Abstract
Tricyclic antidepressant overdose is one of the most common cause of serious drug poisonings. Sometimes amitriptyline intoxication can be difficult to treat with standard treatments. At that case hemodiafiltration (HD) can be an eligible choice. We report a successful treatment of severe case using hemodiafiltration in addition to the supportive measures. Management with gastric lavage, activated charcoal, alkalinization and supportive care is the common approach and not enough for patients in deep coma. We satisfied that HD may have a beneficial role in lethal doses of amitriptyline as an additional therapy.
Keywords: Amitriptyline, hemodiafiltration, intoxication
INTRODUCTION
Tricyclic antidepressant (TCA) poisoning is one of the most common cause of serious intoxications. Amitriptyline intoxication is the most common in TCA poisonings which can be result in hypotension, cardiac dysrhtmia, depression of central nervous system (CNS) and seizures. Current therapy includes vasopressors for hypotension, sodium bicarbonate for dysrhythmia and benzodiazepine for seizures. Hemofiltration is termed hemodiafiltration (HD) when its used combination with hemodialysis. Blood is pumped through the blood compartment of a high rate of ultrafiltration is used, so there is a high rate of movement of water and solutes from blood to dialysate that must be replaced by substitution fluid that is infused directly into the blood line. The combination is useful because of its good results in removal of both large and smaller molecular weight solutes. Here we report a 25 year old man with severe amitriptyline intoxication. HD was performed after no response to conventional therapies and the result was successful.
CASE REPORT
A 24 years old previously healthy male patient was brought to emergency service in coma (GCS:3). He was found unconscious at home by his friend and there was a suicide note near him. He had taken 40 tablets of amitriptyline 25 mg (16 mg/kg) about 8 hours before admission. After admission to intensive care unit, heart rate, invasive blood pressure, central venous pressure were monitored. A total urine output was obtained during 24 hours.
On physical examination the patient was unconscious and there was no response to painful stimulus. The pupils were isochoric and light reflex was bilaterally positive. There were generalized tonic-clonic seizures but no neurological localizing signs were noted. His blood pressure was 110/60 mmHg, heart rate 130/min, respiration rate 28/min, and temperature 36.3°C. Arterial blood gas (ABG) values were pH: 7.39, pCO2: 45 mmHg, pO2: 77.5 mmHg, HCO2: 27.6 mmol/L and base excess (BE): 2.7 mmol/L. Laboratory findings of the patient were: Hemoglobin 16.3 g/dL; hematocrit, 27.6%; white blood cell count, 11.300/mm3; and platelet count, 223,000/ mm3. Serum electrolytes were sodium: 142 mmol/L, potassium: 4.5 mmol/L, urea: 0.72 mg/dL., creatinine: 0.69 mmol/L, Aspartate transaminase (AST): 33 IU/L, Alanine transaminase (ALT): 22 IU/L. Plasma drug concentration was 0.9 μg/ml. Electrocardiography (ECG) showed ventricular tachycardia with wide QRS complexes [Figure 1] and QT (0.50 ms) prolongation. Chest X-ray showed a pneumonic infiltrate, possibly due to aspiration of gastric content.
Figure 1.
