed for one example PCR clone within the ITGB3 gene in the genome, along with the readouts of the nucleotides of the translated products. No uncertainties were noted in any clones sequenced in these regions. The ITGA2B gene did not show mutations from WT ITGA2B in any region of the gene. (A) Normal human ITGB3 sequence of the region coding for amino acids S123–V138 of WT αIIb. (B) The 2nd nucleotide (G) of the codon for R131 is mutated from G to C(*) in GT-1, thus altering R131 to P131 in the translated product. (C) Normal human ITGB3 sequence of the region spanning amino acids A462–G477. (D) An insertion mutation of an A in the 3rd nucleotide (*) of the codon for N470 alters this amino acid to K470 and shifts the reading frame such that a stop codon (∧) in the ITGB3 gene of GT-1 replaces the WT amino acid, S471. All protein sequences are numbered from Met1 of the ORF of the protein. All corresponding nucleotide sequences are numbered from the 1st residue of the ATG translation initiation sequence.
A second mutation was found in another location of the ITGB3 gene of GT-1, specifically insertion of an A38,427 (Figure 3C, D), located in exon 10. This mutation altered the WT-AAT codon to AAA, providing the mutation, [N470K], and altering the reading frame such that a [S471stop] occurred in the β3 protein. A total of 5/11 subclones contained this mutation, while the others displayed the WT amino acid, S471, at this position. This mutation most likely occurred in the other parental allele. No other alterations occurred in the exons or intron splice junctions in ITGB3 in this patient.
Thus, the complete genetic data show that GT-1 is doubly heterozygous in the ITGB3 alleles, with one parent providing the [R131P] mutation, and the other transmitting the [N470S471]/[K471stop] mutations. Since GT is an autosomal recessive disorder, it would appear that either mutation, in itself, would inactivate the αIIb/β3 complex, thus severely attenuating fibrin(ogen)-dependent platelet aggregation and platelet contributions to stable clot formation, as is seen experimentally. We conclude that patient GT-1 is a double heterozygote of two β3 integrin inactivating mutations.
Patient GT-2
The genetics of GT-2 have been previously studied and a 6 residue deletion (G1392TAGAC; numbered from A1TG) was found in exon 13 of the ITG2AB gene [16], corresponding to a 2 amino acid (V453D454; numbered from M1) deletion in integrin αIIb protein. This deletion eliminated two highly conserved amino acids from the fourth Ca2+ binding domain of αIIb, resulting in diminished surface expression of αIIb and a loss of the native conformation of the heterodimeric αIIb/β3.
Patient GT-3
Molecular genetic testing was not performed on GT-3 or GT-3M.
Deposition of Nucleotide Sequences
Nucleotide sequences of the abnormal maternal (BSS-1M) and paternal (BSS-1F) GP1BA alleles, both of which are inherited by BSS-1, the homozygous abnormal GP1BA alleles of BSS-2, the ITGB3 abnormal alleles in patient GT-1, and one abnormal ITG2AB allele of GT-2 have been deposited in the GenBank database. The accession numbers for the 5 sequences are KC120774-KC120778.
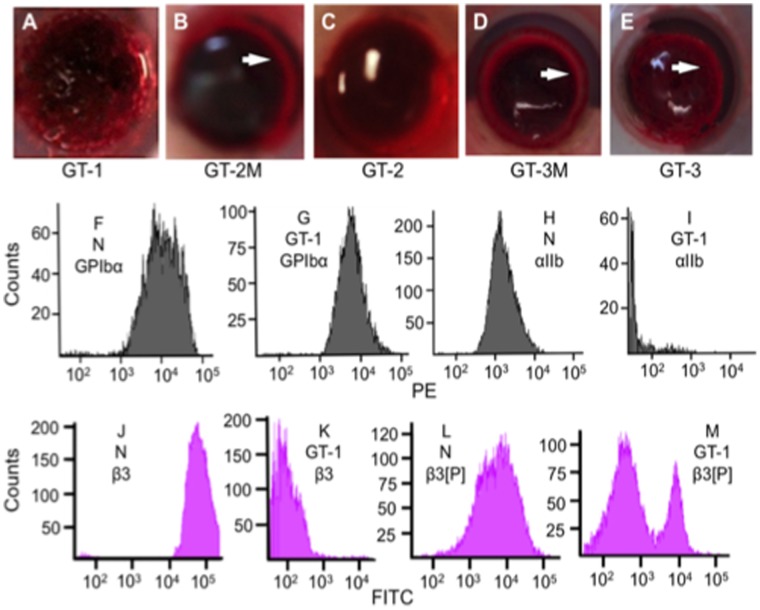
Clot Retraction Studies of GT Patients
Clot retraction performed on the GT specimens were variable. GT-1 (Figure 4A), showed no clot retraction after 30 min and instead revealed a homogeneous image without any distinctive contractile movement along the transverse plane, demonstrating impaired platelet function. Clot retraction of GT-2M (Figure 4B) whole blood was normal, while GT-2 (Figure 4C) showed weaker retraction tendencies (∼2% of WT) than WT blood. The blood of GT-3M (Figure 4D) was normal in this regard, and that of GT-3 (Figure 4E) showed ∼50% of GT-3M retraction after 30 min. The weaker retraction properties of GT blood are due to the genetic functional attenuation of receptor αIIb/β3, which mediates platelet contraction and aggregation [16]. These three patients appear to have variable disease severity, as measured by clot retraction properties, with GT-1 the most profound example of GT, and GT-3 the least. This diversity in properties is likely due to the wide array of possible mutations present in αIIb and β3.
Figure 4. Platelets of GT patients.
