Abstract
Purpose
The aims of this anatomical study were to evaluate the feasibility of minimally invasive plate osteosynthesis (MIPO) using a posterolateral approach in distal tibial fractures and to study the relationship between neurovascular structures and the plate.
Methods
Two separate incisions, one proximal and one distal, were made on the posterolateral aspect of ten cadaveric legs in the prone position. A 14-hole contralateral anterolateral distal tibial locking plate was inserted into the submuscular tunnel using a posterolateral approach, and one screw was fixed on each side of the proximal and distal tibia. The MIPO tunnel was then explored to identify the relationship between neurovascular bundles and plate.
Results
For the proximal incision, retraction of the flexor hallucis longus and the tibialis posterior muscles medially was very important because it could protect the posterior tibial artery and the tibial nerve during plating. The sural nerve and lesser saphenous vein were easily identified and retracted in the superficial layer of the distal incision. In addition, we achieved satisfactory outcomes after using this MIPO technique in one patient.
Conclusion
Based on the results of our study, it seems that using the MIPO technique through a posterolateral approach should be a reasonable and safe treatment option for distal tibial fractures, especially when the anterior soft tissue is compromised. However, studies with a higher level of evidence should be done in more patients to confirm the clinical safety of using this technique.
Introduction
High-energy distal tibial or pilon fractures are normally associated with complications of soft-tissue injury, especially in the anteromedial or anterolateral aspects. Several studies show that the optimal operative technique in these fractures involves an initial external fixator in an acute setting, followed by delayed definite internal fixation after the recovery of any associated soft-tissue injury [1, 2]. The posterolateral approach to the tibia was first described by Harmon in 1945 for treating tibial nonunion [3]. This approach has also been reported in many studies as an alternative treatment for distal tibial or pilon fractures when soft-tissue concerns preclude an anterior approach [4–10]. In addition, it has shown good outcomes and fewer complications of compromised soft tissue because of the more abundant soft-tissue coverage.
Minimally invasive plate osteosynthesis (MIPO) of distal tibial fractures using an anteromedial or anterolateral approach has been popular in recent years, with satisfactory clinical outcomes, as this method has less soft-tissue disruption with preservation of fracture haematoma and blood supply to the bone fragments [11–20]. However, using a posterolateral approach with the MIPO technique in distal tibial fractures has not been previously reported in the literature. The aims of this study were to determine the possibility of applying the MIPO technique in treating distal tibial fractures using the posterolateral approach and to observe the anatomical relationships between the posterior tibial artery (PTA), tibial nerve (TN), sural nerve (SN), lesser saphenous vein (LSV) and the plate.
Materials and methods
This study was performed on ten legs from five fresh cadavers obtained within 72 hours after death. The procedures were done in the prone position. Firstly, a 2.5-cm skin incision was made at the midpoint between the posteromedial border of the distal fibula and the lateral border of the Achilles tendon, beginning at the level of the tip of the lateral malleolus and extending proximally to the distal fibular shaft (Fig. 1a). When making the distal incision, it was important to identify the SN and LSV, which are located under the superficial fascial layer. Exposure of the posterior aspect of the distal tibia was achieved by separating the interval between the peroneal tendons laterally and the muscle of the flexor hallucis longus (FHL) medially. With sharp dissection of the FHL along its lateral border, the entire posterior aspect of the tibial surface was exposed by retracting this muscle medially, which also protected the posteromedial neurovascular bundle (Fig. 1b).
Fig. 1.
a Distal and proximal skin incisions (red lines). b Cross-section of the distal tibia showing the interval plane between the peroneal muscles and the flexor hallucis longus (FHL). c Cross-section of the mid tibia showing the interval plane between the peroneal muscles and the FHL
Secondly, a 2.5-cm proximal skin incision was made about one fingerbreadth below the posterolateral border of the mid fibula in the same line as the distal incision (Fig.1a). The posterior aspect of the mid tibia was exposed by splitting between the peroneal muscles laterally and the FHL medially. A sharp dissection of the FHL muscle was made subperiosteally from the posterior border of the mid fibula. The tibialis posterior muscle (TP) was medial to the FHL along the interosseous membrane and was attached to the posteromedial aspect of tibia. Then, the TP was dissected from the interosseous membrane. Finally, the entire posterior aspect of the mid tibial surface was exposed by retracting the FHL and the TP medially, also protecting the posteromedial neurovascular bundle (Fig. 1c).