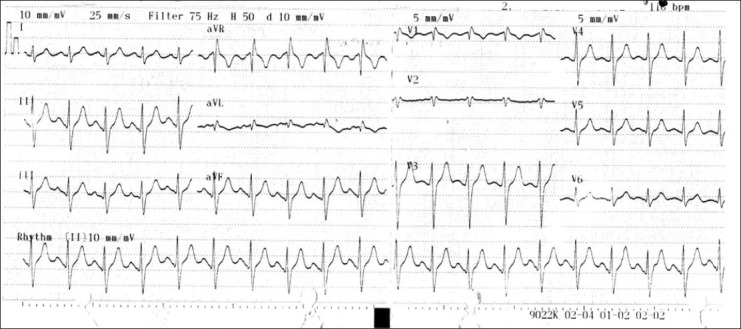
Ventricular tachycardia with wide QRS complexes and QT prolongation (0.50 ms) were detected in ECG
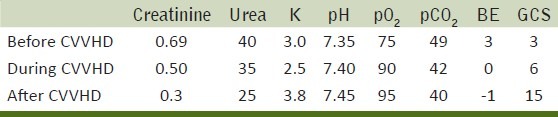
Generalized tonic-clonic seizures were stopped with midazolam. Activated charcoal (1 g/kg per dose) was administered via nasogastric tube, sodium bicarbonate (2 mEq/kg) infusion was started for alkalinization. Initially nasal oxygen with a 5 L/dk was given but 2 hours after admission to ICU because of the decrease in pO2 levels evaluated with ABG as pH: 7.35, pCO2: 49 mmHg, pO2: 75 mmHg, HCO2: 28 mmol/L and base excess (BE): 3 mmol/L the patient was intubated and mechanical ventilation support was started in SIMV mode. Yet there was no response to conventional therapies, GCS was 3 and urine output was very low (10 ml/hr). Although the level of creatinine was 0.69 mmol/L HD was performed to the patient in deep coma. It was the 15th hour of ingestion HD started and applied for 20 hours with 27 lt potassium free solution and 12000 U heparin. Flow rate was arranged between 50 and 100 ml/min according to hemodynamic condition of the patient and coagulation parameters were followed and there was no complication. Neurologic and cardiovascular status returned to normal after HD. GCS was 15 and QRS complexes were also normal [Table 1]. The patient extubated on the second day of admission. On the 3rd day laboratory findings and vital signs were stable. After psychiatric consultation he was discharged from hospital on the 4th day.
Table 1.
Various diagnostic parameters used, before, during and after hemodiafiltration
DISCUSSION
TCA overdose affects the cardiovascular, respiratory, autonomic and central nervous systems.[1] TCA exerts its therapeutic effects by inhibiting the neuronal re-uptake of noradrenaline and serotonin after the release at pre-synaptic sympathetic nerves.[2] Tricyclics are rapidly absorbed from the gastrointestinal tract and undergo first pass metabolism. They are highly protein bound and have a large volume of distribution, resulting in a long half-life of elimination that generally exceeds 24 hours and in the case of amitriptyline is 31-46 hours.[3,4] For amitriptyline serious toxicity dose varies between 10 and 30 mg/kg in adults.[5,6] Ash et al.[7] reported that the lethal dose can be variable and ingestion of more than 1 g TCA or a blood level of 1.000 mg/l predicts a high risk of mortality. Kerr et al.[3] reported that the dose ingested, even if reliably confirmed, is a poor predictor of the subsequent clinical outcome. Doses of less than 20 mg/ kg are unlikely to be fatal or cause severe complications but individual variation in absorbtion, protein binding and metabolism limit any meaningful prediction.[8,9] Boehnert et al. reported that owing to TCAs extensive tissue distribution, measurement of serum drug level has been unrewarding.[10] Our patient took 16 mg/kg amitriptyline, plasma drug concentration was 0.9 μg/ml and his condition was severe on admission.
Like all medical emergencies, initial management of TCA poisoning should focus on the support of airway, breathing and circulation. Complications like hypotension, arrhythmia, seizure and coma may develop suddenly and require immediate attention.[2]
Despite the TCA's anticholinergic effect in delaying gastric emptying, there is no consensus on the exact role of gastric lavage.[11,12] The consensus statement of European toxicologists that gastric lavage should only be performed within one hour of the ingestion of a potentially life threatening dose is based on such papers.[12]
TCA have a very large volume of distribution and this restricts the role of methods designed to increase drug clearance from the intravascular space. However, there are conflicting reports of the efficacy of hemoperfusion (HP) and HD.
It has been reported that the advice from the British poisons centres concerning the management of tricyclic overdose is not uniform.[13] Available published data of the use of HP in TCA overdose suggest that small quantities of these agents can be removed by HP.[14] Ash et al. and Frank and Klerdorf[7,15] reported that HD would only compensate the acid-base and electrolyte status. Like HD and HP, plasma exchange may also have a beneficial role in serious drug poisoning because of the high plasma protein binding rates of drugs.[5]
There is no report about HD in severe amitriptyline poisoning in literature. Although a few clinical reports suggest that HP and HD is not useful for removing TCA and its metabolites following overdose. We performed HD to our patient and satisfied its effectiveness. The improvement in our patient was dramatic. HD led to an impressive clinical improvement and hemodynamic stabilization. During HD hemodynamic parameters including mean arterial pressure, heart rate and systemic vascular resistance are mostly stable.[16] We could not perform HP which is an expensive method. Plasmapheresis needs time to prepare fresh frozen plasma so could not be performed immediately. In our conditions the best way was to choose HD.