Whole blood clot retraction of (A) GT-1, (B) GT-2M, and (C) GT-2, (D) GT-3M, and (E) GT-3 clots. A ring of retraction (white arrows) is observed in GT-2M and GT-3M clots, whereas the GT-1, GT-2, and GT-3 specimens displayed much weaker retraction at 30 min. (F-M) Flow cytometric analysis of normal and GT-1 PRP. (F, G) Surface expression of GP1bα (CD42b) in (F) normal and (G) GT-1 platelets show similar expression levels of GP1bα. (H, I) Surface expression of integrin αIIb (CD41) in (H) normal and (I) GT-1 platelets show reduced expression of CD41 in GT-1 platelets, likely owing to the reduced levels of β3 and thereby reduced amount of surface αIIb/β3 complexes. (J) Surface expression of integrin β3 (CD61) in normal platelets from PRP shows one peak demonstrating the presence of integrin β3 in the αIIb/β3 complex. (K) Surface expression of platelet β3 of αIIb/β3 in GT-1 PRP shows a lack of reactivity of platelets with this antibody. (L) Surface expression of integrin β3[740–769] (β3[P]) in normal PRP. (M). Surface expression of integrin β3[740–769] (β3[P]) in GT-1 PRP. The downfield peak in (M) is similar to isotype controls and likely corresponds to the protein expressed by the truncated allele of integrin β3 in αIIb/β3 in this patient. The smaller peak in (M) to the right shows a reactivity with the full-length allele of integrin β3 in this complex, which harbors the [R131P] mutation but expresses the [740–769] peptide region of the protein.
FCA of the GT Platelets
Patient GT-1
PRP specimens from GT-1 were analyzed by FCA. A comparison of the FCA graphical representations of normal (N) PRP (Figure 4F) and GT-1 PRP (Figure 4G) shows a normal level of GP1bα. However, when compared to a normal control (Figure 4H), GT-1 displayed a near complete loss of reactivity of the antibody to integrin αIIb (Figure 4I), and was comparable in strength to the isotype IgG1 control. Upon examination of integrin β3 with a conformational antibody to β3 in the αIIb/β3 complex, less than 5% of normal β3 (Figure 4J) was evidenced in the platelets of GT-1 (Figure 4K). Another CD61 antibody, that recognizes the peptide region encompassing amino acids [740–769], reacts with control WT platelets (Figure 4L), but shows mixed reactivity in GT patients (Figure 4M). Since β3 in GT-2 platelets has a stop codon at amino acid 471, the β3 translated by this allelic DNA would not be expected to react with this antibody. This is borne out, as seen by one population in Figure 4M that is similar to the isotype control. However, the other allele of GT-1 platelets would translate a full-length mutated β3 protein, which, if stably produced, would react with this antibody, as seen in the second upfield population of Figure 4M. The results with these two antibodies are in agreement with the DNA sequencing that showed that this patient generates a mutated full-length β3 on one allele and a truncated allele on the other, but the conformation of this protein is altered from the WT protein.
Patient GT-2
The platelets in the PRP of patient GT-2 also displayed normal levels of GP1b, when compared to samples taken from GT-2M, her biological mother (Figure 5A, B). However, reactivity to anti-integrin αIIb was very weak compared to her mother (Figure 5C, D). This suggests a significant loss of the surface native αIIb epitope in GT-2 platelets. Similarly, a loss in reactivity of the conformational epitope to anti-CD61 (β3) is noted in the αIIb/β3 complex on the platelet surface of GT-2, as compared to the platelets of GT-2M (Figure 5E, F). With this antibody, one population displaying no antibody binding was observed, and a second upfield population displaying very weak antibody binding was also seen (Figure 5E, F). Similarly, approximately 50% loss in reactivity to the linear C-terminal reactive antibody of β3 (recognizing 740–769 amino acids of β3) was observed in GT-2 (Figure 5H), when compared to reactivity of the GT-2M platelets (Figure 5G). However, the one subset of platelets (50%) in GT-2 remains, with a native reactivity to the linear C-terminus of β3, as observed by the upfield peak in Figure 5H. These data demonstrate that full-length β3 is present in the platelets of patient GT-2.
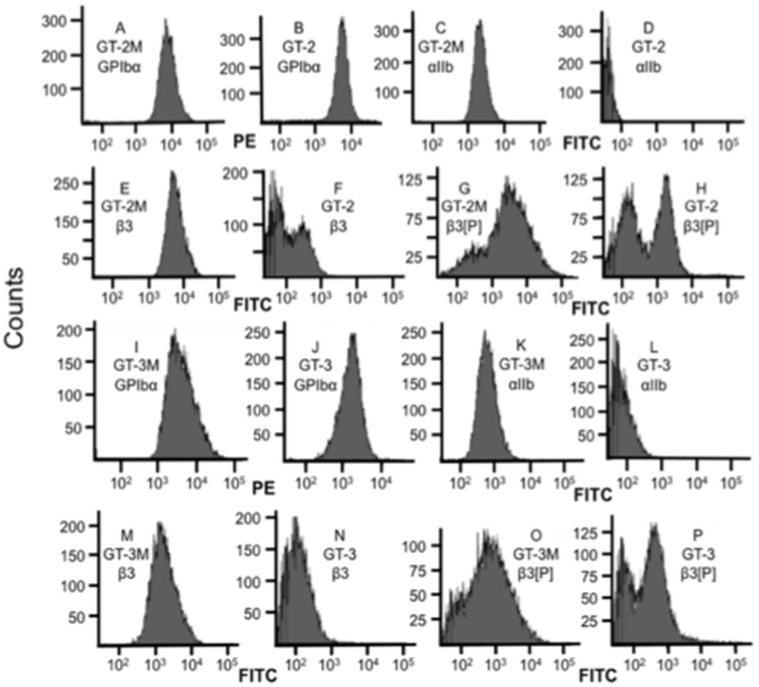
Figure 5. FCA of platelets from PRP of symptomatic GT-2 and GT-3 patient blood, and their heterozygous mothers (GT-2M and GT-3M, respectively).
