Abstract
Purpose
This is a descriptive analysis, of victims of Turkey’s October 23, 2011 and November 21, 2011 Van earthquakes. The goal of this study is investigated the injury profile of the both earthquakes in relation to musculoskeletal trauma.
Methods
We retrospectively reviewed medical records of 3,965 patients admitted to in seven hospitals. A large share of these injuries were soft tissue injuries, followed by fractures, crush injuries, crush syndromes, nerve injuries, vascular injuries, compartment syndrome and joint dislocations. A total of 73 crush injuries were diagnosed and 31 of them were developed compartment syndrome.
Results
The patients with closed undisplaced fractures were treated with casting braces. For closed unstable fractures with good skin and soft-tissue conditions, open reduction and internal fixation was performed. All patients with open fracture had an external fixator applied after adequate debridement. Thirty one of 40 patients with compartment syndrome were treated by fasciotomy. For twelve of them, amputation was necessary. The most common procedure performed was debridement, followed by open reduction and internal fixation and closed reduction-casting, respectively.
Conclusions
The results of this study may provide the basis for future development of strategy to optimise attempts at rescue and plan treatment of survivors with musculoskeletal injuries after earthquakes.
Introduction
Earthquakes have killed and injured millions of people in the past. Adequate and well-timed management to reduce mortality and morbidity of the injured in earthquakes is of concern to rescuers and medical-care professionals [1, 2]. In earthquakes, treatment is often delayed by the destruction of roads, inadequate equipment and damage to hospitals [3]. Whilst surgical and anaesthetic care is influenced by infrastructural constraints, the type of surgical procedures, availability of medication and equipment, and the experience of personnel [4, 5]. The earthquake-related injuries are often caused by falling objects or chronic tissue compression. The role of orthopaedic surgeons is important in earthquakes [5].
On Sunday, 23 October 2011 at 13:41 local time, an earthquake measuring 7.2 on the Richter scale struck the densely populated region of eastern Turkey near the city of Van. Utilities such as electricity, water, gas and telecommunication were interrupted. During the very intense aftershock activity of the Van-centre earthquake, another earthquake occurred at 10 km south of Van, near Edremit province on Wednesday, 09 November 2011 at 21:23 local time. The magnitude of this earthquake was calculated as 5.7 on the Richter scale. According to Disasters and Emergency Situations Directorate (AFAD) of Turkey on 21 November, 644 people were killed in the two earthquakes, in total.
This is a descriptive analysis of the victims of Turkey’s October 23, 2011 and November 9, 2011 Van earthquakes. The goal of this study is to investigate the injury profile of both earthquakes in relation to musculoskeletal trauma.
Materials and methods
The local institutional ethical review board approved the study. This multicentre study retrospectively investigated the clinical records of patients admitted to the Van Research and Education Hospital (Van city), Van Ipekyolu State Hospital (Van city), Bitlis State Hospital (Bitlis city), Mus State Hospital (Mus city), Dicle University Medical School Hospital (Diyarbakir city), Harran University Medical School Hospital (Sanliurfa city) and Gaziantep University Medical School Hospital (Gaziantep city) with earthquake-related musculoskeletal injuries during the seven days that followed the 23 October and 9 November 2011 Van earthquakes.
Five thousand one hundred and seventy three patients with musculoskeletal trauma were treated in the hospitals, 3,965 of them had adequate records for inclusion in our study. We analysed 1,471 patients after the 23 October Van earthquakes and 2,494 patients after the 9 November 2011 incident. Patients were entered in this study according to the following criteria: [1] the aetiology of the injury was associated with the 23 October and 9 November 2011 Van earthquakes; [2] musculoskeletal injuries (soft tissue injury, fracture, dislocation, nerve injury, vascular injury, crush injury, crush syndrome and compartment syndrome) were evaluated by the emergency department. Patients were excluded from the study according to the following criteria: [1] patients who jumped or accidentally fell from heights due to the earthquake; [2] patients who were injured by earthquake-related motor vehicle injury, burn injuries or other aetiologies; and [3] patients who received treatment for to non-musculoskeletal injuries.
We conducted an injury profile of all patients with musculoskeletal trauma, and recorded hospital distribution of the patients, admission time of the patients, age and gender, profile of injury, infections, and treatments. The patients were classified according to their primary injuries.
This study was approved by the Ethical Committee of the Yuzuncu Yil University Medical School Hospital of Van city. No informed consent was necessary as this study used existing data.