In conclusion, the conventional methods of activated charcoal, alkalinization and symptomatic treatment of complications are not enough for comatose patients. There are different types of life-saving therapeutic approaches causing rapid improvement in symptoms. However, HD might be considered in severe amitriptyline overdose as a life-saving therapeutic approach.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Baysal T, Oran B, Doğan M, Cimen D, Elmas S, Karaaslan S. Beta-blocker treatment in an adolescent with amitriptyline intoxication. Anadolu Kardiyol Derg. 2007;7:324–5. [PubMed] [Google Scholar]
- 2.Choy CH, Kitchell AKB, Kam CW. Lethal tricyclic antidepressant overdose. Hong Kongj. emerg med. 2001;8:101–5. [Google Scholar]
- 3.Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. 2001;18:236–41. doi: 10.1136/emj.18.4.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollister L. Antidepressants. In: Katzung BG, editor. Basic and Clinical Pharmacology. 3rd ed. Connecticut: Appleton and Lange; 1987. pp. 327–35. [Google Scholar]
- 5.Erdem D, Akan B, Albayrak D, Üstünbaş P, Ugış C, Gögüs N. Plasmapheresis application in high-dose amitriptyline intoxication. Eur J Surg Sci. 2010;1:58–62. [Google Scholar]
- 6.Deegan C, O’Brien K. Amitriptyline poisoning in a 2-year old. Paediatr Anaesth. 2006;16:174–7. doi: 10.1111/j.1460-9592.2005.01624.x. [DOI] [PubMed] [Google Scholar]
- 7.Ash SR, Levy H, Akmal M, Mankus RA, Sutton JM, Emery DR, et al. Treatment of severe tricyclic antidepressant overdose with extracorporeal sorbent detoxification. Adv Ren Replace Ther. 2002;9:31–41. doi: 10.1053/jarr.2001.30475. [DOI] [PubMed] [Google Scholar]
- 8.Crome P. Poisoning due to tricyclic antidepressant overdose.Clinical presentation and treatment. Med Toxicol. 1986;1:261–85. doi: 10.1007/BF03259843. [DOI] [PubMed] [Google Scholar]
- 9.Spiker DG, Biggs JT. Tricyclic antidepressants.Prolonged plasma levels after overdose. JAMA. 1976;236:1711–2. doi: 10.1001/jama.236.15.1711. [DOI] [PubMed] [Google Scholar]
- 10.Boehnert MT, Lovejoy FH., Jr Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313:474–9. doi: 10.1056/NEJM198508223130804. [DOI] [PubMed] [Google Scholar]
- 11.Vale JA. Position statement gastric lavage.American Academy of Clinical Toxicology; European Association of poisons centres and clinical toxicologists. J Toxicol Clin Toxicol. 1997;35:11–9. doi: 10.3109/15563659709162568. [DOI] [PubMed] [Google Scholar]
- 12.Bosse GM, Barefoot JA, Pfeifer MP, Rodgers GC. Comparison of three methods of gut decontamination in tricyclic antidepressant overdose. J Emerg Med. 1995;13:203–9. doi: 10.1016/0736-4679(94)00153-7. [DOI] [PubMed] [Google Scholar]
- 13.Emerton D. British poison centres’ advice concerning dothiepin overdosage in young children. J Accid Emerg Med. 1997;14:200. doi: 10.1136/emj.14.3.200-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dönmez O, Çetinkaya M, Canbek R. Hemoperfusion in a child with amitriptyline intoxication. Pediatr Nephrol. 2005;20:105–7. doi: 10.1007/s00467-004-1654-2. [DOI] [PubMed] [Google Scholar]
- 15.Frank RD, Kierdorf HP. Is there a role for hemoperfusion/hemodialysis as a treatment option in severe tricyclic antidepressant intoxication? Int J Artif Organs. 2000;23:618–23. [PubMed] [Google Scholar]
- 16.Badawy SS, Fahmy A. Efficacy and cardiovascular tolerability of continuous veno-venous hemodiafiltration in acute decompensated heart failure: a randomized comparative study. J Crit Care. 2012;27:106.e7–13. doi: 10.1016/j.jcrc.2011.05.013. [DOI] [PubMed] [Google Scholar]