(A–H) Analysis on the PRP of GT-2 and her heterogyzous mother (GT-2M). Normal expression of GPIbα is seen in (A) GT-2M and (B) GT-2. Integrin βIIb is expressed on platelets of (C) GT-2M, but not (<5%) expressed on the platelets of (D) GT-2. Integrin β3 in the αIIb/β3 complex is expressed on platelets of (E) GT-2M, but not (<5%) expressed on the platelets of (F) GT-2. The amino-terminal peptide [residues 740–769] of β3 (β3[P]) is expressed on the platelets of (G) GT-2M and partly expressed (<10%) on platelets of (H) GT-2 (upfield peak), with another peak (downfield) of weak expression on GT-2. (I, J) Expression of GPIbα is similar in GT-3M and GT-3, whereas (K, L) expression of αIIb is greatly attenuated in GT-3, compared to GT-3M. (M, N) Similarly, integrin β3 in αIIb/β3 displays greatly reduced expression in GT-3 compared to GT-3M. (O, P) The C-terminal peptide region of β3 is recognized in GT-3M, and only partly recognized GT-3 (likely maternal allele), suggesting that a truncation of β3 is present in one allele (likely paternal) in the patient.
Patient GT-3
The platelets of GT-3M and GT-3 essentially showed the same FCA properties (Figure 5I-P) with these antibodies when compared to GT-2M and GT-2, with only qualitative differences between the paired samples.
TEG Analysis of Normal Human Whole Blood Clotting
We considered the values of R, K20, A, MAmax, LY30, and LY60 (Figure 6A, inset) in recalcified plasma of control samples (Figure 6A; Table 2), as basal measures of overall normal hemostasis balance in whole blood. It is seen that the fibrin formed in heparin/reptilase/hFXIIIa (Figure 6C), absent thrombin-induced platelet involvement, has very low viscoelastic strength, as reflected by the MAmax value (Figure 6C; Table 2). Thus, MAF is minimal (Figure 6C; Table 2). Additionally, in the case of a fibrinogen deficiency, activated platelets, alone, do not provide a thrombus that is of measurable viscoelastic strength, with MA values being essentially zero [17]. These data suggest that both functional platelets and fibrinogen are critical to development of a stable viscoelastic thrombus. Regarding fibrinolysis, the activation state (-tPA) or potential activation state (+tPA ± EACA) of the fibrinolytic system, as reflected by LY30 and/or LY60, are employed as diagnostic measures of pathological fibrinolysis in individuals, while also reporting the overall competency of the fibrinolytic system. The values for normal blood are provided in Table 2, as obtained from traces, such as in Figure 6B.
Figure 6. Representative TEG traces of human whole blood.
(A–D) Representative normal control. Samples were collected in citrate-containing plastic tubes for additions of (A) Ca2+, Ca2+/kaolin, Ca2+/sTF/kaolin, or Ca2+/thrombin; (B) Ca2+/sTF/kaolin/tPA or Ca2+/sTF/kaolin/tPA/EACA, compared to the trace with Ca2+/sTF/kaolin/tPA. Samples were collected in heparin-containing plastic tubes and used for platelet stimulation of the MAF generated by (C) reptilase/hFXIIIa with AA or ADP; or (D) COL, RIST, PA-1, or PA-4. The MAmax obtained (from A) with Ca2+/kaolin was used as the 100% reference to compare all agonists for calculation of the degree of agonist stimulation. The inset in Figure 6A displays the parameters that were calculated by the software. (E-I) Similar measurements for (E, F) BSS-2 and (G-I) GT-1 whole blood, collected under the same conditions as normal control blood.
Table 2. Whole blood TEG parameters.
| Human | R (min) | K20 (min) | A (degrees) | MAmax (mm) | LY30 (%) | LY60 (%) |
| Controls a Ca2+ Ca2+/kaolin Ca2+/sTF/kaolin Ca2+/sTF/kaolin/htPA Ca2+/thrombin Reptilase/hFXIIIa | 9.6±0.6 7.3±0.4 0.8±0.1 0.6±0.1 0.8±0.1 1.2±3 | 2.6±0.2 2.1±0.2 1.2±0.2 1.5±0.2 2.8±0.3 nd | 56±3 59±3 75±2 72±2 60±4 nd | 62±2 63±2 64±2 62±3 45±4 5.4±0.8 | 0 0 2.5±1.1 48±7 0 nd | <2<2 5.0±0.7 75±3<2 nd |
| BSS-1 c Ca2+ Ca2+/kaolin Ca2+/sTF/kaolin Ca2+/sTF/kaolin/htPA Ca2+/thrombin Reptilase/hFXIIIa | 10.6; 18 7.7; 14.9 0.8; 1.1 0.3 0.8; 0.8 0.8; 2.2 | 5.8; 4.4 2.3; 3.4 2.5; 2.7 4.8 6.2; 5.4 nd | 34; 41 57; 47 71; 63 71 37; 40 16; 17 | 54; 59 63; 60 62; 57 26 46; 49 8; 4 | 0 0 0 49 0 0 | <2<2<2 74<2 0 |
| BSS-2 c Ca2+ Ca2+/kaolin Ca2+/sTF/kaolin Ca2+/sTF/kaolin/htPACa2+/thrombin Reptilase/hFXIIIa | 11; 5.7 8.6; 5.4 0.7; 0.8 0.2; 0.7 0.8; 0.6 0.9; 0.5 | 2.7; 1.7 2.5; 1.7 1.1; 1.6 1.7; 1.6 3.5; 2.2 nd; nd | 56; 68 58; 54 78; 73 69; 72 53; 65 27; 55 | 71; 76 75; 77 74; 69 37; 37 63; 74 7; 10 | 0; 0 0; 0 0; 0 77; 87 0; 0 nd; nd | <2; <2<2; <2<2; <2 74; 100<2; <2 nd; nd |
