Abstract
Purpose
Functional results of reversed total prostheses (RTP) have—to a very limited degree—been compared with those of other shoulder prosthesis types. The aim of our study was to compare results of four different types of shoulder prostheses in terms of function, pain, and quality of life (QoL).
Methods
Questionnaires were completed by 859 patients with shoulder prostheses registered in the Norwegian Arthroplasty Register. Patients with osteoarthritis (OA), rheumatoid arthritis (RA), or fracture sequela (FS) were included. Symptoms and function were assessed using the Oxford Shoulder Score (OSS, scale 0–48), and the EuroQoL-5D (EQ-5D) was used to assess QoL.
Results
Best functional results were obtained using conventional total prostheses (TPs) and RTPs —mean OSS improvement 18 and 16 units, respectively, vs 11 with hemiprostheses (HPs). For patients with OA, TPs performed best; for those with RA and FS, RTPs performed best; and those with HPs had the worst results in all diagnostic groups. The greatest improvement in QoL was seen in patients with TPs and RTPs.
Conclusions
Conventional TPs provide the best improvement in pain, function and QoL in OA patients; RTPs are superior in patients with RA and FS.
Introduction
Only a few randomised controlled trials (RCTs) have been performed to study shoulder replacement surgery [1–5]. In a recent Cochrane review assessing surgery for shoulder osteoarthritis (OA), total shoulder prostheses (TPs) compared favourably with hemiprostheses (HP) with respect to shoulder function, but no difference in pain or quality of life QoL was found [6]. To our knowledge, no previous study comparing functional results for the four major shoulder prosthesis types has been published.
An increased rate of complications has been reported in relation to the reverse total prostheses (RTPs) [7], but clinical results have been promising [8]. Prosthesis survival is often used as a measure of success in arthroplasty surgery, being a tough and reliable outcome measure. Even so, it has been shown that although revision rates do not differ between treatment groups, there may be differences in the degree of pain experienced by the patients [9]. The Norwegian Arthroplasty Register (NAR) lacks information on functional results and pain, and to collect such information, patients with shoulder arthroplasties reported in the NAR were posted a questionnaire in 2010. The aim of the study was to evaluate and compare results of four major types of shoulder prosthesis in terms of function, pain and QoL.
Materials and methods
A more detailed description of patients and methods can be found in our previous publication from the same survey [10].
Participants
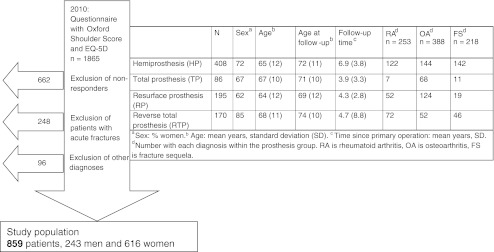
In February 2010, questionnaires were posted to all patients aged 18 years or more with a shoulder arthroplasty reported to the NAR from 1994 to 2008 for any diagnosis except cancer (n = 1,865). The inclusion process is shown in Fig. 1. Nonresponders were older (mean 70 vs 66 years), and there were more women nonresponders (79 % vs 72 %). The five year prosthesis survival rate was 89 % in nonresponders and 91 % in responders, p = 0.31.
Fig. 1.
Inclusion of patients and patient characteristics
Data on patient demographics, diagnosis and type of prosthesis were obtained from the NAR (Fig. 1). More than one diagnosis may be registered in the NAR, but in this study, each patient was assigned one diagnosis according to a system in which FS ranked above RA and OA and RA ranked above OA. Sixty-four patients underwent at least one revision operation. Patients having undergone revision were analysed together with the other patients, but in addition, separate analyses were performed for these patients. Along with the questionnaire, a patient information letter and consent form was sent to and completed by all participants. The project was approved by the Regional Committee for Medical Research Ethics, Western Norway (date of issue: 07/01/2009; registration number: 246:09).
