Abstract
Purpose
Tibial nail interlocking screw failure often occurs during delayed fracture consolidation or at early weight bearing of nailed unstable fractures, in general when high implant stress could not be reduced by other means. Is there a biomechanical improvement in long-term performance of angle stable locking screws compared to conventional locking screws for distal locking of intramedullary tibial nails?
Methods
Surrogate bones of human tibiae were cut in the distal third and distal locking of the 10 mm intramedullary tibial nail was performed with either two angle stable locking screws or two conventional locking screws in the mediolateral plane. Six specimens per group were mechanically tested under quasi-static and cyclic axial loading with constantly increasing force.
Results
Angle stable locking screw constructs exhibited significantly higher stiffness values (7,809 N/mm ± 647, mean ± SD) than conventional locking screw constructs (6,614 N/mm ± 859, p = 0.025). Angle stable locking screw constructs provided a longer fatigue life, expressed in a significantly higher number of cycles to failure (187,200 ± 18,100) compared to conventional locking screw constructs (128,700 ± 7,000, p = 0.004).
Conclusion
Fatigue performance of locking screws can be ameliorated by the use of angle stable locking screws, being especially important if the nail acts as load carrier and an improved stability during fracture healing is needed.
Introduction
Intramedullary nailing has become a standard procedure of most displaced tibial shaft fractures [1–3], combining high mechanical stability with biological advantages in internal fixation [4]. With upcoming implant technology, indication for intramedullary tibial nailing has extended towards extra-articular fractures of the distal third of the bone [5, 6]. This change is accompanied by adverse effects like high rates of delayed bone healing, nonunion or malalignment and an incidence of distal locking screw failure ranging from 6 % to 14 % [1, 3, 7, 8]. Due to the anatomical fact that the intramedullary canal flares towards distal, loading of the nail–screw interface is emphasized by reduced nail–bone contact [9]. A milestone was the introduction of the angle stable locking principle for nail interlocking, which is already well established for plate osteosynthesis [10] of distal tibial fractures [11]. Compared with conventional distal locking screws, previous in vitro studies [12–14] revealed higher construct stiffness and less fracture gap motion when angle stable distal locking screws were used. However, a difference in cycles and load to failure, indicating an improved fatigue life due to angular stability, was not investigated in these studies.
In delayed fracture healing, higher shear forces have to be transmitted by the implant for longer time periods. Particularly in small diameter nails breakage of locking screws becomes a problem, increasing the importance of installing an adequate fatigue strength [15].
Angle stable distal locking of the Expert Tibial Nail (Synthes GmbH, Solothurn, Switzerland) with angle stable locking screws (ASLS) might be associated with a lower screw breakage rate, since screws toggle less inside the nail. Angular stability is achieved with special conical locking screws and a 70:30 poly(L-lactide-co-D, L-lactide) sleeve spread in the locking hole of the nail during screw insertion.
The purpose of this in vitro study was to compare the fatigue performance of the distal screw–nail interface locked with angle stable versus conventional locking screws in a tibial nail construct under cyclic axial loading.
Materials and methods
Study groups
Twelve medium, left, fourth generation, composite human tibiae (Sawbone Europe, Malmö, Sweden, Ref. nr. 3401) were used in this study. This surrogate bone was chosen because it provides a stable screw purchase in order to avoid failure at the bone–screw interface and the influence of varying bone quality on the results.
The intramedullary canal of the surrogate bone was overreamed up to 13 mm and the distal end was cut at 6.7 cm to allow tilting of the distal fragment and to mimic a clinical situation of an unstable distal third of the tibial, where the intramedullary canal flares towards the distal end of the bone. Cannulated 10 mm diameter Expert Tibial Nails (Synthes GmbH, Solothurn, Switzerland) were used in this study. The choice of this nail diameter was based on the wide use of this nail size as well as on the findings of previous studies who report screw and nail breakage in small diameter nails [3, 15]. The Expert Tibial Nail was implanted in the distal part of the synthetic bone and two distal locking holes in the mediolateral plane were drilled via a custom-made distal aiming arm (see Fig. 1).
Fig. 1.