| GT-1 c Ca2+ Ca2+/kaolin Ca2+/sTF/kaolin Ca2+/sTF/kaolin/htPACa2+/thrombin Reptilase/hFXIIIa | 9.0; 12 6.9; 8.6 0.8; 1.0 0.3; 0.6 0.5; 1.2 0.6; 0.5 | 3.4; 9.8 2.5; 3.5 1.8; 4.9 2.1 nd; nd nd; nd | 52; 35 39; 23 77; 62 75; 72 55; 35 51; 67 | 25; 21 32; 28 30; 27 23; 15 18; 17 15; 15 | 0; 0 0; 0 0; 0 72; 88 0; 0 nd; nd | 0; 0 0; 0 0; 0 86; 93 0; 0 nd; nd |
| GT-2 Ca2+ Ca2+/kaolin Ca2+/sTF/kaolin Ca2+/sTF/kaolin/htPACa2+/thrombin Reptilase/hFXIIIa | 10 5.1 0.9 0.9 1.1 0.7 | 6 4.6 5.4 5.7 nd nd | 36 51 64 65 32 57 | 30 34 36 25 13 10 | 0 0 0 81 0 nd | 0 0 0 91 0 nd |
| GT-3 Ca2+ Ca2+/kaolin Ca2+/sTF/kaolin Ca2+/sTF/kaolin/htPACa2+/thrombin Reptilase/hFXIIIa | 4.8 3.8 0.9 0.6 0.8 0.3 | 1.8 1.6 1.8 1.6 4.5 nd | 66 67 69 75 46 53 | 67 66 64 27 47 21 | 0.2 0.5 1.1 95 0 nd | nd nd nd nd nd nd |
Normal human controls, N = 10.
[htPA] = 200 ng/ml.
Data are from separate blood draws >4 months apart.
nd, not determined.
These concepts were expanded by analyses of rates, levels, and strength of thrombus formation after additions of other components of the clotting cascade to blood samples. R-values were greatly decreased upon addition of Ca2+/thrombin, and thrombi of high viscoelastic strength were formed (Figure 6A; Table 2). In this case, the MAmax achieved was not optimal since the high thrombin level initially present likely affected the strength of the thrombus, possibly resulting from the alteration of strand assembly dynamics of the fibrin via the more rapid formation of fibrin by exogenous thrombin [18], [19]. Thrombi formed with Ca2+/kaolin provided thromboelastogram-derived values that were only slightly altered from those of Ca2+, alone (Figure 6A; Table 2). This shows that the intrinsic pathway is operating to near maximal capacity in maintenance of basal hemostasis and does not accelerate or stabilize thrombi upon further addition of kaolin. However, addition of Ca2+/sTF/kaolin to blood resulted in much lowered R and K20 values and provided a high MAmax (Figure 6A, Table 2), demonstrating that the TF pathway is likely not highly functional in basal hemostasis and likely provides a rapid response mechanism to injury. Lastly, unstimulated LY30 and LY60 values were very low in control blood (Figure 6B, Table 2), suggesting a minor degree of basal fibrinolysis in healthy individuals. With thrombi rapidly formed by Ca2+/sTF/kaolin, inclusion of htPA (200 ng/ml) to human blood resulted in complete lysis (Figure 6B). Further, addition of EACA to Ca2+/sTF/kaolin/htPA completely inhibited the lysis of whole blood thrombi (Figure 6B).
Platelets Provide Viscoelastic Strength to the Human Thrombus in Normal Plasma
In the case of TEG-based platelet functional analysis of normal human whole blood, the MAA is measured in heparin/reptilase/hFXIIIa blood after addition of a platelet activator (e.g., ADP, AA, RIST, COL, PA-1, PA-4). In these experiments, fibrin is formed by reptilase, which is very similar to that formed by thrombin [20], and crosslinked by exogenous FXIIIa, and any thrombin generated is inhibited by heparin/antithrombin III. Different platelet activators are then added, and the MAmax determined. The MA ratios (with the MAF subtracted), with and without platelet activators, allowed assessment of the effectiveness of the individual platelet agonists to stimulate the assembly of strong whole blood thrombi. The data obtained for the human controls (Figure 6C, D; Table 3) show that the agonists, ADP and AA (Figure 6C), as well as the PAR-1 and PAR-4 agonist peptides, PA-1, and PA-4, respectively (Figure 6D), result in thrombi of strong viscoelasticity. However, RIST and COL do not allow thrombi of high strength to be formed (Figure 6D) at concentrations of each that effectively aggregate platelets in whole blood (Figure 7C,E, Table 4), when aggregation is measured independently of thrombus formation.
Table 3. Platelet mapping by TEG.
| Human | ADPc (%) 2 µMd | AAc (%) 1 mMd | RISTc (%) 0.3 mg/mld | COLc (%) 3.2 µg/mld | PA-1c (%) 31 µMd | PA-4c (%) 663 µMd |
| Controlsa | 78±4 | 99±2 | 4±2 | 5±2 | 84±6 | 73±6 |
| BSS-1b | 22; 36 | 62; 66 | −6.4; 0 | −4.4; 1 | 48 | 32 |
| BSS-2b | 20; 5 | 92; 90 | −1.3; 0 | 0.5; 0 | 84; 60 | 64; 71 |
| GT-1b | 22; 0 | 26; 0 | 7; 0 | 0; 3 | 14; 0 | 0; 0 |
| GT-2 | 0 | 37 | 0 | 0 | 20 | 0 |
| GT-3 | 68 | 0 | 0 | 21 | 69 | 76 |
Normal human controls, N = 10.