Statistical analysis
The patients’ age, sex and the cause of injury for the earthquake victims were recorded. The numbers of patients with soft tissue injuries, fractures, crush injury, crush syndrome, and compartment syndrome were enumerated. The continuous variables were expressed as means ± standard deviation, and the categorical variables were expressed as numbers and percentages.
Results
Hospital distribution of the patients
One thousand six hundred and thirty nine earthquake victims admitted to Van Research and Education Hospital, 2001 earthquake victims admitted to Van Ipekyolu State Hospital, 237 earthquake victims admitted to Bitlis State Hospital, 30 earthquake victims admitted to Mus State Hospital, 55 earthquake victims admitted to Dicle University Medical School Hospital, two earthquake victims admitted to Sutcu Imam University Medical School Hospital and one earthquake victim admitted to Gaziantep University Medical School Hospital formed the hospital distribution of the patients. Two thousand seven hundred and fifty nine patients (69.6 %) were admitted to hospital over the first three days after the Van earthquakes (Fig. 1).
Fig. 1.
The earthquake victims were admitted to in seven hospitals. Van Research and Education Hospital (Van city), Van Ipekyolu State Hospital (Van city), Bitlis State Hospital (Bitlis city), Mus State Hospital (Mus city), Dicle University Medical School Hospital (Diyarbakir city), Harran University Medical School Hospital (Sanliurfa city) and Gaziantep University Medical School Hospital (Gaziantep city)
Admission time of the patients and follow up
The average length of hospital stay of the earthquake victims after admission to hospitals was 4.1 ± 2.8 days for all of the patients, 3.1 ± 2.7 for those with soft tissue injury, 5.2 ± 2.6 for those with fractures.
The mean follow up period in the hospital was 13 days (Range: 2–24 days). Definitive operations were performed after 52.3 hours on average (range: 1–157 hours) after admission.
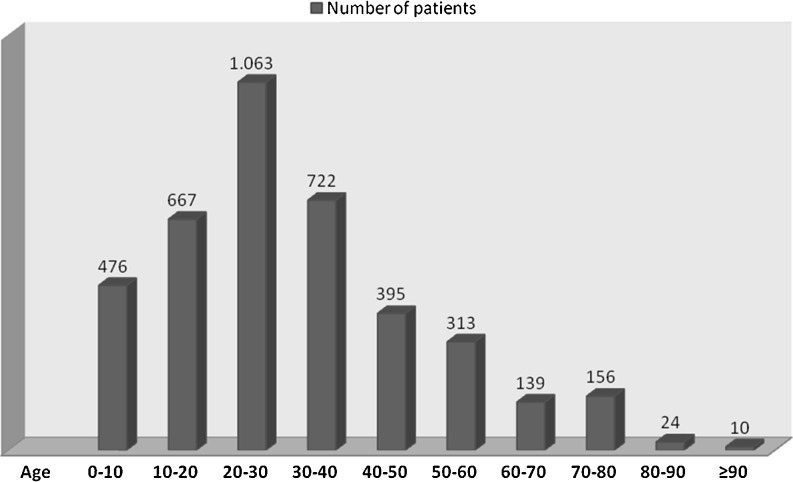
Age and gender distribution
Two thousand four hundred and seventy eight patients (62.5 %) were male and 1,487 (37.5 %) were female. Patients between 20 and 30 years of age accounted for the majority (1,063, 26.8 %) of the patients, followed by those between 30 and 40 years of age (722, 18.2 %). The mean age was 23.5 (range 0–94). The age distribution of victims is shown in Fig. 2.
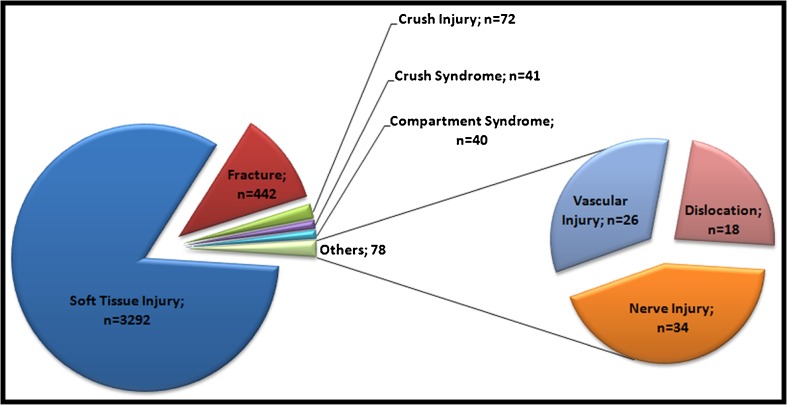
Fig. 3.