Implants
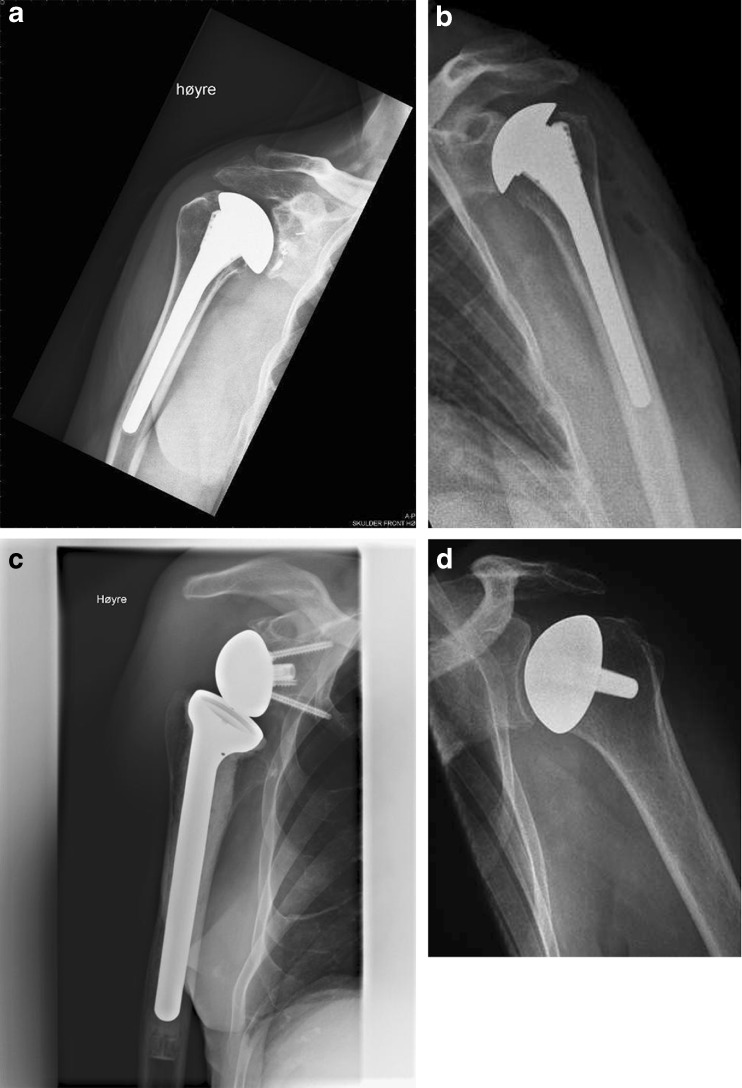
A complete list of all prosthesis brands used in the study is found in the annual report 2009 from the NAR http://nrlweb.ihelse.net/default.htm. Patients were divided into four groups according to prosthesis type: TP (Fig. 2a), HP (Fig. 2b), RTP (Fig. 2c) and resurfacing hemiprosthesis (RP, Fig. 2d). The use of these prosthesis types within each diagnostic group is shown in Fig. 1. No resurfacing total prostheses were reported to the register.
Fig. 2.
a Anatomical total prosthesis, b hemiprosthesis, c reverse total prosthesis, d resurfacing prosthesis
Outcome measures
The primary outcome measure was the Oxford Shoulder Score (OSS), which assesses patient-reported symptoms and function in relation to shoulder surgery [11]. The OSS consists of 12 items scored from 0 to 4, and in Table 1 mean results for each item are given. A total OSS ranging from 0 to 48 was calculated based on all 12 items. The patients completed one questionnaire concerning symptoms and function presurgery and another relating to the time of receiving the questionnaire. For the presurgery questionnaire, patients were specifically asked to address the time before the primary operation. Presurgery results were designated “preoperative” and results concerning the time of completing the questionnaire “present”. In accordance with a previous publication, the minimal clinically important difference (MCID) for the OSS was set at 4.5 points (about 10 % of the range) [12].
Table 1.