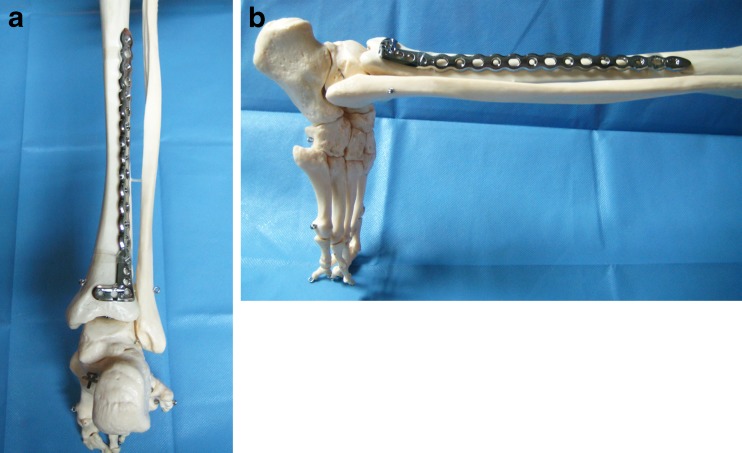
Thirdly, a submuscular extraperiosteal tunnel was created by passing a tunnelling instrument from the distal to the proximal incisions. To avoid injury to the PTA and the TN at the medial aspect of the mid tibia, the tunnelling instrument was passed along the posterolateral surface of the tibia. After preparation of the submuscular tunnel, a 14-hole contralateral anterolateral distal tibial locking plate (4.0 mm; Stryker Trauma AG, Selzach, Switzerland), which was precontoured to fit the posterolateral aspect of the tibia (plastic bone; Fig. 2a, b), was inserted from the distal to the proximal incisions following the track previously made by the tunnelling instrument (Fig. 3a).
Fig. 2.
a Precontouring the anterolateral distal tibial locking plate to the shape of the posterolateral aspect of the tibia (plastic bone) in AP view. b Precontouring the anterolateral distal tibial locking plate to the shape of the posterolateral aspect of the tibia (plastic bone) in lateral view
Fig. 3.
a Insertion of the plate from the distal to the proximal incisions. b Opening the tunnel to explore structures at risk during proximal incision [posterior tibial artery (PTA) and tibial nerve (TN); white arrow). c Measurement of distances between the neurovascular bundle (black arrow) and the plate (asterisk) at the proximal incision
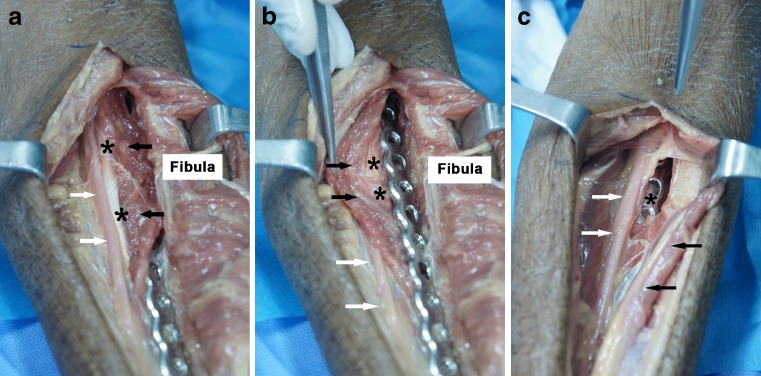
After insertion, the distal position of the plate was 1 cm above the posterior joint line of the ankle. The plate was then fixed to the distal tibia with one screw. After fixing the plate in the proximal position on the centre of the mid tibia, a second screw was inserted to secure the plate to the bone. To identify the relationship between neurovascular structures (SN/LSV, PTA, TN) and the plate in the submuscular tunnel, a longitudinal skin incision was made from the proximal to the distal incisions. The MIPO tunnel was dissected deeply into the plate (Fig. 3b). The nearest distances from the proximal and distal positions of the plate to these neurovascular structures were measured using a digital vernier calliper with precision of 0.01 mm (Insize Co., Ltd., Suzhou New District, China; Fig. 3c). Because the SN and LSV are in the subcutaneous layer of the distal incision, the distances from the most proximal and distal ends of the distal incision to these neurovascular structures were also measured using the same method. This MIPO method using a posterolateral approach was then applied in an actual patient with an open fracture of the left distal tibia. The indication for using MIPO with a posterolateral approach in this case was compromised soft tissue on the anterior aspect of the distal leg. The following data was collected for this patient: time to fracture union, range of motion of ankle joint and complications.