Data are from separate blood draws >3 months apart.
The stimulation by each of these agents with respect to the MA of Ca2+/kaolin ( = 100%).
Final concentration in the reaction vessel.
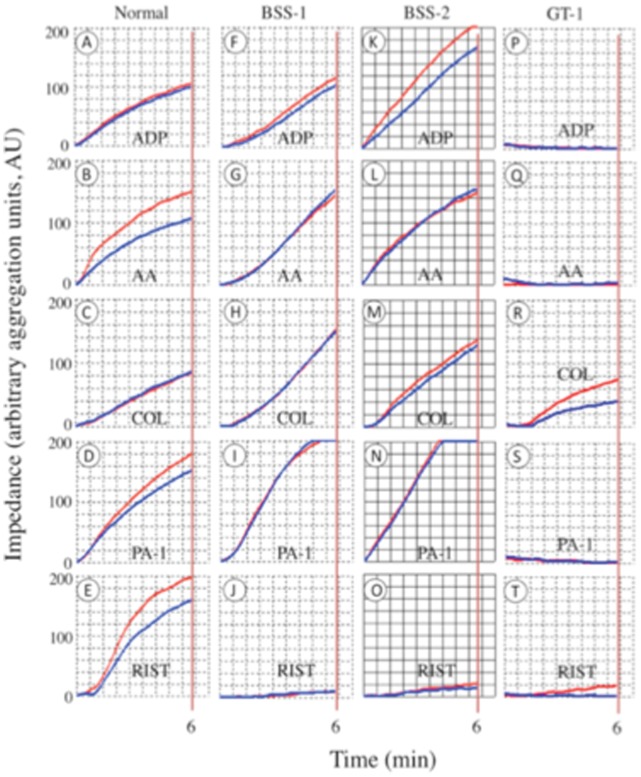
Figure 7. Human whole blood platelet aggregation measurements.
The increase in impedance of platelets aggregated on multiplate sensors and transformed by software into arbitrary aggregation units is plotted against time. Curves are generated for 6 min and the areas under the curve, from 0–6 min, are calculated by the software as a measure of platelet aggregation. Two independent runs were generated for each agonist (blue and red curves in each panel) and the mean of the areas was employed. The agonists are listed on each panel. Data were collected on normal human whole blood, and on BSS-1, BSS-2, and GT-1 blood.
Table 4. Impedance-based platelet aggregometry (AU) of the study groupsa.
| Humanb | ADP 6.5 µMd | AA 0.5 mMd | RIST 0.88 mg/mld | COL 3.2 µg/mld | PAR-1 32 µMd | PAR-4 663 µMd |
| Controlsb | 125±10 | 143±10 | 146±8 | 136±10 | 195±47 | 213±8 |
| BSS-1c | 109; 93; 92 | 147; 148; 121 | 10; 0; 8 | 150; 149; 84 | 219; 182; 165 | 161; 153 |
| BSS-2c | 187; 146; 168 | 150; 137; 150 | 18; 37; 37 | 134; 60; 124 | 272; 199 | 162; 171 |
| GT-1c | 0; 0 | 0; 0 | 10; 0 | 57; 85 | 0; 5 | 0 |
| GT-2 | 0 | 105 | 74 | 163 | 5 | 5 |
| GT-3 | 29 | 43 | 95 | 69 | 42 | 39 |
Two analyses were performed for each agonist in all cases. Data are reported as the mean value of the areas under the respective curves.
Normal human controls, N = 10.
Data are from separate blood >4 months apart.
Final concentration in the reaction vessel.
TEG and Platelet Aggregometry Analyses of BSS and GT Whole Blood Clotting
There are differences between whole blood thrombus stability in normal and BSS-derived whole blood, but some differences between the two BSS patients are also seen (Table 2), probably due to the disparate nature of the deficiencies in each case. Upon recalcification of citrated blood, the R and K20 are slightly prolonged in BSS-1 samples, and less so in BSS-2 blood (Figure 6E; Table 2). This indicates a defective level of functional thrombin in these patients, undoubtedly due to the thrombocytopenia and the large platelet surface areas. Both of these factors would attenuate the levels and availability of the prothrombinase complex on platelets. This hypothesis is fortified by the large decrease in R after addition of Ca2+/thrombin (Figure 6E, Table 2). K20 is not affected in this situation because new thrombin is not formed at a more rapid rate when Ca2+/thrombin is added. However, the R and K20 of BSS whole blood (BSS-2 is shown as the example) are greatly decreased after addition of Ca2+/sTF/kaolin (Figure 6E, Table 2). As with normal whole blood, addition of Ca2+/kaolin did not remarkably alter these TEG parameters, again showing that the intrinsic system functions to maintain basal hemostasis in the individual. Thus, despite low platelet counts and large platelets, strong viscoelastic thrombi are formed with BSS platelets in whole blood. As with normal controls, no unstimulated fibrinolysis occurred in BSS blood (Figure 6F, Table 2), but addition of htPA (200 ng/ml) to BSS blood resulted in complete lysis, a process also nearly completely inhibited by EACA (Figure 6F).
Platelet functionality in whole blood thrombus formation, as analyzed by TEG, is remarkable in that ADP stimulation of BSS platelets is defective with regard to generating strong viscoelastic thrombi with fibrin (Figure 6E, Table 3), compared to control blood, despite the finding that ADP leads to near normal impedance-based aggregation of BSS platelets (Figure 7A, F, K; Table 4). On the other hand, AA stimulation of the MAF is similar to that of normal blood (Figure 6E; Table 3), as is the impedance-based aggregation of these platelets (Figure 7B, G, L; Table 4). As expected, there was severe attenuation of platelet aggregation with RIST in the BSS patients compared to normal blood (Figure 7E,J,O; Table 4), but other platelet activators tested (AA, COL, PA-1, and PA-4; example provided for PA-1 in Figure D, I, N) appeared quantitatively similar to the blood of normal controls (Table 4).