Mean end score and change for each of the 12 Oxford Shoulder Score (OSS) items in patients with four prosthesis types
| OSS item a | Mean end score/change | P valueb | |||
|---|---|---|---|---|---|
| Hemiprosthesis | Total prosthesis | Resurfacing prosthesis | Reverse prosthesis | ||
| Worst pain | 2.7/1.1 | 2.1/1.9 | 2.7/1.3 | 2.3/1.6 | <0.001/<0.001 |
| Dressing | 2.5/0.9 | 1.9/1.5 | 2.2/1.0 | 2.2/1.2 | <0.001/<0.001 |
| Car/public transport | 2.1/0.6 | 1.7/0.9 | 1.8/0.6 | 2.0/0.8 | 0.003/0.01 |
| Knife and fork | 2.0/0.8 | 1.7/1.0 | 1.7/0.8 | 2.0/1.1 | 0.01/0.089 |
| Shopping | 2.3/0.5 | 1.8/1.0 | 2.0/0.7 | 2.3/0.8 | 0.001/0.01 |
| Carry tray | 2.6/0.8 | 2.0/1.4 | 2.2/0.9 | 2.6/1.1 | <0.001/0.002 |
| Brush hair | 3.2/1.0 | 2.2/1.9 | 2.4/1.5 | 2.8/1.4 | <0.001/<0.001 |
| Usual pain | 3.2/1.3 | 2.4/2.3 | 3.1/1.4 | 2.8/1.8 | <0.001/<0.001 |
| Hang clothes | 3.3/0.9 | 2.5/1.9 | 2.6/1.3 | 2.8/1.5 | <0.001/<0.001 |
| Wash under arms | 2.6/1.0 | 1.9/1.9 | 2.1/1.3 | 2.1/1.6 | <0.001/<0.001 |
| Pain influence on work | 2.8/0.8 | 2.2/1.6 | 2.5/1.1 | 2.5/1.3 | <0.001/<0.001 |
| Pain at night | 2.6/1.3 | 2.1/2.1 | 2.7/1.4 | 2.3/1.7 | <0.001/<0.001 |
aThe complete questions may be found at: http://www.orthopaedicscore.com/scorepages/oxford_shoulder_score.html
bEstimated using analysis of variance (ANOVA)
A secondary outcome measure was the EuroQoL-5D (EQ-5D), which assesses QoL using a three-level system with the following five dimensions: mobility, self-care, usual activities, pain/discomfort, anxiety/depression [13]. The EQ-5D index score is calculated using population-based preference weights, and the score ranges from 0 to 1, where 1 represents perfect health and 0 is death. Negative values are allowed and represent a health status considered worse than death. Also included in the EQ-5D is a 20-cm vertical visual analogue scale (EQ-VAS) ranging from 0 to 100, where 0 is worst imaginable health state and 100 is best imaginable health state.
Statistics
Differences in mean change of EQ-5D between prosthesis groups were assessed using analysis of variance (ANOVA, Table 2). A multiple linear regression model with adjustment for diagnosis, age (≤60, 60–70, >70), sex and follow-up time was used to estimate differences in mean OSS change between groups (Table 3). In addition, separate analyses comparing the four prosthesis types within each diagnostic group (OA, RA, FS) were performed (results given in text only), as were separate analyses comparing results for patients never revised to those having undergone at least one revision, adjusting for age, sex, diagnosis, follow-up time and prosthesis type.
Table 2.
Crude mean [standard deviation (SD)] preoperative and present Oxford Shoulder Score (OSS) and EuroQoL-5D (EQ-5D), and mean change in OSS and EQ-5D, according to prosthesis type
| Mean (SD) preoperative | Mean (SD) present | Mean (SD) change | P valuea | ||
|---|---|---|---|---|---|
| OSS total | Hemiprosthesis (n = 408) | 17 (10) | 28 (12) | 11 (14) | |
| Total prosthesis (n = 86) | 16 (8) | 35 (13) | 19 (14) | ||
| Resurfacing prosthesis (n = 195) | 18 (8) | 32 (12) | 14 (12) | ||
| Reverse total prosthesis (n = 170) | 15 (9) | 32 (13) | 17 (14) | ||
| EQ-5D | Hemiprosthesis (n = 408) | 0.43 (0.26) | 0.59 (0.24) | 0.17 (0.32) | <0.001 |
| Total prosthesis (n = 86) | 0.37 (0.21) | 0.73 (0.26) | 0.36 (0.32) | ||
| Resurfacing prosthesis (n = 195) | 0.38 (0.19) | 0.64 (0.26) | 0.26 (0.29) | ||
| Reverse total prosthesis (n = 170) | 0.34 (0.20) | 0.62 (0.24) | 0.28 (0.29) | ||
| EQ-5D VAS | Hemiprosthesis (n = 408) | 47 (25) | 60 (26) | 13 (31) | 0.001 |
| Total prosthesis (n = 86) | 47 (22) | 71 (24) | 24 (33) | ||
| Resurfacing prosthesis (n = 195) | 46 (23) | 67 (24) | 22 (29) | ||
| Reverse total prosthesis (n = 170) | 43 (23) | 66 (25) | 24 (35) | ||
No statistic given for OSS because this is given in the adjusted analysis in Table 3
VAS visual analague scale
aDifference in improvement of EQ-5D and EQ-5D VAS, between the four prosthesis groups
Table 3.