Custom-made aiming arm. Aiming device for distal locking hole drilling was used to ensure a standardized positioning of the drill holes and to minimize influence of varying drill hole positions on the results. Plastic bars were mounted on the nail to provide a standardized positioning of the nail in the overdrilled hole of the surrogate bone. Plastic bars were removed before locking screw setting
Distal locking was performed with either conventional locking screws or angle stable locking screws. Six specimens were instrumented per group (n = 6). In the conventional locking (CL) group, nails were locked distally with two 5.0 mm conventional locking screws with bicortical purchase in the mediolateral plane. In the angle stable locking (ASLS) group, nails were locked distally with two 5.0 mm angle stable screws with biodegradable 70:30 poly(L-lactide-co-D, L-lactide) (P(L/DL)LA) sleeves (ASLS; Synthes GmbH, Solothurn, Switzerland). Nails were cut 14.7 cm proximal to the distal tip, just below the curvature, to avoid influence of nail bending on the results. The medial malleolus of the synthetic bone was cut and the distal end of the surrogate bone was potted in polymethylmethacrylate (PMMA) in a custom made metal jig. Nails and screws were made of titanium aluminum niobium alloy (TiAl6Nb7). The screws were self-tapping.
Mechanical testing
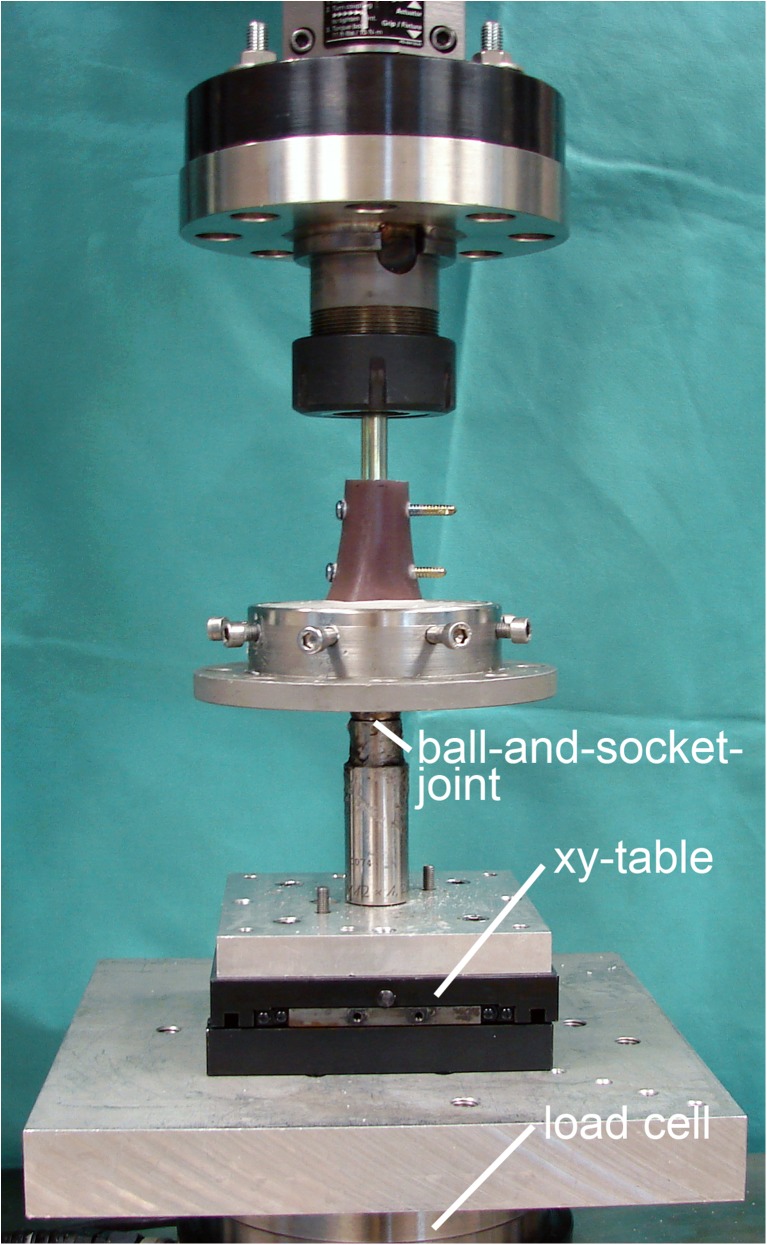
Mechanical testing was performed on a servohydraulic test system (Bionix 858; MTS Systems, Eden Prairie, MN, USA) with a 25 kN load-cell. The proximal end of the nail was rigidly fixed to the actuator of the testing machine using a chuck. The custom made metal jig with the embedded surrogate bone was connected to the load-cell of the testing machine via a ball-and-socket joint aligned with the nail axis. An x-y table was placed between test fixture and load-cell in order to provide the necessary degrees of freedom (see Fig. 2).