Regarding GT whole blood clotting, values of R, K20, and A in recalcified blood were similar to WT control blood (Figure 6G, H; Table 2). The response of these values to thrombus formation with Ca2+/kaolin, Ca2+/thrombin, and Ca2+/sTF/kaolin were also similar to WT controls. This indicates that platelets were activated by thrombin in GT blood and could assemble into a thrombus. However, as reflected by the substantially lower MAmax value (Figure 6G, Table 2), platelet/fibrin interactions were affected and assemble into a substantially weaker thrombus, whether the platelets were activated by thrombin (Figure 6G, Table 2); ADP, AA (Figure 6H); or ristocetin, collagen, PA-1, or PA-4 (not shown). In separate aggregation studies, of all the platelet activators examined, only collagen weakly stimulated aggregation, likely via binding to a separate receptor on platelets. Ristocetin did not function in this manner in aggregation assays, despite the functional presence of GP1b (Figure 7, Table 4).
The thrombi formed in the GT whole blood did not show spontaneous clot lysis, but did display very strong lysis with htPA (Figure 6I, Table 2), in a process that was effectively inhibited by EACA. Perhaps the more rapid lysis of the clots in GT blood displayed at 30 min (Table 2) is due to the weakened clots formed in this system.
Discussion and Conclusions
While it is difficult to recapitulate in vivo hemostasis in ex vivo models, nonetheless much has been learned that is clinically applicable over decades of efforts in this regard. Studies of hemostasis mechanisms in plasma have focused on the role of soluble factors in fibrin formation. However, it is relevant to expand hemostasis mechanistic studies to whole blood to include the role of platelets in clinical consideration of the hemostasis status of patients. A manner of understanding the features of platelets needed to form stable thrombi is to study whole blood that contains platelets with known deficiencies. BSS patients afford one such opportunity. In this case, the contributions of GP1b in whole blood thrombus formation can be studied in the absence of high shear. However, the numbers of these patients are very limited (1∶1,000,000), and only ∼100 cases have been confirmed in the literature. Fortunately, we were able to access two BSS patients for this work. Deficiencies in human GP1b, both genetic and acquired, are found in BSS [21], cardiopulmonary bypass (CPB) [22] surgery, and surgical trauma [23], and in targeted transgenic mice [24], and lead to bleeding diatheses, presumably due to defects in the binding of platelets to the subendothelium. Whether such a deficiency would alter rates of thrombus formation and ultimate strength of the thrombus in whole blood with exogenous soluble subendothelium components, was not known, and is one contribution from this work.
Severe attenuation, of human GP1b expression, as in the case of BSS, leads to macrothrombocytopenia, but this has minimal effects on overall plasma-based coagulation markers. In humans, TEG-based whole blood coagulation parameters are also not substantially affected whether thrombin or a direct pharmacological agonist of downstream PAR-1 activation is employed as the overall activator of platelets. However, when thrombin is blocked and other platelet activators are used to induce thrombus assembly in the presence of fibrin, the results are somewhat surprising. In normal human plasma, RIST and COL aggregate and probably activate platelets, but stable viscoelastic thrombi are minimally formed. On the other hand, ADP and AA both aggregate control platelets and allow normal thrombus assembly. In human BSS blood, AA functions normally, but the effects of ADP on thrombus assembly and/or stability are greatly attenuated compared to normal controls. The fact that direct activation of PAR-1 by PA-1 reverses the weakened stimulation by ADP of the MAF in BSS whole blood links ADP stimulation of thrombi of high viscoelastic strength to PAR-1 activation.
Confirmation of the importance of the fibrin(ogen)-binding integrin, αIIb/β3, in assembling a thrombus has been obtained by examination of the blood of human GT patients. GT-1 is shown as the example, an individual who possessed a rare double heterozygous GP1b mutation that inactivated this receptor. This GT blood did not show effective platelet aggregation with a series of platelet activators, except weakly in the case of collagen, and did not assemble with fibrin into a strong viscoelastic clot. Thus, thromboelastograms obtained on patients with deficiencies or blocks of αIIb/β3, would manifest in very low MAmax values. Qualitatively similar results are seen with 2 other GT patients with different mutations. Thus, while general principles can be established with an array of BSS and GT patients, given the array of possible mutations that lead to BSS and GT, it is suggested that each patient is examined individually.
Overall, the results demonstrate that human platelet activation, as measured by the ability of platelets to aggregate, does not necessarily translate to the assembly of a thrombus of high viscoelastic strength, and further suggests that the platelet receptors engaged for activation are mechanistically related to the nature of the platelet-fibrin assembly that is measured by clot strength. The contribution of platelet defects, and specifically that of attenuation of GP1b expression [25], to whole blood hemostasis has been a long-standing consideration in on-pump CPB surgery, where TEG analysis on whole blood is employed to predict post-surgical bleeding [26], [27], and off-pump coronary artery bypass surgery led to lower platelet activation defects than on-pump surgery [28].
These factors may also be applicable to the coagulopathy of traumatic brain injury [29]–[34], wherein ADP stimulation of platelets to assemble into a thrombus is diminished, as is expression of platelet surface GP1b [23], but AA stimulation of thrombus formation is affected to a lesser degree [35]. As with the high mechanical shear forces to which platelets are exposed in CPB, high tissue shear forces are also present in certain types of severe TBI, e.g., inertial injury, and can result in excess vWF-dependent activation and possible shedding of the ectodomain of GP1b [36], [37]. Thus, platelets might be generated in severe TBI that are GP1bα deficient, as in BSS. Therefore, BSS platelets are not only critical to understand the mechanistic role of GP1bα in platelet aggregation and thrombus strength, but may also model some of the platelet dysfunctions in the hypocoagulopathy of TBI and CPB, and other maladies.