Difference in change from preoperative to present Oxford Shoulder Score (OSS) by diagnosis and prosthesis type, adjusted for sex, age and follow-up time
| Numbera | Mean changeb | Adjusted differencec | 95 % confidence interval | P valuec | |
|---|---|---|---|---|---|
| Prosthesis type | |||||
| Hemiprosthesis | 354 | 10.9 | Ref | ||
| Total prosthesis | 78 | 17.8 | 6.8 | (3.4 to 10.3) | <0.001 |
| Resurfaced | 177 | 12.8 | 1.9 | (−0.7 to 4.5) | 0.16 |
| Reverse | 153 | 16.2 | 5.2 | (2.6 to 7.9) | <0.001 |
| Diagnosis | |||||
| Fracture sequela | 191 | 11.4 | Ref | ||
| Rheumatoid arthritis | 235 | 16.0 | 4.7 | (1.9 to 7.4) | 0.001 |
| Osteoarthritis | 336 | 15.9 | 4.6 | (2.0 to 7.1) | 0.001 |
| Sex | |||||
| Male | 214 | 12.3 | Ref | ||
| Female | 548 | 14.0 | 2.0 | (−0.3 to 4.3) | 0.08 |
| Age in years | |||||
| <60 | 220 | 13.4 | Ref | ||
| 60–70 | 250 | 14.5 | 0.8 | (−1.8 to 3.4) | 0.54 |
| >70 | 292 | 12.7 | −1.7 | (−4.3 to 0.9) | 0.21 |
aNumber = 762 because 97 patients had missing values for at least one of the included variables
bFor diagnosis and prosthesis type, mean changes were adjusted for sex, age, and follow-up time while unadjusted mean change was given for sex and age groups
cDifference in change compared with reference group and corresponding P values calculated using linear regression analysis adjusting for variables in the table as well as for follow-up time
Due to a difference in mean follow-up time for prosthesis types (Fig. 1), analyses were adjusted for follow-up time. Furthermore, separate analyses were performed for a subgroup of patients operated upon between 2002 and 2008. The significance level was set at 5 %, and all p values were two-tailed. All analyses were performed using SPSS version 17.0 (SPSS Inc. Chicago, IL, USA).
Results
Pain and function according to prosthesis type
Patients with TPs had best mean end result for all 12 OSS items, followed by patients with RPs and RTPs. In the TP group, the greatest degree of improvement for all but one item was also seen (Table 1). Patients with RTPs had second-best results in terms of improvement for all but two items, whereas for all items, the worst end result and the smallest degree of improvement was seen in patients with HPs (Table 1). When considering total OSS, patients with TPs, RTPs and RPs reported best end results, as opposed to HP patients (35 vs 28 for TP vs HP, Table 2). The greatest improvement in OSS was seen in patients with TPs whose mean improvement was 18 units , 6.8 units more than the HP group (p < 0.001, Table 3), the difference thus exceeding the MCID for OSS (4.5 units). Patients with RTPs also had good results, with an OSS improvement of 5.2 units more than HP patients (p < 0.001, Table 3). When comparing patients with and without revision, a mean OSS improvement of 7 units was found in revised patients compared with 14 in those never revised (p < 0.001).
Patients with rheumatoid arthritis, osteoarthritis and fracture sequelae
In all three diagnostic groups, HPs performed worst. Apart from this, some differences were observed between groups.
Osteoarthritis
OA patients with TPs reported remarkably good results, with a mean improvement in OSS of 20 units and an end result of 37 units, followed by patients with RTPs (mean improvement 17 units). A 13-unit change was seen for HPs and RPs (p < 0.001 for TP vs HP and p = 0.07 for RTP vs HP).
Rheumatoid arthritis
In the RA group, the magnitude of improvement with TPs, RPs and RTPs was similar (mean OSS improvement 17 for TP and RTP, 16 for RP and 13 for HP). However, only RTPs were statistically significantly better than HPs (p = 0.032), but the number of RA patients with TPs was low (n = 7).