Fig. 2.
Test setup. The tibial nail was cut proximally and directly fixed to the actuator of the test system. The nail axis was aligned with the machine axis. The embedded specimen was connected distally via a ball-and-socket-joint and an x-y table to ensure a statically determined system
First, non-destructive quasi-static testing was performed. After one settling cycle, construct stiffness was determined from the load–displacement curve within the linear elastic range from 200 N to 500 N. Subsequently, cyclic mechanical testing was performed at a rate of 5 Hz under sinusoidal axial compression. The frequency generally used in fatigue testings (20 Hz) was set down to 5 Hz to respect the in vivo loading conditions, being close to the frequency of fast running. The first cycle of the test ranged from 100 N (valley) to 1,300 N (peak). The peak level was then regularly increased at 0.02 N/cycle until catastrophic failure of the locking screws occurred. The principle of fatigue testing with regularly increasing load levels has been proven useful previously [16]. To provide a reasonable cycle number necessary for fatigue testing, the cyclic test was designed such that failure occurred not before 100,000 cycles in both groups.
Data acquisition and analysis
Axial load and axial displacement were recorded from the test system’s transducers at a frequency of 64 Hz. Construct failure was defined as axial displacement of >3 mm. This value was considered reasonable from preceding pilot experiments. Number of cycles to failure and load to failure were determined from the displacement progression of the machine data. Construct stiffness was calculated from the load displacement curve of the machine data in the linear-elastic region (200–500 N) at the beginning of the test after a settling cycle.
The second moment of area was calculated based on the screw diameter at the screw breakage level for ASLS screws and conventional screws.
Statistical analysis was performed with the use of SPSS software (SPSS 14.0.2; SPSS, Chicago, USA). Data did not reveal normal distribution within each group as indicated by the Shapiro-Wilk test. For the detection of significant differences between the two groups regarding axial stiffness and cycles to failure, the Mann–Whitney U test was used. Significance was defined as p < 0.05.
Results
Construct stiffness
The specimens locked with ASLS screws revealed a significantly higher construct stiffness (7,809 N/mm ± 647, mean ± standard deviation) compared to the specimens locked with conventional locking screws (6,614 N/mm ± 859, p = 0.025).
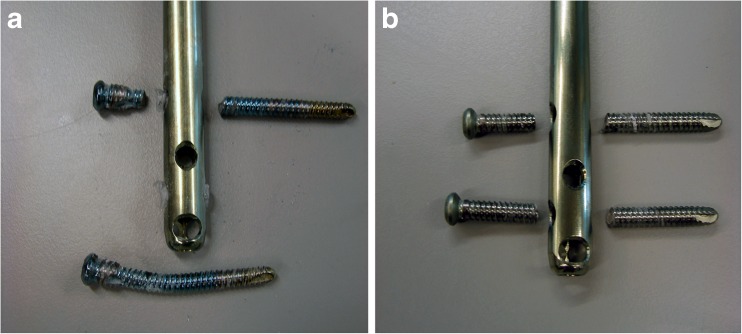
Failure mode
All specimens failed by breakage of one or two screws. We did not observe any nail breakage or fracture of the surrogate bone. Detailed failure analysis is given in Table 1. Figure 3 shows the predominant failure modes of both groups.
Table 1.
Different failure modes of angle stable locking (ASLS) screws compared to conventional locking screws (CL). Whereas in the CL group both screws broke in all specimens, the ASLS group showed screw breakage of one screw and bending of the other in 2/3 of the specimens
| Failure mode | ASLS (no. of specimens) | CL (no. of specimens) |
|---|---|---|
| 1 broken/1 bent screw | 3 proximal broken/distal bent | None |
| 1 proximal bent/distal broken | ||
| 2 broken screws | 2 | 6 |
Fig. 3.