Profile of musculoskeletal injuries in the earthquake of Van, Turkey
Profile of Injuries
A large share of these injuries were soft tissue injuries (3,292 victims, 83.0 %), followed by fractures (442 victims, 11.1 %), crush injuries (72 victims, 1.8 %), crush syndromes (41 victims, 1.0 %), nerve injuries (34 victims, 0.9 %), vascular injuries (26 victims, 0.7 %), compartment syndrome (40 victims, 1.0 %) and joint dislocations (18 victims, 0.5 %), respectively (Fig. 3). A total of 73 crush injuries were diagnosed and 31 of them developed compartment syndrome.
Fig. 2.
Age distribution of patients admitted to the hospitals
Soft tissue injury and fracture were the most common types of injuries. The soft tissue injuries were mostly caused by contusion and lacerations, which accounted for more than 70 % of the soft tissue injuries. Twenty four patients had major soft tissue loss.
Fractures were mostly frequently found in the lower limbs (46.4 %), including tibial-fibular fractures in 100 cases and femoral fractures in 36 cases, followed by upper limb fractures (31.2 %), including radius-ulna fractures in 70 cases and humeral fractures in 23 cases, followed by spine fractures (8.6 %). Thirty seven patients had open fractures, 56 multiple fractures and 19 comminuted fractures. Table 1 shows the distribution of fractures based on anatomical site.
Table 1.
Distribution of fractures based on anatomical site
| Fracture location | Frequency | Percent (%) |
|---|---|---|
| Upper extremity fracture | 138 | 31.2 |
| Scapula and clavicle | 22 | 5.0 |
| Humerus | 23 | 5.2 |
| Radius and ulna | 70 | 15.8 |
| Carpus, metacarpus and phalangeal | 23 | 5.2 |
| Pelvic fracture | 54 | 12.2 |
| Acetabulum fracture | 7 | 1,6 |
| Lower extremity fracture | 205 | 46.4 |
| Femur | 36 | 8.2 |
| Patella | 5 | 1.1 |
| Tibia and fibula | 100 | 22.6 |
| Tarsal, metatarsal and phalangeal | 64 | 14.5 |
| Vertabra fracture | 38 | 8.6 |
| Total | 442 | 100 |
The most common peripheral nerve injury was to the sciatic nerve (12 cases). The sciatic nevre injuries were associated with lower limb fractures or dislocations. Eight patients had spinal injuries, which were all associated with vertebral fractures. Radial nerve injury was seen in four cases. All of the radial nerve injuries were associated with fractures. Other peripheral nerve injuries (axillary, ulnar, femoral, tibial and peroneal) were seen in 11 cases.
Treatment
After admission, all of the patients were uniformly given injections of tetanus immunoglobulin and routine systemic physical examination was done. Patients with closed fractures who underwent operative treatment received a single preoperative prophylactic dose of intravenous cefazolin 2 g. All patients with open fractures were irrigated with sterile saline to remove any gross superficial contaminants and stabilised with plaster splints. Intravenous antibiotics were started. The antibiotic regimen consisted of cefazolin (1 g every eight hours); gentamicin and metronidazole were added for severe soil contamination. Wounds were fully explored and all devitalised tissues excised. The wounds were irrigated with pulse lavage. Antibiotics were continued for three days after surgery. Dressings were applied after debridement.
The treatment of earthquake survivors with musculoskeletal trauma included medical treatment, debridement, fasciotomy, closed reduction, open reduction and amputation. The operations were performed under general anaesthesia in all patients. The method of fracture fixation was divided into internal and external fixation. The external fixation approach also included casting braces. The presence of multiple fractures and comminution of fractures were identified.
The patients with closed undisplaced fractures had a casting brace applied. For closed unstable fractures with good skin and soft-tissue condition, open reduction and internal fixation was performed. All patients with open fractures had an external fixator applied after adequate debridement. Thirty one of 40 patients with compartment syndrome were treated by fasciotomy. Twelve required amputation. The most common procedure performed was debridement (n = 166), followed by open reduction and internal fixation (n = 117) and closed reduction-casting (n = ,91) respectively. Table 2 shows the number of procedures performed for patients.
Table 2.