Fracture sequelae
FS patients obtained best results with RTPs or RPs (mean OSS improvement 15 units), whereas a smaller improvement was obtained with TPs (10 units). HPs performed particularly badly, with a mean improvement in OSS of 7 units (p = 0.007 and 0.07 for RTP and RP vs HP, respectively).
Quality of life
The best end results for QoL were reported by patients with TPs, and the mean improvement in EQ-5D was twice that seen in the HP group (p < 0.001, Table 2). Furthermore, an improvement in EQ-5D VAS of 22–24 units was reported by patients with TPs, RTPs and RPs compared with 13 units for HPs (p = 0.001, Table 2).
Patients operated upon 2002–2008
In patients operated upon between 2002 and 2008, similar results were found, but differences in OSS and EQ-5D between TPs and HPs were even more pronounced. For instance, the adjusted difference in OSS-change between TPs and HPs was 8.2 in patients operated upon from 2002 to 2008 compared with 6.8 for all patients.
Discussion
The main finding of our study was that patients provided with total prostheses, conventional or reverse, had superior results compared with hemiprostheses in terms of improved function, pain and QoL. Similar findings were reported in some previous articles comparing HP and TP [14–16], but results on RTP were not given in those studies.
Conventional and reverse total shoulder arthroplasty
In our study, the best end results as well as the greatest improvement in pain, function and QoL, were seen in OA patients with TPs. This confirms the results of some previous studies [1, 2, 17]. We had no information on the state of the rotator cuff in our patients. Clinical experience would suggest that an RTP was more often used in patients with cuff tears. No RCTs have been performed comparing different prosthesis types in patients with RA [18]. Trail et al. found no difference in pain or function between RA patients with HPs or TPs [19], whereas Sperling et al., who reported no difference between TPs and HPs in RA patients with thin or torn rotator cuffs, found greater improvement with TPs than in HPs in patients with intact rotator cuffs [20]. Among RA patients in our study, RTPs were used much more frequently than TPs, and RTPs performed very well in this patient group. Good functional results and pain relief have previously been demonstrated for RTPs and in patients with RA [21–24], although no comparison of RTPs to HPs has previously been published. The frequent incidence of damaged rotator cuff in RA patients suggests the use of RTPs rather than TPs; randomised studies are needed to further investigate this.
In our study, RTPs were frequently used in patients with FS and performed better than both TPs and HPs. One reason for this might be that these patients often have damaged rotator cuffs and thus benefit from the design of the reverse implants, as was suggested in a previous publication [25].
Hemiprostheses and resurfacing hemiprostheses
Patients with HPs performed worst both for separate OSS items and total OSS, and the difference between HPs and TPs was clinically (greater MCID) and statistically significant. This is in agreement with findings of a previous study in which 46 % of patients with HPs vs 73 % of those with TPs reported themselves to be very satisfied [26]. The follow-up time was longer for patients with HPs, which might have influenced results adversely for the HP group. However, adjustment for follow-up time had little impact on findings; subanalyses assessing only patients operated upon after 2001 revealed the same or even more pronounced differences in OSS and EQ-5D between TPs and HPs. The results of HPs in patients with FS were so inferior that we believe no patients with FS should be treated using an HP if it can be avoided. The inferior results of HPs in general are in contrast to those of good implant survival of HPs shown in some previous studies [27, 28]. This indicates that prosthesis survival is not a sufficient measure of success for shoulder arthroplasty surgery. OSS end results were better for RPs than HPs, but no statistically significant difference in OSS improvement between RP and HP was found. However, with regards to QoL, results were better for RPs than for HPs both in terms of improvement and end results. Moreover, FS patients obtained best OSS results with RPs and RTPs.
Strengths and weaknesses
A weakness of this study is the responder rate of 65%. Reminders were sent to all nonresponders, but even so, we did not reach a higher response rate. Although nonresponders differed slightly in age and gender from responders, the five year implant survival rate was not significantly different between them. Even so, we cannot exclude the possibility of nonresponders being somewhat worse than responders. Another weakness is the retrospective collection of preoperative scores. However, we believe these scores may be trusted for several reasons. Firstly, with this large number of patients, it is reasonable to assume that patients will remember to a similar extent. Secondly, even if patients do exaggerate their preoperative complaints, the change in the score mirrors their perception of improvement due to the operation, which is really what counts. The length of follow-up might influence patients’ recollection of the presurgery state, and thus a difference in follow-up time could influence results. For this reason, subanalyses were performed for patients treated between 2002 and 2008, with the finding of an even greater difference in results for TP vs HP. Finally, this was an observational study in which prosthesis type was not randomly allocated. Analyses were adjusted for all known possible confounders (such as age, gender, diagnosis and follow-up time), but even so, we may not rule out the possibility of unknown confounding factors influencing the results.