Main screw failure modes of the groups. Screws in the angle stable locking (ASLS) group predominantly failed by breakage of one screw and bending of the other (a), whereas in the conventional locking (CL) group failure occurred in breakage of both screws (b)
Second moment of area
The second moment of area was Iy = 22.99 mm4 for ASLS screws and Iy = 23.35 mm4 for conventional locking screws.
Fatigue performance
Fatigue performance of both groups is shown in Table 2. The ASLS group exhibited a significantly longer fatigue life, expressed in a higher number of cycles to failure and correspondingly a higher load to failure. Differences between the groups were statistically significant (p = 0.004).
Table 2.
Fatigue performance of the angle stable locking (ASLS) and conventional locking (CL) group. Fatigue performance is expressed in mean cycles to failure of each group. According to our test protocol with increased peak load per cycle, the corresponding mean load to failure is given
| Group | Mean cycles to failure ± SD | Mean load to failure ± SD in N |
|---|---|---|
| ASLS (n = 6)a | 187,200 ± 18,100 | 5,084 ± 366 N |
| CL (n = 6)a | 128,700 ± 7,000 | 3,870 ± 304 N |
aDifferences between the groups were statistically significant (p = 0.004)
Discussion
This study compares the fatigue performance of nail constructs with or without angle stable distal interlocking with regard to clinical application.
This in vitro study focused on the fatigue behaviour of the interlocking screws and does not include human body environment, which could have influence on corrosion fatigue. The ASLS sleeve consists of a biodegradable polymer which degrades within 18–24 months. Considering the time period of fracture consolidation, we found this aspect dispensable. Our model assumes that the distal locking screws carry the complete load. We applied a single axial force, since the tibial is mainly loaded in axial compression. Two distal locking screws were used in this study. This configuration is widely applied in clinical practice [3, 6, 17, 18]. Screw failure could be predetermined mechanically by the second moment of area as a measure for resistance against bending. This parameter is influenced by the fourth power of the diameter for rods [3, 15, 19]. With regard to screw breakage it is therefore advisable to increase the screw diameter rather than using more screws with smaller diameter [17], whereas the stress at the screw-bone interface could be reduced by increasing the number of screws which enlarges the screw–bone contact area. We calculated the second moment of area for both ASLS screws and conventional screws to exclude an influence of the screw geometry on the observed differences in fatigue life of both constructs. The second moment of area was found comparable for both screw types, which suggests attributing the longer fatigue life to the concept of angle stable locking providing a superior screw–nail interface.
The angle stable locking system ensures mechanical coupling between nail, sleeve and screw by placing the P(L/DL)LA inlet press-fit in between nail hole and screw. It is assumed that this “elastic” configuration results in an even load sharing between the transverse interlocking elements. In contrast, the conventional fixation is likely to be afflicted to an unbalanced distribution of the load. From a mechanical standpoint this configuration is undefined since an adverse “double-fit” of both screws exists. Due to inaccuracies in screw placement one screw is likely to take the bulk of the load while the other lacks contact to the nail. As a result the screws fail successively by overloading like in our study where we observed screw breakage of both screws for all conventional screws; whereas in the ASLS group, in some specimens only one screw was broken while the other was bent.
Another important aspect is the toggling of the screws inside the hole in case of conventional fixation. Within the play of the screw this “loose-lock” stability [20] might contribute to accentuated peak forces in the event of contact between rigid screw and nail material. When using ASLS, the sleeve might create a superior condition of continuous load transfer and may act as an additional shock absorber truncating force peaks. Angle stable locking diminishes screw toggling as indicated by increased construct stiffness, which contributes to interfragmentary stability at the fracture site [21].
Previous studies [12, 14] focused mainly on the anchoring effect of ASLS screws within the bone. In contrast, the present experiment investigates the nail-screw connection, revealing a clear advantage of the angle stable locking concept. Screw loosening and bone fracture around the implant observed previously [12] could be avoided in the present study by using composite bones. However, loosening of the screws in the bone indicates that the bone/screw interface may represent a weak point of the entire repair construct, especially in osteoporotic bone [12–14].
Fatigue performance of the fixation constructs is an important mechanical property, especially if they act as load bearing devices over a long time period. Delayed union, comminution, metaphyseal location, dynamic locking of unstable fractures and bilateral tibial fractures contribute to hardware failure such as locking screw breakage [3, 15, 22].