Results
Distal incision
As the SN and LSV are in the superficial fascial layer, they were easily identified in the distal incision in all specimens and retracted out of the way of the surgical approach. Distances from the distal end of the incision to these neurovascular structures were 2.28–6.34 mm (average 3.88 mm), which was closer than the proximal end (4.11–13.39 mm, average 8.34 mm). The closest distance measured between the plate and the neurovascular bundle was 3.19–8.37 mm (average 6.14 mm).
Proximal incision
The possibility of arterial injury was higher than the possibility of nerve injury because the closest distance between the plate and the TN (3.90–10.00 mm, average 7.30 mm) in our cadavers was more than the distance from the plate to the PTA (1.32–6.70 mm, average 4.49 mm). In consideration of this higher risk, it was very important to expose the posterior aspect of the mid tibia by sharply dissecting the FHL from the posterior mid fibula subperiosteally and then dissecting the TP from the interosseous membrane. Subsequently, the FHL and the TP were retracted medially to protect the PTA and TN and reduce the risk of neurovascular injury(Fig. 4a, b). There was a risk of PTA and/or TN injury when the dissection was made into the wrong intermuscular planes, which are between the plane of FHL and TP or medial to the TP (Fig. 4c).
Fig. 4.
a Tibial nerve (TN) and posterior tibial artery (PTA) (white arrow), just medial to the flexor hallucis longus (FHL) (black arrow) and the tibialis posterior muscle (TP) (asterisk). b To decrease the risk of neurovascular injury, the dissection was initially made between the FHL and the posterior border of the fibula. After that, the FHL (black arrow) and TP (asterisk) were retracted medially to protect the neuromuscular bundle (white arrow). c The plate (asterisk) was very close to the PTA and TN (white arrow), whereas there was no protection from the FHL and TP (black arrow)
Case presentation
A 27-year-old male patient sustained many injuries during a terrorist attack, among the injuries was a Gustilo type IIIB open fracture of the left distal tibia [Arbeitsgemeinschaft für Osteosynthesefragen (AO 43–C2)], without neurovascular or tendon injuries (Fig. 5a). The fracture was anatomically reduced at the time of debridement and primarily stabilised with a spanned external fixator over the left ankle (Fig. 5b). One week after the injury, antibiotic (Colistin) beads were placed in the exposed medial distal tibia to treat an Acinetobacter baumannii infection; this exposed bone was then covered with the sural flap (Fig. 5c).
Fig. 5.
a A 27-year-old polytraumatised male patient with a Gustilo type IIIB open comminuted fracture of the left distal tibia [Arbeitsgemeinschaft für Osteosynthesefragen (AO 43–C2)]. b Initial debridement and stabilisation with a spanned external fixator across the ankle joint. c Colistin beads (white arrow) were placed at the fracture gap, then the exposed medial distal tibia was covered by the sural flap (black arrow). d Two separate proximal and distal incisions (red lines). e Insertion of the locking plate following the track of the minimally invasive plate osteosynthesis (MIPO) tunnel. f Immediate postoperative plain radiographs showing good alignment of the distal tibial fracture. g Radiographs showing complete healing of the distal tibial fracture. h The patient had a good range of motion of the left ankle
Six weeks after the injury, the wound condition was satisfactory, and the blood sedimentation rate had returned to normal. The patient was placed in the left lateral decubitus position on a radiolucent operating table. The prone position was not appropriate for this patient because the anterior frame of the external fixator would be obscured. Our new procedure for the MIPO technique using posterolateral approach as described in the cadaveric study above was undertaken with the external fixator left in place to stabilise fracture reduction during the operation (Fig. 5d, e). A 12-hole contralateral anterolateral distal tibial locking plate (4.0 mm; Stryker), precontoured on a plastic bone before the operation, was used to stabilise this fracture. The plate was fixed with three and four screws, respectively, in the proximal and distal fragments. After that, the patient was turned to the supine position to remove the antibiotic beads through an anterolateral approach; finally, an iliac autogenous bone graft was performed at the medial defect of the left distal tibia (Fig. 5f).
The patient was encouraged to perform passive motions of the left knee and ankle during the first postoperative week. Active motion was started from the second week without any immobilisation. There were no iatrogenic neurovascular injuries. A new bridging callus was seen at the fracture site at six weeks after surgery, and complete union was achieved at six months postoperatively (Fig. 5g). Function and range of motion of the left ankle joint were satisfactory (Fig. 5h).