The most important strength of the study is its large population, allowing comparison of prosthesis types with adjustment for possible confounders, and with comparison within three diagnostic groups. We are not aware of any previous studies comparing the four major types of shoulder prostheses focusing on function, pain and QoL. In particular, functional results of RTPs have, to a very limited degree, been compared with those of other prosthesis types. Pfaler et al. included a similar study population, but only conventional HPs and TPs were compared [15]; our results are in accordance with their findings. Furthermore, as patients were identified using the NAR, patients populations operated upon at all types of hospitals and having a large spectrum of implants were contacted and included, resulting in good external validity. Although an RCT comparing the four prosthesis types in the major diagnostic groups would be desirable to confirm our results, such a study might be difficult to undertake because of the need for a large study population. We believe that the results obtained in our study add new information regarding which prosthesis to select in given patient groups.
Conclusions
Best clinical results in terms of pain relief and improved function and QoL were obtained with TPs, and RTPs. TPs performed best in OA patients, whereas RTPs yielded good results in patients with RA and FS. HPs performed worst for all measured outcomes.
Acknowledgements
We thank the Norwegian surgeons for delivering data to the NAR and the patients for taking the time and trouble to answer our questionnaire. Furthermore, we are grateful to all secretaries and other coworkers at the NAR for helping in the process of distributing and collecting questionnaires.
Contributions of authors
BTSF had full access to all data and takes responsibility for the integrity and accuracy of the data analysis. Study concept and design: BTSF, SHLL, GB, AS, LIH, OF. Data acquisition: BTSF, SHLL, GB, OF. Data analysis and interpretation: BTSF, SHLL, LIH, OF. Drafting of manuscript: BTSF. Critical revision of the manuscript for important intellectual content: All authors. Final approval of the submitted version: All authors.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Lo IK, Litchfield RB, Griffin S, Faber K, Patterson SD, Kirkley A. Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis. A prospective, randomized trial. J Bone Joint Surg Am. 2005;87(10):2178–2185. doi: 10.2106/JBJS.D.02198. [DOI] [PubMed] [Google Scholar]
- 2.Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am. 2000;82(1):26–34. doi: 10.2106/00004623-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Rahme H, Mattsson P, Wikblad L, Nowak J, Larsson S. Stability of cemented in-line pegged glenoid compared with keeled glenoid components in total shoulder arthroplasty. J Bone Joint Surg Am. 2009;91(8):1965–1972. doi: 10.2106/JBJS.H.00938. [DOI] [PubMed] [Google Scholar]
- 4.Kircher J, Wiedemann M, Magosch P, Lichtenberg S, Habermeyer P. Improved accuracy of glenoid positioning in total shoulder arthroplasty with intraoperative navigation: a prospective-randomized clinical study. J Shoulder Elbow Surg. 2009;18(4):515–520. doi: 10.1016/j.jse.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Avidor C, Krishnan SG, Walch G, Kempf JF, Mole D. Cemented polyethylene vs uncemented metal-backed glenoid components in total shoulder arthroplasty: a prospective, double-blind, randomized study. J Shoulder Elbow Surg. 2002;11(4):351–359. doi: 10.1067/mse.2002.125807. [DOI] [PubMed] [Google Scholar]
- 6.Singh JA, Sperling J, Buchbinder R, McMaken K (2010) Surgery for shoulder osteoarthritis. Cochrane Database Syst Rev (10):CD008089. doi:10.1002/14651858.CD008089.pub2 [DOI] [PubMed]
- 7.Farshad M, Gerber C. Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop. 2010;34(8):1075–1082. doi: 10.1007/s00264-010-1125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mizuno N, Denard PJ, Raiss P, Walch G. The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop. 2012;36(8):1647–1653. doi: 10.1007/s00264-012-1539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray DW, Frost SJ. Pain in the assessment of total knee replacement. J Bone Joint Surg Br. 1998;80(3):426–431. doi: 10.1302/0301-620X.80B3.7820. [DOI] [PubMed] [Google Scholar]