Translation of the load cycle magnitudes into a clinical context is difficult, since patient activity and degree of post-operative load bearing range widely [17, 23, 24]. Concerning the load levels, already the start point of the cyclic test (1,300 N) corresponds to 1.9–fold body weight of a 70 kg person which indicates a sufficient load bearing capacity of either conventional or ASLS screws and does not explain screw failure. The process of implant fatigue consists of three stages: initial fatigue damage leading to crack nucleation and crack initiation, progressive cyclic growth of a crack (crack propagation) until the remaining uncracked section of a part becomes too weak to sustain the loads imposed, and finally sudden fracture of the remaining cross section appears [25]. This process explains why fatigue failure mainly occurs under cyclic stresses well below the static yield strength of the material. Ultimate loads to failure are of limited value to predict the fatigue behavior of an object. It is the cyclic activity which maintains the process. If a strategy of early postoperative weight bearing is aimed with a high number of cycles and if the stress on the screws could not be reduced by other means like cortical support in the fracture zone, a sustainable configuration of the fixation hardware should be used. This could be achieved by using larger screw diameter [15, 17] or by the concept of angle stable fixation.
Conclusion
Angle stable interlocking screws revealed a significantly longer fatigue life than conventional locking screws. This finding is especially important for cases of unstable fractures including tibial fractures in the distal third, delayed fracture healing, bilateral fractures, patient’s incompliance and generally for nailing constructs where the fixation hardware is exposed to accentuated physiological loading over long periods.
Acknowledgements
The authors thank Ursula Eberli, MSc for her excellent technical assistance.
Conflict of interest
The authors are not compensated and there are no other institutional subsidies, corporate affiliations, or funding sources supporting this work unless clearly documented and disclosed. Implants were kindly donated by Synthes GmbH, Solothurn, Switzerland.
Footnotes
Mark Lenz and Boyko Gueorguiev contributed equally to this work. This work was performed at the AO Research Institute Davos, Switzerland.
Contributor Information
Mark Lenz, Email: mark.lenz@aofoundation.org.
Boyko Gueorguiev, Email: boyko.gueorguiev@aofoundation.org.
Robert Geoff Richards, Email: geoff.richards@aofoundation.org.
Thomas Mückley, Email: Thomas.Mueckley@med.uni-jena.de.
Gunther Olaf Hofmann, Email: Gunther.Hofmann@med.uni-jena.de.
Dankward Höntzsch, Email: DHoentzsch@bgu-tuebingen.de.
Markus Windolf, Email: markus.windolf@aofoundation.org.
References
- 1.Bhandari M, Guyatt GH, Swiontkowski MF, Schemitsch EH. Treatment of open fractures of the shaft of the tibia. J Bone Joint Surg Br. 2001;83(1):62–68. doi: 10.1302/0301-620X.83B1.10986. [DOI] [PubMed] [Google Scholar]
- 2.Guo JJ, Tang N, Yang HL, Tang TS. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br. 2010;92(7):984–988. doi: 10.1302/0301-620X.92B7.22959. [DOI] [PubMed] [Google Scholar]
- 3.Whittle AP, Wester W, Russell TA. Fatigue failure in small diameter tibial nails. Clin Orthop Relat Res. 1995;315:119–128. [PubMed] [Google Scholar]
- 4.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84(8):1093–1110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 5.Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 2005;59(5):1219–1223. doi: 10.1097/01.ta.0000188936.79798.4e. [DOI] [PubMed] [Google Scholar]
- 6.Mohammed A, Saravanan R, Zammit J, King R. Intramedullary tibial nailing in distal third tibial fractures: distal locking screws and fracture non-union. Int Orthop. 2008;32(4):547–549. doi: 10.1007/s00264-007-0356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bilat C, Leutenegger A, Ruedi T. Osteosynthesis of 245 tibial shaft fractures: early and late complications. Injury. 1994;25(6):349–358. doi: 10.1016/0020-1383(94)90125-2. [DOI] [PubMed] [Google Scholar]
- 8.Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg Br. 1995;77(3):417–421. [PubMed] [Google Scholar]