The results of this study segregate platelet activation, reflected by platelet aggregation, from that represented by assembly into thrombi of high viscoelastic strength, and suggest that the nature of the thrombus formed depends on the receptors and signaling mechanisms that are engaged. ADP stimulation of thrombus formation is a particularly sensitive indicator of the nonsingularity of platelet activation. These findings have implications in treatment of platelet-based coagulopathies, e.g., CPB and TBI, and suggest that platelet counts and platelet aggregation tests, alone, may not sufficiently correlate with effective thrombus formation, and patients, who appear normal in these regards, may still benefit from platelet replacement therapy. More specifically, in the case of coagulopathic patients, thromboelastographic analysis of whole blood thrombus formation and stability is an effective guide for goal-directed administration of blood products [35].
Acknowledgments
We thank the staff of the Freimann Life Sciences Facility for the breeding and husbandry of mice and the phlebotomy team at Memorial Hospital of South Bend for individual blood collection. The cooperation of the Aurora Clinic in our obtaining some of the blood samples is also gratefully acknowledged. We also thank Dr. Robert M. Montgomery, Blood Center of Wisconsin, Dr. Amy D. Shapiro, Indiana Hemophilia & Thrombosis Center, and Dr. Mortimer Poncz, Children's Hospital of Pennsylvania, Carol A. Diamond, University of Wisconsin, and David L. Green and Michael Nardi, New York University, for identifying some of the BSS and GT patients. The TEG equipment was donated by Haemonetics, Inc., and some of the reagent expenses were defrayed by this same company. Similarly, the Multiplate apparatus and some reagents were provided by Verum Diagnostica.
Funding Statement
This work was supported by a grant from Memorial Hospital of South Bend. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Ruggeri ZM (1997) Mechanisms initiating platelet thrombus formation. Thromb Haemost 78: 611–616. [PubMed] [Google Scholar]
- 2. Sugiyama T, Okuma M, Ushikubi F, Sensaki S, Kanaji K, et al. (1987) A novel platelet aggregating factor found in a patient with defective collagen-induced platelet aggregation and autoimmune thrombocytopenia. Blood 69: 1712–1720. [PubMed] [Google Scholar]
- 3. Ezumi Y, Uchiyama T, Takayama H (2000) Molecular cloning, genomic structure, chromosomal localization, and alternative splice forms of the platelet collagen receptor glycoprotein VI. Biochem Biophys Res Commun 277: 27–36. [DOI] [PubMed] [Google Scholar]
- 4. Nuyttens BP, Thijs T, Deckmyn H, Broos K (2011) Platelet adhesion to collagen. Thromb Res 127: S26–S29. [DOI] [PubMed] [Google Scholar]
- 5. Jackson SP, Nesbitt WS, Kulkarni S (2003) Signaling events underlying thrombus formation. J Thromb Haemost 1: 1602–1612. [DOI] [PubMed] [Google Scholar]
- 6. Dorsam RT, Kunapuli SP (2004) Central role of the P2Y12 receptor in platelet activation. J Clin Invest 113: 340–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brass LF, Manning DR, Cichowski K, Abrams CS (1997) Signaling through G proteins in platelets: to the integrins and beyond. Thromb Haemost 78: 581–589. [PubMed] [Google Scholar]
- 8. Lopez JA, Andrews RK, Afshar-Kharghan V, Berndt MC (1998) Bernard-Soulier syndrome. Blood 91: 4397–4418. [PubMed] [Google Scholar]
- 9. Lopez JA, Ludwig EH, McCarthy BJ (1992) Polymorphism of human glycoprotein Ib alpha results from a variable number of tandem repeats of a 13-amino acid sequence in the mucin-like macroglycopeptide region. Structure/function implications. J Biol Chem 267: 10055–10061. [PubMed] [Google Scholar]
- 10. Kaski S, Kekomaki R, Partanen J (1996) Systematic screening for genetic polymorphism in human platelet glycoprotein Ibalpha. Immunogenetics 44: 170–176. [DOI] [PubMed] [Google Scholar]
- 11. Kuijpers RW, Faber NM, Cuypers HT, Ouwehand WH, von dem Borne AE (1992) NH2-terminal globular domain of human platelet glycoprotein Ib alpha has a methionine 145/threonine145 amino acid polymorphism, which is associated with the HPA-2 (Ko) alloantigens. J Clin Invest 89: 381–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Afshar-Kharghan V, Lopez JA (1997) Bernard-Soulier syndrome caused by a dinucleotide deletion and reading frameshift in the region encoding the glycoprotein Ib alpha transmembrane domain. Blood 90: 2634–2643. [PubMed] [Google Scholar]
- 13. Kenny D, Newman PJ, Morateck PA, Montgomery RR (1997) A dinucleotide deletion results in defective membrane anchoring and circulating soluble glycoprotein Ib alpha in a novel form of Bernard-Soulier syndrome. Blood 90: 2626–2633. [PubMed] [Google Scholar]
- 14. Kenny D, Jonsson OG, Morateck PA, Montgomery RR (1998) Naturally occurring mutations in glycoprotein Iba that result in defective ligand binding and synthesis of a truncated protein. Blood 92: 175–183. [PubMed] [Google Scholar]
- 15. Burset M, Seledtsov IA, Solovyev VV (2000) Analysis of canonical and non-canonical splice sites in mammalian genomes. Nucl Acids Res 28: 4364–4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Basani RB, Vilaire G, Shattil SJ, Kolodziej MA, Bennett JS, et al. (1996) Glanzmann thrombasthenia due to a two amino acid deletion in the fourth calcium-binding domain of alpha IIb: demonstration of the importance of calcium-binding domains in the conformation of alpha IIb beta 3. Blood 88: 167–173. [PubMed] [Google Scholar]