- 10.Fevang BT, Lygre SH, Bertelsen G, Skredderstuen A, Havelin LI, Furnes O (2012) Good function after shoulder arthroplasty. Acta Orthop. doi:10.3109/17453674.2012.720118 [DOI] [PMC free article] [PubMed]
- 11.Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78(4):593–600. [PubMed] [Google Scholar]
- 12.Wilson J, Baker P, Rangan A. Is retrospective application of the Oxford Shoulder Score valid? J Shoulder Elbow Surg. 2009;18(4):577–580. doi: 10.1016/j.jse.2009.02.024. [DOI] [PubMed] [Google Scholar]
- 13.EuroQol–a new facility for the measurement of health-related quality of life. The EuroQol Group (1990). Health Policy 16(3):199–208 [DOI] [PubMed]
- 14.Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am. 2005;87(9):1947–1956. doi: 10.2106/JBJS.D.02854. [DOI] [PubMed] [Google Scholar]
- 15.Pfahler M, Jena F, Neyton L, Sirveaux F, Mole D. Hemiarthroplasty vs total shoulder prosthesis: results of cemented glenoid components. J Shoulder Elbow Surg. 2006;15(2):154–163. doi: 10.1016/j.jse.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review. J Shoulder Elbow Surg. 2007;16(4):396–402. doi: 10.1016/j.jse.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Nemoz C, Walch G. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Shoulder Elbow Surg. 2003;12(3):207–213. doi: 10.1016/S1058-2746(02)86804-5. [DOI] [PubMed] [Google Scholar]
- 18.Christie A, Dagfinrud H, Engen Matre K, Flaatten HI, Ringen Osnes H, Hagen KB (2010) Surgical interventions for the rheumatoid shoulder. Cochrane Database Syst Rev (1):CD006188. doi:10.1002/14651858.CD006188.pub2 [DOI] [PubMed]
- 19.Trail IA, Nuttall D. The results of shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Br. 2002;84(8):1121–1125. doi: 10.1302/0301-620X.84B8.12695. [DOI] [PubMed] [Google Scholar]
- 20.Sperling JW, Cofield RH, Schleck CD, Harmsen WS. Total shoulder arthroplasty vs hemiarthroplasty for rheumatoid arthritis of the shoulder: results of 303 consecutive cases. J Shoulder Elbow Surg. 2007;16(6):683–690. doi: 10.1016/j.jse.2007.02.135. [DOI] [PubMed] [Google Scholar]
- 21.Young AA, Smith MM, Bacle G, Moraga C, Walch G. Early results of reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2011;93(20):1915–1923. doi: 10.2106/JBJS.J.00300. [DOI] [PubMed] [Google Scholar]
- 22.Ekelund A, Nyberg R. Can reverse shoulder arthroplasty be used with few complications in rheumatoid arthritis? Clin Orthop Relat Res. 2011;469(9):2483–2488. doi: 10.1007/s11999-010-1654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holcomb JO, Hebert DJ, Mighell MA, Dunning PE, Pupello DR, Pliner MD, Frankle MA. Reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Shoulder Elbow Surg. 2010;19(7):1076–1084. doi: 10.1016/j.jse.2009.11.049. [DOI] [PubMed] [Google Scholar]
- 24.John M, Pap G, Angst F, Flury MP, Lieske S, Schwyzer HK, Simmen BR. Short-term results after reversed shoulder arthroplasty (Delta III) in patients with rheumatoid arthritis and irreparable rotator cuff tear. Int Orthop. 2010;34(1):71–77. doi: 10.1007/s00264-009-0733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Warner JJ, Shah A. Shoulder arthroplasty for the treatment of rotator cuff insufficiency. Instr Course Lect. 2011;60:113–121. [PubMed] [Google Scholar]
- 26.Aldinger PR, Raiss P, Rickert M, Loew M. Complications in shoulder arthroplasty: an analysis of 485 cases. Int Orthop. 2010;34(4):517–524. doi: 10.1007/s00264-009-0780-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cil A, Veillette CJ, Sanchez-Sotelo J, Sperling JW, Schleck CD, Cofield RH. Survivorship of the humeral component in shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19(1):143–150. doi: 10.1016/j.jse.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop. 2009;80(1):83–91. doi: 10.1080/17453670902805098. [DOI] [PMC free article] [PubMed] [Google Scholar]