Discussion
Extensive soft-tissue damage and severe comminution of the bone are common problems in high-energy distal tibial or pilon fractures. Also, an open wound with severe soft-tissue injury is usually found on the medial side of the distal tibia because of the particularly thin subcutaneous tissue. The current standard treatment of this fracture is staged surgery using an MIPO technique in order to minimise further soft-tissue damage, preserve the periosteal blood supply and increase the rate of fracture healing [11, 12]. A number of studies have reported good results with an MIPO technique using both anteromedial and anterolateral approaches in treating these fractures [11–20]. Furthermore, we demonstrate the use MIPO for distal tibial fractures through a posterolateral approach in terms of anatomical safety and also report a case with an excellent outcome.
The posterolateral approach has previously been used for treating distal tibial or pilon fractures in an attempt to minimise soft-tissue problems associated with an anterior approach [4–10]. This posterolateral approach has several advantages over the traditional approaches. Firstly, reduction and fixation of both fibula and tibia can be performed using only one surgical incision [6–8, 10]. Secondly, the bulk of the FHL muscle is located above the posterior tibia, thus acting as a cushion between the tibia and the skin with subcutaneous tissue, which can minimise the incidence of wound complications and irritation from hardware compared with an anterior or medial approach [6, 8]. However, there is a significant disadvantage with this posterolateral approach, which is limited visualisation of the articular surface of the ankle, especially in cases of anterior fracture comminution when anatomical reduction is required. Also, some surgeons may not be familiar with exposing distal tibial or pilon fractures with the patient in the prone position [8]. Thus, considering the potential advantages and disadvantages, the posterolateral approach should be applied as an alternative option when treating distal tibial or pilon fractures, particularly in cases with severe anterior soft-tissue injury.
Our cadaveric anatomical study is the first to examine the possibility of using the MIPO technique to deal with distal tibial fractures through a posterolateral approach. In our study, the distal incision was close to the SN and LSV, which are in the superficial layer and run distally from the lateral border of the Achilles tendon to the anterolateral aspect of the foot (medially to laterally). Therefore, the risk of injury of these neurovascular structures is greater at the distal end than at the proximal end of the distal incision. In addition, previous studies found considerable variation in anatomy of the SN [21, 22], and it is essential if using this surgical approach that the surgeon be cautious with the dissection to avoid injury to this nerve.
Our study found that when doing this procedure, the PTA and TN were closest to the plate at the proximal incision, with average closest distances of 4.49 mm and 7.30 mm, respectively. To reduce the risk of neurovascular injury, it is crucial to dissect in the right intermuscular plane. Firstly, a sharp dissection between the FHL and posterior fibula is made. Secondly, the TP, which lies medial to the FHL, is separated from the interosseous membrane. Lastly, the FHL and TP are retracted medially and used to protect the neurovascular bundle.
We used a contralateral anterolateral distal tibial locking plate when applying the MIPO technique with a posterolateral approach in the distal tibia, because currently, there is no anatomical plate on the market for the posterior aspect of the tibia. Therefore, we recommend precontouring the plate using a plastic bone before starting the operation.
There were some limitations in this study. Our measurements were made in intact tibias, and of course, the anatomical landmarks and tissue planes are usually distorted in patients with distal tibial or pilon fractures. To overcome this problem, fracture reduction and temporary fixation with an external fixator should be performed before tunnelling and plate insertion. Also, we used a single plate design, but it should be kept in mind that the different plate lengths and thicknesses from different companies may affect the risk of neurovascular injury. Finally, only one live patient in our study underwent this surgical technique, and one patient provides only a low level of evidence. Therefore, studies with a higher level of evidence need to be done to clarify the potential benefits of this surgical technique.
Conclusion
We propose a new approach for MIPO of distal tibial fractures in cases with anterior soft-tissue problem. However, as the neurovascular structures of the distal tibia are at risk with this approach, careful dissection is essential to minimise potential complications.