- 17. Castellino FJ, Donahue DL, Navari RM, Ploplis VA, Walsh M (2011) An accompanying genetic severe deficiency of tissue factor protects mice with a protein C deficiency from lethal endotoxemia. Blood 117: 283–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wolberg AS, Allen GA, Monroe DM, Hedner U, Roberts HR, et al. (2005) High dose factor VIIa improves clot structure and stability in a model of haemophilia B. Br J Haematol. 1321: 645–655. [DOI] [PubMed] [Google Scholar]
- 19. Wolberg AS, Monroe DM, Roberts HR, Hoffman M (2003) Elevated prothrombin results in clots with an altered fiber structure: a possible mechanism of the increased thrombotic risk. Blood 101: 3008–3013. [DOI] [PubMed] [Google Scholar]
- 20. Carr ME, Gabriel DA, McDonagh J (1986) Influence of Ca2+ on the structure of reptilase-derived and thrombin-derived fibrin gels. Biochem J 239: 513–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jenkins CS, Phillips DR, Clemetson KJ, Meyer D, Larrieu MJ, et al. (1976) Platelet membrane glycoproteins implicated in ristocetin-induced aggregation. Studies of the proteins on platelets from patients with Bernard-Soulier syndrome and von Willebrand's disease. J Clin Invest 57: 112–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rinder CS, Gaal D, Student LA, Smith BR (1994) Platelet-leukocyte activation and modulation of adhesion receptors in pediatric patients with congenital heart disease undergoing cardiopulmonary bypass. J Thorac Cardiovasc Surg 107: 280–288. [PubMed] [Google Scholar]
- 23. Bunescu A, Widman J, Lenkei R, Menyes P, Levin K, et al. (2002) Increases in circulating levels of monocyte-platelet and neutrophil-platelet complexes following hip arthroplasty. Clin Sci 102: 279–286. [PubMed] [Google Scholar]
- 24. Ware J, Russell S, Ruggeri ZM (2000) Generation and rescue of a murine model of platelet dysfunction: the Bernard-Soulier syndrome. Proc Natl Acad Sci USA 97: 2803–2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Maquelin KN, Berckmans RJ, Nieuwland R, Schaap MCL, ten Have K, et al. (1998) Disappearance of glycoprotein Ib from the platelet surface in pericardial blood during cardiopulmonary bypass J Thorac Cardiovasc Surg. 115: 1160–1165. [DOI] [PubMed] [Google Scholar]
- 26. Cammerer U, Dietrich W, Rampf T, Braun SL, Richter JA (2003) The predictive value of modified computerized thromboelastography and platelet function analysis for postoperative blood loss in routine cardiac surgery. Anesth Analg 96: 51–57. [DOI] [PubMed] [Google Scholar]
- 27. Preisman S, Kogan A, Itzkovsky K, Leikin G, Raanani E (2010) Modified thromboelastography evaluation of platelet dysfunction in patients undergoing coronary artery surgery. Eur J Cardiothorac Surg 37: 1367–1374. [DOI] [PubMed] [Google Scholar]
- 28. Ballotta A, Saleh HZ, El Baghdady HW, Gomaa M, Belloli F, et al. (2007) Comparison of early platelet activation in patients undergoing on-pump versus off-pump coronary artery bypass surgery. J Thorac Cardiovasc Surg 134: 132–138. [DOI] [PubMed] [Google Scholar]
- 29. Basani RB, Richberg M, Poncz M (1999) Molecular biological identification and characterization of inherited platelet receptor disorders. Methods Mol Med 31: 313–336. [DOI] [PubMed] [Google Scholar]
- 30. Kashuk JL, Moore EE, Sawyer M, Le T, Johnson J, et al. (2010) Postinjury coagulopathy management: goal directed resuscitation via POC thrombelastography. Ann Surg 251: 604–614. [DOI] [PubMed] [Google Scholar]
- 31.Davis PK, Musunuru H, Walsh M, Cassady R, Yount R, et al. (2012) Platelet dysfunction is an early marker for traumatic brain injury-induced coagulopathy. Neurocrit Care 2012 Jul 31 [Epub ahead of print]. [DOI] [PubMed]
- 32. Holcomb JB, Minei KM, Scerbo ML, Radwan ZA, Wade CE, et al. (2012) Admission rapid thrombelastography can replace conventional coagulation tests in the emergency department: experience with 1974 consecutive trauma patients. Ann Surg 256: 476–486. [DOI] [PubMed] [Google Scholar]
- 33. Johansson PI (2012) Coagulation monitoring of the bleeding traumatized patient. Current opinion in anaesthesiology 25: 235–241. [DOI] [PubMed] [Google Scholar]
- 34. Wohlauer MV, Moore EE, Thomas S, Sauaia A, Evans E, et al. (2012) Early platelet dysfunction: an unrecognized role in the acute coagulopathy of trauma. J Am Coll Surg 214: 739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Walsh M, Thomas SG, Howard JC, Evans E, Guyer K, et al. (2011) Blood component therapy in trauma guided with the utilization of the perfusionist and thromboelastography. J Extra Corp Tech 43: 162–167. [PMC free article] [PubMed] [Google Scholar]
- 36. Ikeda Y, Handa M, Kawano K, Kamata T, Murata M, et al. (1991) The role of von Willebrand factor and fibrinogen in platelet aggregation under varying shear stress. J Clin Invest 87: 1234–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cheng H, Yan R, Li S, Yuan Y, Liu J, et al. (2009) Shear-induced interaction of platelets with von Willebrand factor results in glycoprotein Ibalpha shedding. Am J Physiol 297: H2128–H2135. [DOI] [PubMed] [Google Scholar]