The table shows the number of procedures performed for patients
| Treatment types | Number of patients | Percent |
|---|---|---|
| Debridement | 166 | 33.1 |
| Closed reduction and casting | 91 | 18.2 |
| Closed reduction and internal fixation | 47 | 9.4 |
| External fixation | 37 | 7.4 |
| Open reduction and internal fixation | 117 | 23.4 |
| Fasciotomy | 31 | 6.2 |
| Amputation | 12 | 2.4 |
| Total | 501 | 100 |
Discussion
A major earthquake frequently causes numerous victims with a wide variety injuries [6–9]. Most orthopaedic injuries during earthquakes involve the extremities [6, 7]. The injuries typically seen in earthquakes are often caused by falling masonry etc. leading to chronic tissue compression.
In our study, 55.6 % of victims were between 0 and 30 years. This differs greatly from the findings of other studies on the victims of other earthquakes [8, 9]. Probably, young age of earthquake survivors is associated to some factors, such as the high percentage of young population in Van, and the high intensity of the disaster leaving elderly unable to escape from the scene immediately and thus dying before rescue.
Mulvey et al. [6] reported that the most common types of injury associated with the 2005 Kashmir earthquake were soft tissue injuries and fractures. In our study also the most common types of injury were soft tissue injury and fracture. The 23 October Van earthquake occured in the afternoon and the 9 November Van earthquake occurred in the early evening. Most earthquake victims were injured while escaping falling debris. When the earthquake occurs in the early morning and most victims are asleep, proximal bones are more commonly involved [10]. The Van earthquakes occurred in the afternoon and evening, so distal bones were commonly involved. The number of lower limb fractures was greater than upper limb extremity fractures as seen in 2009 Western Sumatra earthquake [11]. Limb extremity fractures were also seen most commonly in our study. To reduce severe injuries in areas at high risk of earthquake, self-rescue education programs should be performed.
In the early period following a catastrophe, the most urgently needed orthopaedic protocols are external fixation, amputation, and debridement; and often there is no facility or equipment to perform more complex procedures [12]. Amputation is a frequently performed procedure during earthquakes and mass casualties related to industrial accidents and military conflicts where large civilian populations are subjected to severe musculoskeletal trauma [13]. The decision to perform an amputation is always difficult [14–16]. We observed in our study; the most frequently performed operation was debridement (33.1 %). Amputations were required in 12 patients. A post-amputation rehabilitation program is often considered to be more important than the amputation (the surgical act) itself and its cornerstone is the fitting of a prosthetic device [17]. In 2005 earthquake in Pakistan, they managed 112 amputees and placed them in a rehabilitation program [18]. We also established a rehabilitation program for our patients who were amputees.
The most common causes of amputation were serious crush injuries and compartment syndrome. They had lead to vascular damage and eventual infection, a condition that could have been preventable by early fasciotomy operation. In addition, the initiation of early therapy to prevent acute tubular necrosis due to crush syndrome is well shown by the relation between time elapsed since injury to first medical aid and incidence of renal failure. If sepsis and renal insufficiency were controllable and responsive to conservative measures, we avoided amputation operations.
In conclusion, it is clearly not possible at present to prevent an earthquake or to estimate the time, location and severity of earthquake damage and injury. On the other hand, investigation of the injuries profile of patients associated with earthquake will have a positive effect on rescue attempts and treatment planning for musculoskeletal injuries caused by future disasters.
Contributor Information
Savas Guner, Phone: +90-533-2433873, Email: gunersavas@gmail.com.
Sukriye Ilkay Guner, Email: ilkay.guner@hotmail.com.
Yasemin Isik, Email: yaseminmd@yahoo.com.
Gokay Gormeli, Email: ggormeli@yahoo.com.
Ali Murat Kalender, Email: kalenderalimurat@hotmail.com.
Ugur Turktas, Email: uturktas@yahoo.com.
Mehmet Ata Gokalp, Email: doktorata@hotmail.com.
Abdurrahim Gozen, Email: abdurrahimgozen@hotmail.com.
Mustafa Isik, Email: drmustafaisik@yahoo.com.
Sezai Ozkan, Email: doktorsezai@hotmail.com.
Tulin Turkozu, Email: tturkozu@hotmail.com.
Sevdegul Karadas, Email: sevdegulkaradas@yahoo.com.tr.
Mehmet Fethi Ceylan, Email: mfethiceylan@hotmail.com.
Levent Ediz, Email: leventediz@gmail.com.
Mehmet Bulut, Email: bulmeh@yahoo.com.
Yusuf Gunes, Email: hyusufgunes@hotmail.com.
Ayse Gormeli, Email: ayseyazici@yahoo.com.
Cemil Erturk, Email: erturkc@yahoo.com.
Metehan Eseoglu, Email: metehaneseoglu@gmail.com.
Recep Dursun, Email: drrecepdursun@hotmail.com.