- 9.Forster MC, Bruce AS, Aster AS. Should the tibia be reamed when nailing? Injury. 2005;36(3):439–444. doi: 10.1016/j.injury.2004.09.030. [DOI] [PubMed] [Google Scholar]
- 10.Frigg R. Locking compression plate (LCP). An osteosynthesis plate based on the dynamic compression plate and the point contact fixator (PC-Fix) Injury. 2001;32(2):63–66. doi: 10.1016/S0020-1383(01)00127-9. [DOI] [PubMed] [Google Scholar]
- 11.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38(3):365–370. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 12.Gueorguiev B, Ockert B, Schwieger K, Wähnert D, Lawson-Smith M, Windolf M, Stoffel K. Angular stability potentially permits fewer locking screws compared with conventional locking in intramedullary nailed distal tibia fractures: a biomechanical study. J Orthop Trauma. 2011;25(6):340–346. doi: 10.1097/BOT.0b013e3182163345. [DOI] [PubMed] [Google Scholar]
- 13.Gueorguiev B, Wähnert D, Albrecht D, Ockert B, Windolf M, Schwieger K. Effect on dynamic mechanical stability and interfragmentary movement of angle-stable locking of intramedullary nails in unstable distal tibia fractures: a biomechanical study. J Trauma. 2011;70(2):358–365. doi: 10.1097/TA.0b013e3181dbaaaf. [DOI] [PubMed] [Google Scholar]
- 14.Horn J, Linke B, Höntzsch D, Gueorguiev B, Schwieger K. Angle stable interlocking screws improve construct stability of intramedullary nailing of distal tibia fractures: a biomechanical study. Injury. 2009;40(7):767–771. doi: 10.1016/j.injury.2009.01.117. [DOI] [PubMed] [Google Scholar]
- 15.Weninger P, Schueller M, Jamek M, Stanzl-Tschegg S, Redl H, Tschegg EK. Factors influencing interlocking screw failure in unreamed small diameter nails—a biomechanical study using a distal tibia fracture model. Clin Biomech (Bristol, Avon) 2009;24(4):379–384. doi: 10.1016/j.clinbiomech.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Windolf M, Muths R, Braunstein V, Gueorguiev B, Hänni M, Schwieger K. Quantification of cancellous bone-compaction due to DHS blade insertion and influence upon cut-out resistance. Clin Biomech (Bristol, Avon) 2009;24(1):53–58. doi: 10.1016/j.clinbiomech.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 17.Griffin LV, Harris RM, Zubak JJ. Fatigue strength of common tibial intramedullary nail distal locking screws. J Orthop Surg Res. 2009;4:11. doi: 10.1186/1749-799X-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kneifel T, Buckley R. A comparison of one versus two distal locking screws in tibial fractures treated with unreamed tibial nails: a prospective randomized clinical trial. Injury. 1996;27(4):271–273. doi: 10.1016/0020-1383(95)00116-6. [DOI] [PubMed] [Google Scholar]
- 19.Boenisch UW, de Boer PG, Journeaux SF. Unreamed intramedullary tibial nailing—fatigue of locking bolts. Injury. 1996;27(4):265–270. doi: 10.1016/0020-1383(95)00150-6. [DOI] [PubMed] [Google Scholar]
- 20.Perren SM, Fernandez Dell’Oca A, Lenz M, Windolf M. Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech. 2011;78(3):190–199. [PubMed] [Google Scholar]
- 21.Wähnert D, Stolarczyk Y, Hoffmeier KL, Raschke MJ, Hofmann GO, Mückley T. The primary stability of angle-stable versus conventional locked intramedullary nails. Int Orthop. 2012;36(5):1059–1064. doi: 10.1007/s00264-011-1420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cole JD, Latta L. Fatigue failure of interlocking tibial nail implant. J Orthop Trauma. 1992;6(4):507. doi: 10.1097/00005131-199212000-00084. [DOI] [Google Scholar]
- 23.Kinkel S, Wollmerstedt N, Kleinhans JA, Hendrich C, Heisel C. Patient activity after total hip arthroplasty declines with advancing age. Clin Orthop Relat Res. 2009;467(8):2053–2058. doi: 10.1007/s11999-009-0756-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Winter CC, Brandes M, Müller C, Schubert T, Ringling M, Hillmann A, Rosenbaum D, Schulte TL. Walking ability during daily life in patients with osteoarthritis of the knee or the hip and lumbar spinal stenosis: a cross sectional study. BMC Musculoskelet Disord. 2010;11:233. doi: 10.1186/1471-2474-11-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuhn H, Medlin D (eds) (2000) ASM handbook, volume 08: mechanical testing and evaluation. ASM International