Acknowledgments
The authors thank Suthorn Bavornratanavech, MD, of Bangkok Hospital Bangkok, Kanyika Chamniprasas, MD, of the Department of Orthopaedic Surgery and Physical Medicine, Faculty of Medicine, Prince of Songkla University and Theerachai Apivatthakakul, MD, of the Department of Orthopaedics, Faculty of Medicine, Chiang Mai University, for their support
Conflict of interest
The authors declare that they have no conflict of interest
References
- 1.Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999;13(2):85–91. doi: 10.1097/00005131-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Sirkin M, Sanders R, DiPasquale T, et al. A stage protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999;13(2):73–84. doi: 10.1097/00005131-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Harmon PH. A simplified surgical approach to the posterior tibia for bone-grafting and fibular transference. J Bone Joint Surg Am. 1945;27(3):496–498. [Google Scholar]
- 4.Abdelgawad AA, Kadous A, Kanlic E. Posterolateral approach for treatment of posterior malleolus fracture of the ankle. J Foot Ankle Surg. 2011;50(5):607–611. doi: 10.1053/j.jfas.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Amorosa LF, Brown GD, Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma. 2010;24(3):188–193. doi: 10.1097/BOT.0b013e3181b91927. [DOI] [PubMed] [Google Scholar]
- 6.Gobezie RG, Ponce BA, Vrahas MS. Pilon fractures: use of the posterolateral approach for ORIF. Oper Tech Orthop. 2003;13(2):113–119. doi: 10.1053/otor.2003.0171. [DOI] [Google Scholar]
- 7.Ketz J, Sanders R. Staged posterior tibial plating for the treatment of Orthopaedic Trauma Association 43C2 and 43C3 tibial pilon fractures. J Orthop Trauma. 2012;26(6):341–347. doi: 10.1097/BOT.0b013e318225881a. [DOI] [PubMed] [Google Scholar]
- 8.Konrath GA, Hopkins G., 2nd Posterolateral approach for tibial pilon fractures: a report of two cases. J Orthop Trauma. 1999;13(8):586–589. doi: 10.1097/00005131-199911000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Sheerin DV, Turen CH, Nascone JW. Reconstruction of distal tibia fractures using a posterolateral approach and a blade plate. J Orthop Trauma. 2006;20(4):247–252. doi: 10.1097/00005131-200604000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Tornetta P, 3rd, Ricci W, Nork S, et al. The posterolateral approach to the tibia for displaced posterior malleolus injuries. J Orthop Trauma. 2011;25(2):123–126. doi: 10.1097/BOT.0b013e3181e47d29. [DOI] [PubMed] [Google Scholar]
- 11.Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibia fractures: preliminary results in 21 patients. Injury. 2004;35(6):608–614. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 12.Borrelli J, Jr, Prickett W, Song E, et al. Extraosseous blood supply of the tibia and the effects of different plating techniques: human cadaveric study. J Orthop Trauma. 2002;16(10):691–695. doi: 10.1097/00005131-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Collinge C, Protzman R. Outcomes of minimally invasive osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010;24(1):24–29. doi: 10.1097/BOT.0b013e3181ac3426. [DOI] [PubMed] [Google Scholar]
- 14.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38(3):365–370. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 15.Helfet DL, Shonnard PY, Levine D, et al. Minimal invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(Suppl 1):A42–A48. doi: 10.1016/S0020-1383(97)90114-5. [DOI] [PubMed] [Google Scholar]
- 16.Mushtaq A, Shahid R, Asif M, et al. Distal tibial fracture fixation with locking compression plate (LCP) using the minimally invasive percutaneous osteosynthesis (MIPO) technique. Eur J Trauma Emerg Surg. 2009;35(2):159–164. doi: 10.1007/s00068-008-8049-1. [DOI] [PubMed] [Google Scholar]
- 17.Redfern DJ, Syed SU, Davies SJM. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004;35(6):615–620. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 18.Sohn OJ, Kang DH. Staged protocol in the treatment of open distal tibia fracture: using lateral MIPO. Clin Orthop Surg. 2011;3(1):69–76. doi: 10.4055/cios.2011.3.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maffulli N, Toms AD, McMurtie A, et al. Percutaneous plating of distal tibial fractures. Int Orthop. 2004;28(3):159–162. doi: 10.1007/s00264-004-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng W, Li Y, Manyi W. Comparison study of two surgical options for distal tibia fracture-minimally invasive plate osteosynthesis vs. open reduction and internal fixation. Int Orthop. 2011;35(5):737–742. doi: 10.1007/s00264-010-1052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lawrence SJ, Botte MJ. The sural nerve in the foot and ankle: an anatomical study with clinical and surgical implications. Foot Ankle Int. 1994;15(9):490–494. doi: 10.1177/107110079401500906. [DOI] [PubMed] [Google Scholar]
- 22.Webb J, Moorjani N, Radford M. Anatomy of the sural nerve and its relation to the Achilles tendon. Foot Ankle Int. 2000;21(6):475–477. doi: 10.1177/107110070002100604. [DOI] [PubMed] [Google Scholar]