References
- 1.Aylwin CJ, König TC, Brennan NW, Shirley PJ, Davies G, Walsh MS, Brohi K. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. 2006;368:2219–2225. doi: 10.1016/S0140-6736(06)69896-6. [DOI] [PubMed] [Google Scholar]
- 2.Hirshberg A, Holcomb JB, Mattox KL. Hospital trauma care in multiplecasualty incidents: a critical view. Ann Emerg Med. 2001;37:647–652. doi: 10.1067/mem.2001.115650. [DOI] [PubMed] [Google Scholar]
- 3.Seaman J. Disaster epidemiology: or why most international disaster relief is ineffective. Injury. 1990;21:5–8. doi: 10.1016/0020-1383(90)90143-I. [DOI] [PubMed] [Google Scholar]
- 4.Buckenmaier CC, 3rd, Lee EH, Shields CH, Sampson JB, Chiles JH. Regional anesthesia in austere environments. Reg Anesth Pain Med. 2003;28:321–327. doi: 10.1016/s1098-7339(03)00198-6. [DOI] [PubMed] [Google Scholar]
- 5.Mellor AJ. Anaesthesia in austere environments. J R Army Med Corps. 2005;151:272–276. doi: 10.1136/jramc-151-04-09. [DOI] [PubMed] [Google Scholar]
- 6.Mulvey JM, Awan SU, Qadri AA, Maqsood MA. Profile of injuries arising from the 2005 Kashmir earthquake: the first 72 h. Injury. 2008;39(5):554–560. doi: 10.1016/j.injury.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 7.Bulut M, Fedakar R, Akkose S, Akgoz S, Ozguc H, Tokyay R. Medical experience of a university hospital in Turkey after the 1999 Marmara earthquake. Emerg Med J. 2005;22:494–498. doi: 10.1136/emj.2004.016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuwagata Y, Oda J, Tanaka H, et al. Analysis of 2702 traumatized patients in the 1995 Hanshin-Awaji earthquake. J Trauma. 1997;43(3):427–432. doi: 10.1097/00005373-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Fan Z, Li A, Lian B, Zhou B, Wei H, Chen C, Xu P. Injury types of victims in the 12th May 2008 Wenchuan earthquake: analysis of 1,038 patients in Jiangyou City. Eur J Trauma Emerg Surg. 2011;37:3–7. doi: 10.1007/s00068-010-0045-6. [DOI] [PubMed] [Google Scholar]
- 10.Tahmasebi MN, Kiani K, Mazlouman SJ, Taheri A, Kamrani RS, Panjavi B, et al. Musculoskeletal injuries associated with earthquake. A report of injuries of Iran’s December 26, 2003 Bam earthquake casualties managed in tertiary referral centers. Injury. 2005;36:27–32. doi: 10.1016/j.injury.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Hee-Nee P, Wilfred L, Wei-Chong C, Benjamin S. Management of musculoskeletal injuries after the 2009 western Sumatra earthquake. J Orthop Surg. 2011;19(1):3–7. doi: 10.1177/230949901101900102. [DOI] [PubMed] [Google Scholar]
- 12.Sechriest VF, 2nd, Lhowe DW. Orthopaedic care aboard the USNS mercy during operation unified assistance after the 2004 Asian tsunami: A case series. J Bone Joint Surg Am. 2008;90:849–861. doi: 10.2106/JBJS.G.00821. [DOI] [PubMed] [Google Scholar]
- 13.Wolfson N. Amputation in natural disasters and mass casualties: staged approach. Int Orthop. 2012;36(10):1983–1988. doi: 10.1007/s00264-012-1573-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herard P. Amputation in emergency situations: indications, techniques and MSF-France’s experience in Haiti. Int Orthop. 2012;36(10):1979–1981. doi: 10.1007/s00264-012-1552-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rigal S. Extremity amputation: how to face challenging problems in a precarious environment. Int Orthop. 2012;36(10):1989–1993. doi: 10.1007/s00264-012-1548-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinsenkamp M. SICOT contribution to natural disasters assistance. Int Orthop. 2012;36:1977–1978. doi: 10.1007/s00264-012-1554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Demey D. Post-amputation rehabilitation in emergency crisisfrom pre-operative to community. Int Orthop. 2012;36(10):2003–2005. doi: 10.1007/s00264-012-1553-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Awais SM. Amputations of limbs during the 2005 earthquake in Pakistan: a first hand experience of the author. Int Orthop. 2012;36(11):2323–2326. doi: 10.1007/s00264-012-1589-3. [DOI] [PMC free article] [PubMed] [Google Scholar]